Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Aqil B. Primary effusion lymphoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaeffusion.html. Accessed April 2nd, 2025.
Definition / general
- Primary effusion lymphoma (PEL) is a large B cell lymphoma that involves pleural, pericardial or peritoneal cavities
- There is no nodal or extranodal involvement with the exception of a presence of body cavity related tumor mass
Essential features
- PEL comprises ~4% of human immunodeficiency (HIV) related lymphomas and < 1% of non-HIV associated lymphomas
- Present with lymphomatous effusions involving serous cavities
- Large cells with immunoblastic, plasmablastic or anaplastic features
- Characteristic phenotype: dim to negative expression of CD45 and positive for CD38, CD138, HLA-DR; negative for B cell associated markers (CD19, CD20 and surface and cytoplasmic immunoglobulin light chains)
- Frequently positive for Kaposi sarcoma associated herpesvirus / human herpes virus 8 (KSHV / HHV8) and Epstein-Barr virus (EBV) encoded small RNAs (EBER)
- PEL and extracavitary PEL in HIV positive patients are usually HHV8+ and EBV+; however, in elderly HIV negative individuals, EBV is usually negative
- In extracavitary presentation, the diagnosis of HHV8 positive DLBCL, NOS should be favored in EBV negative patients with cytoplasmic IgM lambda or associated with multicentric Castleman disease
Terminology
- Primary effusion lymphoma
- Extracavitary primary effusion lymphoma
ICD coding
- ICD-11: 2A81.9 - primary effusion lymphoma
