Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Singh AP, Gru AA. EBV+ mucocutaneous ulcer. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaebvmucocutulcer.html. Accessed March 30th, 2025.
Definition / general
- Indolent and rare mature B cell neoplasm associated with age related or iatrogenic immunosuppression
- Almost all Epstein-Barr virus positive mucocutaneous ulcer (EBVMCU) patients achieve remission with the reduction or discontinuation of immunosuppressants
Essential features
- Indolent and rare mature B cell neoplasm
- Shallow, sharply circumscribed, unifocal mucosal or cutaneous ulcer
- Associated with various forms of immunosuppression (including immune senescence) and often spontaneous regression
- Proliferation of EBV+, variable sized, atypical CD30+ B cells
ICD coding
- ICD-O: 9680/1 - EBV+ mucocutaneous ulcer
Epidemiology
- Elderly, patients on immunosuppressive drugs, HIV infected patients, solid organ transplant recipients (J Clin Exp Hematop 2019;59:64)
- Mild female predominance (J Clin Exp Hematop 2019;59:64)
- Median age > 60 (J Clin Exp Hematop 2019;59:64, Int J Mol Sci 2021;22:1053, Am J Surg Pathol 2010;34:405)
Sites
- Oral mucosa > skin > gastrointestinal tract (Int J Mol Sci 2021;22:1053)
- Regional isolated lymphadenopathy is rarely seen (Semin Diagn Pathol 2017;34:60)
