Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ravindran A, Teruya-Feldstein J. Kimura disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodeskimurasdisease.html. Accessed April 2nd, 2025.
Definition / general
- Benign chronic inflammatory disorder of unknown etiology (Am J Surg Pathol 2004;28:505)
- Eosinophilic infiltrates forming microabscesses in a background of polymorphous inflammatory cells
Essential features
- Benign disorder of unknown etiology with an indolent clinical course
- Predominantly affects young Asian males
- Involves nodal and extranodal sites, most commonly skin, head and neck
- Commonly recurs postsurgical excision
Terminology
- First described in 1937 by Kimm and Szeto as eosinophilic hyperplastic lymphogranuloma
- In 1948, Kimura described it as "unusual granulation combined with hyperplastic changes in lymphoid tissue"; subsequently, this process was widely known as Kimura disease (Am J Otolaryngol 2017;38:626)
ICD coding
- ICD-10: D21.9 - Kimura disease
Epidemiology
- Predominantly affects males
- Peak incidence between ages 20 - 40 years (Int J Oral Maxillofac Surg 2017;46:350)
- Most common in Asians
Sites
- Nodal and extranodal
- Extranodal commonly includes skin and subcutaneous tissue, head and neck sites, including major salivary glands
Pathophysiology
- Th1 / Th2 cytokine imbalance has been postulated as an underlying pathogenesis
- Th2 cells may result in increased IgE production through interleukins (IL4 and IL5) and promote activation of eosinophils
- Reference: Auris Nasus Larynx 2011;38:77
Etiology
- Cause unknown
- Presumed to be a consequence of an infection triggering an abnormal immune response
Clinical features
- Insidious onset with an indolent clinical course
- Slow growing nodules / masses, often painless and nontender
- Systemic symptoms uncommon
- Nephrotic syndrome may occur in a subset (Ren Fail 2019;41:126)
- Recurrence is common after surgical excision
Diagnosis
- Morphologic diagnosis characterized by hyperplastic reactive follicles surrounded by eosinophilic infiltrates in a background of polymorphous inflammatory cells
Laboratory
- Elevated serum immunoglobulin IgE levels (Arch Pathol Lab Med 2007;131:650)
- Peripheral blood eosinophilia (Am J Otolaryngol 2017;38:626)
Radiology description
