Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Aljuaid R, Tsang P. Progressive transformation of germinal centers. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodesPTGC.html. Accessed March 30th, 2025.
Definition / general
- Progressive transformation of germinal centers (PTGC) is a clinicopathologic entity characterized by chronic lymphadenopathy with a wide age distribution
- Characterized by enlarged nodal lymphoid follicles with ingress of mantle zone B cells into the germinal centers (Arch Otolaryngol Head Neck Surg 2006;132:797)
- Nonspecific manifestation of a variety of associated conditions, including immune and autoimmune disorders
- Associated with previous, concurrent or subsequent lymphoma, particularly nodular lymphocyte predominant Hodgkin lymphoma (NLPHL), in a small proportion of patients; less frequently with classic Hodgkin lymphoma (J Clin Exp Hematop 2014;54:205)
Essential features
- Common differential diagnosis of persistent reactive lymphadenopathy, especially in adolescent boys (Pediatr Blood Cancer 2022;69:e29638)
- Expansile lymphoid follicles with mantle zone B cells expanding into and disrupting the germinal centers in a hyperplastic lymph node (Pediatr Blood Cancer 2022;69:e29638)
- Not a premalignant condition; may occur prior to, concurrent with or following Hodgkin lymphoma, most commonly NLPHL (Int J Pediatr Otorhinolaryngol 2002;65:195)
- Associated with immune and autoimmune conditions in some patients
Terminology
- Progressive transformation of germinal centers
- Follicle lysis: follicle centers fractured by ingrowth of mantle cells
ICD coding
- ICD-10: R59.9 - enlarged lymph nodes, unspecified
Epidemiology
- M:F = 3:1 (Int J Pediatr Otorhinolaryngol 2002;65:195)
- Occurs in both adult and pediatric populations (Int J Pediatr Otorhinolaryngol 2002;65:195)
Sites
- Cervical lymph nodes: most commonly affected site (50%) (Pediatr Blood Cancer 2022;69:e29638)