Epidemiology
- Commonly seen in HIV / AIDS patients
- HIV negative elderly individuals residing in KSHV / HHV8 endemic regions (sub-Saharan Africa and Mediterranean countries)
- Other immunosuppressed conditions, especially posttransplant state (BMC Cancer 2021;21:468)
- Incidence of PEL cases among HIV patients treated with antiretroviral therapy (ART) has increased (J Acquir Immune Defic Syndr 2016;72:177)
Sites
- PEL involves pleural, pericardial or peritoneal cavities
- Lymph nodes and extranodal sites are involved in extracavitary primary effusion lymphoma (EC PEL)
Pathophysiology
- HHV8 / KSHV has a basic pathogenic mechanism for developing PEL and has double stranded DNA
- Following latent gene products of HHV8 / KSHV are postulated to play a significant role in lymphomagenesis (Intractable Rare Dis Res 2014;3:65, Science 1999;284:641, Nat Med 2000;6:1121, Nature 1997;386:517, Mol Cell 2001;7:833)
- LANA1
- LANA1 binds the HHV8 / KSHV episome to the nuclear chromosome and replicates HHV8 / KSHV DNA at mitosis, leading to its distribution to daughter cells
- C terminus of LANA1 binds to TP53, resulting in the inhibition of TP53 dependent apoptosis
- Binding to retinoblastoma (RB), lead to cell proliferation through the RB / E2F pathway
- LANA2 / viral interferon regulatory factor 3 (vIRF3) induces drug resistance by binding to polymerized microtubules, decreasing their stability
- Viral homolog of cyclin D (vCyclin) binds to cyclin dependent kinase 6 (CDK6), leads to the inactivation of RB protein
