Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Saksena A, Jaffe ES. HHV8 positive DLBCL, NOS. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphomaHHV8DLBCL.html. Accessed April 3rd, 2025.
Definition / general
- HHV8 related diffuse large B cell lymphoma (DLBCL) is a neoplasm characterized by a monoclonal proliferation of HHV8 infected lymphoid cells that resemble plasmablasts and express IgM lambda
- Neoplastic cell corresponds to a naïve IgM producing B cell without immunoglobulin somatic hypermutations
Essential features
- Usually arises in association with multicentric Castleman disease (MCD) and HIV infection
- Morphologically similar to plasmablasts but correspond to naïve IgM producing B cell without somatic hypermutations
- Sheets of HHV8 latency associated nuclear antigen (LANA1) positive plasmablasts efface lymph node architecture
- Atypical cells are strongly positive for cytoplasmic IgM with lambda light chain restriction and negative for EBV encoded small RNA (EBER)
Terminology
- HHV8+ large B cell lymphoma arising in multicentric Castleman disease (obsolete)
- HHV8 positive plasmablastic lymphoma (obsolete)
- HHV8+ diffuse large B cell lymphoma, not otherwise specified
ICD coding
- ICD-O: 9738/3 - large B cell lymphoma arising in HHV8 associated multicentric Castleman disease
- ICD-10:
- C83.3 - diffuse large B cell lymphoma
- C83.30 - diffuse large B cell lymphoma, unspecified site
- C83.31 - diffuse large B cell lymphoma, lymph nodes of head, face and neck
- C83.32 - diffuse large B cell lymphoma, intrathoracic lymph nodes
- C83.33 - diffuse large B cell lymphoma, intra-abdominal lymph nodes
- C83.34 - diffuse large B cell lymphoma, lymph nodes of axilla and upper limb
- C83.35 - diffuse large B cell lymphoma, lymph nodes of inguinal region and lower limb
- C83.36 - diffuse large B cell lymphoma, intrapelvic lymph nodes
- C83.37 - diffuse large B cell lymphoma, spleen
- C83.38 - diffuse large B cell lymphoma, lymph nodes of multiple sites