- Inguinal (25%) and axillary (22%) lymph nodes also common (Pediatr Blood Cancer 2022;69:e29638)
- Abdominal lymph nodes infrequent (Int J Pediatr Otorhinolaryngol 2002;65:195)
Pathophysiology
- Nonspecific, likely multifactorial, representing a state of follicular hyperplasia following reactive stimuli (Case Rep Otolaryngol 2017;2017:5982168)
- Does not follow the typical progression of lymphoid follicular reaction (whereby germinal center reaction comes to an end, follicle regresses, reaction dissipates)
- However, there is somatic hypermutation, clonal expansion and selection, similar to usual hyperplastic germinal centers (Blood 2001;97:714)
- Instead, germinal center proceeds through morphologically distinct stages
- Germinal center becomes enlarged and mantle zone thickens
- Mantle zone B cells migrate into the germinal center, disrupting the follicular dendritic meshwork and fracturing the germinal center into irregular clusters of centrocytes and centroblasts (follicle lysis)
- Stromal microenvironment is distorted and the follicle becomes entirely overrun by mantle cells (Ann Diagn Pathol 2020;44:151421)
Etiology
- Unknown etiology; probably a nonspecific lymphoid reaction
- May represent an abnormal or unusual immune response to a variety of stimuli (Am J Surg Pathol 1992;16:252)
Clinical features
- Can present as an isolated lesion or as part of the presentation of systemic conditions (Pediatr Blood Cancer 2022;69:e29638)
- More commonly presents as slow growing lymphadenopathy with no constitutional symptoms (Semin Diagn Pathol 2023;40:371)
- May involve numerous lymph nodes in one region (Pediatr Blood Cancer 2022;69:e29638)
- Lymphadenopathy with constitutional symptoms should raise the suspicion of concurrent malignancy or other systemic disorders (Pediatr Blood Cancer 2022;69:e29638)
- Associated noncausally, most commonly with NLPHL, which may precede, follow or coincide with the diagnosis of PTGC (Leuk Lymphoma 2011;52:2041)