- Viral homolog of FLICE inhibitory protein (vFLIP) inhibits apoptosis by blockade of caspase activation mediated by FAS and tumor necrosis factor (TNF), and also activates the NFκB pathway through activation of IκB kinase γ (IKKγ)
- Kaposin has multiple isoforms
- Kaposin A regulates oncogenesis through cytokesin 1
- Kaposin B stabilizes cytokine expressions such as interleukin 6 (IL6) and granulocyte macrophage colony stimulating factor by stabilization of cytokine mRNA containing adenylate uridylate rich elements, which are important for latent infection of HHV8 / KSHV
- LANA1
- HHV8 / KSHV infected B cells acquire the characteristics of malignancy, such as immune evasion, drug resistance, antiapoptosis, cell cycle progression and cytokine stabilization
- PEL tumor cells fail to express the EBV transforming protein EBV nuclear antigen 2 (EBNA2) and latent membrane protein 1, while they express EBNA1, denoted as latency type I phenotype (Blood 1997;90:1186, Leukemia 2000;14:271, J Gen Virol 1998;79:1445)
Etiology
- KSHV / HHV8 coinfection with EBV noted in 80% of cases in a background of immunosuppression
Clinical features
- Presents with serous effusions, including pleural, pericardial or peritoneal cavities
- Rarely a tumor mass related to the body cavity is noted
- Commonly associated with HIV infection in a setting of low CD4 cell count (< 0.2 x 109/L) (Am J Hematol 2016;91:233)
- EC PEL involves lymph nodes or extranodal sites, such as gastrointestinal tract, lung, skin or presents as an intravascular tumor in CNS or bone marrow (Int J Surg Pathol 2020;28:868, Clin Case Rep 2021;9:e04100)
