Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Peripheral smear description | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Janowiak K, Ewton A, Ravindran A, Okoye E. ALK+ histiocytosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodesalkhistiocytosis.html. Accessed January 10th, 2025.
Definition / general
- ALK positive histiocytosis (APH) is a histiocytic neoplasm characterized by ALK (anaplastic lymphoma kinase) gene rearrangements and ALK immunoreactivity in the lesional histiocytes (Leukemia 2022;36:1703, Blood 2022;140:1229, Blood 2022;139:256)
- Initially described in 2008 presenting as systemic histiocytosis in infants (Blood 2008;112:2965)
Essential features
- Rare non-Langerhans cell histiocytic neoplasm with heterogeneous clinical features, presenting as single system disease, multisystem with systemic hematopoietic involvement (liver, spleen or marrow, skin, central nervous system [CNS]) or other multisystem disease (tumorous involvement of ≥ 2 organ systems)
- ALK expression by immunohistochemistry, predominantly in a cytoplasmic pattern, rarely in a membranous or Golgi (dot-like) pattern and practically never in a nuclear pattern
- Cytoplasmic ALK expression by immunohistochemistry with coexpression of histiocytic markers (CD68, CD163, CD4) is crucial to distinguish this entity from other histiocytic or spindle cell morphologic mimics