- Ultrasonography (US) and magnetic resonance imaging (MRI) studies are useful to detect extent of disease
- CT findings may demonstrate the following findings (AJNR Am J Neuroradiol 1996;17:382)
- Enlarged lymph nodes with homogeneous enhancement
- Major salivary glands and soft tissue may show heterogeneous enhancement
- US findings include the following findings (AJNR Am J Neuroradiol 2001;22:513)
- Enlarged lymph nodes appear as solid, hypoechoic and maintain hilar architecture
- Nodal involvement often exhibits hilar vascularity and occasionally a mixed hilar and capsular vascular pattern
- Soft tissue masses appear hypoechoic and predominantly solid but may occasionally have a cystic component with homogenous or heterogeneous internal architecture
- MRI findings may demonstrate varying signal intensity proportionate to amount of fibrosis and vascular proliferation (AJNR Am J Neuroradiol 1996;17:382)
Prognostic factors
- Benign entity with an indolent course
- Recurrence is common after surgical excision (Int J Oral Maxillofac Surg 2017;46:350)
Case reports
- 4 year old boy with bilateral upper eyelid swelling (Allergy Asthma Clin Immunol 2021;17:48)
- 7 year old boy with paralysis of bilateral lower extremities (BMC Surg 2020;20:209)
- 14 year old boy with submandibular swelling (Med Pharm Rep 2019;92:195)
- 18 year old man with nontender, mobile subcutaneous nodule below right ear (J Clin Diagn Res 2017;11:ME01)
- 28 year old man with multiple subcutaneous swellings of head and neck (Indian J Otolaryngol Head Neck Surg 2019;71:589)
Treatment
- Conservative management in asymptomatic cases
- Surgery followed by radiotherapy has been shown to result in longer period of remission (Int J Oral Maxillofac Surg 2017;46:350)
- Other options include corticosteroids with or without immunosuppressants (e.g. cyclosporine)
Gross description
- Enlarged lymph nodes
- Soft tissue involvement presents as large, tumor-like masses
Frozen section description
- Reactive lymphoid hyperplasia admixed with abundant eosinophils
- Other entities need to be evaluated on permanent sections prior to classification as Kimura disease (see Differential diagnosis)
Microscopic (histologic) description
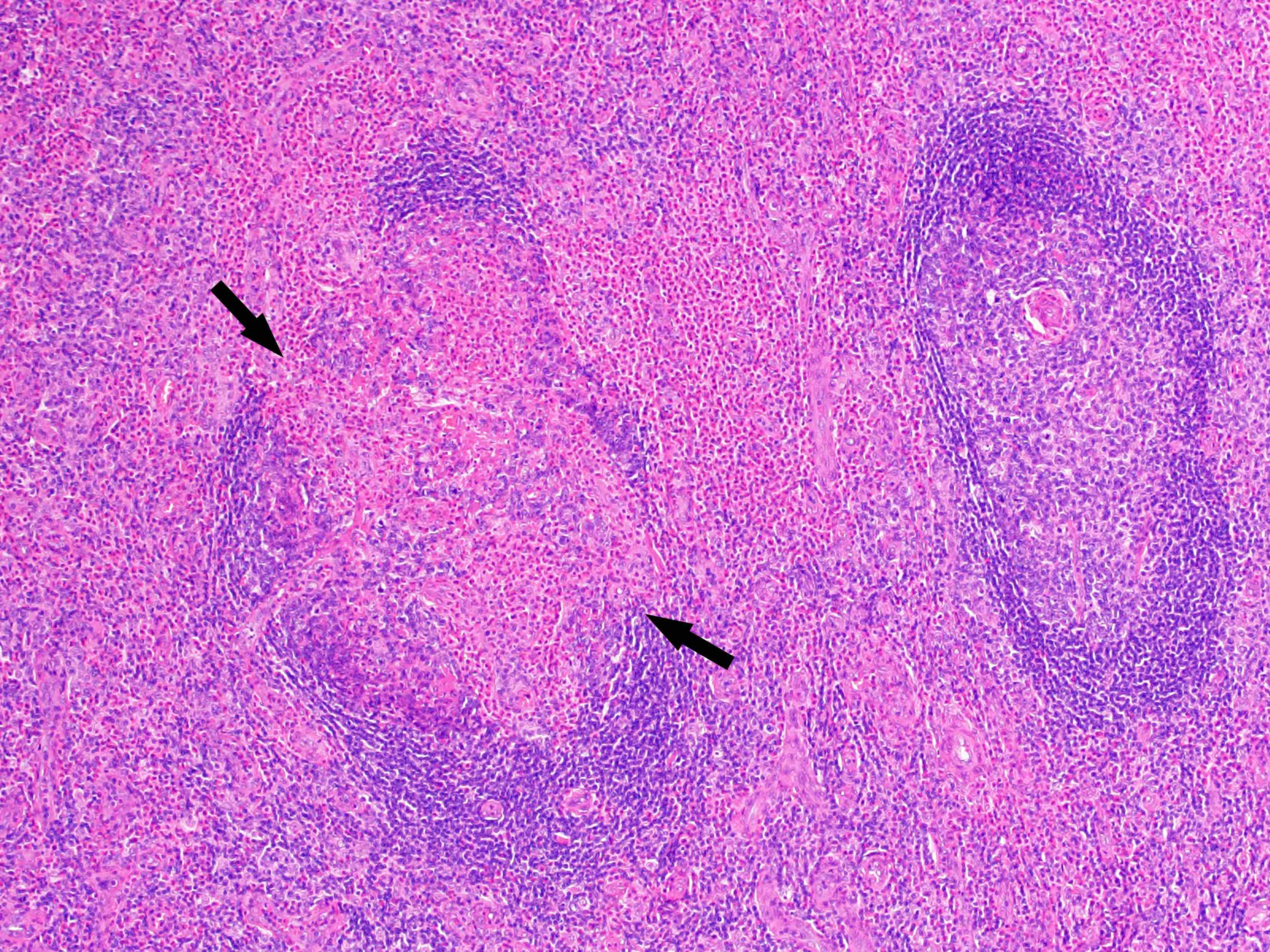
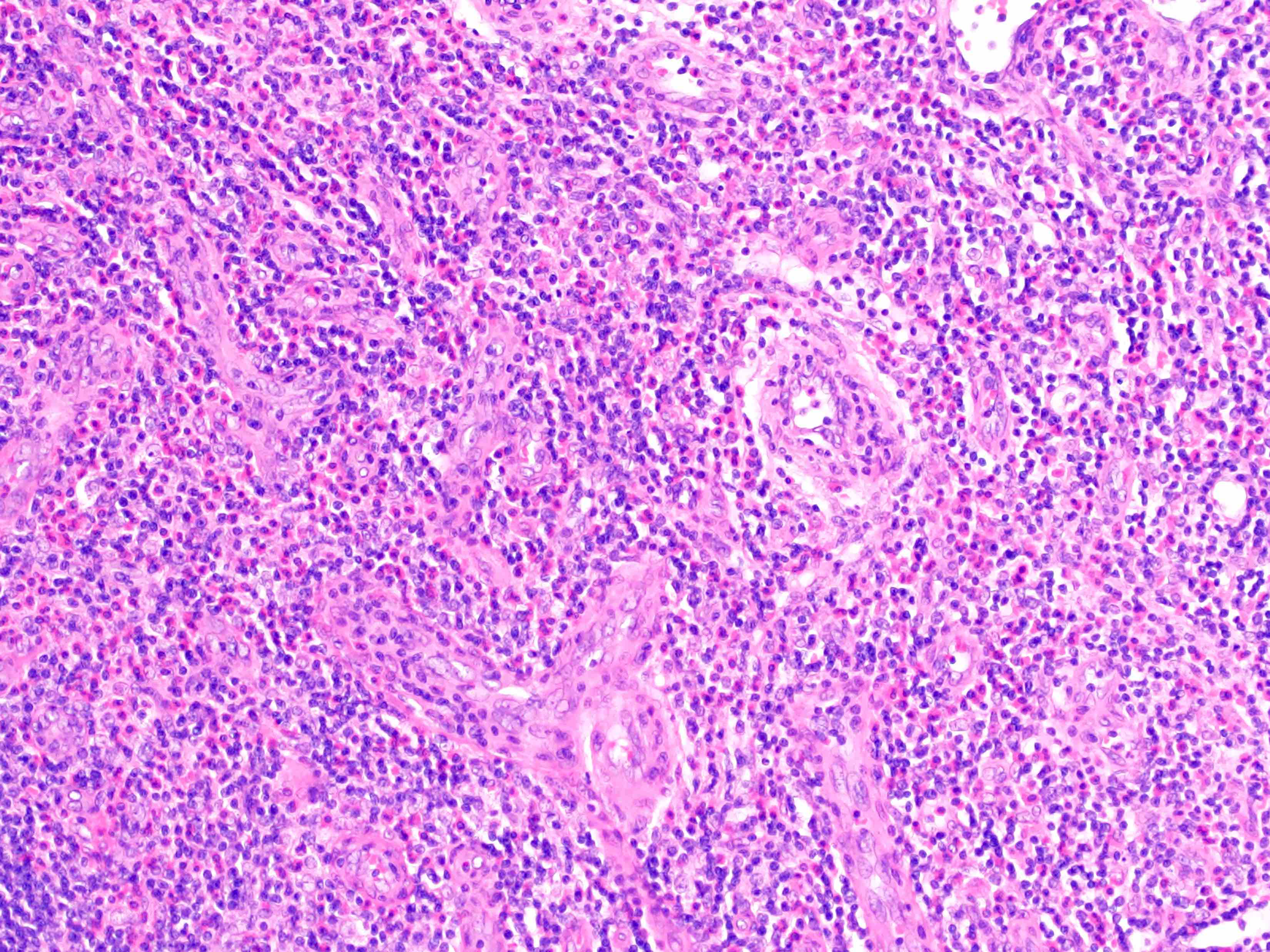
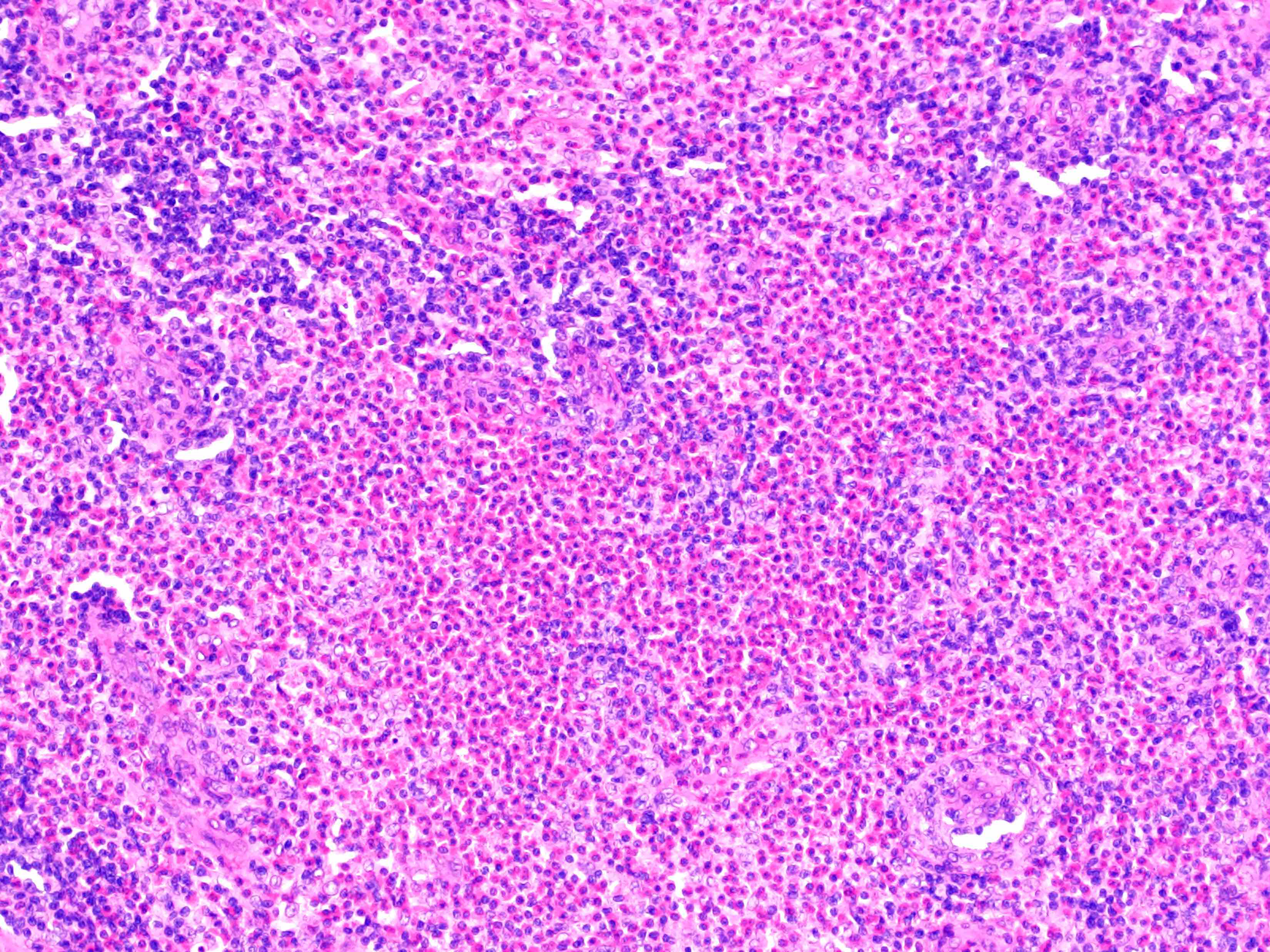