- C83.39 - diffuse large B cell lymphoma, extranodal and solid organ sites
- ICD-11: 2A81.Y - other specified diffuse large B cell lymphomas (large B cell lymphoma arising in HHV8 associated multicentric Castleman disease)
Epidemiology
- Rare disease with overall frequency of 0.1% (Leuk Lymphoma 2018;59:1375)
- Median age is 47 years (range 39 - 66); M:F = 3.3:1 (Pathology 2020;52:53)
- Usually arises in association with HHV8 positive multicentric Castleman disease (MCD) and HIV (15 times higher risk) (Blood 2002;99:2331)
Sites
- Characteristically involves lymph nodes or spleen
- Can disseminate to other viscera including liver, lungs and gastrointestinal tract
- Can also manifest as a leukemia with involvement of peripheral blood (Blood 2002;99:2331)
Pathophysiology
- HHV8 infects singly scattered cells that are morphologically similar to plasmablasts with abundant cytoplasmic immunoglobulin but are, in fact, naïve IgM producing B cells that lack IG somatic hypermutations and are polyclonal at the molecular level
- HHV8 positive plasmablasts form aggregates (microlymphomas), which can be polyclonal or monoclonal (Am J Clin Pathol 2017;147:171)
- HHV8 positive aggregates rarely can expand to HHV8 positive large B cell lymphoma, which is monoclonal
Etiology
- By definition, the large plasmablastic cells in all cases are positive for HHV8
- Molecular mechanism is similar to other HHV8 positive entities (Blood 2004;104:3349)
Clinical features
- Usually manifests with profound immunodeficiency, enlarging lymph nodes and massive splenomegaly
- There may be manifestations of Kaposi sarcoma (Blood 2002;99:2331)
- Rarely, may arise in absence of MCD (Mod Pathol 2017;30:745)
Diagnosis
- Biopsy of involved lymph node with immunohistochemistry
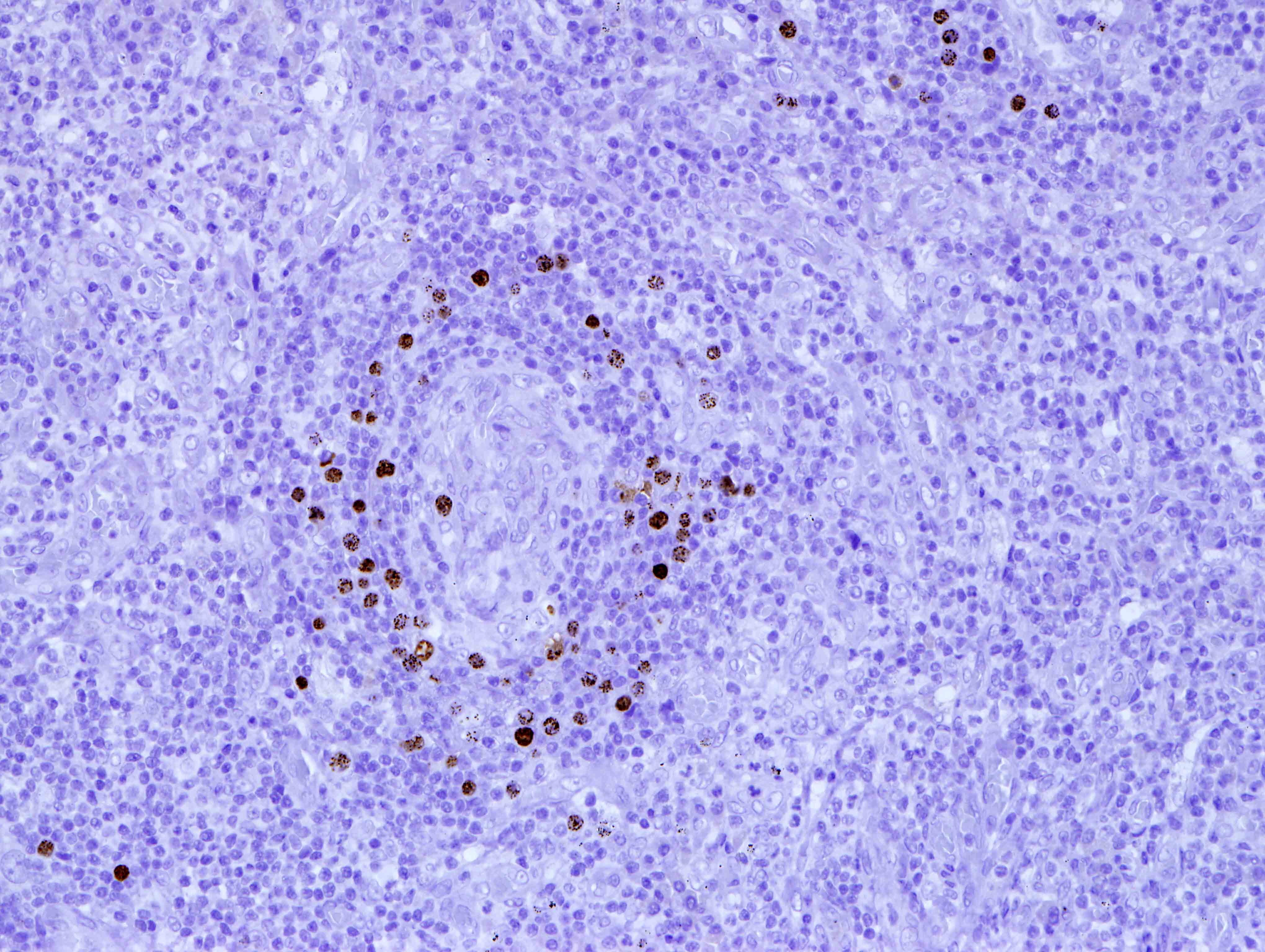
- Effacement of lymph node architecture by sheets of HHV8 positive, LANA1 positive and EBER negative plasmablasts (Am J Clin Pathol 2017;147:171)
Laboratory
- Rarely, there is involvement of bone marrow and peripheral blood by HHV8 positive IgM lambda plasmablasts (Eur J Haematol 2013;91:497)