- Characteristic ALK gene rearrangements allow for targeted therapy with ALK inhibitors
Terminology
- ALK related histiocytosis
- ALK rearranged histiocytosis
ICD coding
- ICD-10: D76.3 - other histiocytosis syndromes
Epidemiology
- Affects any age group, including children and young adults, with a female predilection (Blood 2022;139:256)
Sites
- Multisystem with systemic hematopoietic involvement
- Systemic involvement of liver, spleen or bone marrow with or without involvement of additional sites (Blood 2022;139:256, Leukemia 2022;36:1720)
- Multisystem disease, others
- ≥ 2 organs, most commonly central and peripheral nervous system, bone, lung and skin (Leukemia 2022;36:1720, Blood 2022;139:256)
- Single system disease
- Tumorous involvement of a single organ with solitary or multiple lesions
- Most common sites include central and peripheral nervous system, skin, soft tissue and breast (Blood 2022;139:256)
Pathophysiology
- Fusion of the receptor tyrosine kinase domain of the ALK gene, most commonly to exon 24 of KIF5B, results in constitutive activation of downstream signaling, including RAS-RAF-MEK-ERK (MAPK) and PI3K / AKT / mTOR signaling pathways
- MAPK pathway activation leads to phosphorylation of downstream ERK, ultimately resulting in transcription of various effector genes, including the gene encoding for cyclin D1 (CCND1); translation of CCND1 messenger RNA to the cyclin D1 protein is mTOR dependent (Blood 2022;139:256)