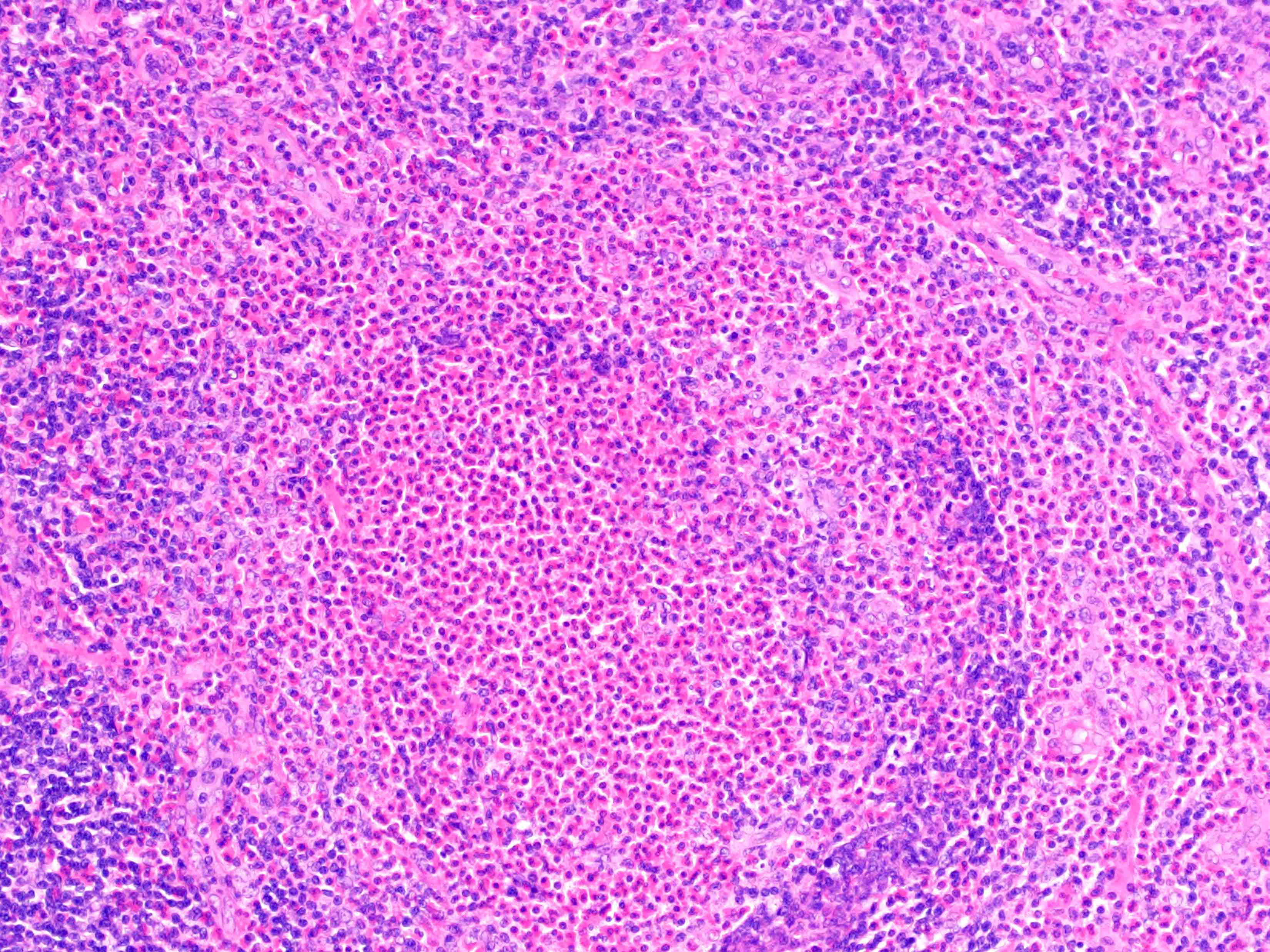
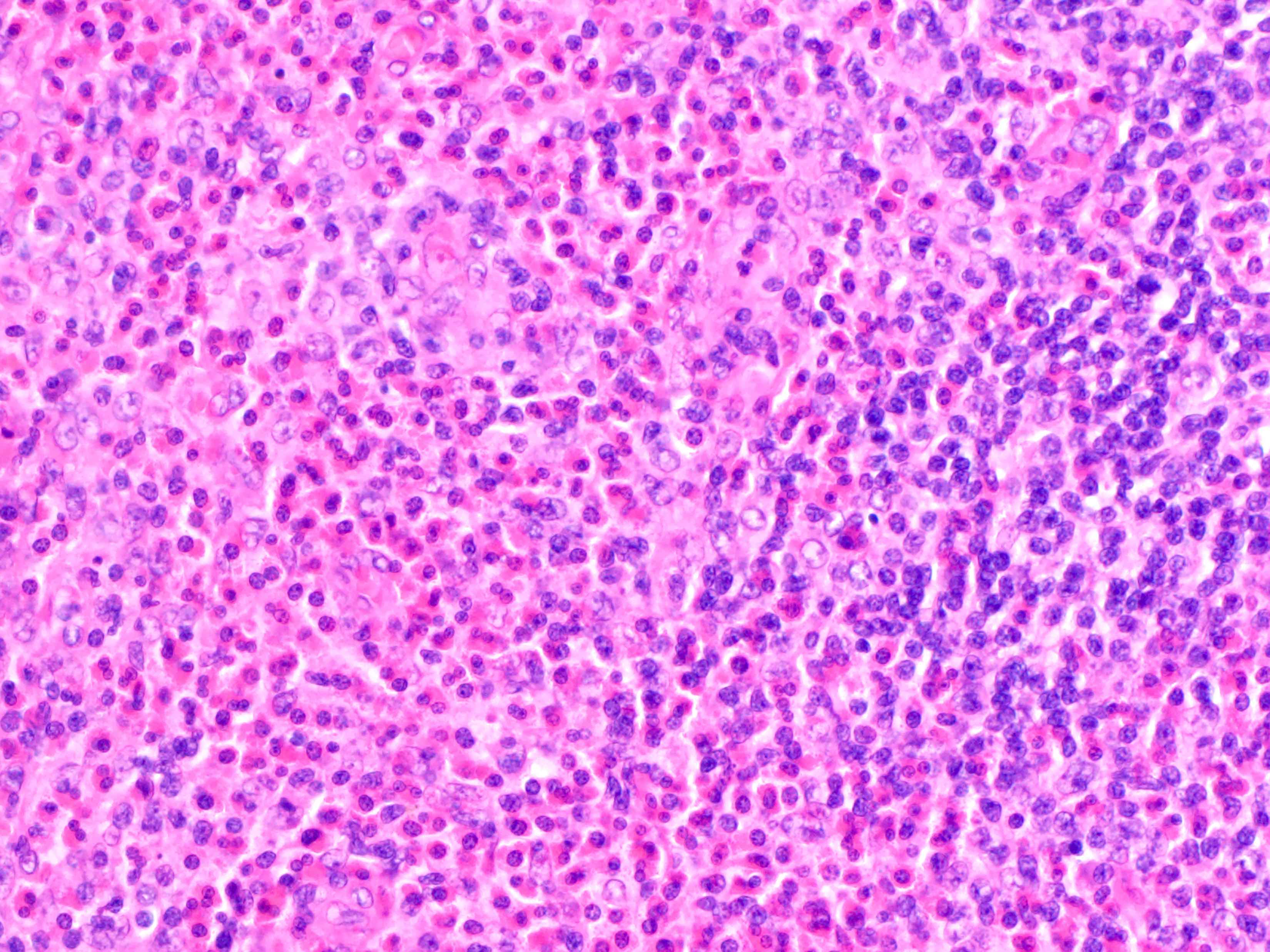
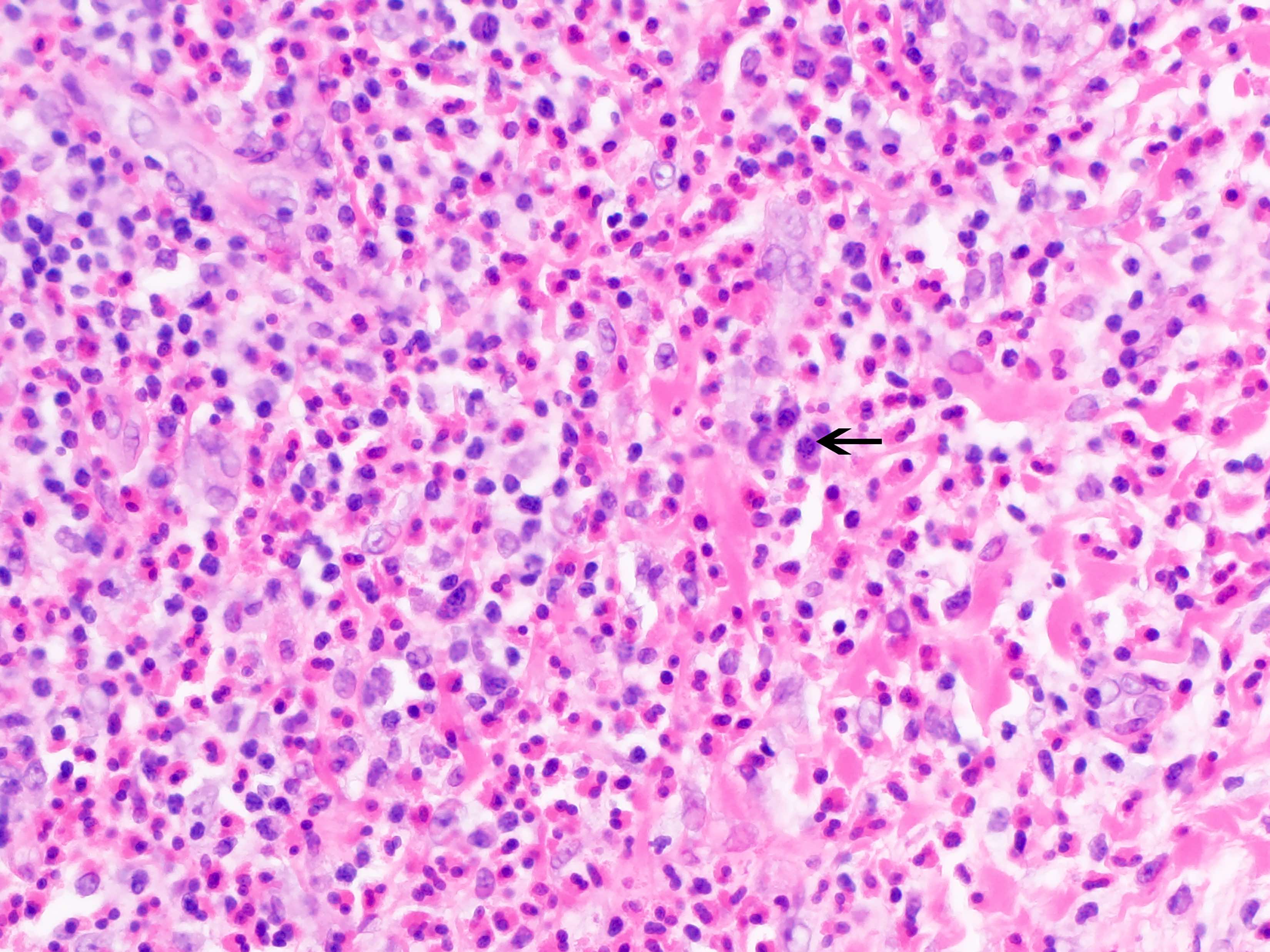
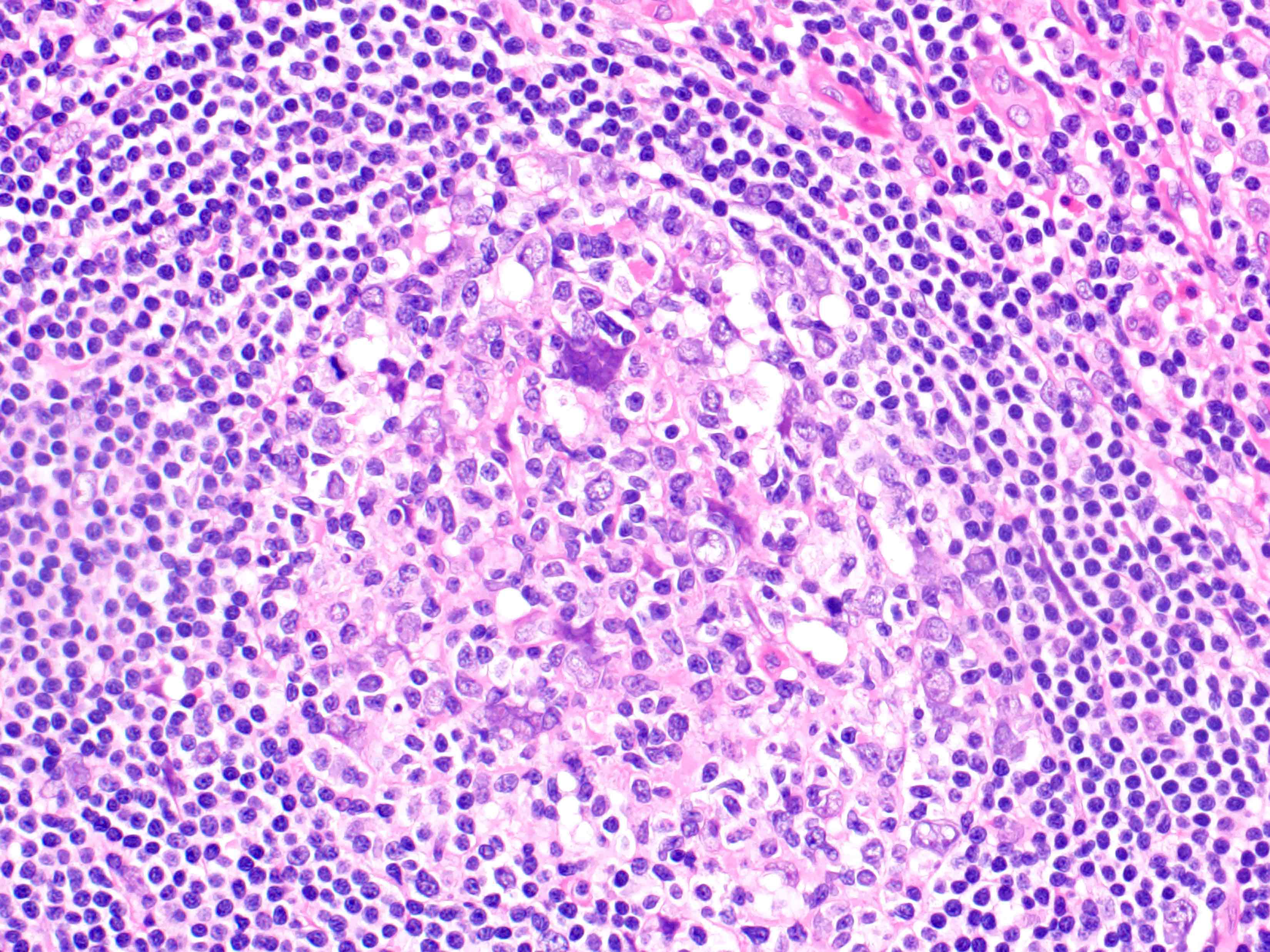
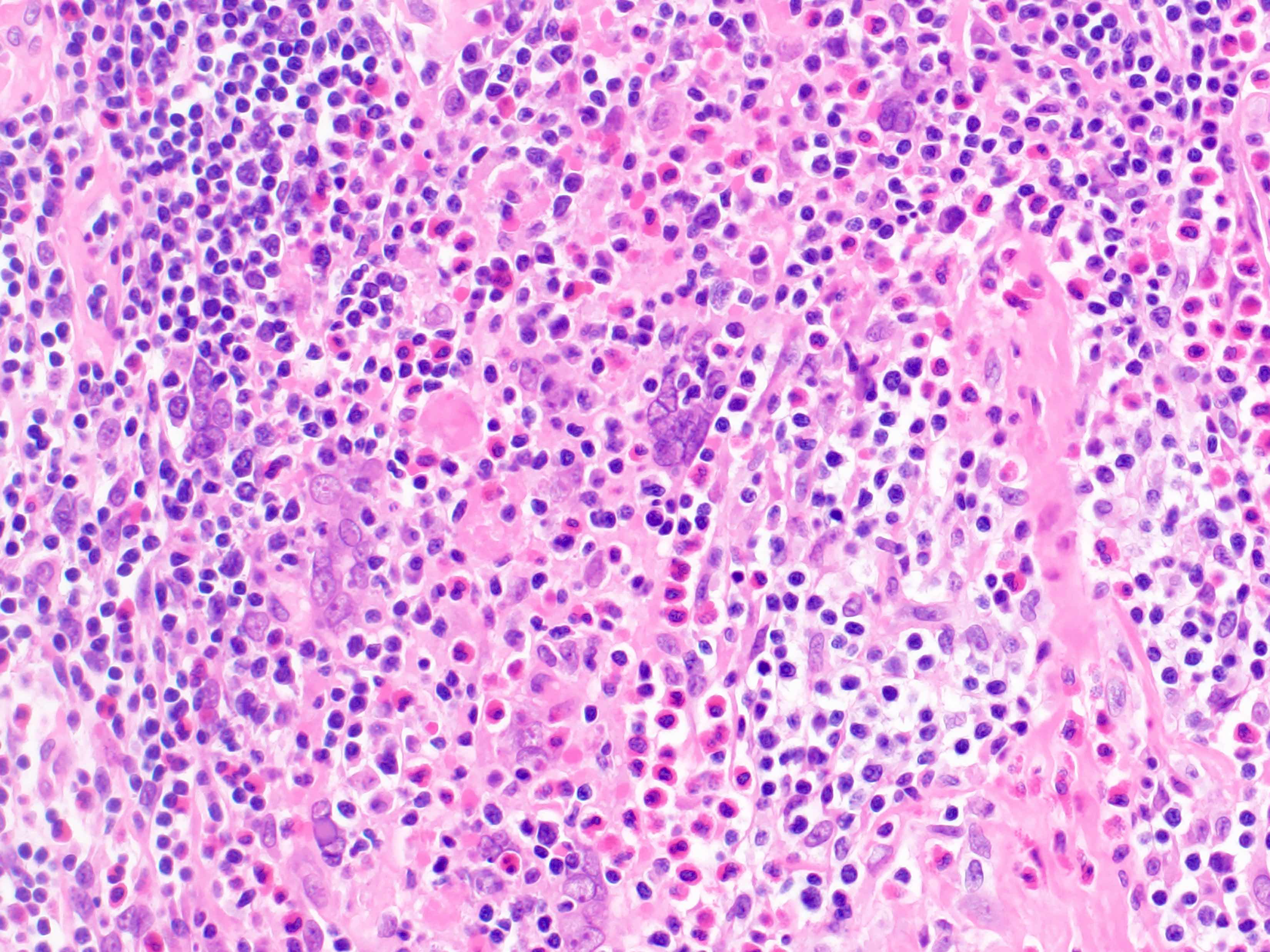
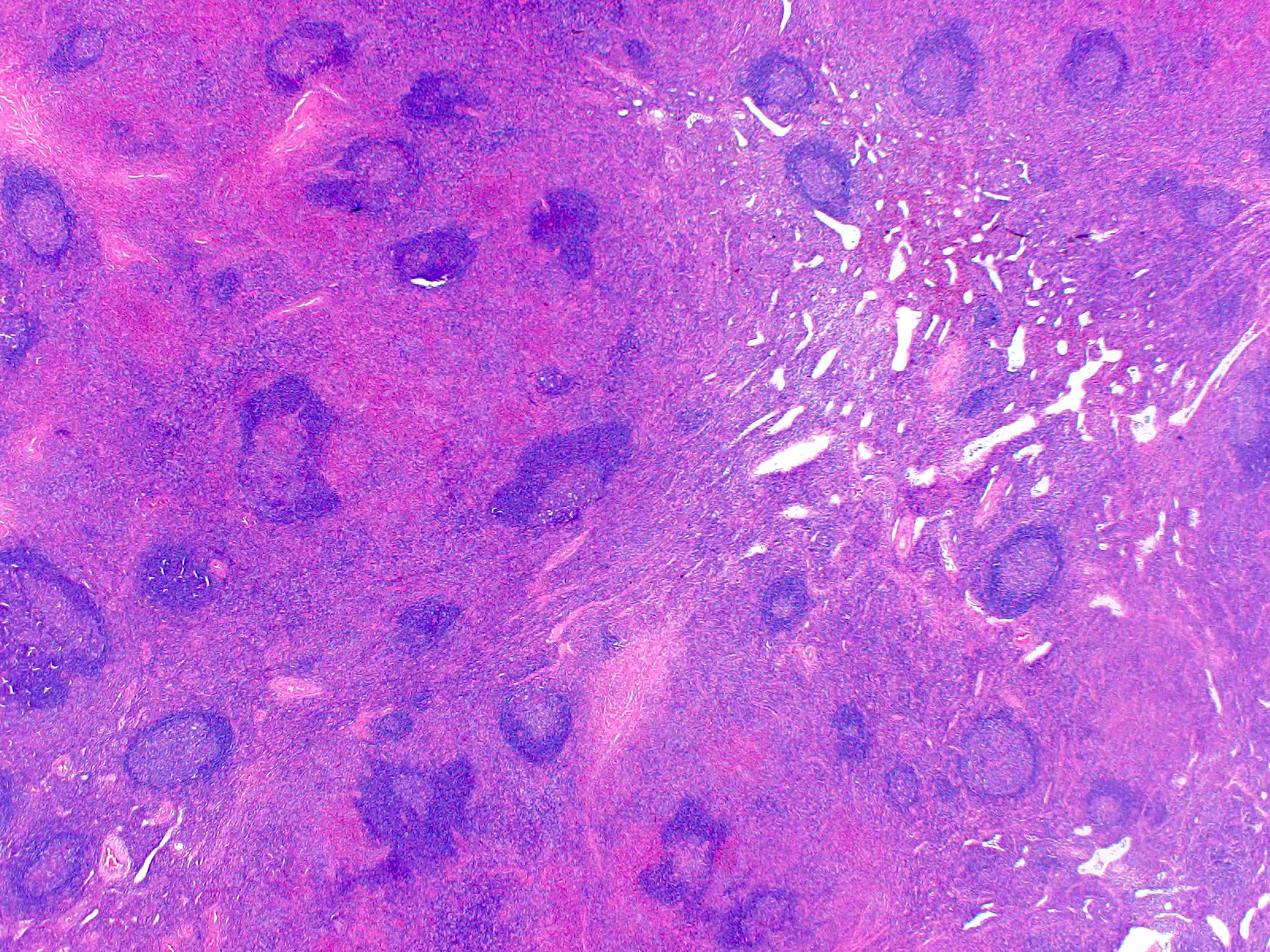
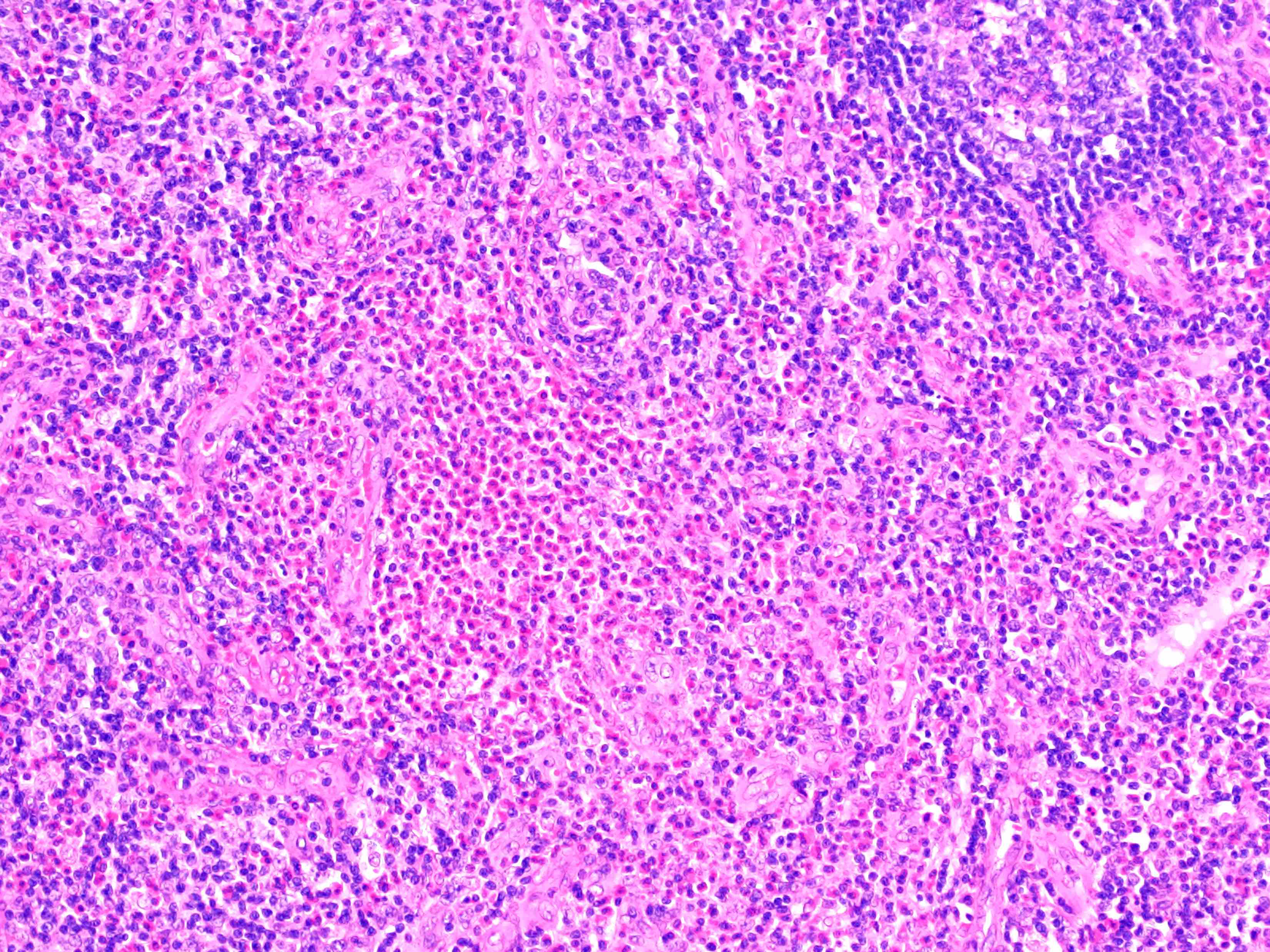
- Hyperplastic follicles with germinal centers associated with expansion of interfollicular areas by abundant eosinophils, often forming eosinophilic microabscesses (Arch Pathol Lab Med 2007;131:650)
- Disruption of follicles by increased eosinophils causing folliculolysis
- Proteinaceous material may be present in germinal center due to increased IgE deposition
- Admixed with polymorphous populations of lymphocytes, plasma cells, mast cells and histiocytes
- Polykaryocytes of Warthin-Finkeldey type may be present (Am J Surg Pathol 1989;13:177)
- Vascular proliferation in interfollicular areas
- Necrosis may be present
- Varying degree of sclerosis may be seen
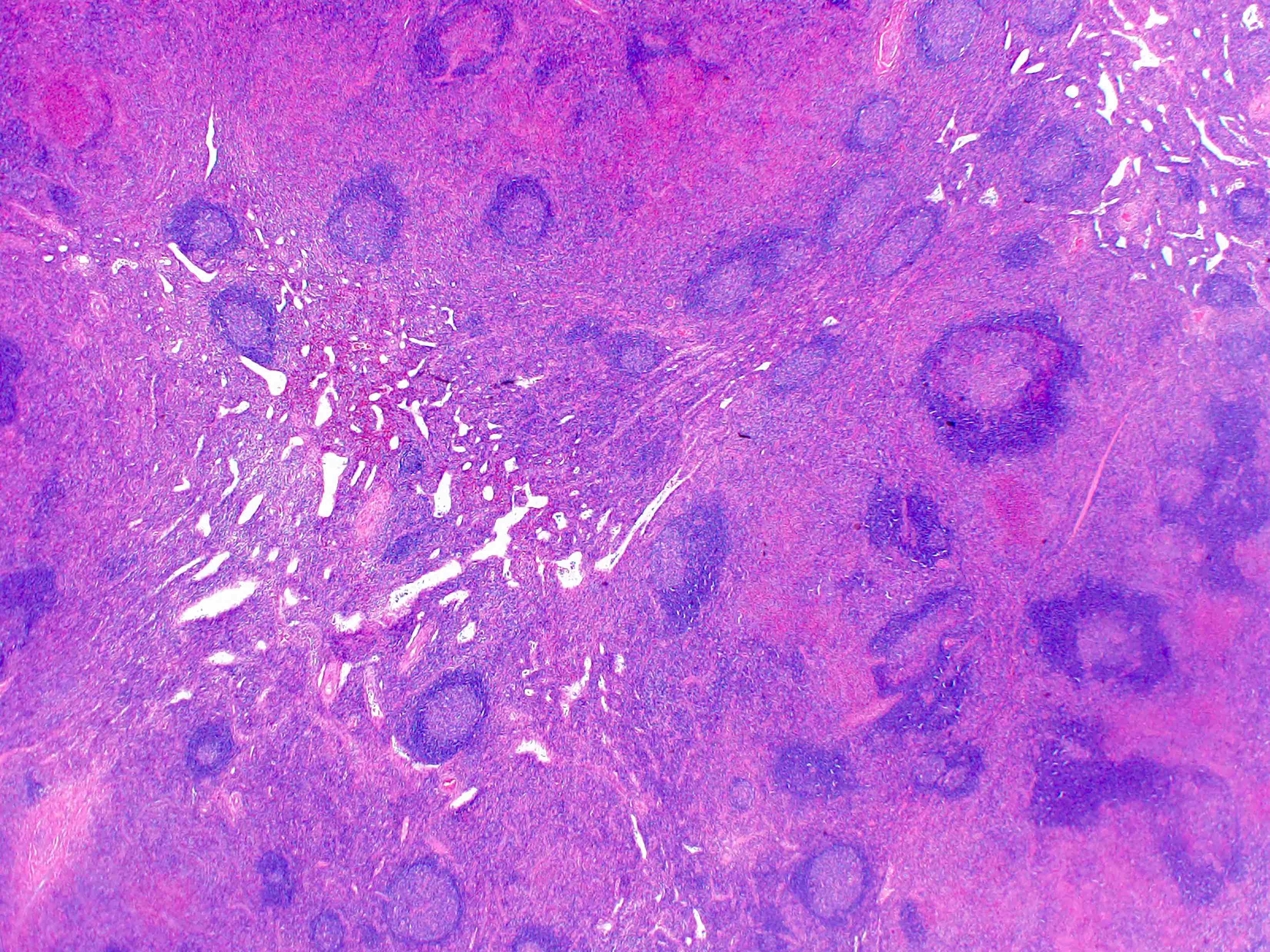
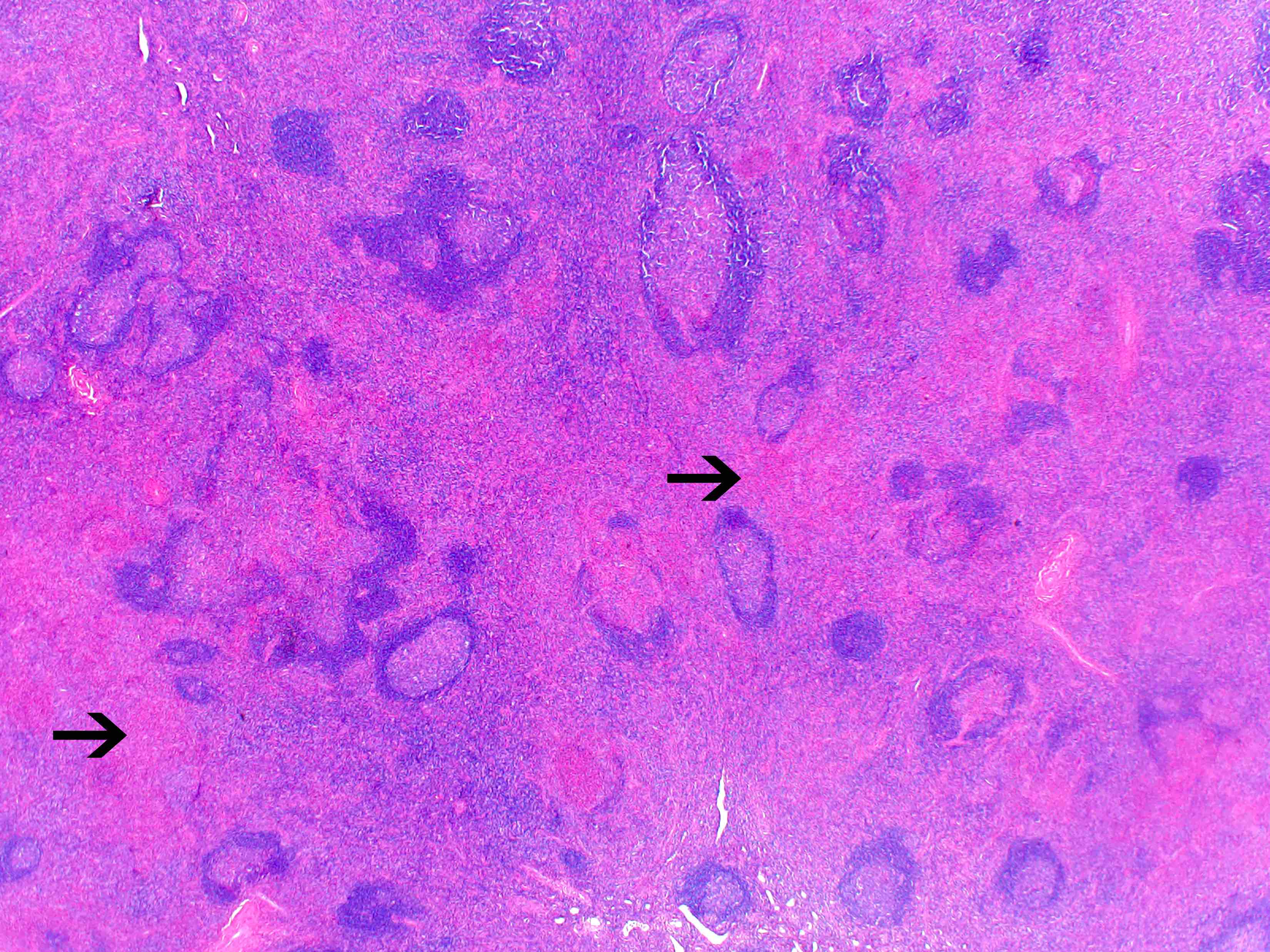
Microscopic (histologic) images
Cytology description