Diagnosis
- Essential diagnostic criteria for PEL
- Lymphoma presenting as a serous effusion and involving body cavities or a tumor mass directly associated with the effusion
- Large pleomorphic cells with terminally differentiated B cell phenotype (positive for HLA-DR, CD30, EMA, CD38, VS38c, CD138, IRF4 / MUM1 and BLIMP1) (Blood 1996;88:645, Blood 2018;132:1879)
- Positive for KSHV / HHV8 (LANA by immunohistochemistry) (Onco Targets Ther 2018;11:3747, Blood 2018;132:1879, Cancers (Basel) 2021;13:878, Case Rep Hematol 2019;2019:4536157)
- Essential diagnostic criteria for EC PEL
- Lymphoma involving nodal or extranodal sites without effusion
- Large pleomorphic cells with terminally differentiated B cell phenotype (positive for HLA-DR, CD30, EMA, CD38, VS38c, CD138, IRF4 / MUM1 and BLIMP1) (Oncologist 2007;12:569, Blood 2018;132:1879, Cancers (Basel) 2021;13:878)
- Positive for KSHV / HHV8 (LANA by immunohistochemistry)
- Desirable criteria for both entities
- Presence of EBV (Cancers (Basel) 2021;13:878)
Radiology description
- Chest Xray, CT scans of chest and abdomen show unilateral or bilateral pleural effusions or ascites
- There may be slight thickening of the parietal pleura or pericardium
- Parenchymal masses or lymphadenopathy are not usually present in PEL
Prognostic factors
- PEL / EC PEL prognosis is poor and median survival even with treatment remains < 24 months (Blood 2019;133:1753)
- Prognosis is worsened by performance status, concurrent untreated HIV and the involvement of the pericardial cavity as opposed to the pleural or peritoneal cavities