- May also be associated with immune and autoimmune disorders, such as Castleman disease and lupus (Pediatr Blood Cancer 2013;60:26)
- Rare case associated with papillary thyroid carcinoma (Case Rep Otolaryngol 2016;2016:6469073)
Diagnosis
- Excisional biopsy is needed to establish the diagnosis, usually evident at low magnification
- Careful microscopic examination for the possibility of potential concurrent Hodgkin lymphoma
- Evaluation for possible associated conditions should be tailored for patients with constitutional symptoms (Pediatr Blood Cancer 2022;69:e29638)
Laboratory
- Not usually associated with elevated lactate dehydrogenase (LDH), as seen in lymphoma
Radiology description
- Hypoechoic lymph node on ultrasound (Ann Hematol 2018;97:1081)
Prognostic factors
- PTGC follows a clinically indolent course (Semin Diagn Pathol 2023;40:371)
- Increased risk of recurrence seen in pediatric patients (Pediatr Blood Cancer 2022;69:e29638)
- Not a premalignant condition but there is a noncausal association with NLPHL in a small number of patients (Leuk Lymphoma 2011;52:2041)
- May also be seen in association with immune and autoimmune conditions
Case reports
- 2 year old boy with a lump in the right axilla (Children (Basel) 2022;9:214)
- 32 year old woman with palpable lymph nodes in the left axilla (Taehan Yongsang Uihakhoe Chi 2021;82:423)
- 39 year old woman with right neck lymphadenopathy (Case Rep Otolaryngol 2017;2017:5982168)
Treatment
- Standard of care: active surveillance (Leuk Lymphoma 2011;52:2041)
- Ongoing follow up and annual examination, including biopsy of any subsequent enlarged lymph nodes to assess for possibility of reactive follicular hyperplasia, PTGC or Hodgkin lymphoma (Int J Pediatr Otorhinolaryngol 2002;65:195)
Gross description
- Well encapsulated, enlarged lymph node
- Pale gray to tan lobulated cut surface; typically not fish flesh as seen in lymphoma
Microscopic (histologic) description
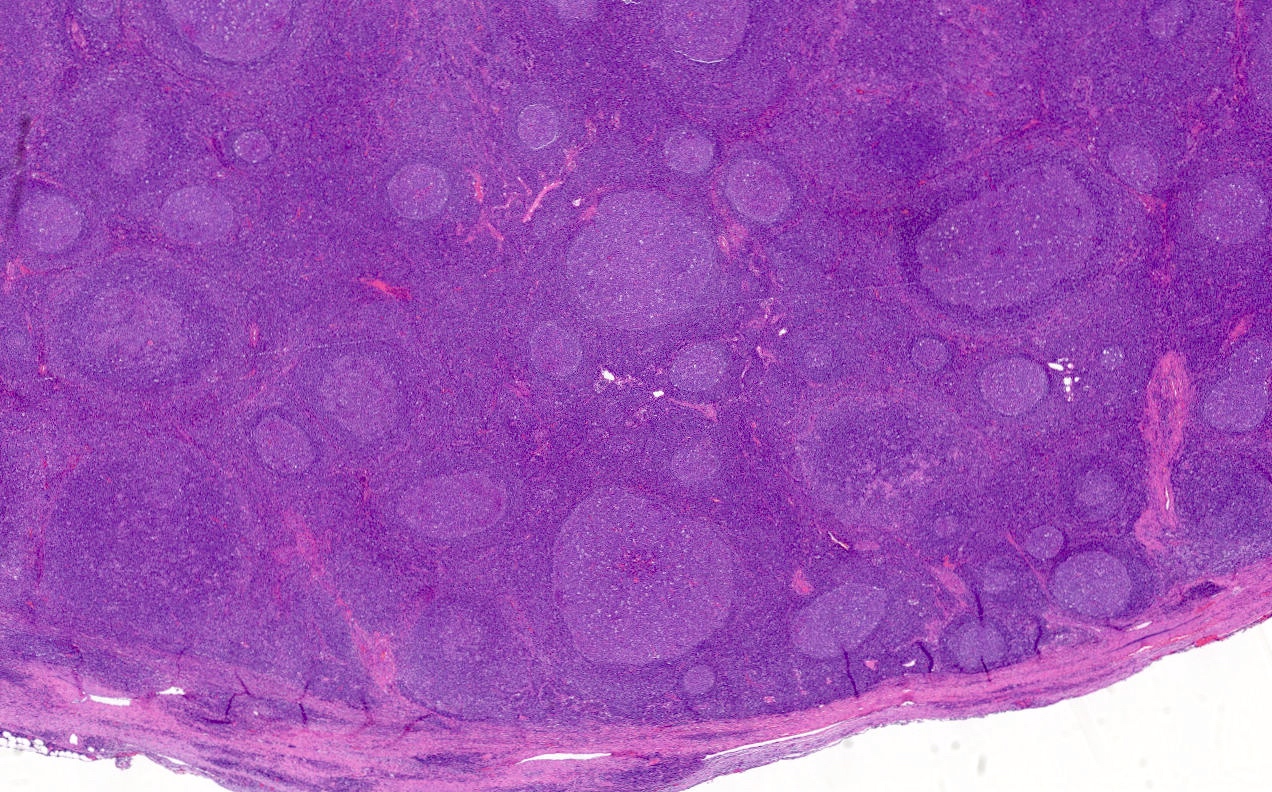
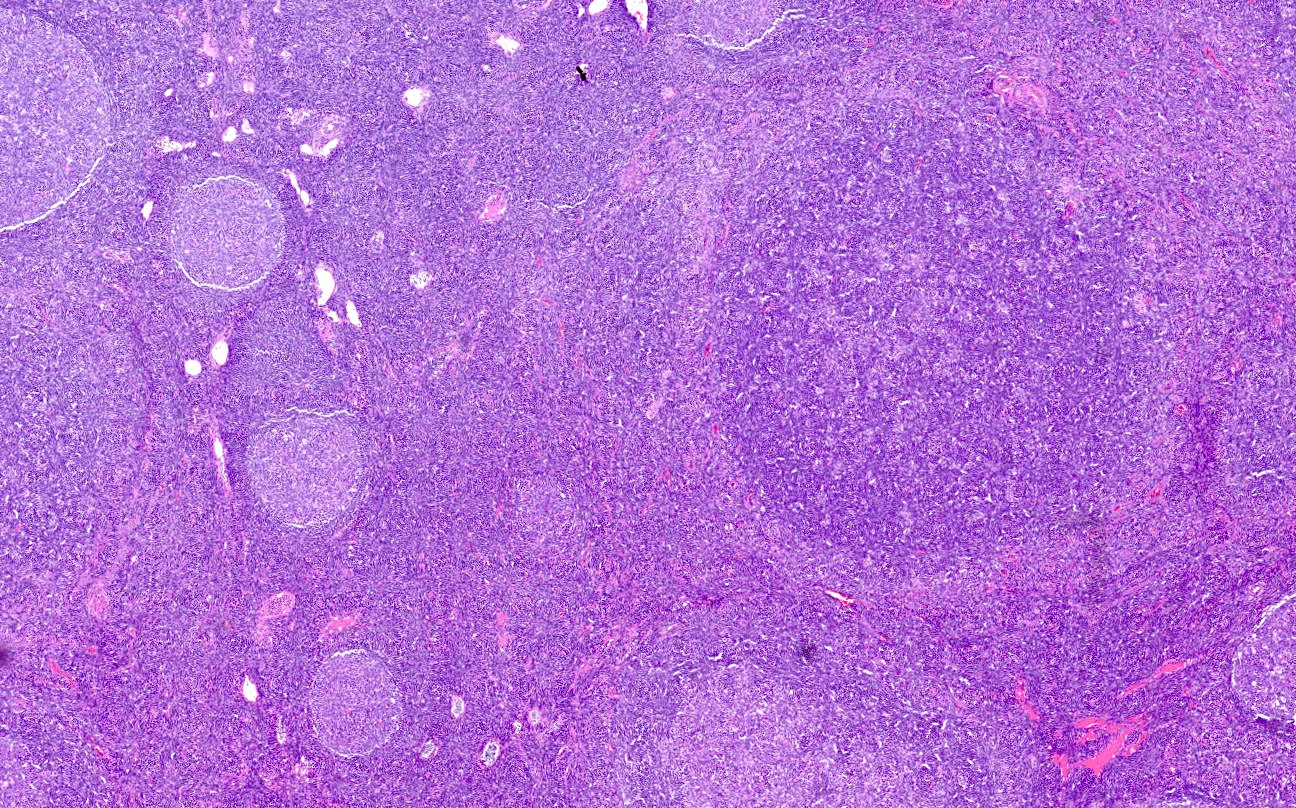