- Polymorphous population comprised of markedly increased eosinophils admixed with inflammatory cells (lymphocytes, plasma cells and occasionally histiocytes)
- Cytologic findings are not sufficient to diagnose; biopsy is required for definitive characterization (Acta Cytol 2002;46:357)
Positive stains
- Diagnosed on morphology; immunostains often not required
- Involved tissue shows a reactive background with a mixture of CD3 positive T cells and CD20 positive B cells
- IgE deposits in germinal centers (Am J Surg Pathol 1989;13:177)
Flow cytometry description
- Absence of abnormal B cells, aberrant T cell population or increased blasts
Molecular / cytogenetics description
- No known clonal gene rearrangements
- Negative for gene translocations
Sample pathology report
- Lymph node, right groin, excisional biopsy:
- Kimura disease (see comment)
- Comment: The right groin lymph node is involved by a proliferation of enlarged but well spaced secondary lymphoid follicles that maintain the normal zoning pattern of follicle center cells. The paracortex (interfollicular areas) is expanded by numerous eosinophils accompanied by small lymphocytes and occasional immunoblasts. Eosinophilic microabscesses are present and eosinophils also infiltrate some of the follicle centers. Additionally, the paracortex shows vascular proliferation. No malignant cells of any type are seen.
Differential diagnosis
- Reactive follicular hyperplasia:
- Clinical history is important
- May occur in a variety of conditions, such as infections, medications, autoimmune diseases
- Progressive transformation of germinal center:
- Hyperplastic germinal center follicles (4 - 5 times the normal) in a background of reactive follicular hyperplasia
- Eosinophilic microabscesses absent
- Epithelioid hemangioma (angiolymphoid hyperplasia with eosinophilia):
- Benign vascular neoplasm, common in superficial dermis
- Morphology shows lobular proliferation of capillaries that are lined by plump, epithelioid endothelial cells, usually associated with eosinophilic and lymphocytic inflammatory infiltrate
- Subset shows FOSB gene rearrangements
- Castleman disease, hyaline vascular variant:
- Large follicles with regressed germinal centers surrounded by concentric rings of mantle zone
- Interfollicular areas show increased vascular proliferation and plasmacytoid dendritic cells
- Eosinophilic microabscesses absent
- Dermatopathic lymphadenopathy (Clin Case Rep 2018;6:1637):
- Commonly involves axillary and inguinal lymph nodes
- Paracortical expansion of lymph node parenchyma by mixed population of Langerhans cells, pigment laden histiocytes and small lymphocytes
- Eosinophilic microabscesses absent
- Langerhans cell histiocytosis:
- Hodgkin lymphoma, mixed cellularity type:
Board review style question #1
A 30 year old previously healthy Asian man presented with enlarged cervical lymph node (see images above). Infectious and autoimmune workup were unrevealing. He was not taking any medications. Immunohistochemistry showed a mixture of CD3 positive T cells and CD20 positive B cells. Which of the following is the best diagnosis?
- HIV lymphadenitis
- Kikuchi-Fujimoto disease
- Kimura disease
- Langerhans cell histiocytosis
- Rosai-Dorfman disease
Board review style answer #1
Board review style question #2
Microabscesses in Kimura disease are composed of which of the following inflammatory cells?
- Eosinophils
- Langerhans cells
- Lymphocytes
- Neutrophils
- Plasma cells
Board review style answer #2