- Poor outcome has been suggested with multiple cavity involvement versus single cavity (Onco Targets Ther 2018;11:3747, Leuk Lymphoma 2012;53:2378, J Clin Oncol 2005;23:4372)
- Presence of EBV positivity in PEL is associated with improved survival while elevated IL6 is associated with inferior survival (Blood 2019;133:1753)
Case reports
- 41 year old man with back pain and lower extremity weakness (Ann Diagn Pathol 2023;63:152084)
- 47 year old man who presented with an asymptomatic plaque (Cutis 2023;111:E39)
- 60 year old HIV negative woman who presented with fever and dyspnea (J Med Case Rep 2019;13:301)
- 84 year old woman presented with fever, dyspnea and dry cough (Clin Case Rep 2021;9:2305)
Treatment
- Common treatment regimens include dose adjusted (DA) EPOCH (etoposide, prednisone, vincristine, cyclophosphamide and doxorubicin) or traditional chemotherapy with CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone) (Blood 1989;73:792, J Clin Oncol 2005;23:4372)
- Rituximab has been used for CD20+ PEL but due to reduced expression of this marker on the surface of PEL cells, it is not a significant therapeutic regimen
- High dose methotrexate (HD MTX) addition to the CHOP regimen has shown a modest increase in median overall survival (OS) from 6 to 10 months (Blood 2018;132:1879)
- Patients with concurrent AIDS should be treated with full dose chemotherapy regimens and concurrent antiretroviral therapy (ART) (Leuk Lymphoma 2018;59:1851)
