Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Beckman A, Courville E. Kikuchi disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodeskikuchi.html. Accessed April 2nd, 2025.
Definition / general
- Benign, self limited lymphadenitis of unknown etiology with distinct histopathologic features
Essential features
- Benign, self limited lymphadenitis of unknown etiology
- Predominantly affects young adults, with cervical lymphadenopathy, fever and often leukopenia
- Involved lymph nodes show histiocytes, plasmacytoid dendritic cells, immunoblasts and necrosis with karyorrhectic debris
- Histologic features overlap with autoimmune disease associated lymphadenitis, especially systemic lupus erythematosus
- Clinically and histologically may mimic lymphoma
Terminology
- Kikuchi-Fujimoto disease
- Kikuchi lymphadenitis
- Histiocytic necrotizing lymphadenitis
- Subacute necrotizing lymphadenitis
ICD coding
- ICD-10: I88 - nonspecific lymphadenitis
Epidemiology
- M:F = 1:1 - 4
- Primarily young adults (average 20 - 30 years) but any age may be affected
- Initially described in Asia; now known to occur worldwide
- References: Semin Diagn Pathol 1988;5:329, Int J Infect Dis 2009;13:322, Acta Pathol Jpn 1993;43:635, Am J Surg Pathol 1995;19:798, Otolaryngol Head Neck Surg 2003;128:650, Clin Rheumatol 2007;26:50, Semin Arthritis Rheum 2012;41:900, Cureus 2020;12:e7383
Sites
- Cervical lymph nodes, especially posterior