- No systemic lymphadenopathy, hepatosplenomegaly or bone marrow involvement (Semin Diagn Pathol 2017;34:60)
Etiology
- Iatrogenic or age associated immunosuppression
Diagrams / tables
Clinical features
- Unifocal, sharply circumscribed ulcer involving the cutaneous / mucosal surfaces (J Clin Exp Hematop 2019;59:64, Int J Mol Sci 2021;22:1053)
Diagnosis
- Biopsy
Prognostic factors
- Good prognosis, with spontaneous resolution in > 90% of the patients after removing the cause of immunosuppression (Int J Mol Sci 2021;22:1053)
- < 3% of people can develop progressive disease (Int J Mol Sci 2021;22:1053)
Case reports
- 54 year old woman, a renal transplant recipient with EBVMCU (S D Med 2018;71:252)
- 59 year old woman with rheumatoid arthritis on methotrexate presented with a cheek ulcer (Indian J Pathol Microbiol 2018;61:255)
- 75 year old woman with inactive Crohn's disease presented with a 2 month history of necrotic ulcerative lesions of the palate (ACG Case Rep J 2018;5:e32)
- 81 year old woman with a painful oral ulcer (Clin Case Rep 2015;3:531)
Treatment
- Resolution of immunosuppression
- Systemic chemotherapy is often unnecessary in patients with EBVMCU (Int J Mol Sci 2021;22:1053)
- 100% 1 year treatment free survival (J Clin Exp Hematop 2020;60:159)