- Talc pleurodesis has been assessed as a palliative modality in elderly and poor functional status individuals who cannot tolerate aggressive therapies
- The National Comprehensive Cancer Network (NCCN) B cell Lymphoma Guidelines (Version 3.2021) include axicabtagene ciloleucel (axi-cel) as a category 2A recommendation for the treatment of relapsed / refractory PEL (NCCN: NCCN Guidelines - B-Cell Lymphomas [Accessed 2 August 2024])
- In a small cohort, the immune checkpoint inhibitor pembrolizumab (in combination with pomalidomide) showed an improvement in overall survival when used to treat patients living with HIV (PLWH) who have relapsed / refractory disease (J Immunother Cancer 2021;9:e002097)
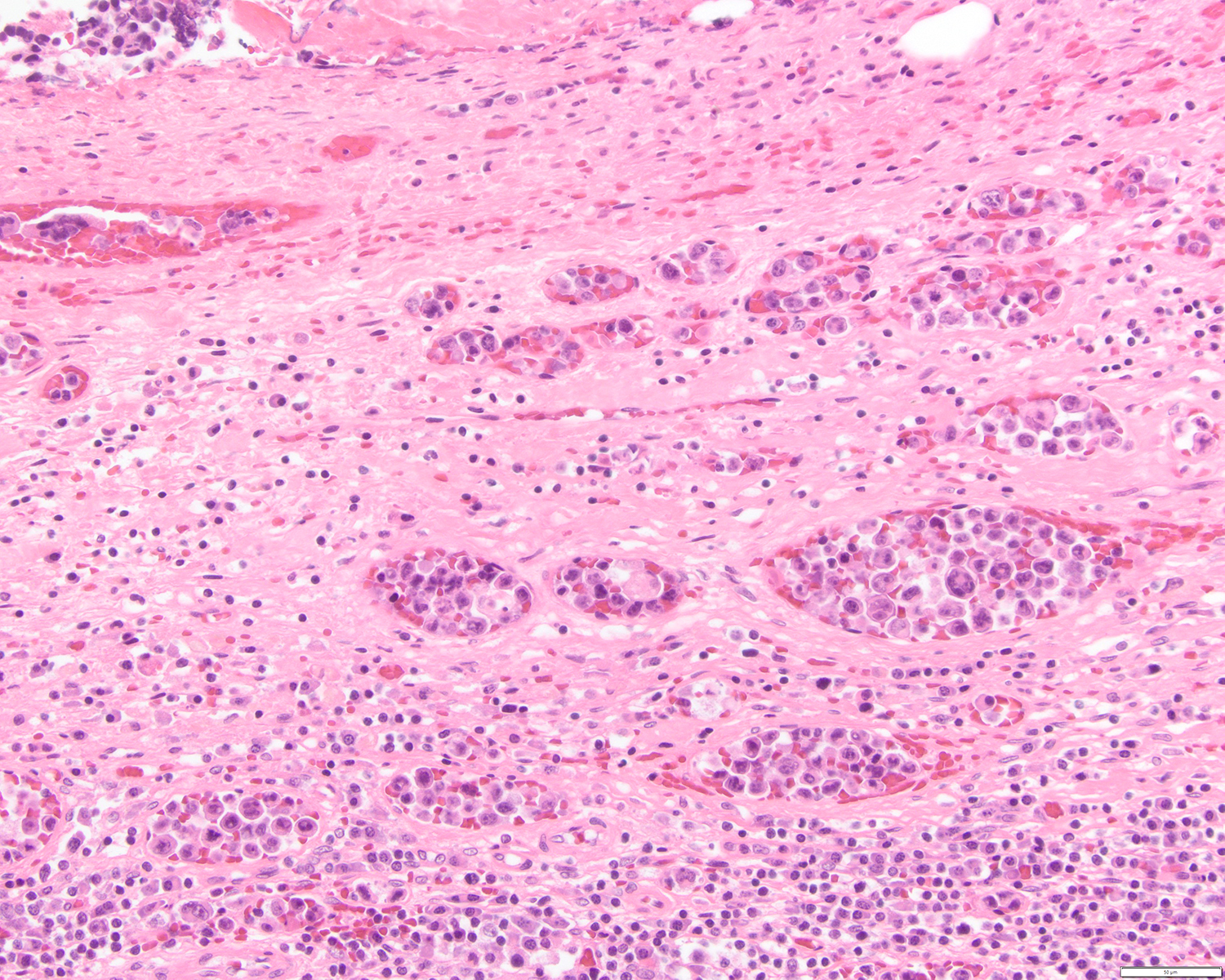
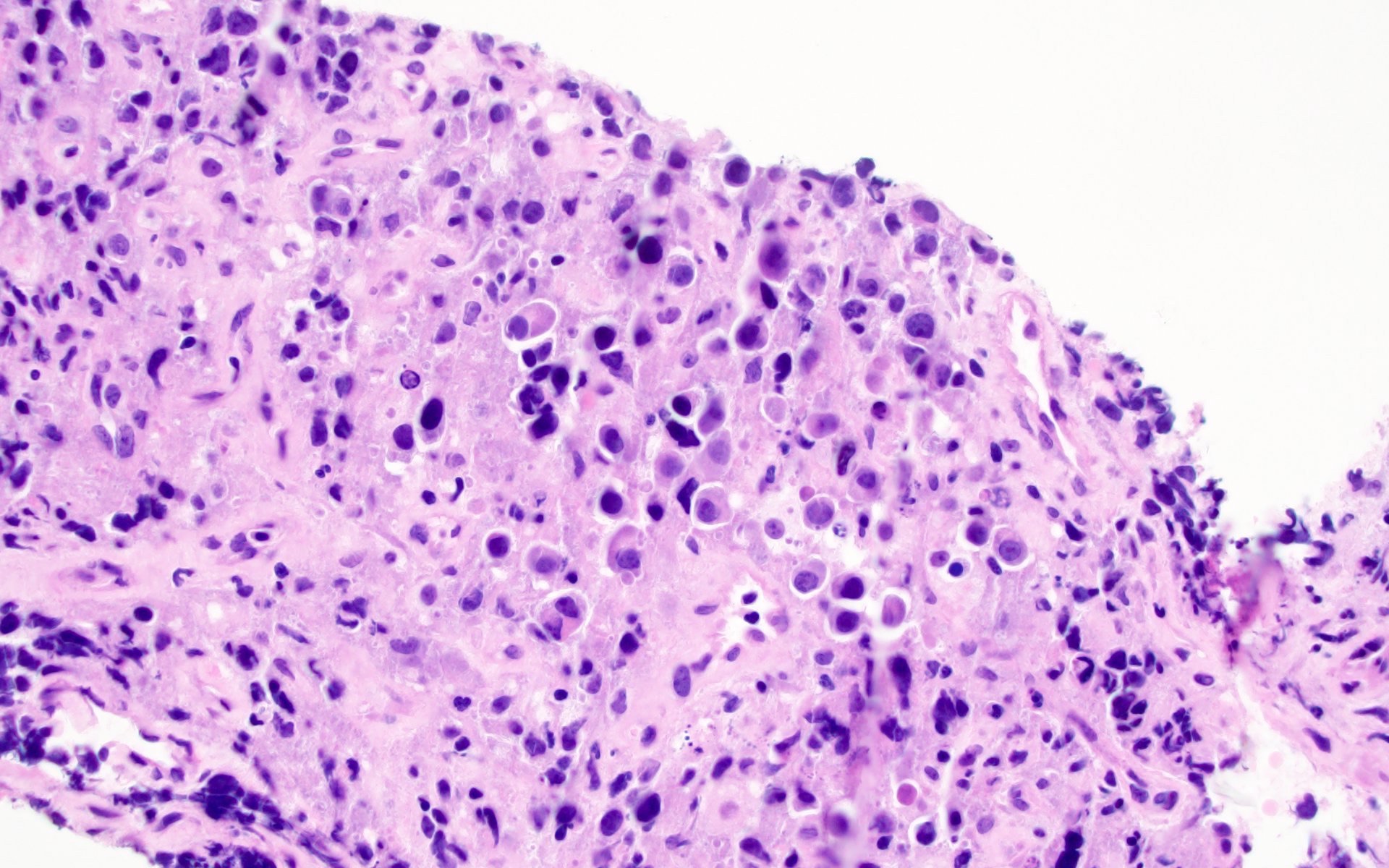
Microscopic (histologic) description
- Large pleomorphic cells with irregular nuclear contours, condensed chromatin, prominent nucleoli and abundant cytoplasm (Diagn Cytopathol 2006;34:335, Cancer 2007;111:224)
- Some of the cells may have cytoplasmic vacuoles or multinucleation
- In nodal and extranodal location, effacement of the architecture
Microscopic (histologic) images
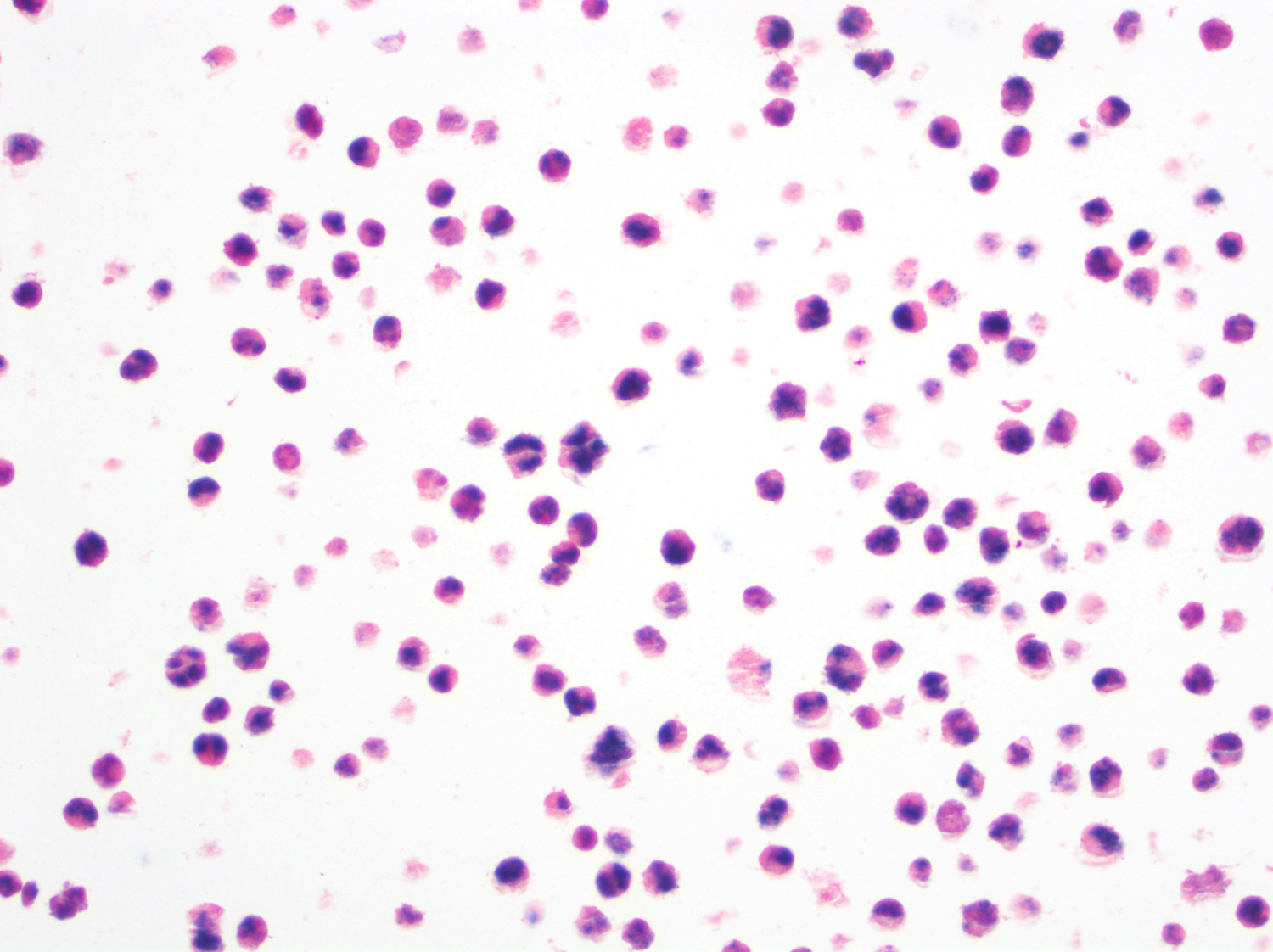
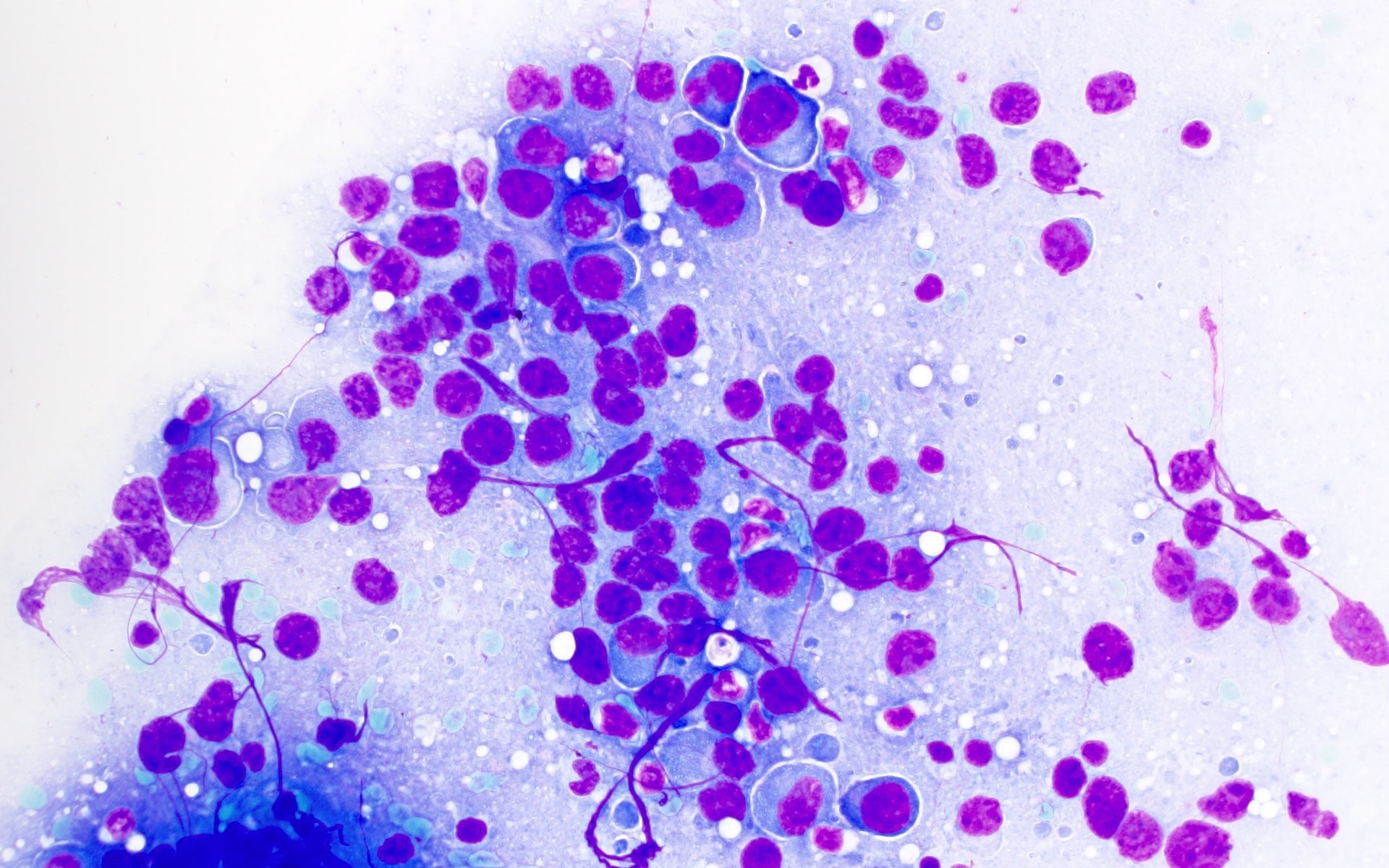
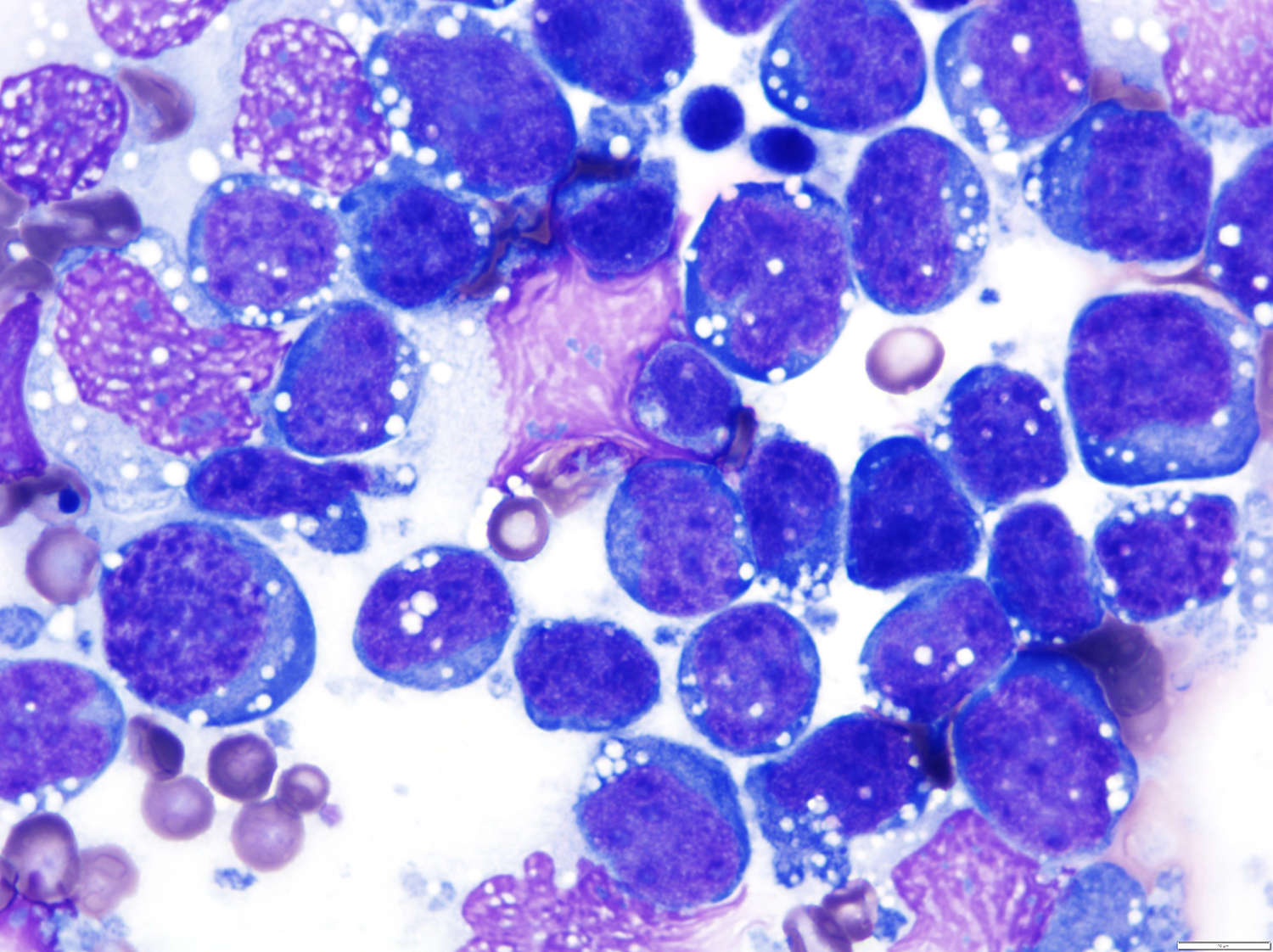
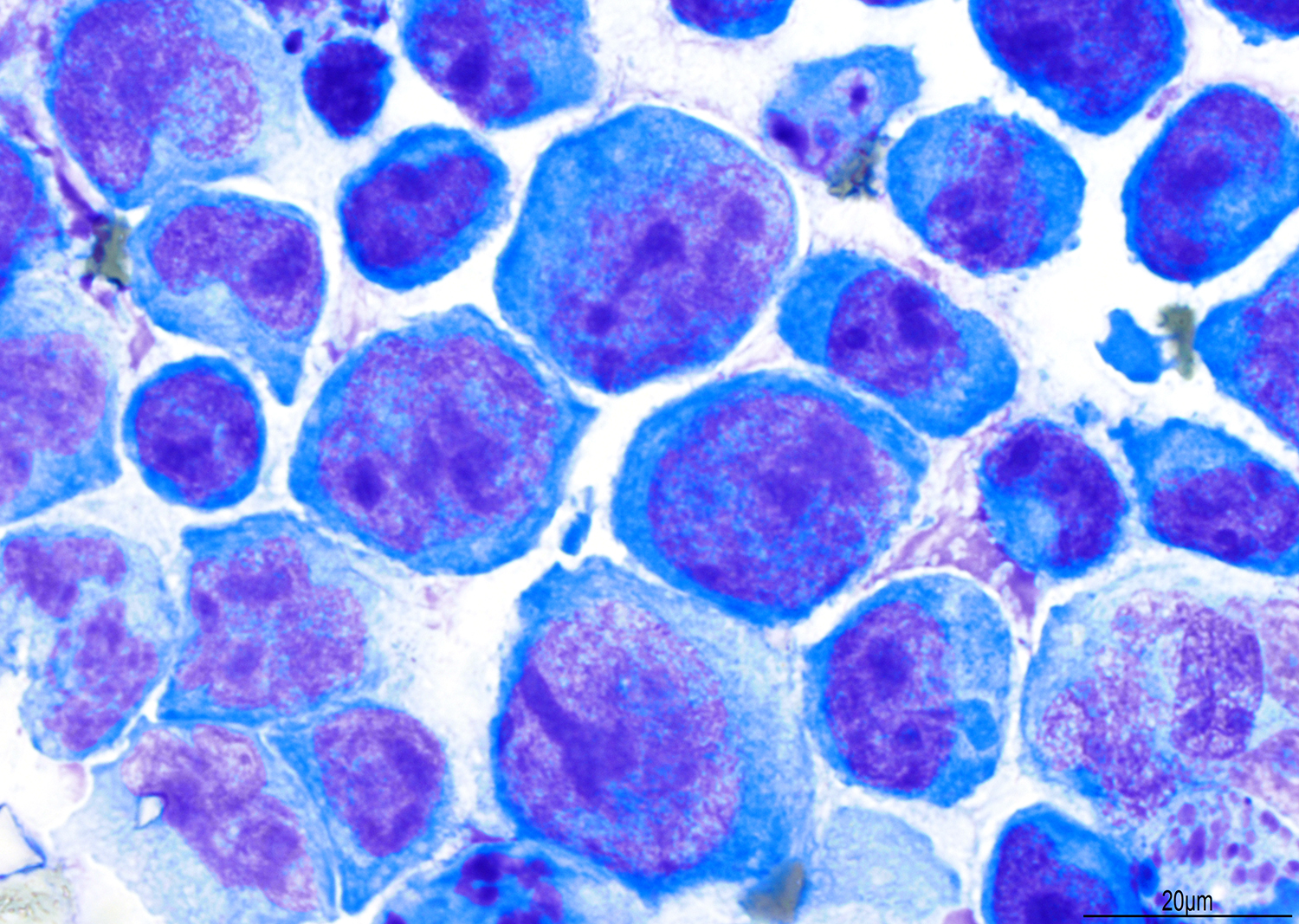
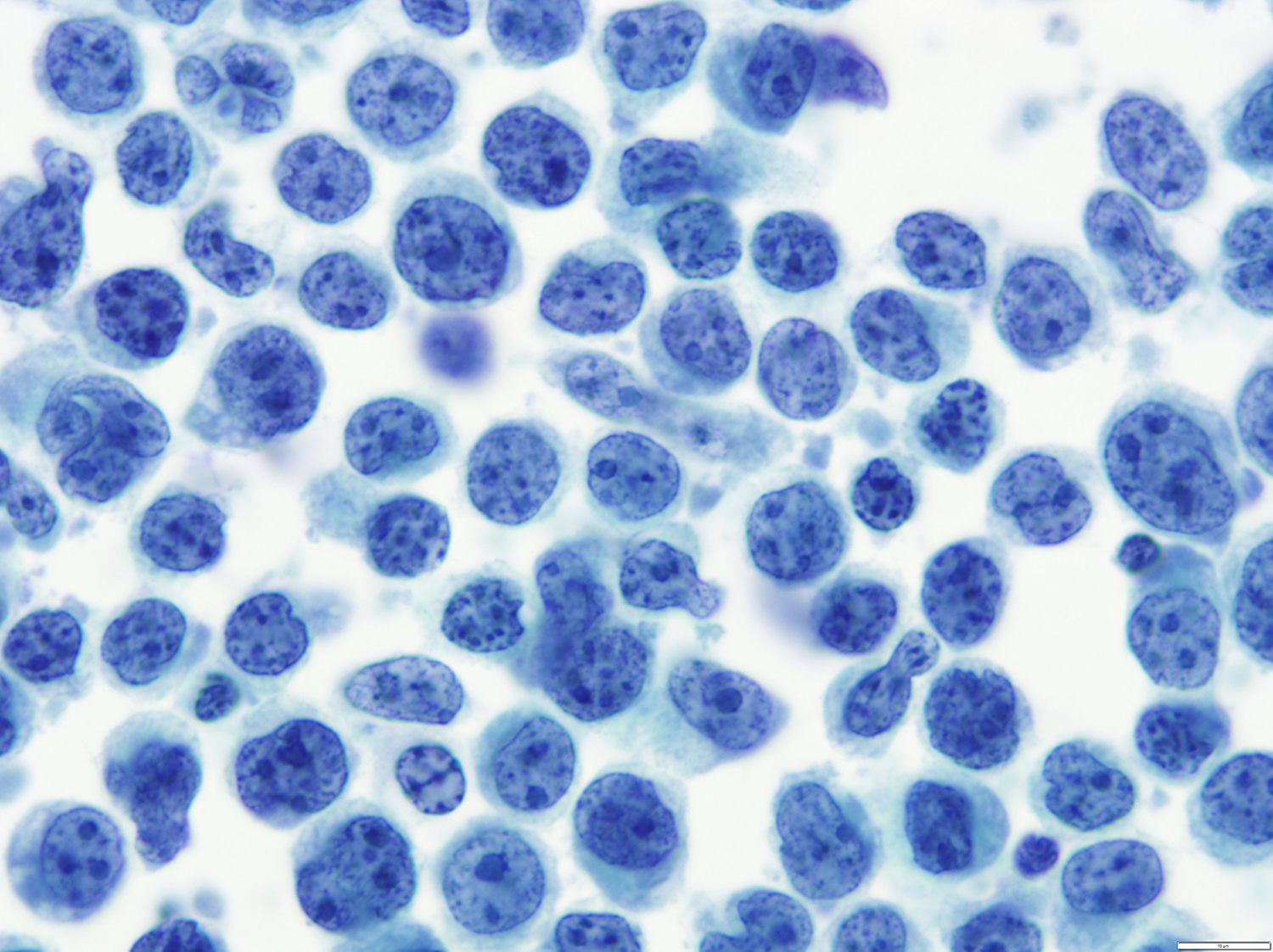
Cytology description
- Large pleomorphic cells with irregular nuclear contours, condensed chromatin, prominent nucleoli and abundant cytoplasm (Diagn Cytopathol 2006;34:335, Cancer 2007;111:224)