- Other lymph nodes less commonly involved (axillary, mediastinal, abdominal, inguinal)
- Rarely, extranodal sites, including skin
Pathophysiology
- Necrosis is due to apoptotic cell death mediated by cytotoxic T cells (Acta Otolaryngol Suppl 1998;538:250, Mod Pathol 1997;10:231)
Etiology
- Etiology unknown
- May represent a T cell and histiocyte mediated immune reaction to an infectious agent; however, no definitive causal relationship with a specific infection established (Pathologica 2016;108:120, Cancer Control 2014;21:313, Clin Rheumatol 2007;26:50)
- May represent a self limited autoimmune process (Semin Diagn Pathol 1988;5:329, Semin Arthritis Rheum 2012;41:900)
- May be more likely in genetically predisposed individuals: HLA class II alleles DPA1*01 and DPB1*0202 more frequent among Japanese patients with Kikuchi disease than controls (Tissue Antigens 1999;54:246)
Clinical features
- Acute or subacute onset
- Lymphadenopathy (typically painful), usually cervical; may affect lymph nodes at other sites or be generalized
- Fever is common
- Additional symptoms may include weight loss, night sweats, fatigue, malaise, erythematous rash, headache, upper respiratory tract symptoms, joint pain, diarrhea, nausea, vomiting (J Microbiol Immunol Infect 2010;43:366, Pathologica 2016;108:120, Clin Rheumatol 2007;26:50, Semin Diagn Pathol 1988;5:329, Int J Infect Dis 2009;13:322)