Prognostic factors
- Extremely aggressive clinical course and poor prognosis
Case reports
- 37 and 42 year old men with multifocal hepatic Kaposi sarcoma and intravascular HHV8 positive (EBV negative) systemic DLBCL, NOS (Autops Case Rep 2020;10:e2020206)
- 56 year old man with an unusual EBV associated HHV8 positive large B cell lymphoma (Clin Case Rep 2019;7:587)
- 59 year old woman with hemoglobin sickle cell disease and sequential development of HHV8 positive DLBCL and chronic myelomonocytic leukemia (Pathol Res Pract 2019;215:152704)
Treatment
- No definite treatment guidelines
- Can be treated with the same regimens described for patients with HIV associated DLBCL
Gross description
- Involved lymph node is enlarged
- Firm, fleshy mass
Microscopic (histologic) description
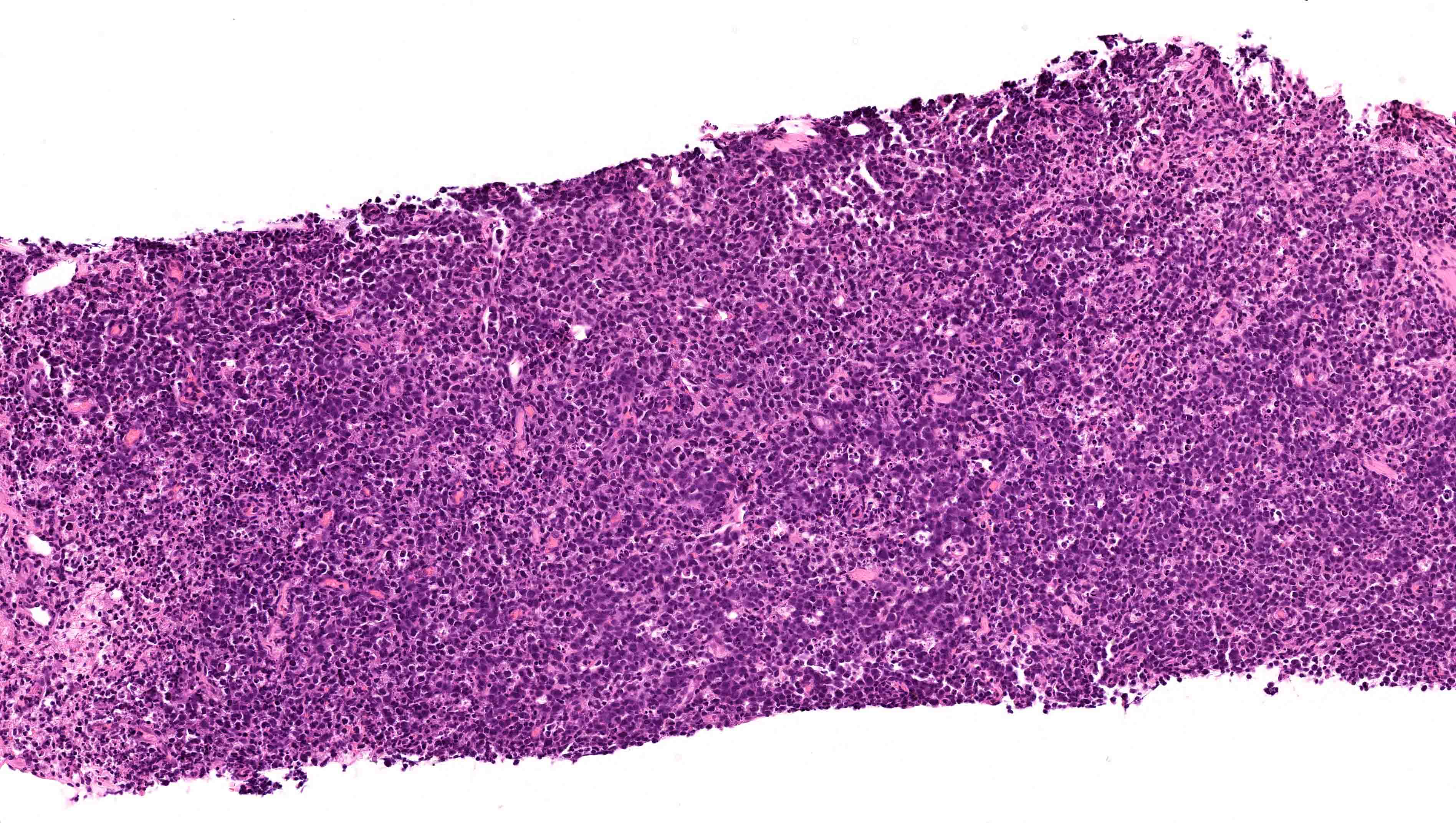
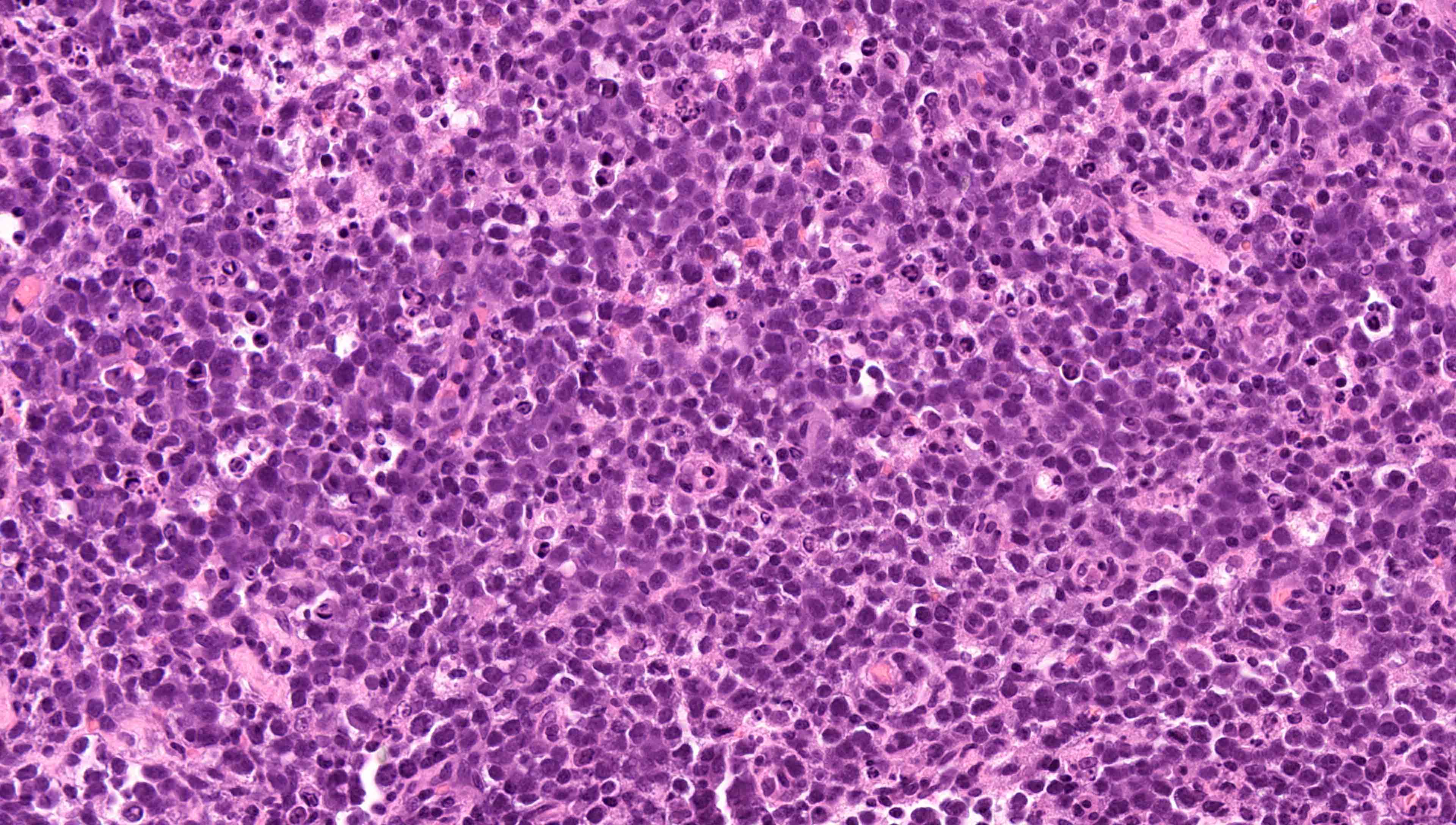
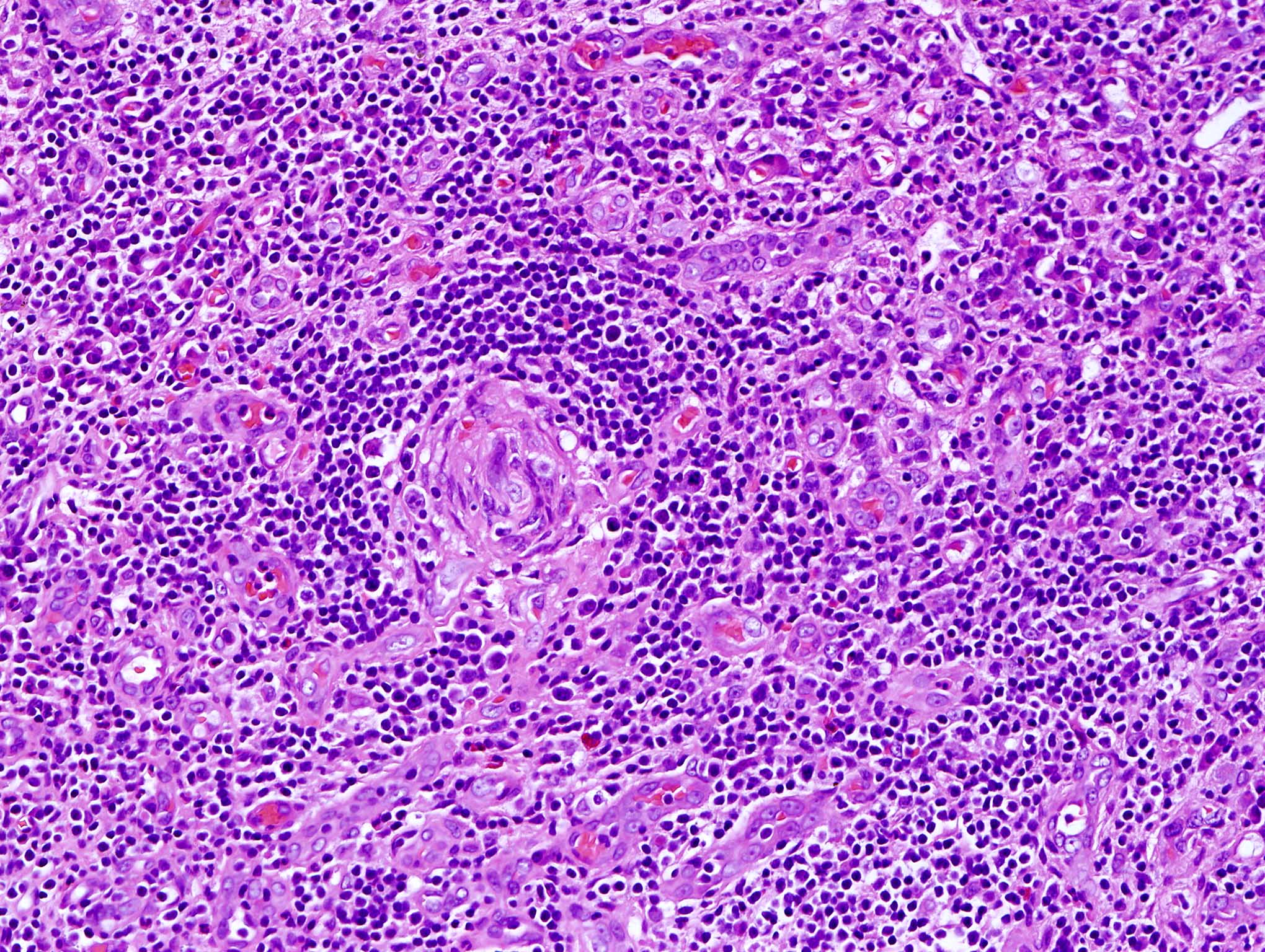
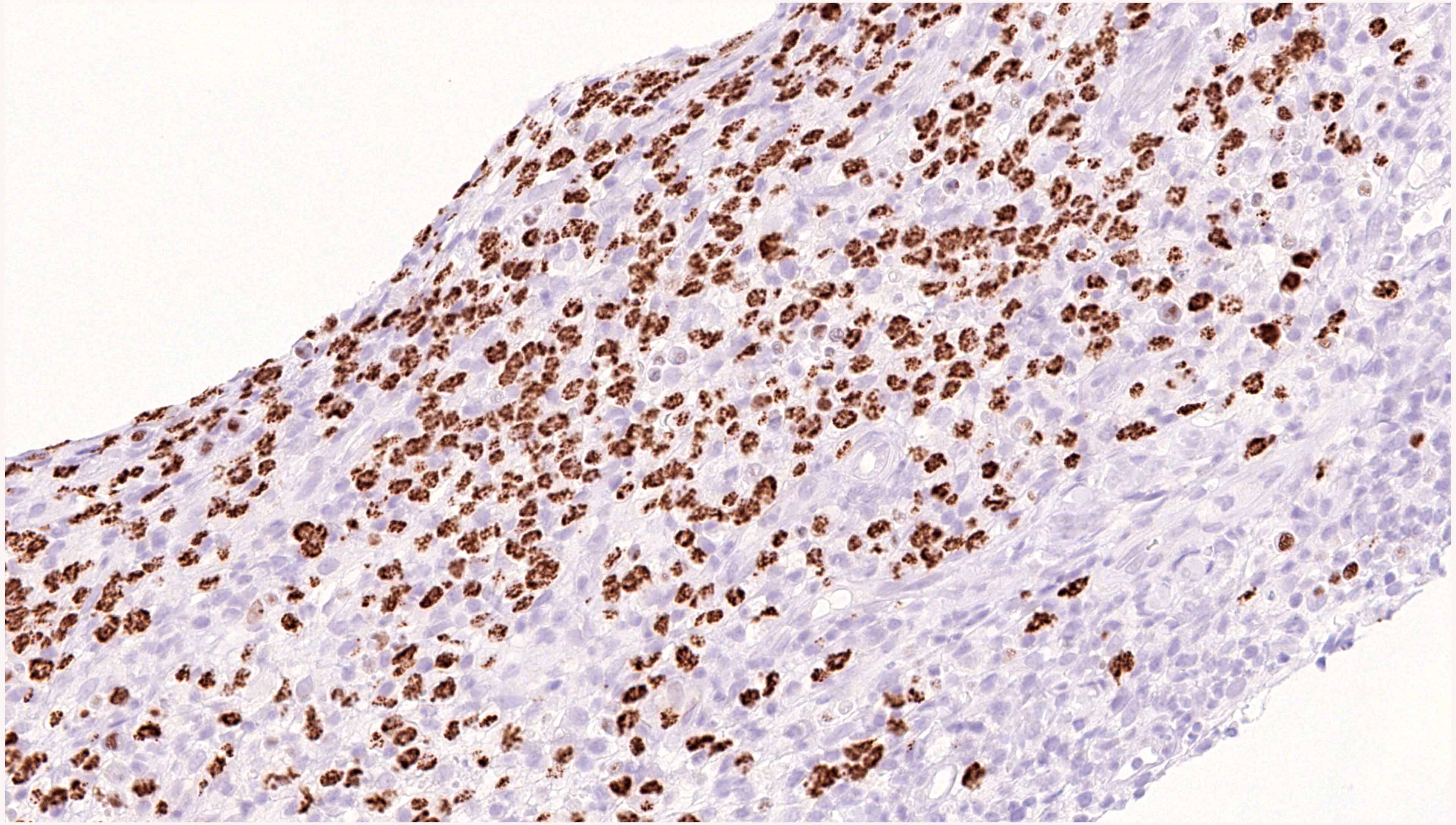
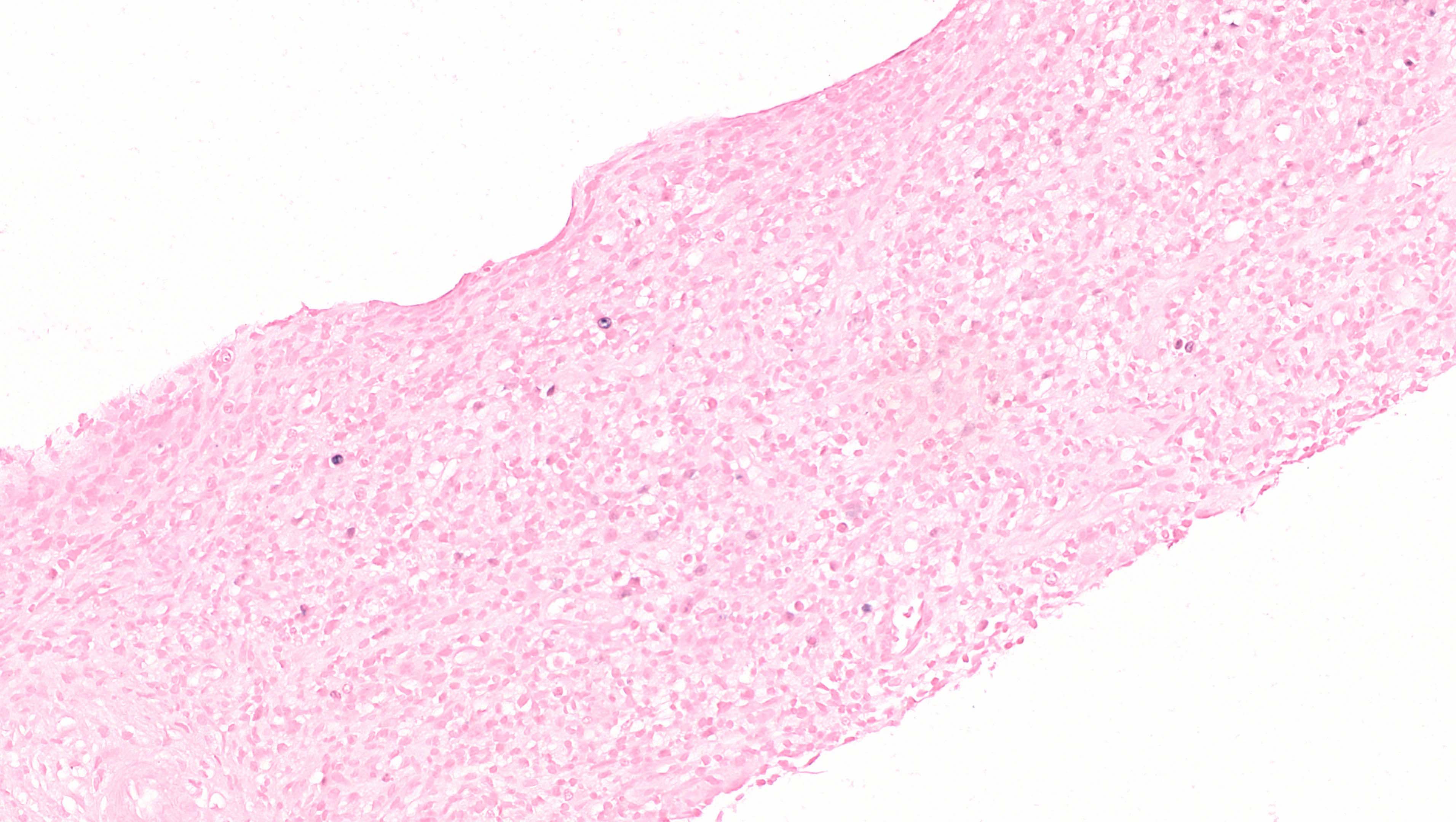