- Some of the cells may have cytoplasmic vacuoles or multinucleation
Cytology images
Contributed by Barina Aqil, M.D., Mario L. Marques-Piubelli, M.D. and Roberto N. Miranda, M.D. (Case #519)
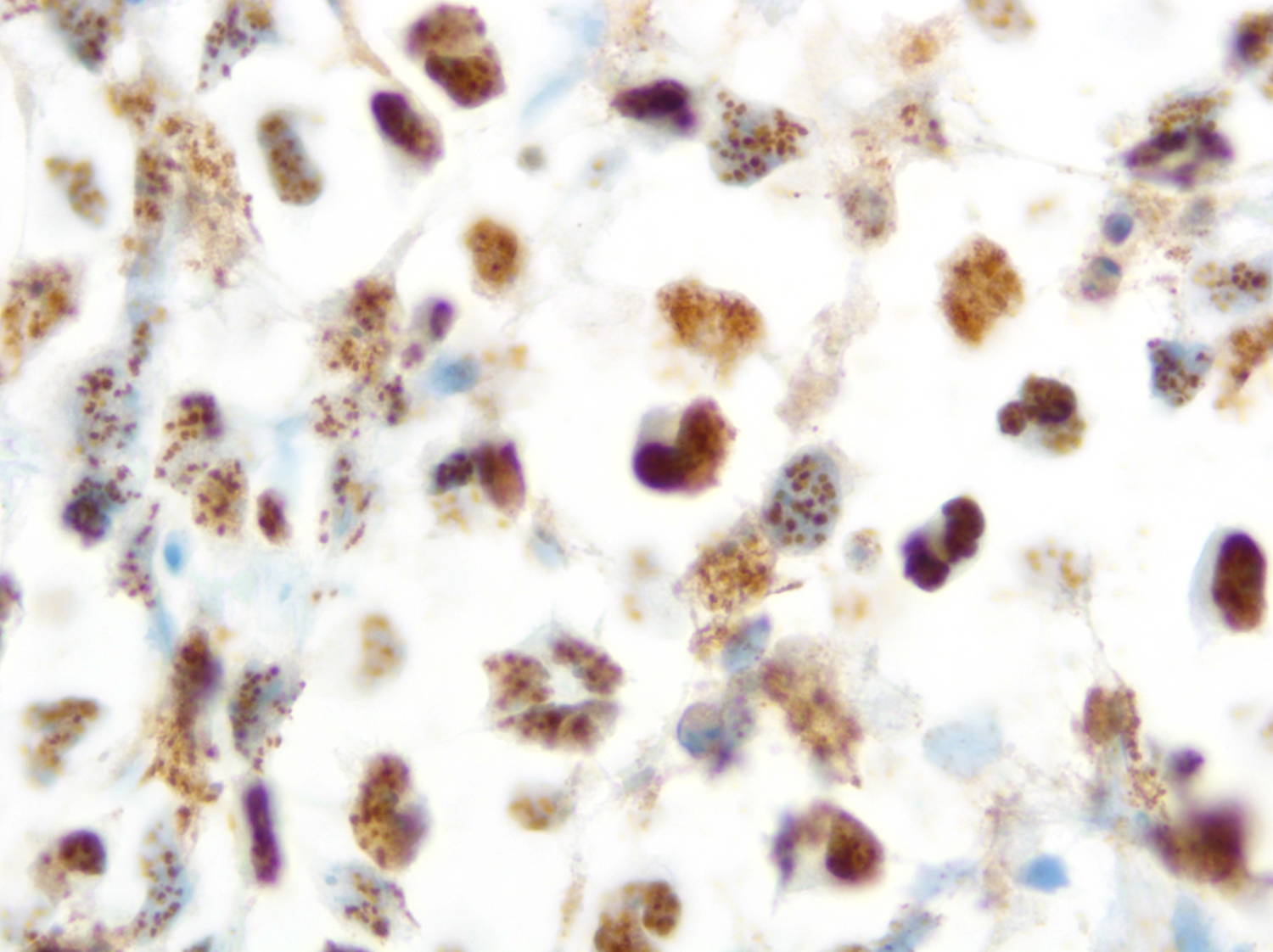
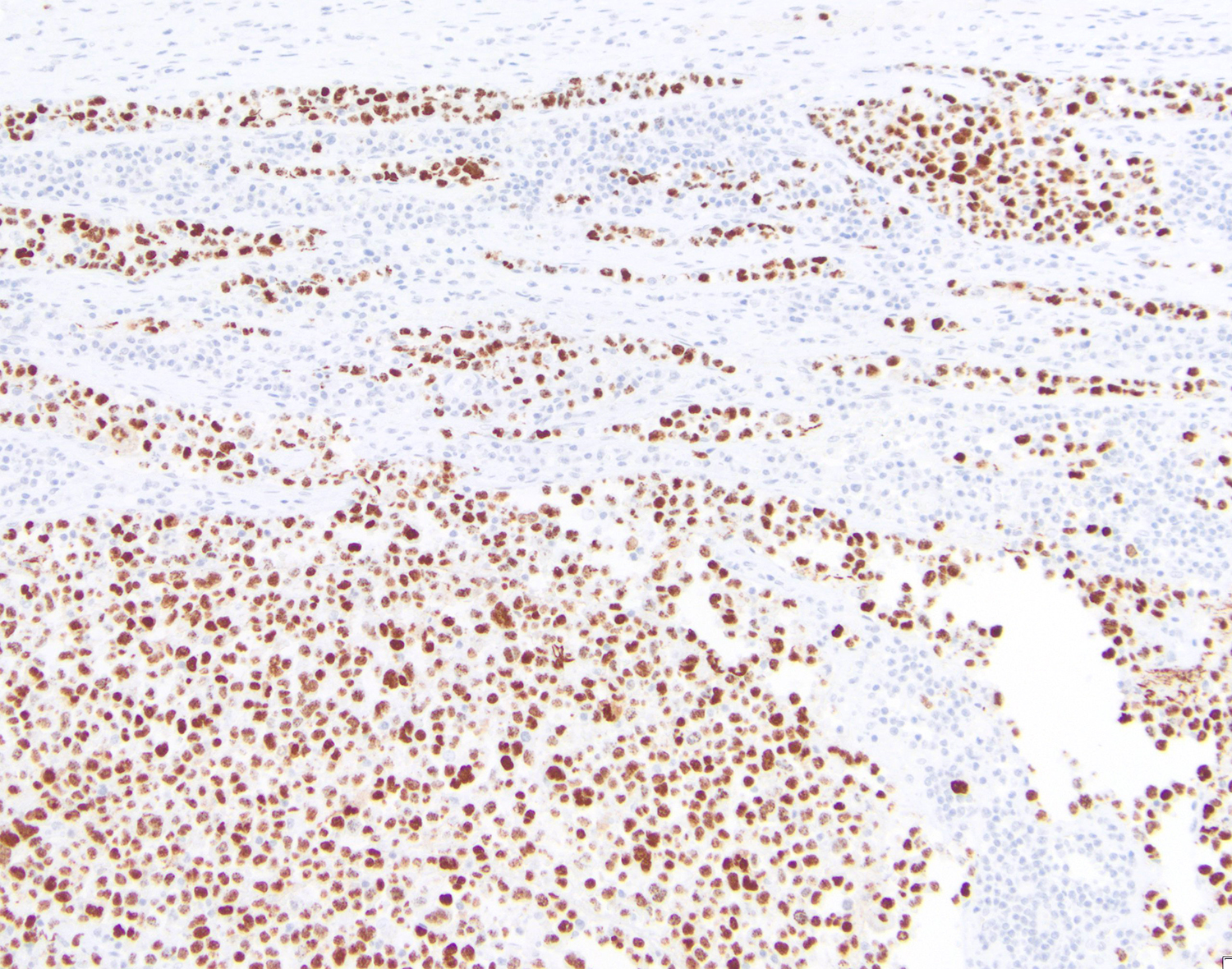
Positive stains
- PEL
- HLA-DR, CD30, EMA, CD38, VS38c, CD138, IRF4 (MUM1) and BLIMP1
- Aberrant T cell antigens can be demonstrated (CD3, CD2, CD5, CD7) (Arch Pathol Lab Med 1999;123:257, Am J Hematol 2004;76:88, Am J Hematol 2016;91:233)
- KSHV / HHV8 / LANA
- PEL cases in HIV patients are positive for EBV encoded small RNA (EBER)
- EC PEL
- May express some of the B cell antigens (CD20, CD22) or immunoglobulin light chain (lambda) (Am J Surg Pathol 2004;28:1401)
Negative stains
Flow cytometry description
Molecular / cytogenetics description
- Clonally rearranged and hypermutated immunoglobulin genes (Oncologist 2007;12:569)
- PCR positive for KSHV / HHV8 and EBV (Am J Surg Pathol 2004;28:1401)
- Overexpression of cellular proteins, including cyclin D2, cFLIP and MCL1 (Nat Commun 2018;9:3263)
- Trisomy 7, trisomy 12 and alterations in the proximal long arm of chromosome 1 (1q) (Br J Haematol 2002;116:113)
Sample pathology report
- Pleural cavity, effusion, cytology and cell block:
- Primary effusion lymphoma, positive for human herpes virus 8 (see comment)
- Comment:
- Cytology: The cytospin preparation showed at atypical large pleomorphic cells with irregular / multinucleated with prominent nucleoli and abundant basophilic cytoplasm.