- May co-occur with or precede a diagnosis of systemic lupus erythematosus (2 - 23% of patients) or another autoimmune condition (Sjögren syndrome, polymyositis, rheumatoid arthritis, vasculitis, antiphospholipid syndrome, Still disease)
- If associated with systemic lupus erythematosus, may be best diagnosed as lymphadenitis associated with systemic lupus erythematosus (Semin Arthritis Rheum 2012;41:900, Case Rep Hematol 2018;2018:1791627, Int J Infect Dis 2009;13:322, Otolaryngol Head Neck Surg 2003;128:650)
Diagnosis
- Lymph node excision with pathologic examination
Laboratory
- No definitive diagnostic laboratory test
- Leukopenia
- Leukocytosis, especially in young children (Cureus 2020;12:e7383)
- Anemia
- Elevated lactate dehydrogenase
- Elevated erythrocyte sedimentation rate; elevated C reactive protein
- Antinuclear antibodies (ANA), anti-DNA antibodies and rheumatoid factor (RF) typically negative
- Viral serologies typically negative
- References: Otolaryngol Head Neck Surg 2003;128:650, Semin Diagn Pathol 1988;5:329, Semin Arthritis Rheum 2012;41:900, Clin Rheumatol 2007;26:50, Pathologica 2016;108:120, J Microbiol Immunol Infect 2010;43:366
Prognostic factors
- Usually self limited; resolves within 1 - 6 months
- May recur (3 - 21% of patients) (Am J Surg Pathol 1995;19:798, Am J Surg Pathol 1994;18:219, Int J Infect Dis 2009;13:322, Semin Diagn Pathol 1988;5:329, J Microbiol Immunol Infect 2010;43:366)