Microscopic (histologic) description
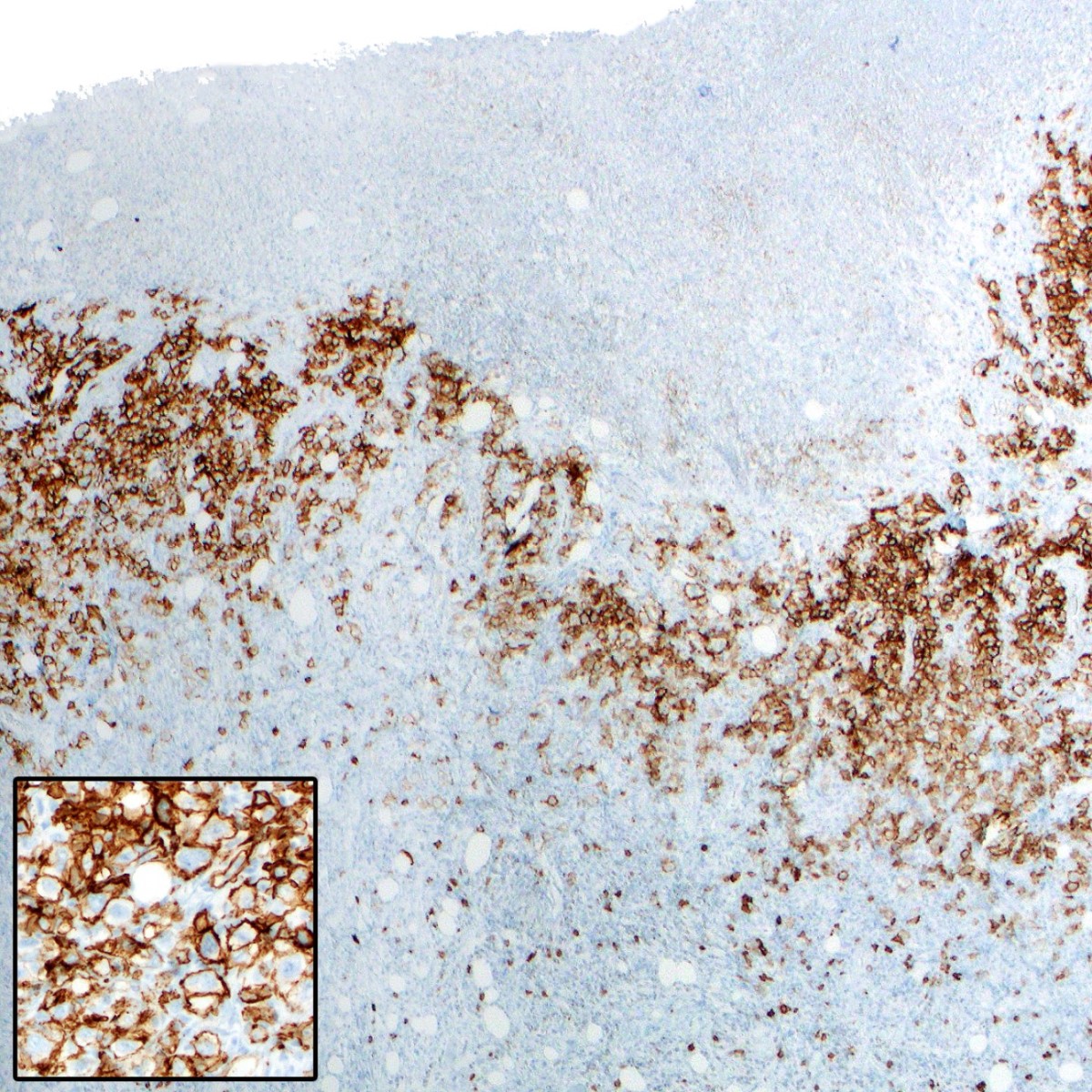
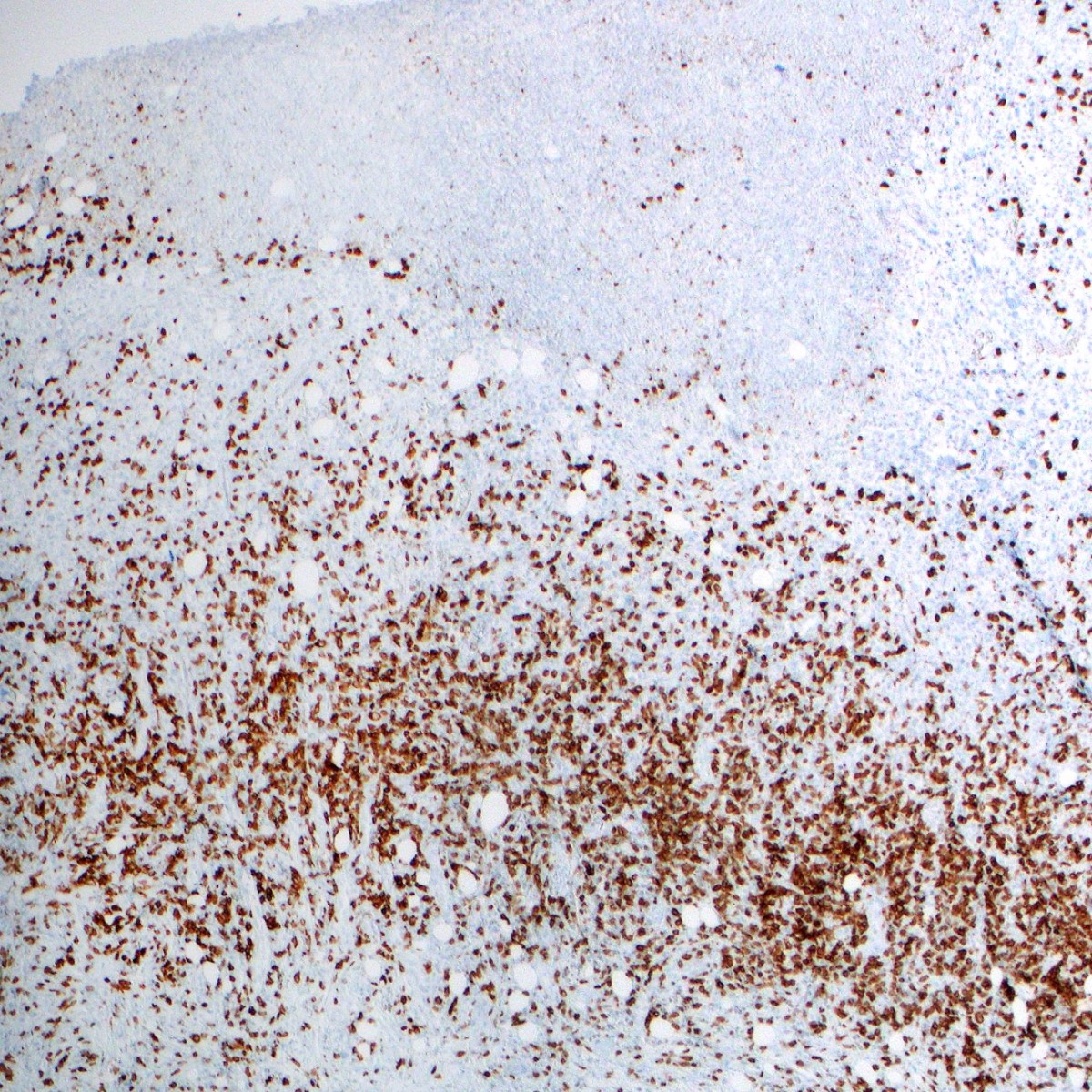
- Shallow, mucosal or cutaneous ulcers with adjacent acanthosis of the epidermis or mucosa and sometimes pseudoepitheliomatous changes (Semin Diagn Pathol 2017;34:60)
- Variable angiotropism
- Polymorphic infiltration with various inflammatory cells such as plasma cells, histiocytes and granulocytes
- Atypical cells (EBV+) range in size from small to large and may resemble classic Hodgkin Reed-Sternberg (HRS) cells
- A rim of small T lymphocytes at the base of the lesions is usually noted
Microscopic (histologic) images
Positive stains
Negative stains
- Large cells negative for CD3, CD56, TIA, granzyme B
Sample pathology report
- Tongue, left base, biopsy:
- Atypical B cell lymphoproliferative process, EBV+ (see comment)
- Comment: Examination of hematoxylin and eosin stained slides reveals stratified nonkeratinized squamous epithelium accompanied by a submucosal infiltrate dominated by small lymphocytes and plasma cells. The epithelium displays focal ulceration, while the infiltrate showcases a focal area of abundant apoptotic debris that includes frequent scattered large atypical immunoblastic cells. These large cells exhibit nucleomegaly with prominent nucleoli and multinucleation.