Etiology
- Unknown at this time
Clinical features
- Diverse clinical presentations depending on site(s) of involvement
- Infants with multisystem disease involving the hematopoietic system present with hepatomegaly, anemia and thrombocytopenia, often accompanied by splenomegaly and coagulopathy
- Other multisystem and single system disease presents with varying mass effects depending on tumor size and location (Blood 2022;139:256)
- Neurologic involvement may present with headache, nausea / vomiting, ataxia, paresis, seizure, diplopia or trigeminal neuralgia
- Pulmonary involvement may present with dry cough or respiratory dysfunction requiring oxygen therapy
- Liver involvement may present with jaundice, coagulopathy or fever
- Cutaneous lesions present as slowly growing papules or nodules
Diagnosis
- Comprehensive patient evaluation including clinical history, physical examination and imaging studies
- Coexpression of histiocytic markers and ALK should prompt molecular confirmation of ALK gene rearrangement either by RNA sequencing or by FISH (fluorescence in situ hybridization) analysis
- References: Mod Pathol 2019;32:598, Blood 2022;139:256
Laboratory
- Variable, depending on organ system(s) involved
- Liver involvement can be associated with elevated liver enzymes, elevated bilirubin and low fibrinogen (Blood 2022;139:256)
- Hematopoietic involvement can be associated with anemia, thrombocytopenia and prolonged prothrombin time and activated partial thromboplastin time (Blood 2022;139:256)
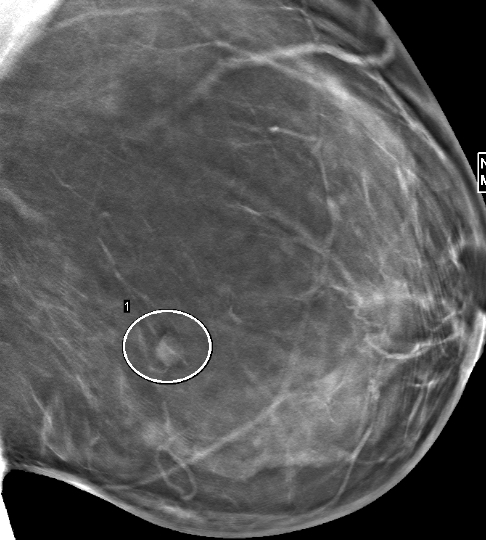
Radiology description
- Mass lesions can be identified by ultrasound, Xray, magnetic resonance imaging (MRI), computed tomography (CT), positron emission tomography (PET) CT and other imaging modalities (Blood 2022;139:256)
- Liver, pancreas, long bone lesions appear hypermetabolic on PET CT imaging
- Liver and thyroid lesions appear hypoechoic on ultrasound
- Kidney tumors appear hypodense on CT imaging
- Tumors of the vertebral bodies and liver appear hyperintense by T2 weighted MRI
- CNS tumors rarely can mimic meningioma on MRI (Radiol Case Rep 2023;18:2259)
Radiology images
Prognostic factors
- Prognosis depends on extent of disease and location(s) of tumor(s)
- Typically favorable outcomes in cases with single system disease
- Reports of death due to multisystem disease progression include every age group (Mod Pathol 2019;32:598, Blood 2022;139:256, JCO Precis Oncol 2021;5:PO.20.00383)
Case reports
- 17 month old boy with a 5.1 cm intracranial mass, multiple nodules in the liver and bilateral lungs, as well as multiple skin papules (Orphanet J Rare Dis 2023;18:53)
- 27 year old man with a 1.5 cm intradural extramedullary enhancing lesion (Turk Patoloji Derg 2021;37:172)