- Rare fatalities reported (Pathologica 2016;108:120, Cancer 1989;63:1856, Clin Rheumatol 2007;26:50)
Case reports
- 20 month old boy with enlarged axillary lymph node and rash (Cureus 2020;12:e7383)
- 4 year old boy with Kikuchi disease and hemophagocytic lymphohistiocytosis (Medicine (Baltimore) 2020;99:e23500)
- 20 year old man with fevers and cervical adenopathy (Blood 2017;129:917)
- 38 year old woman with cervical lymphadenopathy (Head Neck Pathol 2020;14:272)
Treatment
- Observation or supportive care (for example, nonsteroidal anti-inflammatory drugs) (Arch Pathol Lab Med 2010;134:289, Arch Pathol Lab Med 2018;142:1341)
- May include corticosteroid therapy (J Laryngol Otol 2000;114:709, Medicine (Baltimore) 2014;93:372)
- Followup is recommended, along with relevant laboratory studies, if indicated, to monitor for development of systemic lupus erythematosus
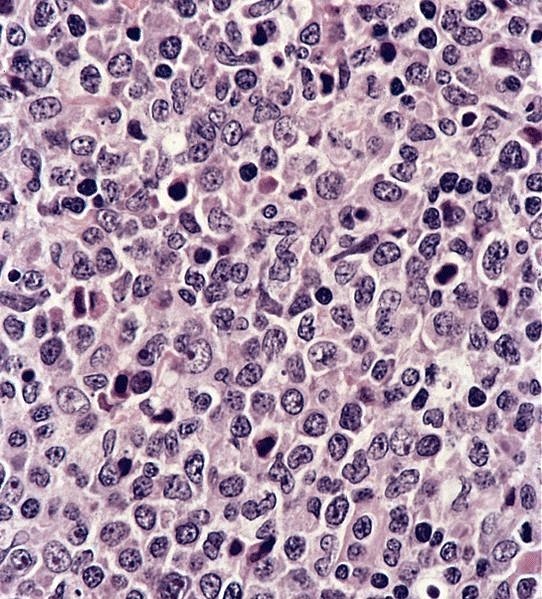
Microscopic (histologic) description
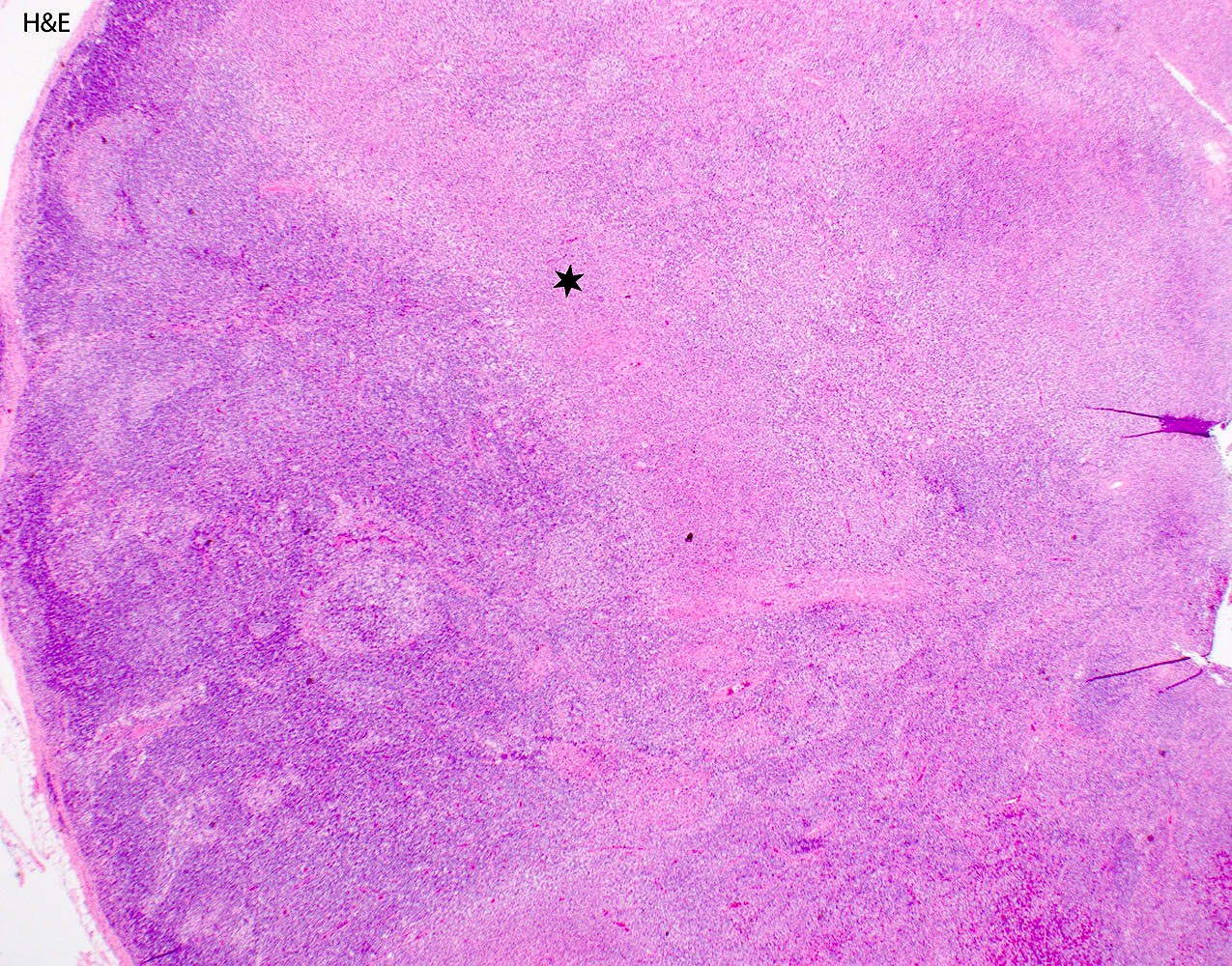
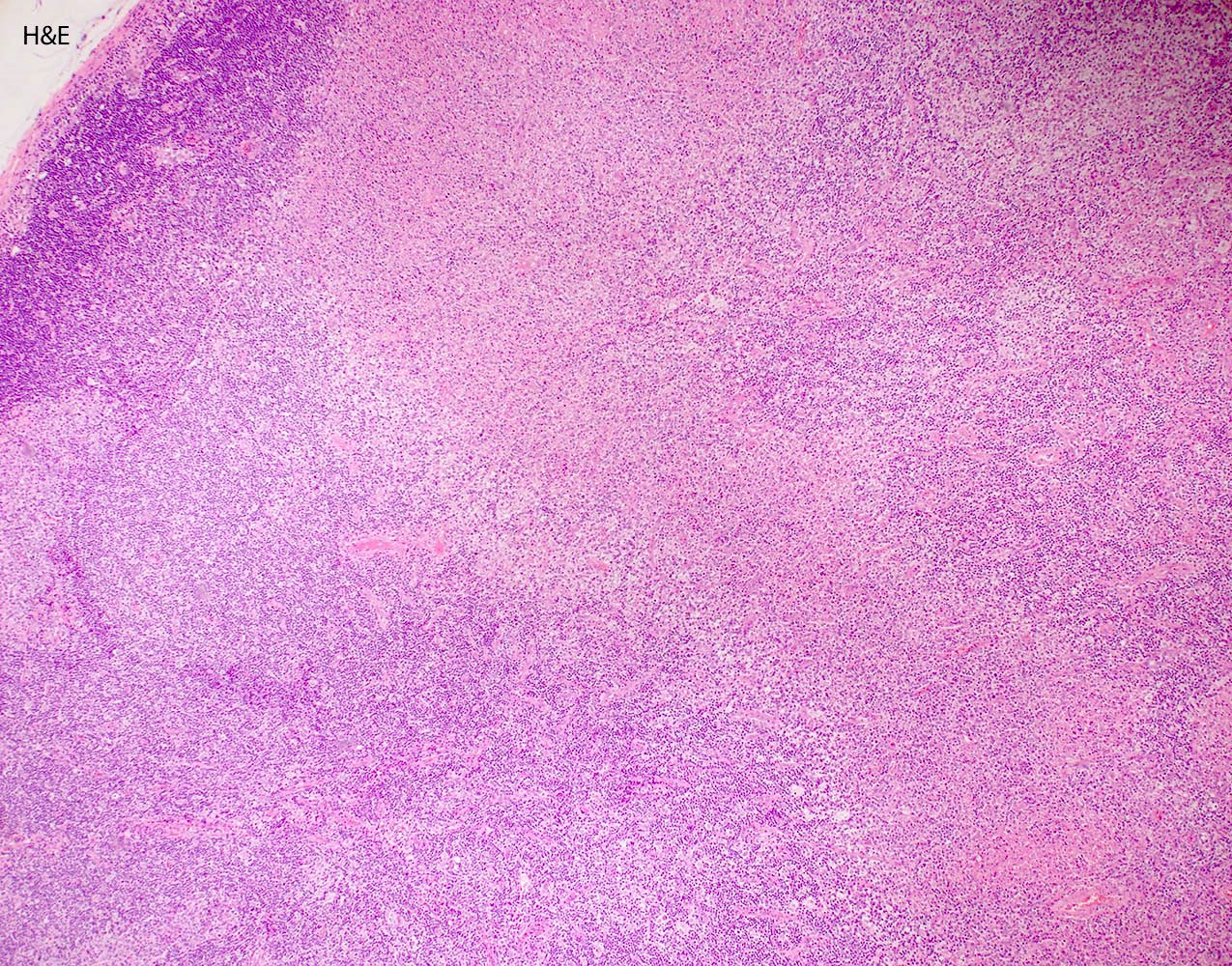
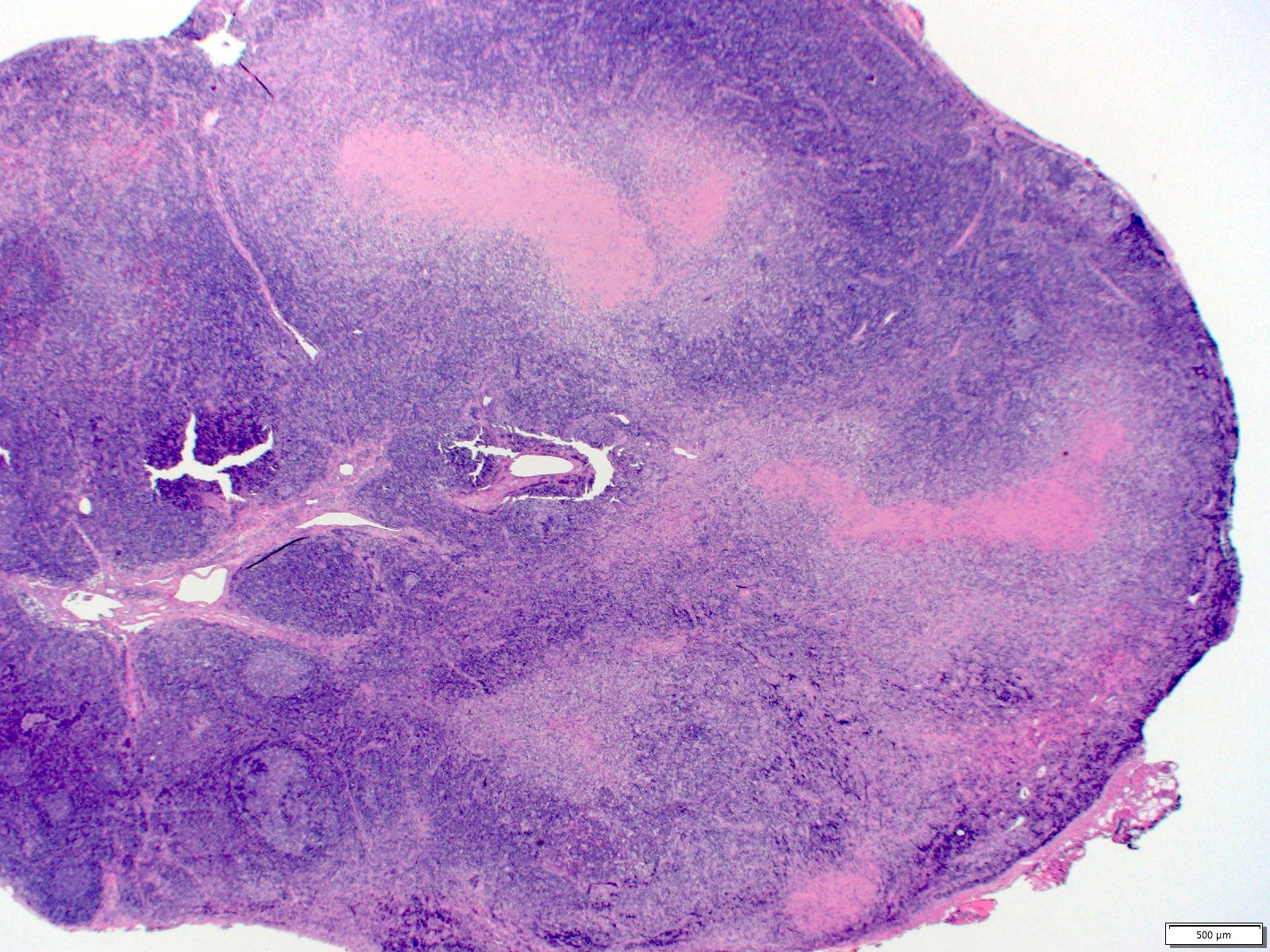
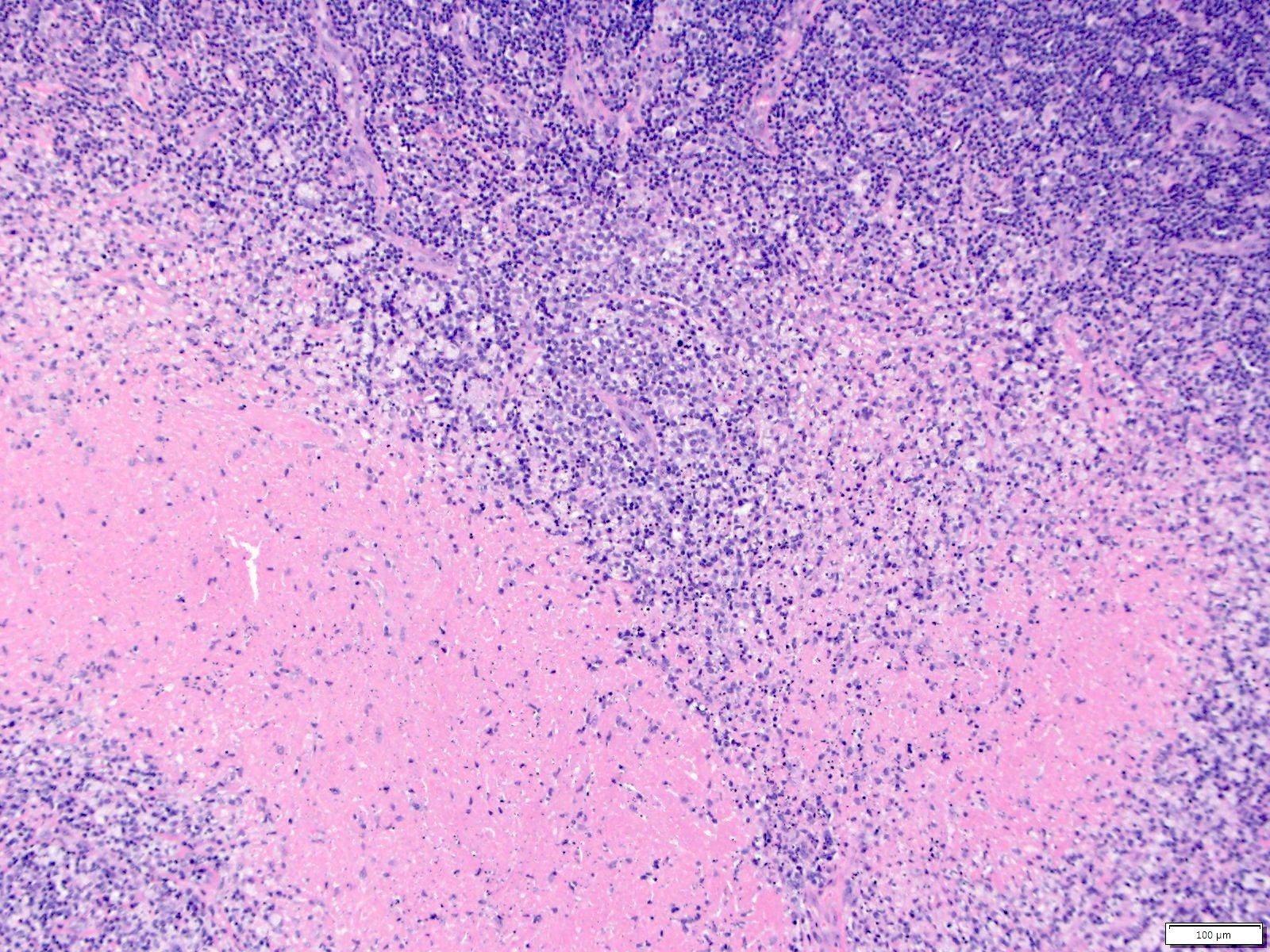
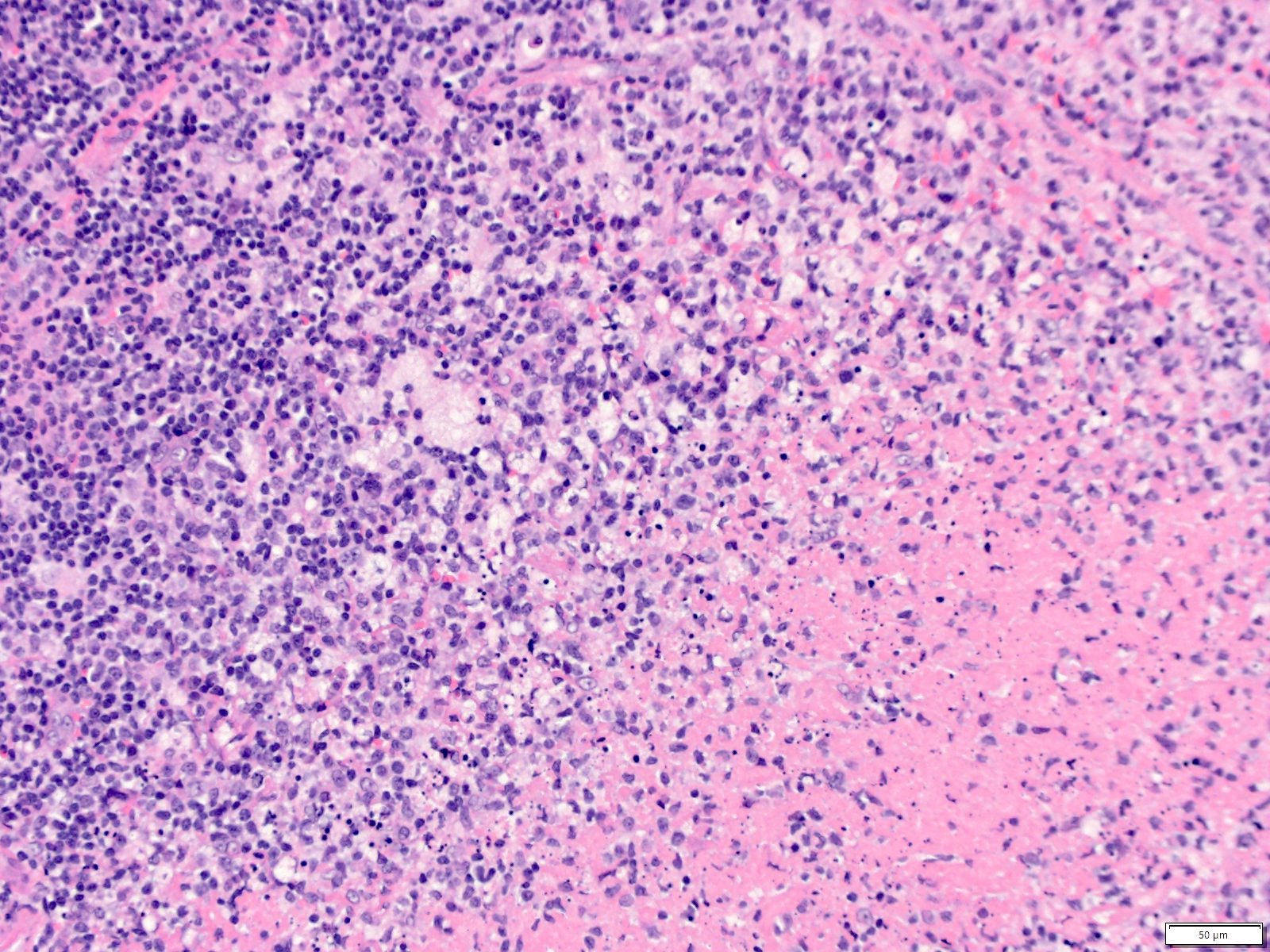
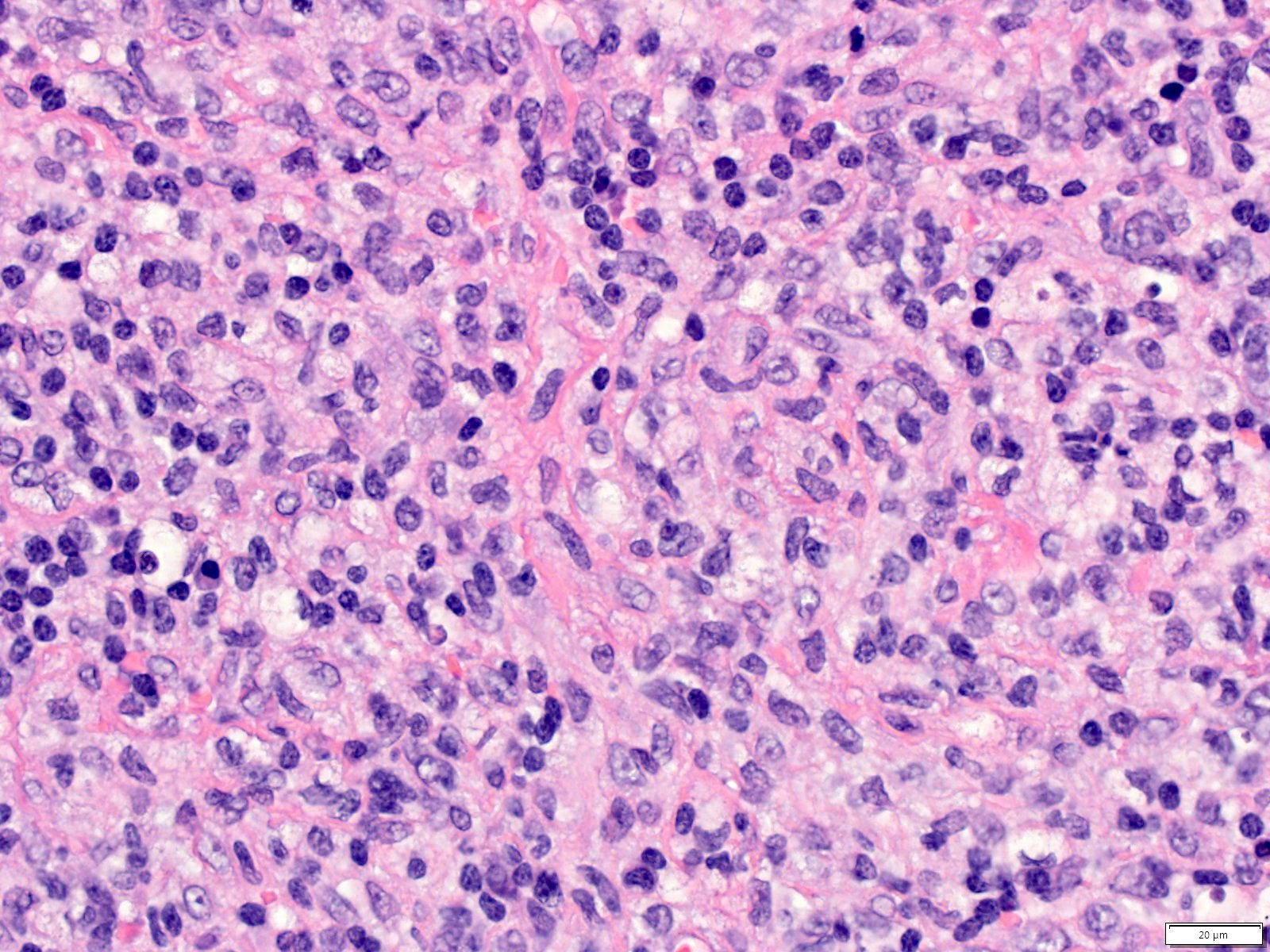
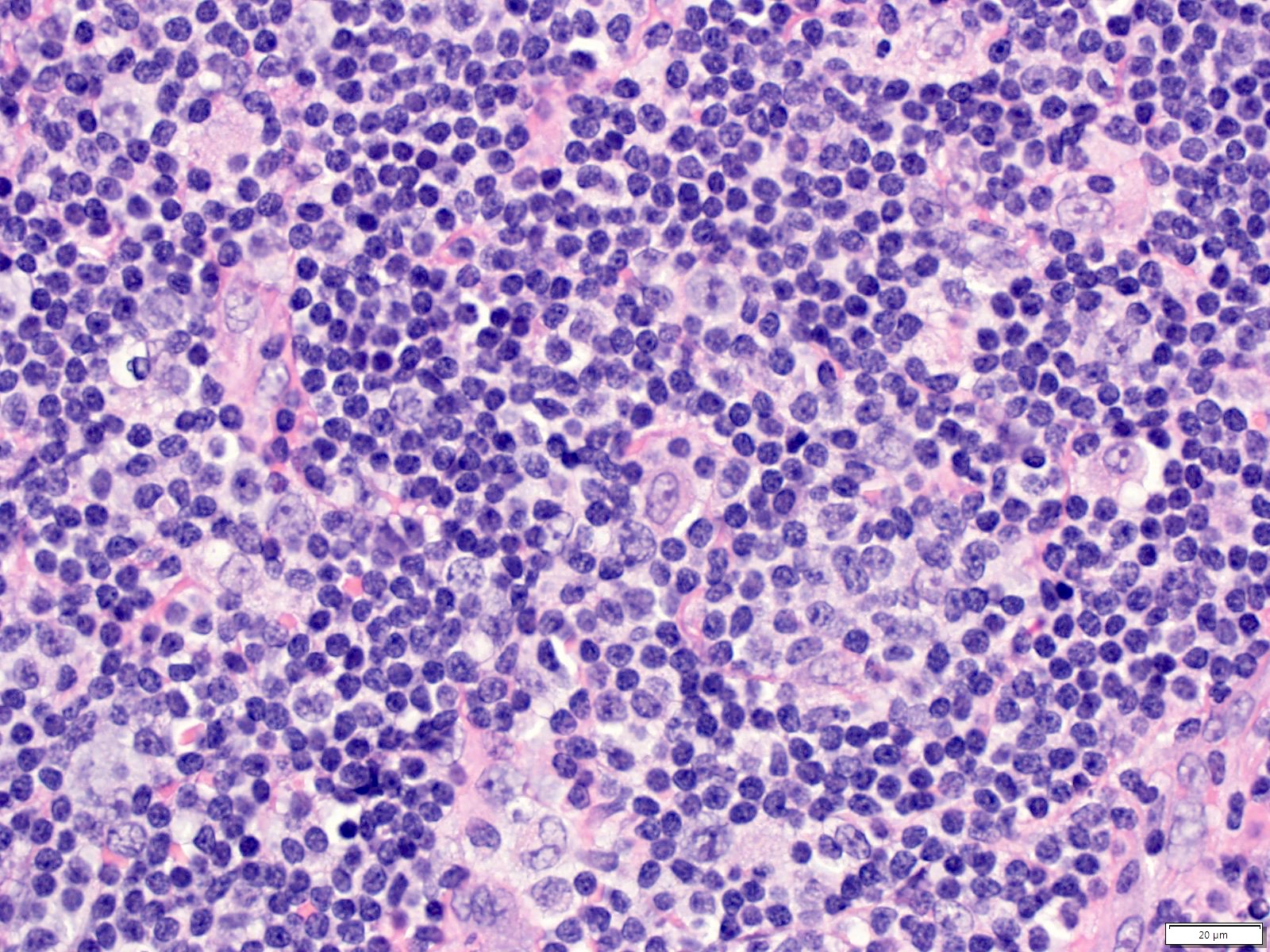
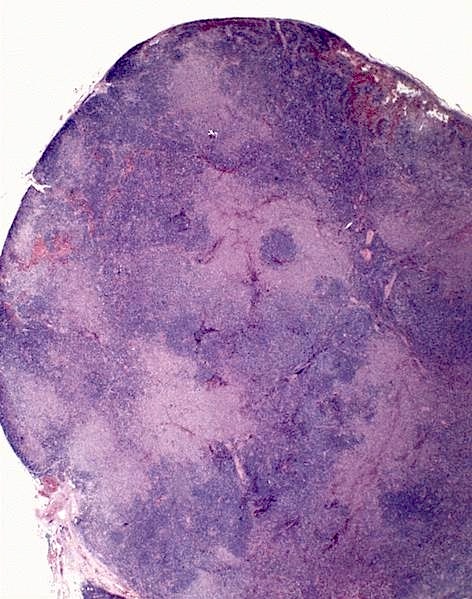
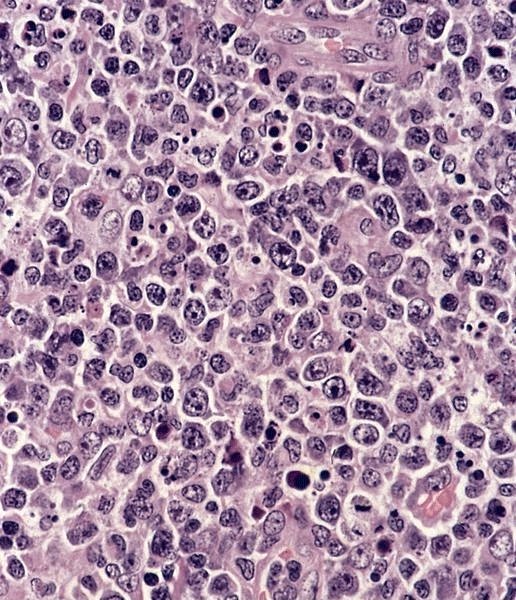
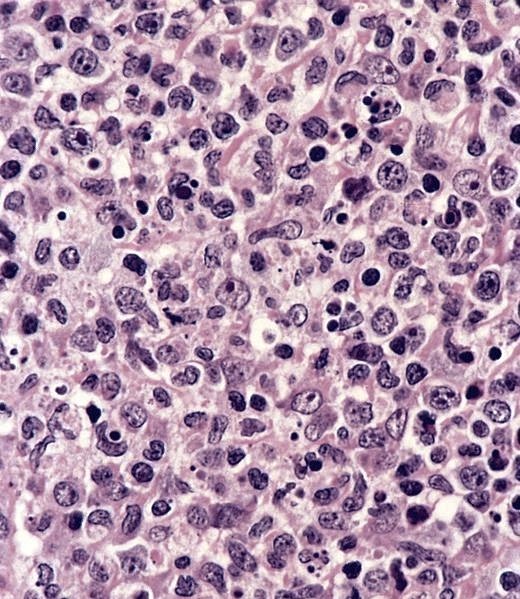