- Immunohistochemical stains are performed, revealing that CD20 and PAX5 highlight small B cells in nodules as well as the scattered large atypical cells. Similarly, CD79a demonstrates a comparable pattern in the small B cells. CD3 highlights an abundance of small T cells in the background, with CD4 and CD8 immunostains indicating that most of the T cells are CD4+. BCL6 is negative and BCL2 is positive in B and T cell areas. CD56 highlights rare scattered small cells, while CD30 is positive in the large atypical cells and CD15 highlights scattered granulocytes. The c-myc immunostain is negative but CD138 highlights the abundant plasma cells. In situ hybridization studies of kappa and lambda light chains demonstrate polytypic light chain expression. MUM1 highlights the plasma cells and in situ hybridization for EBV (EBER) is positive in the large atypical cells.
- In summary, examination of the patient's tissue reveals ulcerated squamous mucosa with an atypical submucosal lymphoplasmacytic infiltrate consisting of aggregates of B cells and scattered large atypical lymphocytes that test positive for EBER, CD30 and CD20. The immunomorphologic observations of the infiltrate are indicative of EBV mucocutaneous ulcer and clinical correlation is necessary.
Differential diagnosis
- EBV+ DLBCL (Pathogens 2018;7:28):
- Classical Hodgkin lymphoma (Pathogens 2018;7:28):
- Extranodal NK / T cell lymphoma (Curr Hematol Malig Rep 2016;11:514):
- Lymphomatoid granulomatosis (Am J Surg Pathol 2010;34:e35):
- Angiocentric, angiodestructive lesion composed of B cells, CD30+
- Pulmonary nodules, skin lesions, B symptoms
- EBV+ polymorphic lymphoproliferative disorder:
- Often linked to immunosuppression, such as posttransplant
- Systemic symptoms like fever, weight loss and lymphadenopathy
- Involves multiple anatomical locations, mainly lymph nodes, spleen and liver
- Heterogeneous lymphoid population, including B cells, T cells and plasma cells
- Reed-Sternberg-like cells may be present but are not definitive
- Immunophenotype similar to EBVMCU; B cells often express EBV latent membrane proteins (EBER, LMP1, EBNA2) in a range of cell sizes
- Monoclonal or oligoclonal IG rearrangements
Board review style question #1
A 34 year old woman presents with a painful ulcer on her upper lip (as shown in the image above). The lesion has been present for ~4 weeks and has not responded to topical treatments. The lesion is about 1.5 cm in diameter, has a raised border and a yellowish base. She reports no history of trauma to the area but reports a recent onset of fatigue and malaise. The patient has a history of Hodgkin lymphoma, which was treated with chemotherapy and radiation therapy 2 years ago. A biopsy of the lesion shows diffuse infiltration of large atypical lymphoid cells, positive for CD20, CD30, PAX5 and Epstein-Barr virus (EBV) and negative for CD15 and CD56. There is a mixed inflammatory infiltrate, including lymphocytes and plasma cells. What is the most likely diagnosis?
- Classic Hodgkin lymphoma
- EBV+ mucocutaneous ulcer
- Extranodal NK / T cell lymphoma
- Lymphocyte predominant Hodgkin lymphoma
- Posttransplant associated lymphoproliferative disorder (PTLD)
Board review style answer #1
B. EBV+ mucocutaneous ulcer. EBV+ mucocutaneous ulcer (EBVMCU) is the most likely diagnosis for this patient due to the presence of a localized ulcer on her upper lip and the histological findings of a polymorphous infiltrate with large atypical cells, positive for CD20 and CD30 and negative for CD15, which align with the typical profile of EBVMCU. Additionally, the presence of Epstein-Barr virus (EBV) in the atypical cells, as well as the patient's history of immunosuppression following treatment for Hodgkin lymphoma, further support the diagnosis. EBVMCU is a self limited, often recurring disease that usually occurs in the setting of immune dysregulation or immunosuppression, fitting well with the patient's clinical context.