- 30 year old man with cavernous sinus lesion mimicking meningioma (Radiol Case Rep 2023;18:2259)
- 38 year old woman with multiple unilateral breast lesions (Int J Surg Case Rep 2022;97:107435)
- 50 year old woman with appendiceal nodule (Haematologica 2019;104:e534)
- 51 year old woman with lesions identified in the right lung, central nervous system and iliac lymph nodes (Ann Palliat Med 2021;10:10095)
Treatment
- Management varies depending on extent of disease and site(s) of involvement
- Surgical resection is often definitive treatment for single system disease (Blood 2022;139:256)
- Systemic therapy for incompletely resected or unresectable tumors and for multisystem disease includes steroids, intravenous immune globulin (IVIG) or chemotherapy
- Targeted therapy with ALK inhibitors has been used as first or second line treatment in a majority of cases (Blood 2022;139:256, JCO Precis Oncol 2021;5:PO.20.00383, Oncologist 2017;22:1444)
- ALK inhibitors include alectinib, loratinib, brigatinib, crizotinib, ceritinib and entrectinib
- Used as monotherapy or in combination with other treatment modalities
- Rare cases have resulted in spontaneous regression (Blood 2022;139:256)
Gross description
- Tumors may be well circumscribed or ill defined with a tan, white or yellow cut surface
Microscopic (histologic) description
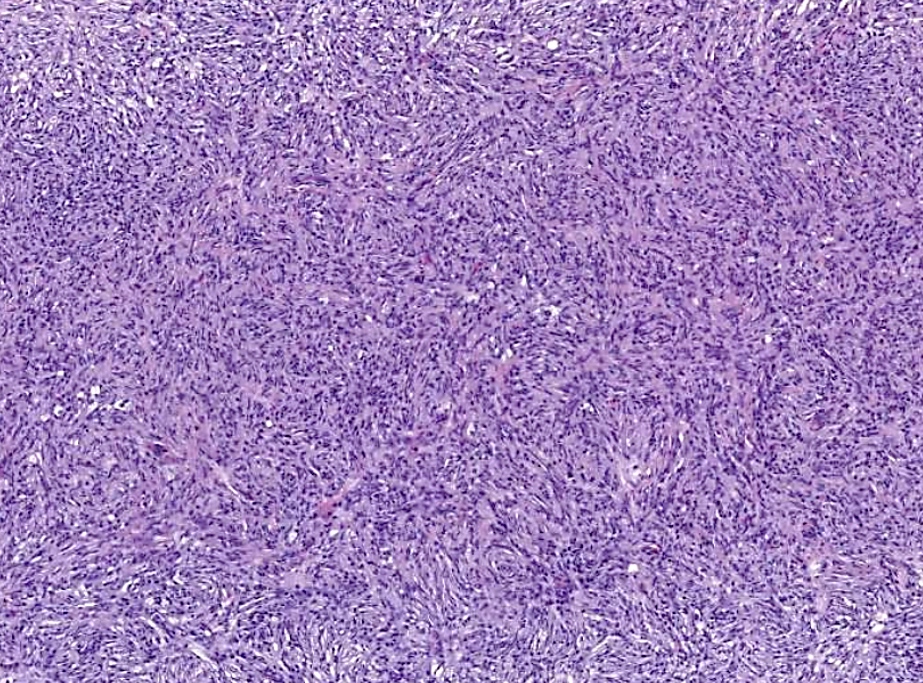