- Partial or complete lymph node involvement by irregularly shaped, pale areas composed of histiocytes, plasmacytoid dendritic cells, eosinophilic granular material and abundant karyorrhectic debris (nuclear dust), often surrounding a central zone of overt necrosis
- Karyorrhectic areas may extend beyond nodal capsule or involve residual germinal centers
- Regions between pale areas include small lymphocytes admixed with immunoblasts and clusters of plasmacytoid dendritic cells, causing a mottled or starry sky appearance
- Histiocytes include phagocytic cells with eosinophilic cytoplasm and crescent shaped nuclei (crescentic histiocytes) and nonphagocytic cells with twisted or reniform nuclei (Am J Surg Pathol 1994;18:219)
- Plasmacytoid dendritic cells are intermediate in size with amphophilic cytoplasm, round nuclei, small nucleoli; difficult to recognize on H&E (Diagn Cytopathol 2010;38:521)
- No neutrophils; rare to absent plasma cells (Clin Rheumatol 2007;26:50)
- Overt necrosis not required for diagnosis (Am J Surg Pathol 1994;18:219)
- 3 stages described based on histology (Am J Surg Pathol 1995;19:798, Pathol Int 2004;54:237):
- Proliferative: proliferation of plasmacytoid dendritic cells, immunoblasts and histiocytes
- Necrotizing: areas of necrosis with karyorrhectic debris
- Xanthomatous: foamy histiocytes predominate; may represent histologic variant
Microscopic (histologic) images
Contributed by Elizabeth Courville, M.D. and Amy Beckman, M.D.