- Effacement of lymph node / splenic architecture by confluent sheets of large plasmablastic cells
- Large plasmablastic cells have amphophilic cytoplasm and vesicular, often eccentrically placed nuclei containing 1 or 2 prominent nucleoli (Am J Clin Pathol 2017;147:171)
- High mitotic activity
Microscopic (histologic) images
Positive stains
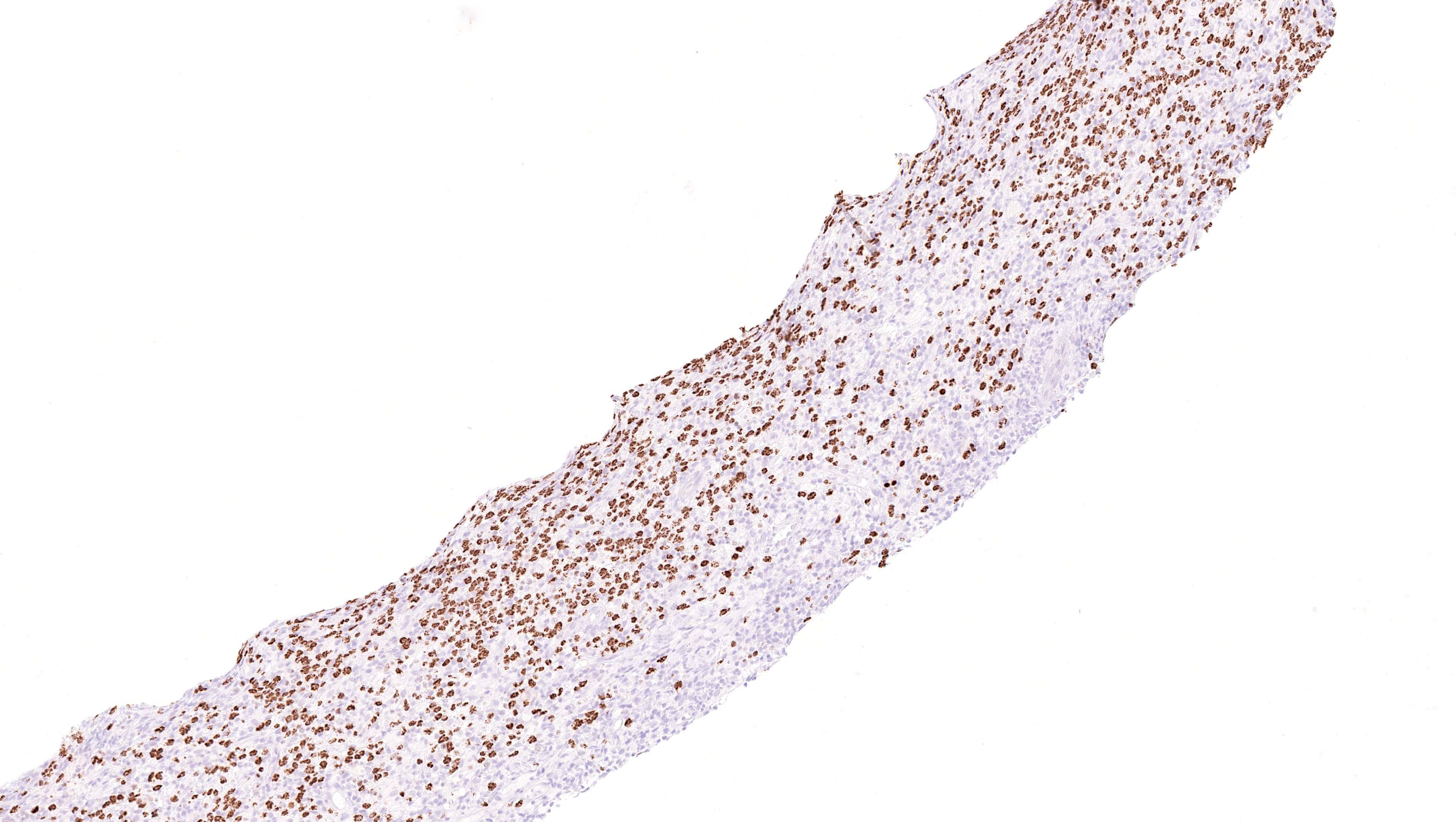
- Stippled nuclear staining for HHV8 (LANA1) in large plasmablasts in all cases
- Strongly express cytoplasmic IgM with lambda light chain restriction (Blood 2002;99:2331)
- MUM1
- CD20 and CD38 may be positive
Negative stains
Molecular / cytogenetics description
- PCR reveals a monoclonal B cell population
- Immunoglobulin (IG) genes are unmutated, lacking somatic hypermutation
Sample pathology report
- Lymph node, right cervical, excision:
- Diffuse large B cell lymphoma, HHV8 positive, NOS
Differential diagnosis
- Extracavitary primary effusion lymphoma (Am J Surg Pathol 2004;28:1401):