- Cell block: Shows clusters and sheets of large pleomorphic cells that are positive for CD138, MUM1, LANA (HHV8), EBER and negative for CD19, CD20, PAX5, OCT2, BOB1 and CD79a.
- Flow cytometry identified an abnormal plasmacytoid cell population, that is dim CD45+, CD138+, CD38+, CD19-, CD20-, CD22-, CD23-, CD5-, CD10-, CD52+ and negative for surface and cytoplasmic immunoglobulin light chains.
Differential diagnosis
Differential diagnosis of PEL
| Primary effusion lymphoma | Fluid overload associated large B cell lymphoma | Diffuse large B cell lymphoma associated with chronic inflammation | Plasmablastic lymphoma | Diffuse large B cell lymphoma | |
| HIV | +++/- | ---/+ | - | ++/-- | ---/+ |
| Associations | Organ transplant; immune senescence (elderly) | Fluid overload, in chronic heart failure, renal insufficiency, protein losing enteropathy or liver failure / cirrhosis | Longstanding chronic inflammation | Immunodeficiency (organ transplant, elderly) | Primary / acquired immunodeficiency |
| Clinical presentation | Pleural, peritoneal or pericardial effusion | Pleural, peritoneal or pericardial effusion | Chest and back pain; fever; and respiratory symptoms | Nodal, extranodal disease, B symptoms | Nodal, extranodal disease, B symptoms |
| Location | Body cavities | Body cavities | Pleural cavity, bone (especially the femur), joints and periarticular soft tissue | Extranodal and nodal | Extranodal and nodal |
| Morphology | Large pleomorphic cells (immunoblastic, plasmablastic or anaplastic morphology) | Large pleomorphic cells (immunoblastic, plasmablastic or anaplastic morphology) | Large centroblastic or immunoblastic cells | Large plasmablastic morphology | Large centroblastic, immunoblastic or anaplastic morphology |
| EBV positivity | 70% | 13 - 30% | 70% | 60 - 75% | 9 - 15% |
| HHV8 | + | - | - | - | - |
| Phenotype |
CD45-/+ CD20- CD19- CD79a- PAX5- MUM1+ CD38+/- CD138+/- CD30+/- Ig light chain-/+ |
CD45+/- CD20+/- CD19+/- CD79a+/- PAX5+/- MUM1+/- CD38-/+ CD138-/+ CD30-/+ Ig light chain-/+ |
CD45+ CD20+/- CD19+ CD79a+/- PAX5+ MUM1+ CD38-/+ CD30+/- Ig light chain+/- |
CD45-/+ CD20- CD19- CD79a-/+ PAX5- MUM1+ CD38+ CD138+ CD30-/+ Ig light chain+ |
CD45+ CD20+ CD19+ CD79a+ PAX5+ IRF4 / MUM1+/- CD38-/+ CD138-/+ CD30-/+ |
| B cell origin | Post-germinal center | Post-germinal center | Post-germinal center | Post-germinal center | Germinal center or post-germinal center |
| Prognosis | Median survival < 2 years | 2 year survival 85% | 5 year survival 20 - 35% | Median survival < 1 year | Variable 5 year survival > 60% |
- Fibrin associated large B cell lymphoma:
- Associated with EBV but not with HHV8
- Carries an excellent prognosis
- Associated with previous cavities or around textured breast implants (Mod Pathol 2021;34:2154)
Differential diagnosis of EC PEL
- Germinotropic lymphoproliferative disorder:
- KSHV / HHV8+ and EBV- large B cells colonizing the germinal centers
- Seen in immunocompetent elderly patients
- Presents with lymphadenopathy without B symptoms
- Localized clusters / sheets of large cells showing partial or complete effacement of germinal centers
- Cells positive for LANA and EBER
- Most of the cells are CD138-, CD30-, MUM1+ and immunoglobulin can be positive or negative
- KSHV / HHV8 positive diffuse large B cell lymphoma:
- Disorders associated with KSHV / HHV8:
- Kaposi sarcoma (KS)
- Primary effusion lymphoma (PEL)
- KSHV associated multicentric Castleman disease (MCD)
- KSHV inflammatory cytokine syndrome (KICS)
Additional references
Board review style question #1
A 57 year old HIV+ man presented with chest pain and dyspnea. Chest computed tomography (CT) showed pleural effusion. Which of the following KSHV / HHV8 diseases may be associated at the time of presentation in this patient?
- AESOP (adenopathy and extensive skin patch overlying plasmacytoma) syndrome
- Multicentric Castleman disease
- POEMS (polyneuropathy, organomegaly, endocrinopathy, M protein and skin changes) syndrome
- TEMPI (telangiectases, elevated erythropoietin and erythrocytosis, monoclonal gammopathy, perinephric fluid collection and intrapulmonary shunting) syndrome
Board review style answer #1
B. Multicentric Castleman disease and Kaposi sarcoma are present in ~50% of patients at the time of presentation.
Answers A, C and D are incorrect because POEMS syndrome, TEMPI syndrome and AESOP syndrome are paraneoplastic syndromes associated with plasma cell neoplasms and have no association with KSHV / HHV8 disease.
Comment Here
Reference: Primary effusion lymphoma
Comment Here
Reference: Primary effusion lymphoma