Lymph node from a 38 year old woman:
Cervical lymph node from a 40 year old woman:
AFIP images
Virtual slides
Cytology description
- Phagocytic histiocytes with peripheral nuclei; plasmacytoid dendritic cells
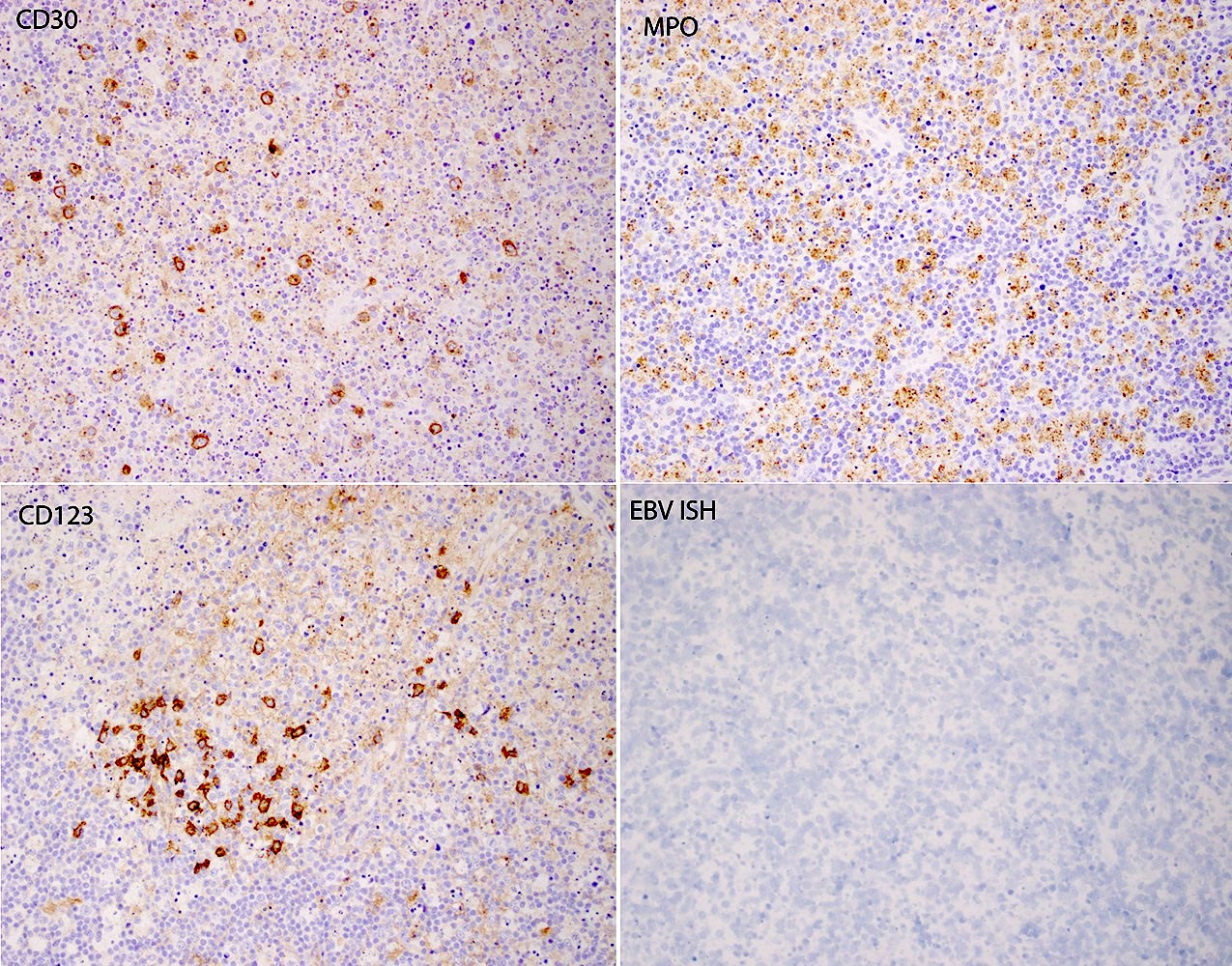
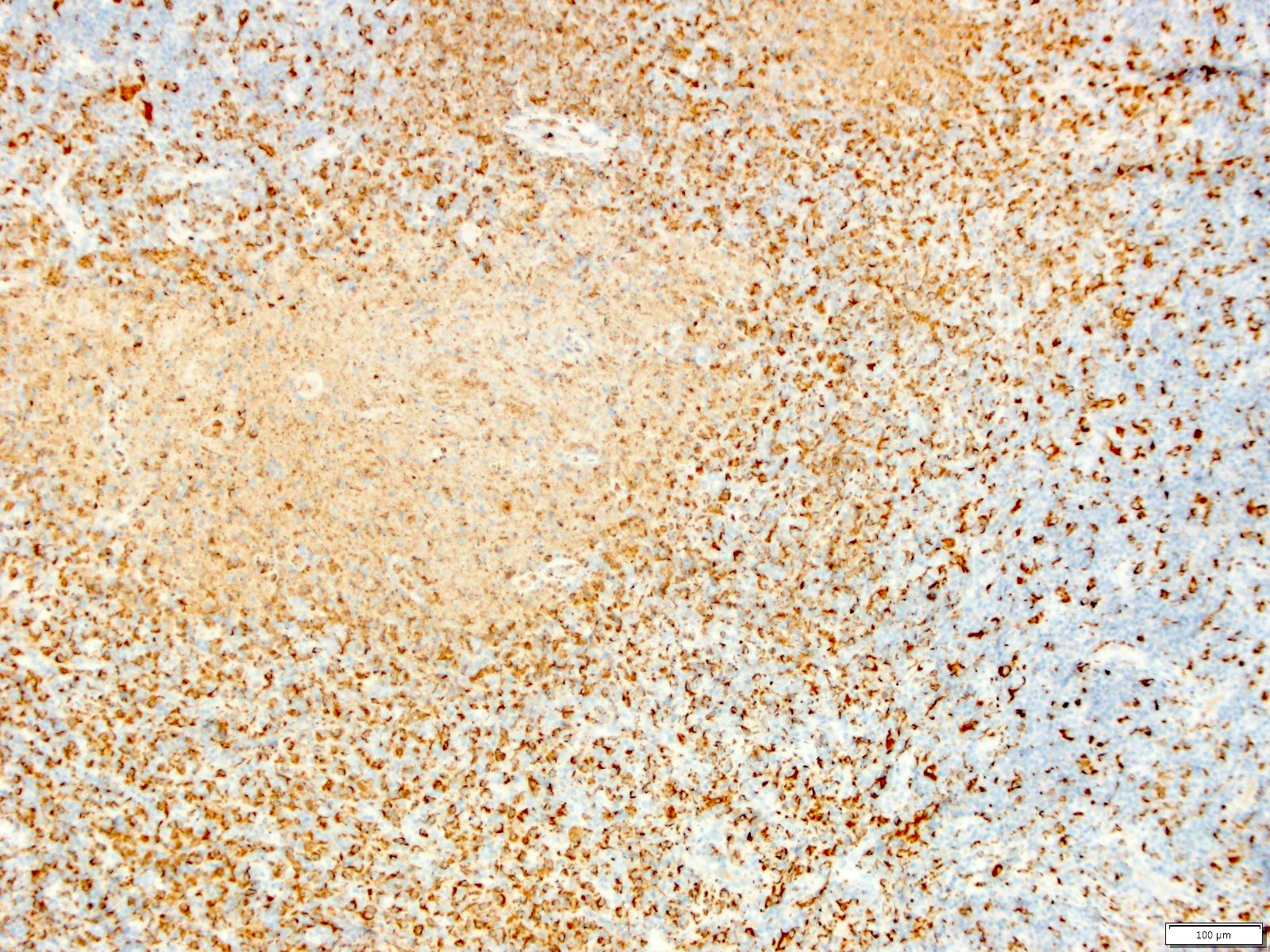
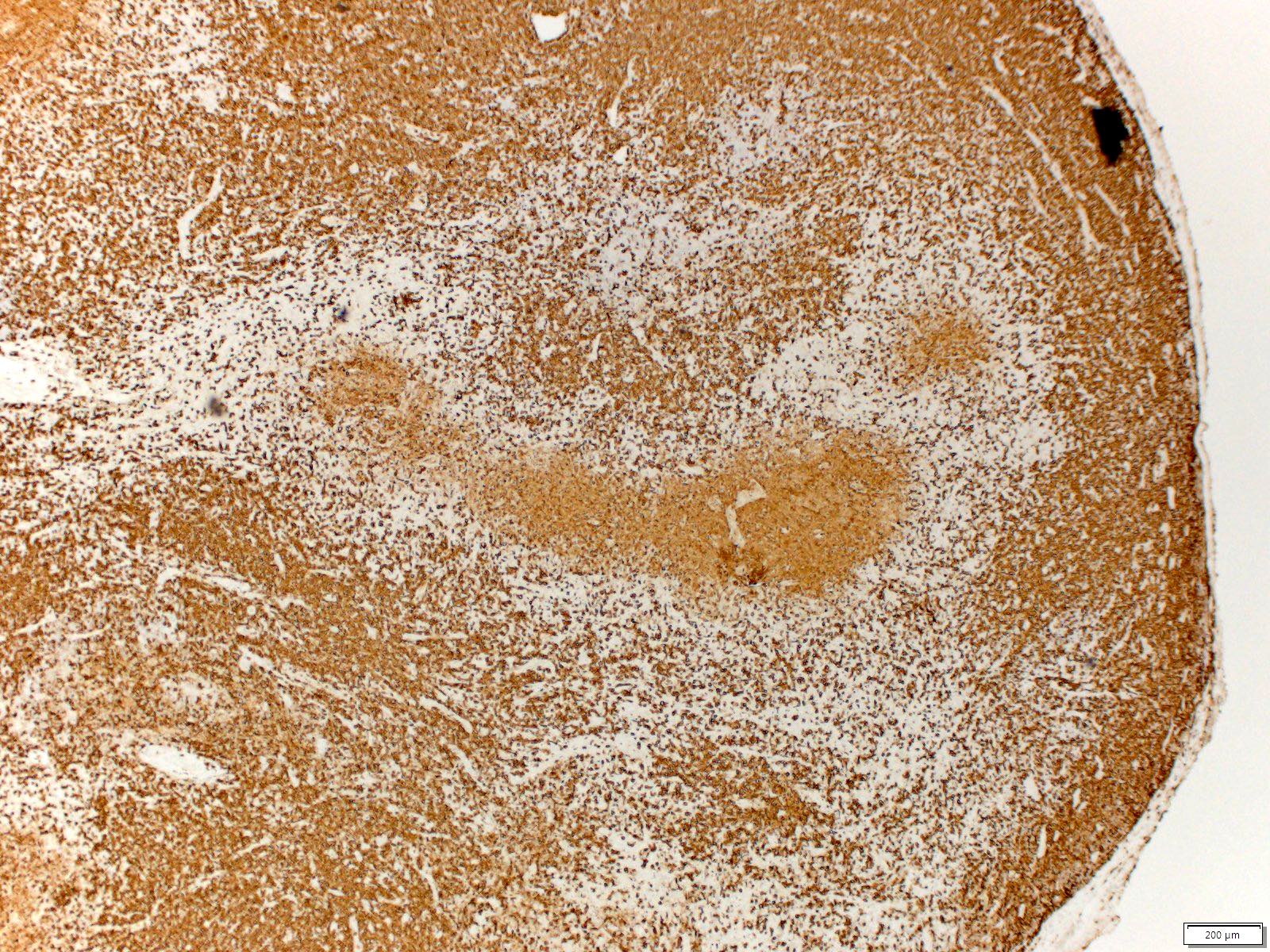
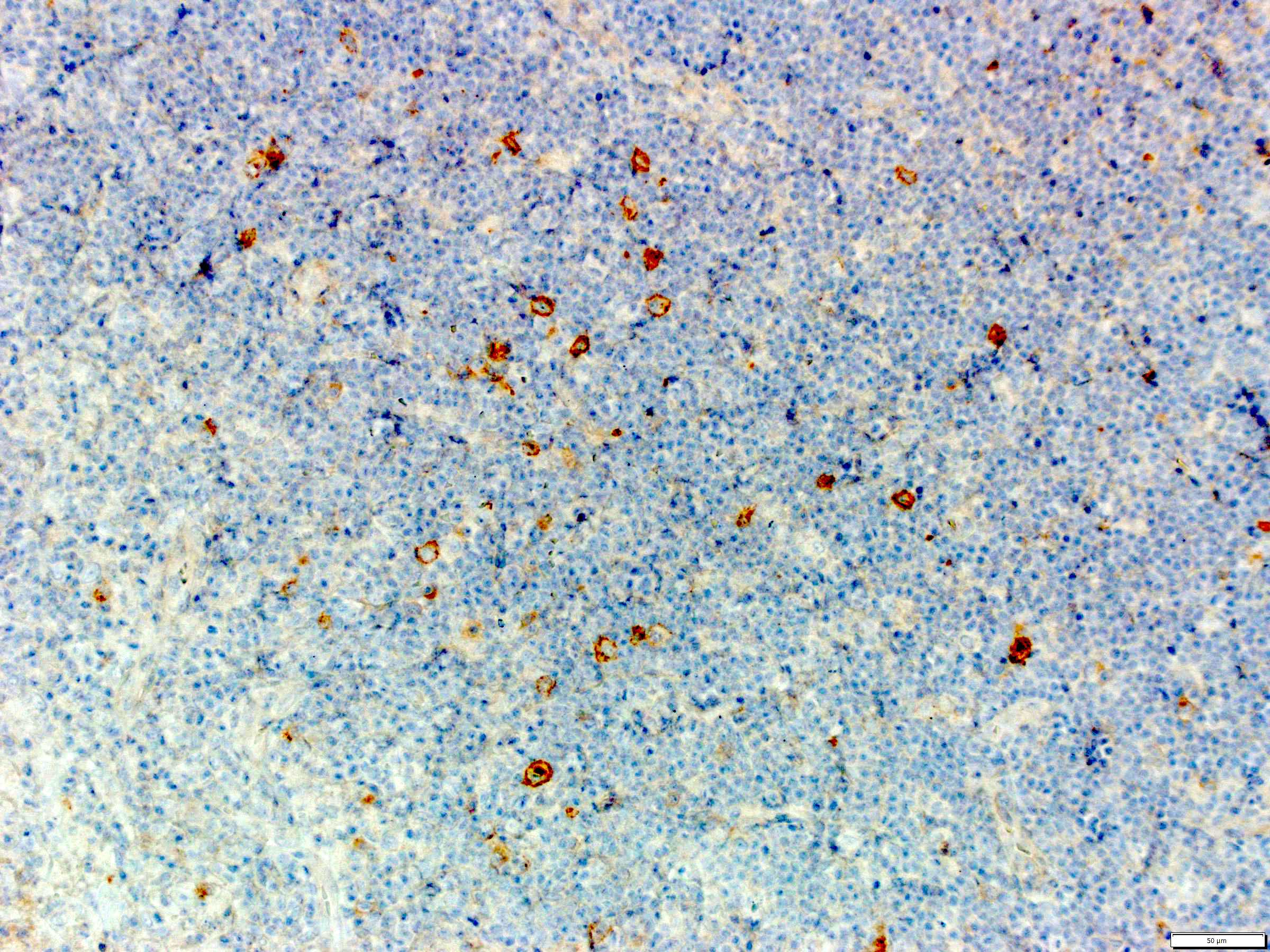
Positive stains
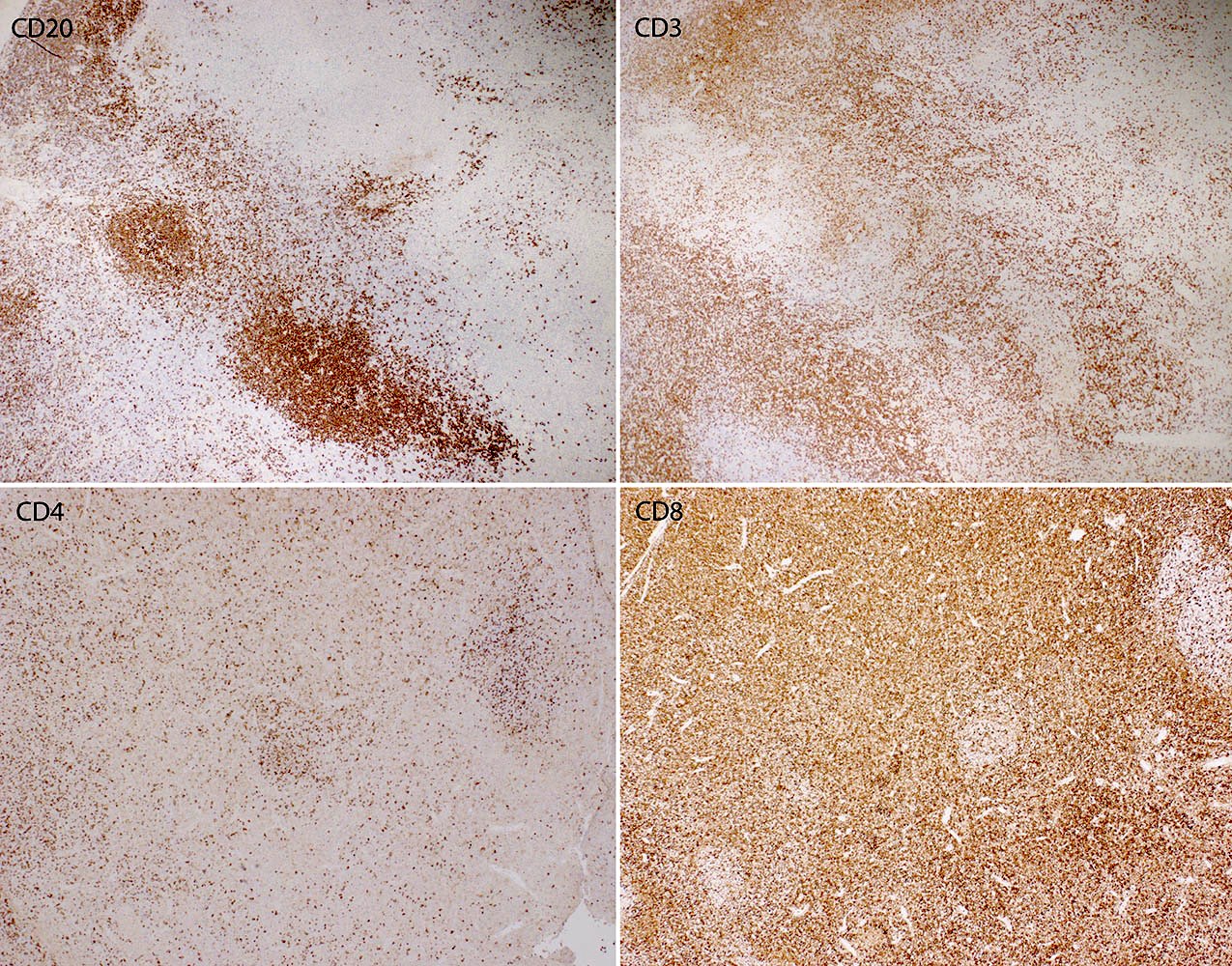
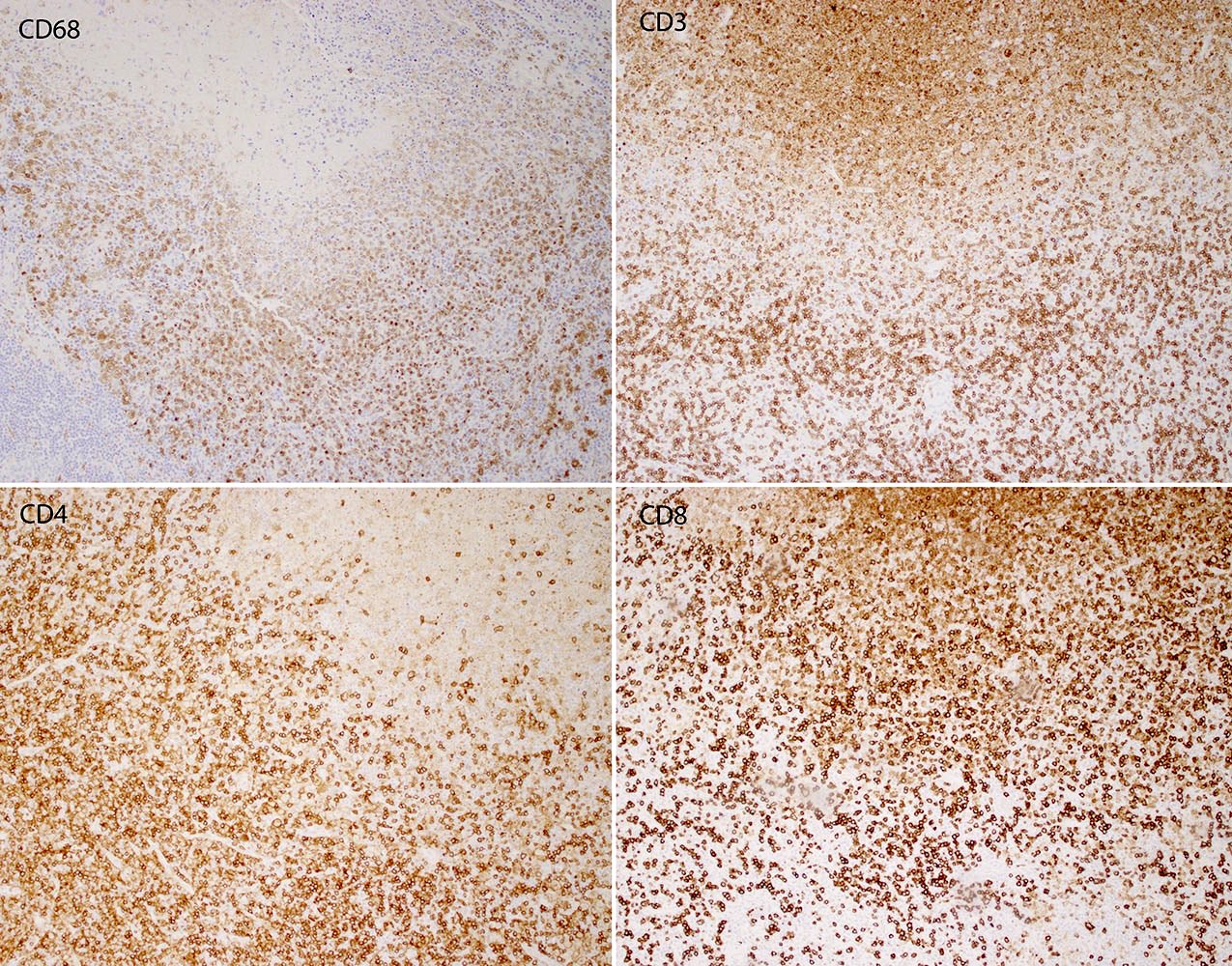
- CD3, CD4, CD8 highlight abundant T cells; CD8+ T cells > CD4+ T cells
- Lysozyme, CD4 (weak) are positive in histiocytes
- CD4 (weak), CD123 (bright) and TCL1 highlight plasmacytoid dendritic cells (Diagn Cytopathol 2010;38:521)
- CD20 stains B cells present in uninvolved areas but absent from karyorrhectic areas
- Myeloperoxidase: may stain histiocytes; emphasizes absence of granulocytes / neutrophils
Negative stains
- Fite acid fast stain, Gomori methenamine silver (GMS)
- HSV, CMV, in situ hybridization for EBV encoded RNA (EBER ISH)
- Reference: Arch Pathol Lab Med 2018;142:1341
Electron microscopy description
- Tubuloreticular structures present in cytoplasm of immunoblasts, endothelial cells and histiocytoid cells (Am J Pathol 1982;107:292)
- Cells at various stages of apoptosis; histiocytes containing phagocytosed karyorrhectic debris / apoptotic bodies (Acta Otolaryngol Suppl 1998;538:250, Acta Pathol Jpn 1993;43:635)