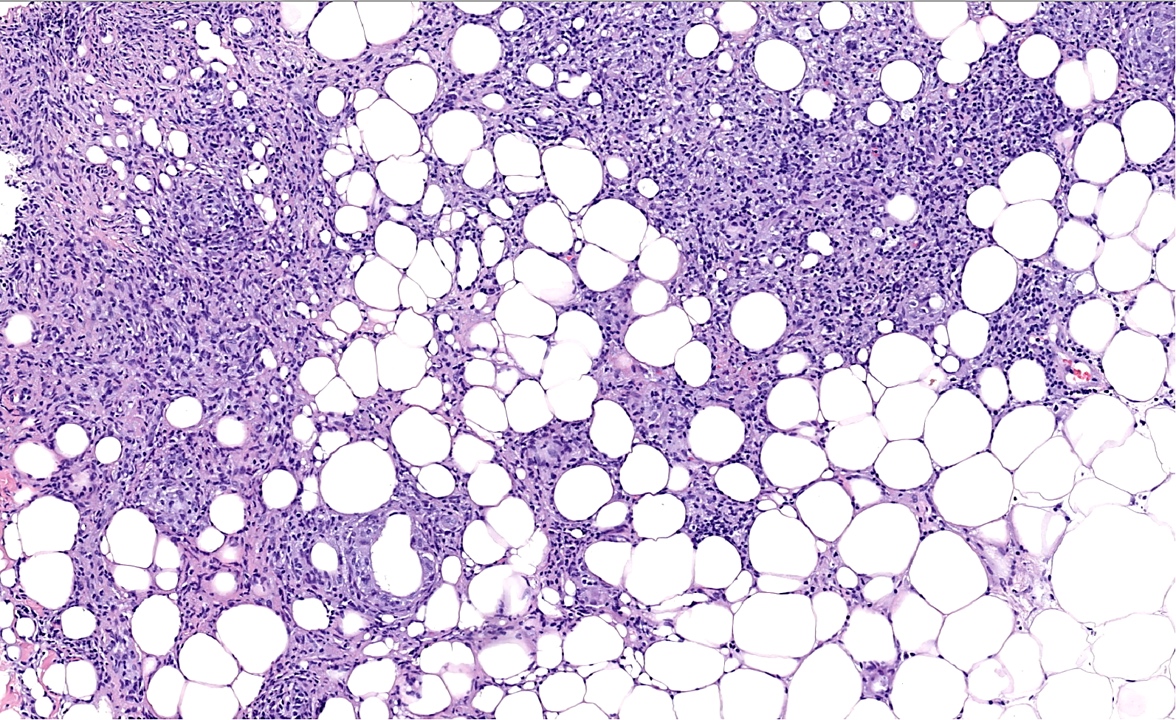
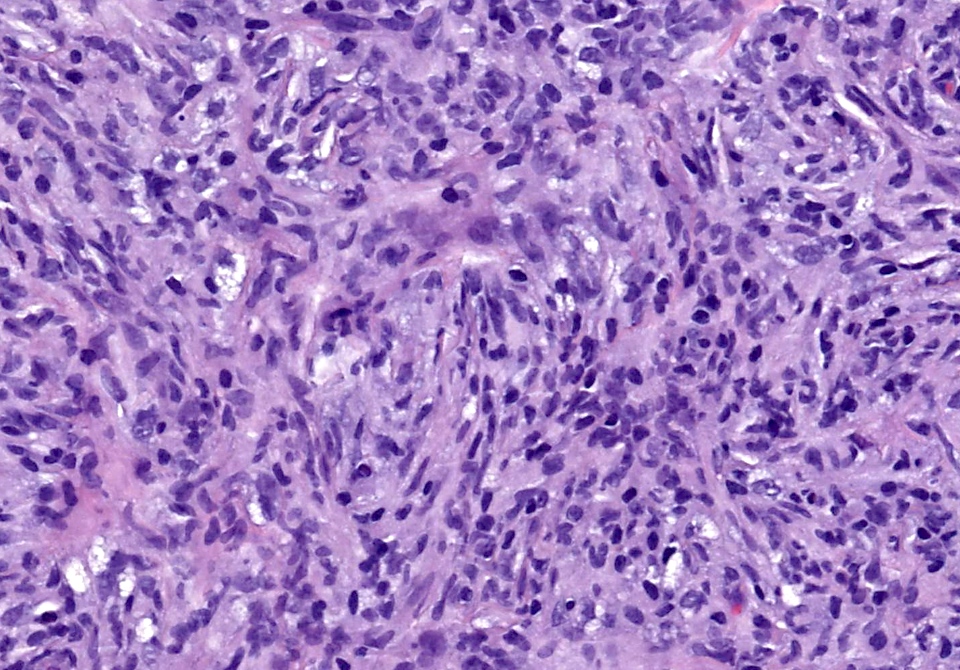
- Large oval (epithelioid), foamy or spindle cells in varying proportions without significant nuclear atypia and abundant eosinophilic cytoplasm (Mod Pathol 2019;32:598, Blood 2022;139:256)
- Large histiocytes may show irregular nuclear contours (indentation, folding, clefting, lobulation) with fine chromatin and small nucleoli (Mod Pathol 2019;32:598, Blood 2022;139:256)
- Occasional multinucleated cells, including Touton giant cells, may be present (Mod Pathol 2019;32:598, Blood 2022;139:256)
- Emperipolesis, characterized by engulfment of inflammatory cells (similar to Rosai-Dorfman disease), may be observed (Mod Pathol 2019;32:598, Blood 2022;139:256)
- Hepatic involvement may show coalescing histiocytes indistinguishable from hepatocytes (Mod Pathol 2019;32:598)
- Bone marrow infiltration may vary from focal to extensive involvement (Mod Pathol 2019;32:598)
- Skin lesions are often noncircumscribed, nonepidermotropic infiltrates composed of sheets of histiocytes with varying degree of fibrosis (Mod Pathol 2019;32:598)
- Fascicular and storiform growth patterns common in breast tumors (Am J Surg Pathol 2021;45:347)
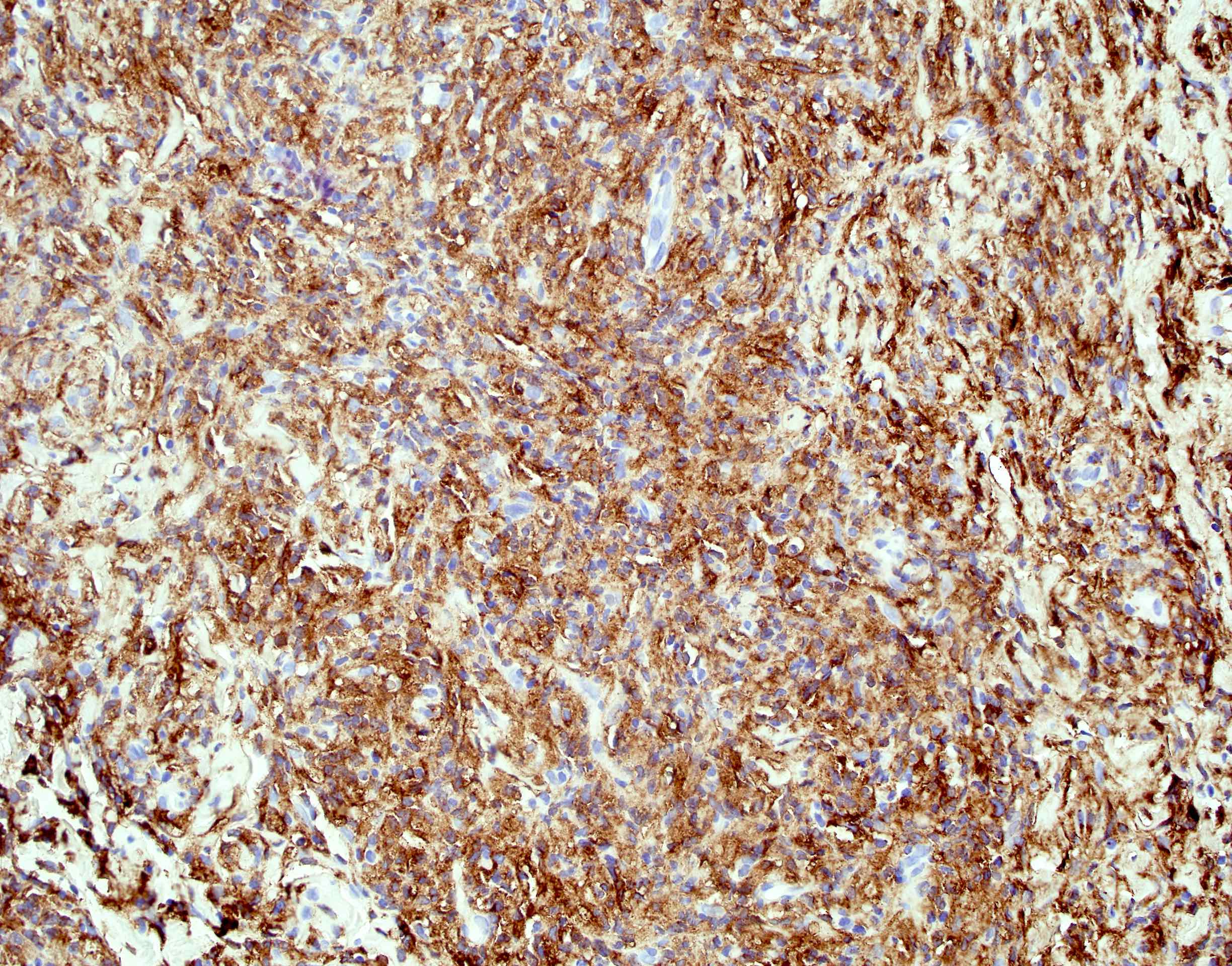
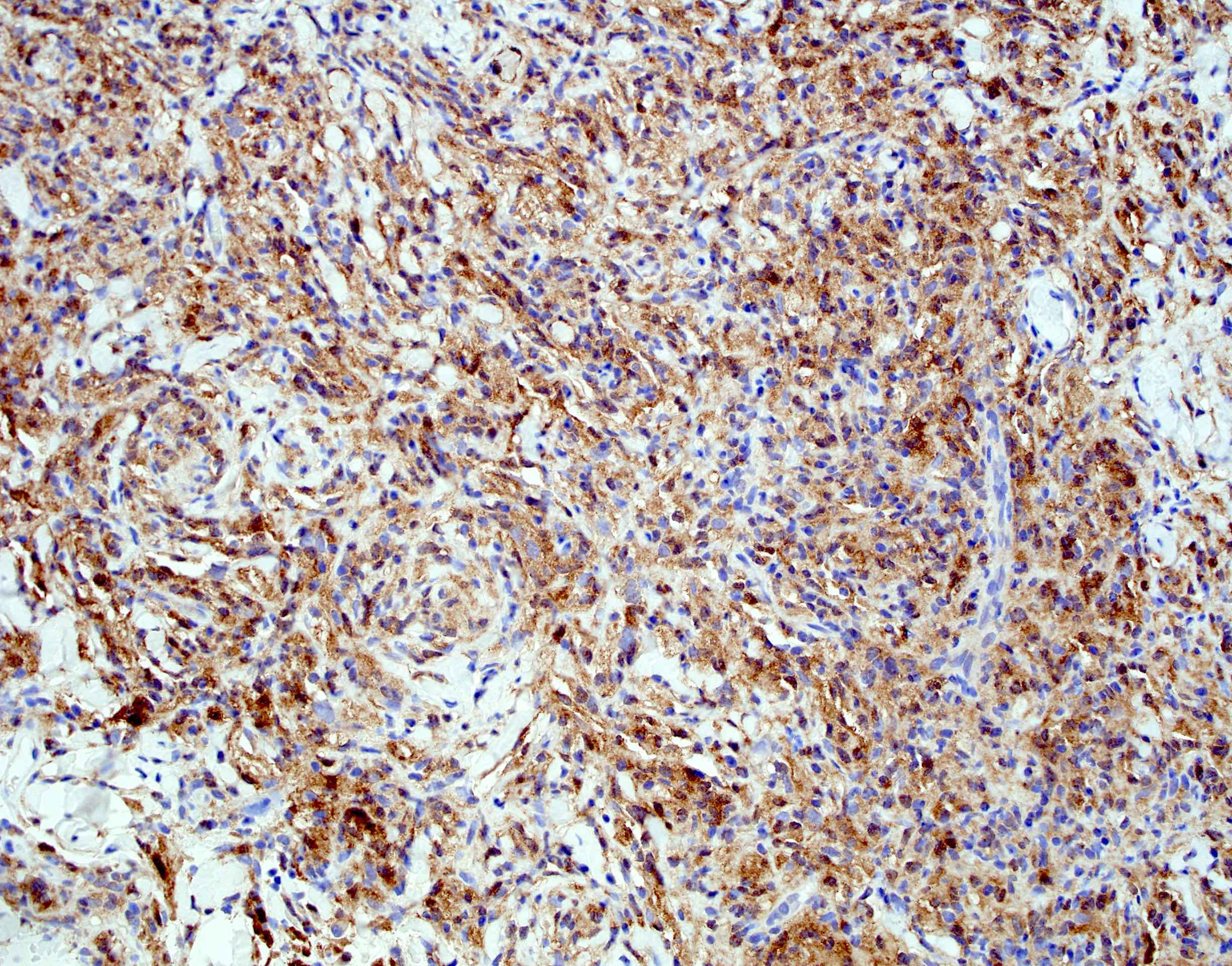
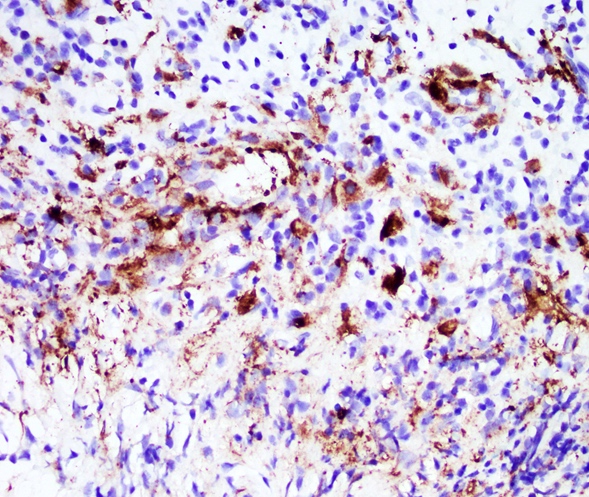
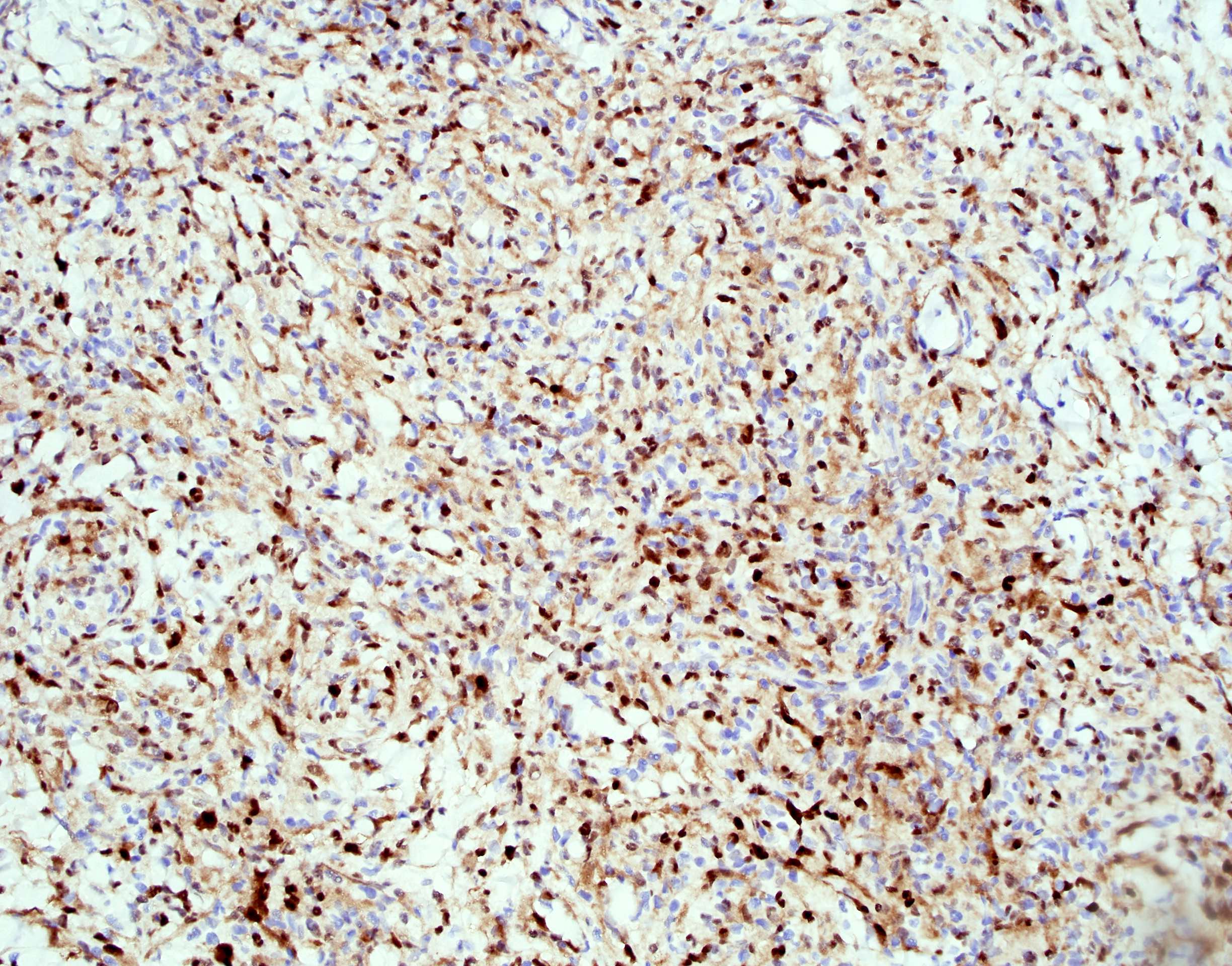
Microscopic (histologic) images