- HHV8+ multicentric Castleman disease (MCD) (Blood 2014;123:2924, Blood 2001;97:2130):
- Often presents with generalized lymphadenopathy and constitutional symptoms
- Abnormal follicles with varied degree of hyalinization and involution of germinal centers
- Widened concentric rings of mantle zones (onion skinning) and prominent penetrating venules
- Interfollicular plasma cell hyperplasia
- Plasmablasts predominantly in mantle zones and lambda light chain restricted
- Polyclonal pattern of IG rearrangement
- HHV8 related germinotropic lymphoproliferative disorder (Blood 2002;100:3415, Ann Pathol 2014;34:373):
- Occurs in immunocompetent patients
- HIV-
- Localized or sometimes multifocal lymph node involvement
- Retention of lymph node architecture with HHV8+ plasmablasts involving or replacing germinal centers
- EBER+, CD38+, kappa or lambda light chain restriction
- Polyclonal or oligoclonal pattern of IGH rearrangement
- Favorable response to chemotherapy or radiation
- Plasmablastic lymphoma (Histopathology 2012;61:1183, Am J Surg Pathol 2010;34:1686):
- Often presents in oral cavity or extranodal sites
- Association with immunodeficiency or HIV
- EBER+, HHV8-
- Usually expresses a plasma cell phenotype (CD38+, CD138+, MUM1+)
- Cytoplasmic immunoglobulin positive (mostly IgG and kappa / lambda)
- Frequently class switched and hypermutated IG genes
- MYC translocation in approximately 50% of cases
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is true about HHV8 related diffuse large B cell lymphoma (DLBCL), NOS?
- Clonal rearrangement pattern with somatic hypermutation of IG genes
- Clonal rearrangement pattern without somatic hypermutation of IG genes
- Polyclonal rearrangement pattern with somatic hypermutation of IG genes
- Polyclonal rearrangement pattern without somatic hypermutation of IG genes
Board review style answer #2
B. Clonal rearrangement pattern without somatic hypermutation of IG genes
Comment Here
Reference: HHV8 related DLBCL, NOS
Comment Here
Reference: HHV8 related DLBCL, NOS