Electron microscopy images
Sample pathology report
- Lymph node, cervical, excision:
- Necrotizing lymphadenitis (see comment)
- Comment: The findings favor a diagnosis of Kikuchi disease, a benign and typically self limited lymphadenitis. There is no evidence of lymphoma. Histologically, changes associated with autoimmune disease may mimic those seen in Kikuchi disease. Clinical correlation, along with evaluation for a possible autoimmune disease, such as systemic lupus erythematosus, is recommended.
- Microscopic description: H&E stained sections show a lymph node with architecture distorted by pale areas composed of eosinophilic, granular material, karyorrhectic debris and interspersed lymphocytes and histiocytes. These areas are surrounded by histiocytic cells (some with twisted nuclei and others with so called crescentic nuclei) and cells with morphology suggestive of plasmacytoid dendritic cells. Outside the pale areas, there is an expansion of small lymphocytes admixed with immunoblasts. Residual primary and secondary follicles are present but neutrophils are not seen and plasma cells are rare to absent. Neither hematoxylin bodies nor aggregates of large atypical lymphocytes are identified. Immunohistochemical stains are performed with appropriate controls. CD3 highlights numerous T cells; CD8 positive cells outnumber CD4 positive cells. CD20 stains residual nodules of B cells. CD68 stains histiocytes within and adjacent to karyorrhectic areas. CD123 highlights plasmacytoid dendritic cells, which surround and form clusters outside of karyorrhectic areas. CD4 shows weak staining in both histiocytes and plasmacytoid dendritic cells.
Differential diagnosis
- Lupus lymphadenitis:
- Infectious lymphadenitis:
- Neutrophils, granulomatous inflammation, viral cytopathic changes
- Lymphoma (e.g., diffuse large B cell lymphoma, peripheral T cell lymphoma, NOS, Hodgkin lymphoma):
- Nodal effacement by monotonous or atypical lymphocytes or presence of Reed-Sternberg / Hodgkin cells
- Pattern of staining seen with a panel of immunohistochemical stains (for example, CD3, CD20, CD30, PAX5) and interpreted in the context of morphology on routine hematoxylin and eosin stain is important in making the distinction from Kikuchi disease
Additional references
Board review style question #1
Which disease shows similar morphologic and immunohistochemical features to Kikuchi lymphadenitis?
- Classic Hodgkin lymphoma
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Toxoplasmosis
Board review style answer #1
Board review style question #2
Board review style answer #2