Peripheral smear description
- In systemic cases with hematopoietic involvement, anemia, thrombocytopenia and leukocytosis are usually seen
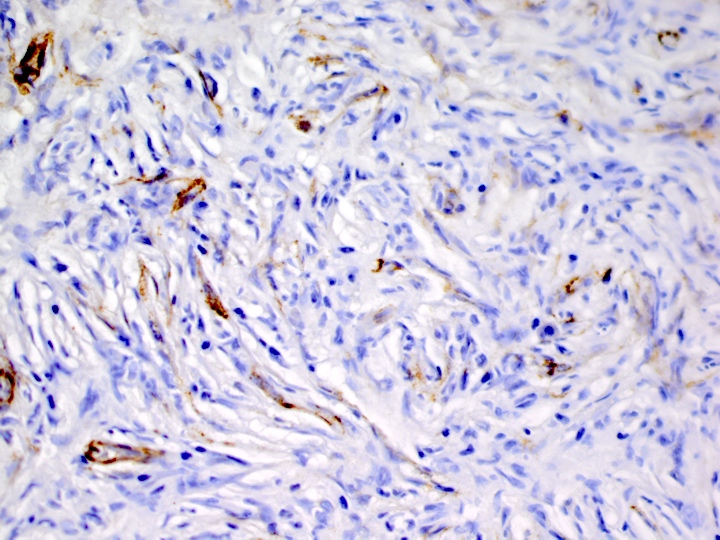
Positive stains
- ALK
- Cytoplasmic staining most common; occasionally membranous or dot-like Golgi pattern
- Lacks nuclear expression
- Can be weak or focal
- CD163, CD68, CD14, CD4, lysozyme
- Factor XIIIa, fascin, cyclin D1 (Am J Clin Pathol 2023;160:1)
- Some cases show positivity for S100 and OCT2, mimicking Rosai-Dorfman disease (Blood 2008;112:2965, Am J Clin Pathol 2023;160:1)
- pERK expression as a consequence of MAPK pathway activation
Negative stains
Molecular / cytogenetics description
- ALK rearrangements detected by FISH
- ALK fusion partners identified via targeted RNA sequencing (Blood 2022;139:256)
- Most common: KIF5B::ALK fusion (~70 - 75% of cases)
- Other fusion partners reported: CLTC, TPM3, TFG, EML4, DCTN1, TRIM33, COL1A2
Sample pathology report
- Left breast mass, lumpectomy:
- ALK positive histiocytosis, 9 mm in greatest dimension (see comment)
- Comment: Lesional histiocytes are characterized by cytoplasmic expression of ALK with coexpression of histiocytic markers (CD68, CD163) and cyclin D1. Molecular analysis by RNA sequencing was positive for KIF5B::ALK fusion. The overall immunophenotype in conjunction with the molecular analysis supports the above diagnosis.