Answer A is incorrect because the clinical presentation and the immunophenotypic profile of the cells are not typical for classic Hodgkin lymphoma (CHL). CHL usually presents as lymphadenopathy rather than a mucocutaneous ulcer. Furthermore, CHL is characterized by the presence of Reed-Sternberg cells, which are typically CD30 positive, CD15 positive and CD20 negative, in contrast to the cells in this case, which are CD15 negative and CD20 positive.
Answer C is incorrect because extranodal NK / T cell lymphoma is typically associated with Epstein-Barr virus (EBV) infection but the neoplastic cells are typically T cells or NK cells, not B cells. The cells in this case are positive for CD20, a B cell marker, which makes NK / T cell lymphoma unlikely. Additionally, extranodal NK/T cell lymphoma frequently involves sites such as the nasal cavity, whereas this lesion is on the lip.
Answer D is incorrect because lymphocyte predominant Hodgkin lymphoma (LPHL) is characterized by the presence of LP cells, which are variants of Reed-Sternberg cells. LP cells typically express CD20 but not CD30. This case presents cells that are both CD20 and CD30 positive, which is not characteristic of LPHL. Furthermore, LPHL typically presents as lymphadenopathy, not as a mucocutaneous ulcer.
Answer E is incorrect because despite the patient's history of immunosuppression, the findings do not match those of a posttransplant lymphoproliferative disorder (PTLD). Polymorphic LPDs can appear in multiple settings of immune deficiency, not just posttransplant. They usually manifest as mass forming lesions composed of heterogeneous infiltrate of cells, including those similar to Hodgkin / Reed-Sternberg cells. While they share some immunophenotypic similarities with EBV+ mucocutaneous ulcers, polymorphic LPDs more often show monoclonal or oligoclonal IG rearrangements and have a broader range of potential sites of involvement, more commonly lymph nodes and various organs. The solitary painful lip ulcer in this case is more consistent with an EBV+ mucocutaneous ulcer.
Comment Here
Reference: EBV+ mucocutaneous ulcer
Answer A is incorrect because the clinical presentation and the immunophenotypic profile of the cells are not typical for classic Hodgkin lymphoma (CHL). CHL usually presents as lymphadenopathy rather than a mucocutaneous ulcer. Furthermore, CHL is characterized by the presence of Reed-Sternberg cells, which are typically CD30 positive, CD15 positive and CD20 negative, in contrast to the cells in this case, which are CD15 negative and CD20 positive.
Answer C is incorrect because extranodal NK / T cell lymphoma is typically associated with Epstein-Barr virus (EBV) infection but the neoplastic cells are typically T cells or NK cells, not B cells. The cells in this case are positive for CD20, a B cell marker, which makes NK / T cell lymphoma unlikely. Additionally, extranodal NK/T cell lymphoma frequently involves sites such as the nasal cavity, whereas this lesion is on the lip.
Answer D is incorrect because lymphocyte predominant Hodgkin lymphoma (LPHL) is characterized by the presence of LP cells, which are variants of Reed-Sternberg cells. LP cells typically express CD20 but not CD30. This case presents cells that are both CD20 and CD30 positive, which is not characteristic of LPHL. Furthermore, LPHL typically presents as lymphadenopathy, not as a mucocutaneous ulcer.
Answer E is incorrect because despite the patient's history of immunosuppression, the findings do not match those of a posttransplant lymphoproliferative disorder (PTLD). Polymorphic LPDs can appear in multiple settings of immune deficiency, not just posttransplant. They usually manifest as mass forming lesions composed of heterogeneous infiltrate of cells, including those similar to Hodgkin / Reed-Sternberg cells. While they share some immunophenotypic similarities with EBV+ mucocutaneous ulcers, polymorphic LPDs more often show monoclonal or oligoclonal IG rearrangements and have a broader range of potential sites of involvement, more commonly lymph nodes and various organs. The solitary painful lip ulcer in this case is more consistent with an EBV+ mucocutaneous ulcer.
Comment Here
Reference: EBV+ mucocutaneous ulcer