Differential diagnosis
- Reactive fibrohistiocytic proliferation:
- Rosai-Dorfman disease (RDD):
- Parenchymal effacement of nodal / extranodal tissue by large histiocytes with round / oval nuclei, pale chromatin, distinct nucleoli and abundant pale cytoplasm with frequent engulfment of inflammatory cells (emperipolesis)
- Abundant plasma cells and small lymphocytes; occasionally, neutrophils may also be present
- By immunohistochemistry, positive for S100, OCT2; uniformly negative for ALK
- ~10% of cases are negative for CD163 (Am J Clin Pathol 2023;160:1)
- Lacks ALK gene fusions
- Juvenile xanthogranuloma (JXG):
- Usually affects pediatric population with ~33% of cases presenting within the first year of life
- Predominantly cutaneous involvement presenting as papulonodular lesions and usually asymptomatic / self resolving over months / years
- < 5% may be systemic JXG, including CNS that may present as seizures, hydrocephalus, diabetes insipidus; bone marrow involvement presents with cytopenias
- Nonencapsulated circumscribed lesions composed of large xanthomatous (foamy) histiocytes with bland nuclear features and Touton giant cells; occasionally lesions may be composed of spindled, epithelioid or oncocytic histiocytes
- Typically has an inflammatory background with a mixed population of lymphocytes, eosinophils, plasma cells, neutrophils and mast cells
- IHC negative for ALK
- Lacks ALK gene fusions
- Erdheim-Chester disease:
- Heterogeneous clinical manifestations, most commonly presenting with bone pain, secondary to bilateral symmetric osteosclerosis of metadiaphysis of femur, tibia and fibula
- Bland appearing histiocytes characterized by abundant foamy (xanthomatous) cytoplasm with surrounding fibrosis (Mod Pathol 2018;31:581)
- Negative for OCT2 and ALK (Am J Surg Pathol 2021;45:35, Am J Clin Pathol 2023;160:1)
- Associated with MAPK pathway mutations, with BRAF V600E mutated in ~50 - 60% of cases
- Lacks ALK gene fusions
- Langerhans cell histiocytosis:
- Langerhans cells characterized by irregular, grooved, folded or indented nuclei with fine chromatin, inconspicuous nucleoli and abundant pale eosinophilic cytoplasm
- Positive for S100, CD1a and langerin; negative for factor XIIIa and ALK (Am J Clin Pathol 2023;160:1)
- Lacks ALK gene fusions
- Inflammatory myofibroblastic tumor (especially breast and soft tissue tumors):
- Proliferation of ALK positive spindle cells of myofibroblastic origin with variable prominent lymphoplasmacytic infiltrates
- Lesional cells are positive for vimentin (diffuse, strong), smooth muscle actin, muscle specific actin, calponin and desmin (variable)
- CD68 / CD163 positive histiocytes may be present in the background but are not the lesional cells
Additional references
- WHO Classification of Tumours Editorial Board: Haematolymphoid Tumours, 5th Edition, 2024, BMJ Case Rep 2018;2018:bcr2018224506, Acta Neuropathol 2019;138:335, Neuropathol Appl Neurobiol 2021;47:878, Leuk Lymphoma 2021;62:1234, J Breast Imaging 2022;4:336, J Hematopathol 2021;14:89, Hum Pathol Case Rep 2021;24:200504, Hum Pathol Case Rep 2020;21:200404
Board review style question #1
A 41 year old woman underwent a core needle biopsy for a 3 cm breast mass discovered on her first screening mammogram. The lesional spindle cells show the CD68 immunostaining pattern seen above; they are also positive for ALK and negative for SMA and desmin. Which of the following is the most likely diagnosis?
- ALK positive histiocytosis
- Erdheim-Chester disease
- Extranodal Rosai-Dorfman disease
- Inflammatory myofibroblastic tumor
- Juvenile xanthogranuloma
Board review style answer #1
A. ALK positive histiocytosis (APH) can occur as a localized mass in many anatomic locations or as multisystem disease. Morphologic features vary and may include spindled, epithelioid or foamy histiocytes with or without background lymphoplasmacytic infiltrate. Lesional histiocytes show positive immunostaining for at least 1 histiocytic marker (CD68, CD163, etc.) and for ALK. Answers B, C and E are incorrect because the lesional histiocytes in each of these lesions do not show positive immunostaining for ALK. Answer D is incorrect because the neoplastic spindle cells in inflammatory myofibroblastic tumor (IMT) are myofibroblastic in origin and are therefore positive for SMA and desmin and negative for CD68.
Comment Here
Reference: ALK+ histiocytosis
Comment Here
Reference: ALK+ histiocytosis