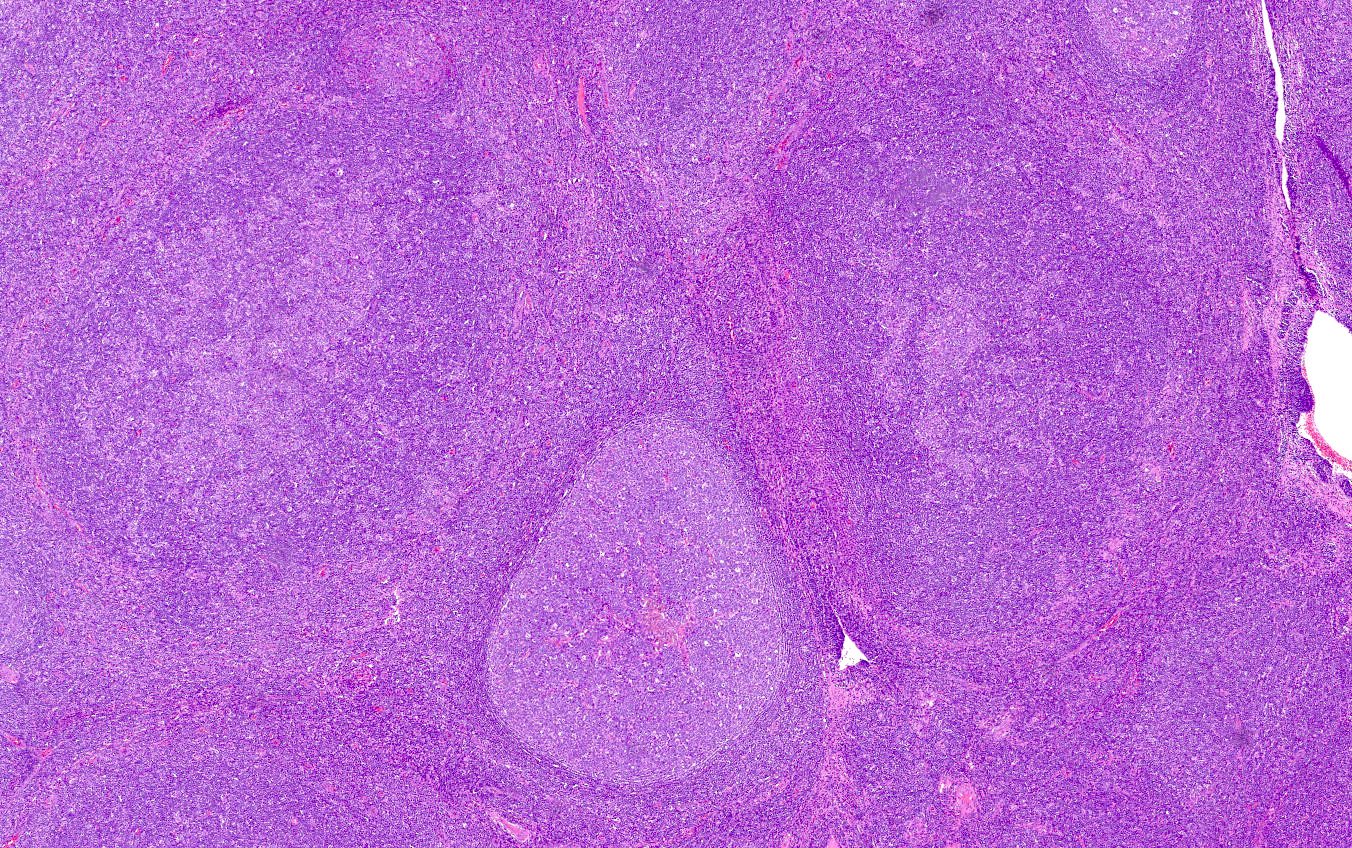
- Occurs in a background of follicular hyperplasia of lymph node
- Preserved nodal architecture with PTGC follicles diameter being 3 - 5 times larger than usual reactive follicles (Am J Clin Pathol 1990;93:219)
- Background lymphoid follicles appear as primary follicles when PTGC is associated with NLPHL (Hum Pathol 2015;46:1655)
- PTGC nodules may appear in different morphologic stages
- Multifocal migration of small lymphocytes from the thickened mantle zone into the germinal center, disrupting the germinal center and breaking up the germinal center into variegated clusters of follicle center cells (follicle lysis)
- Loss of demarcation between germinal center and mantle zone
- Normal germinal center cells (centrocytes, centroblasts, follicular dendritic cells) may be lost (Acta Haematol 2002;108:33)
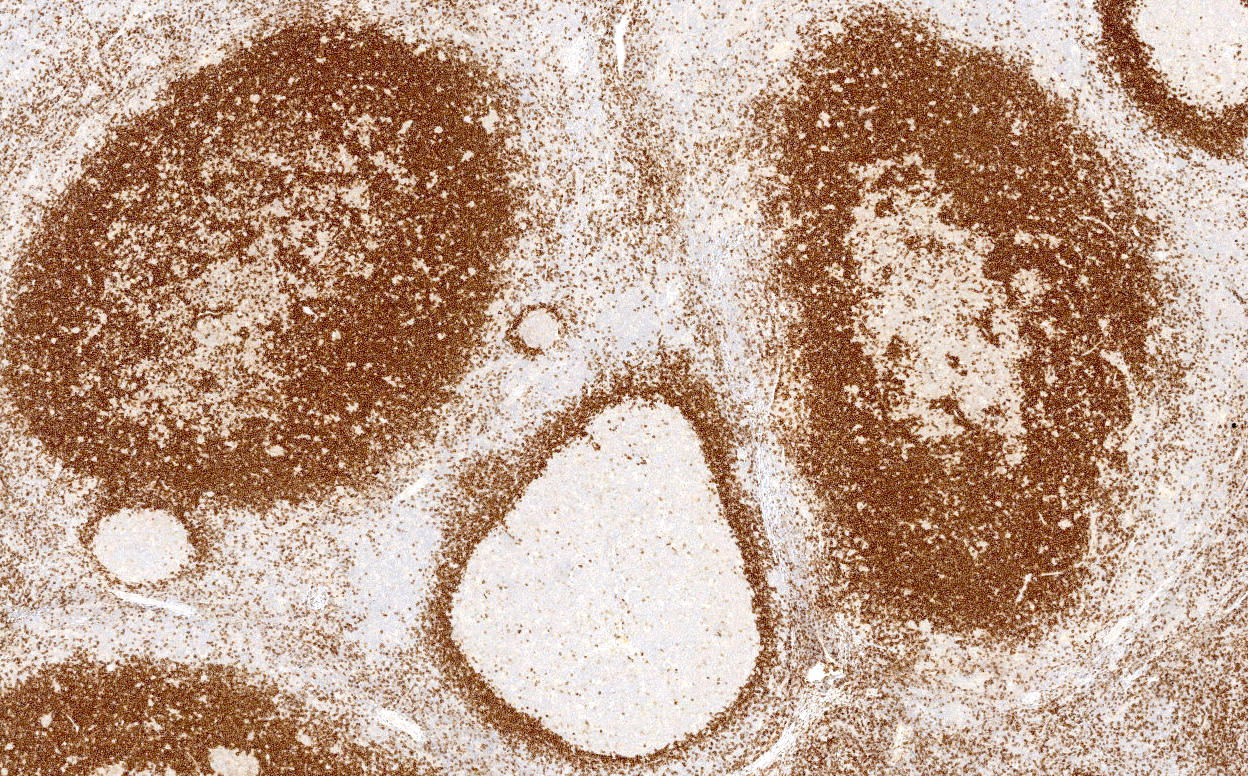
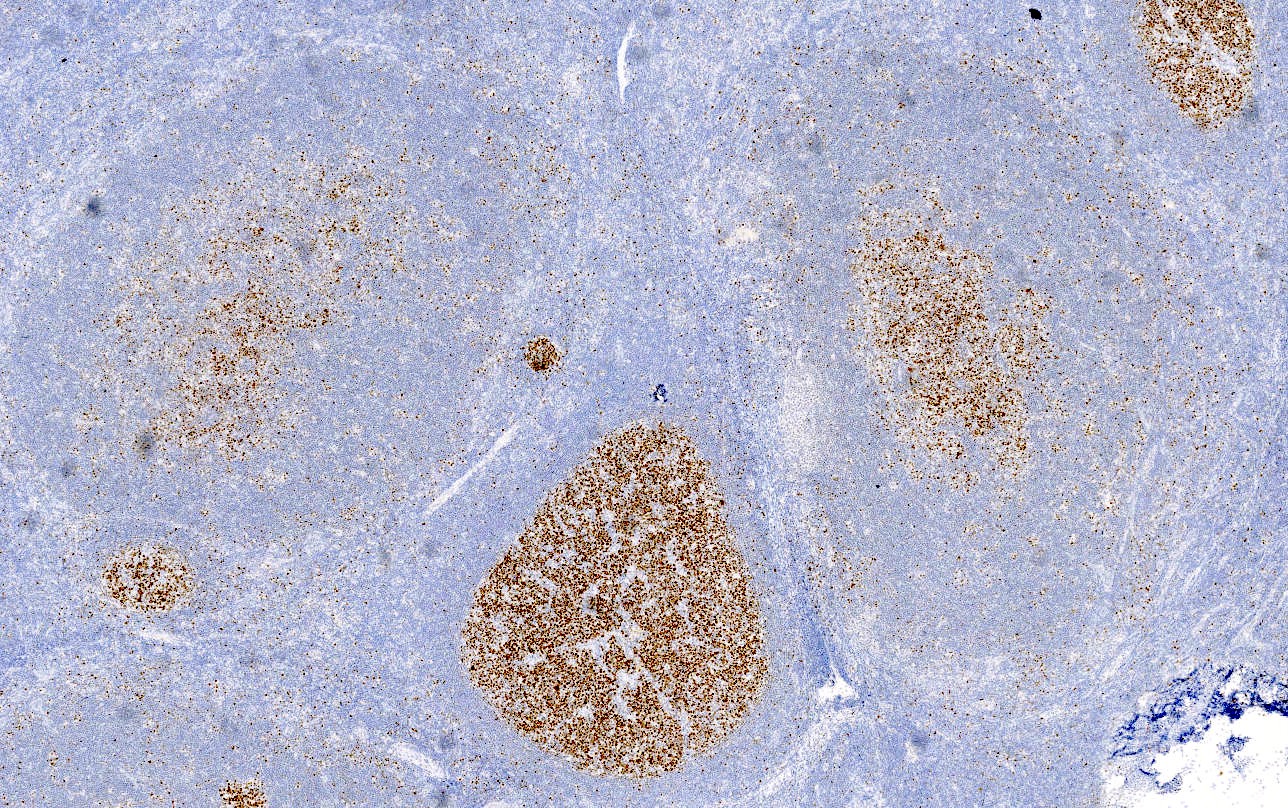
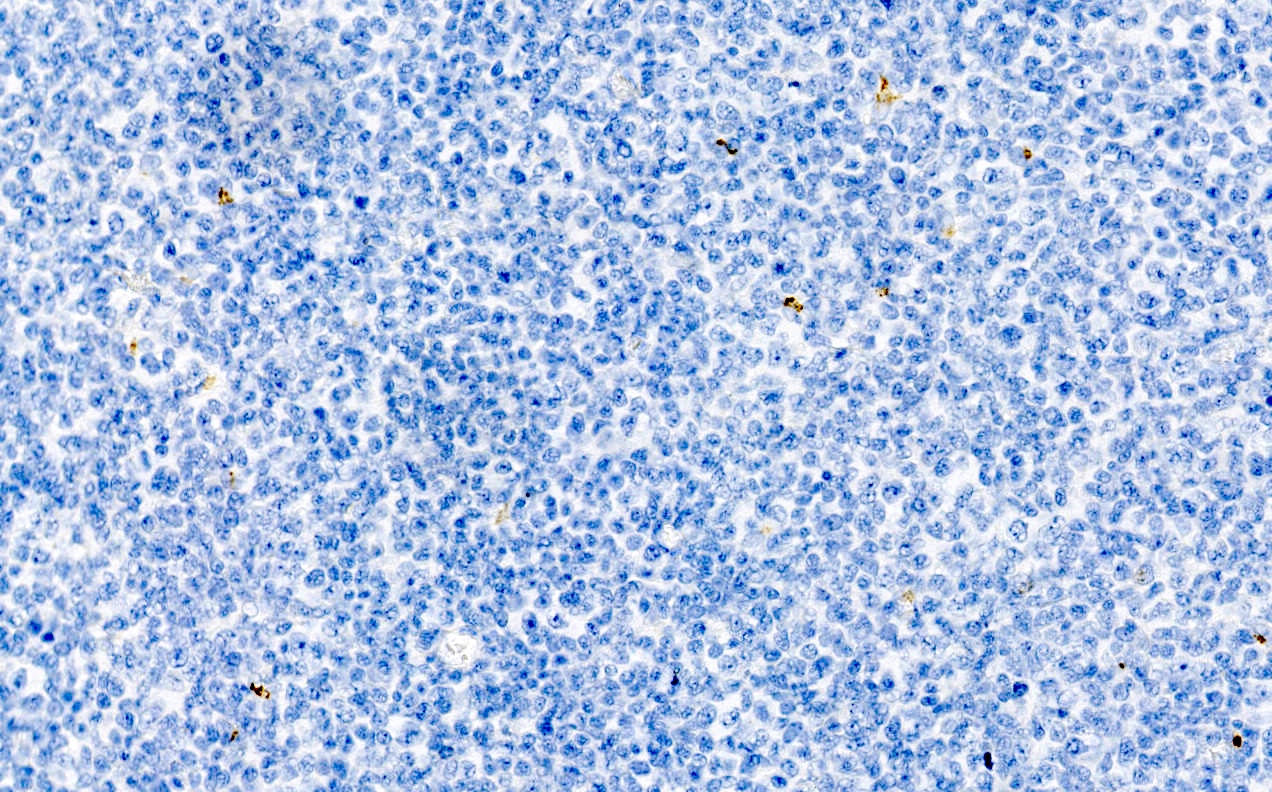
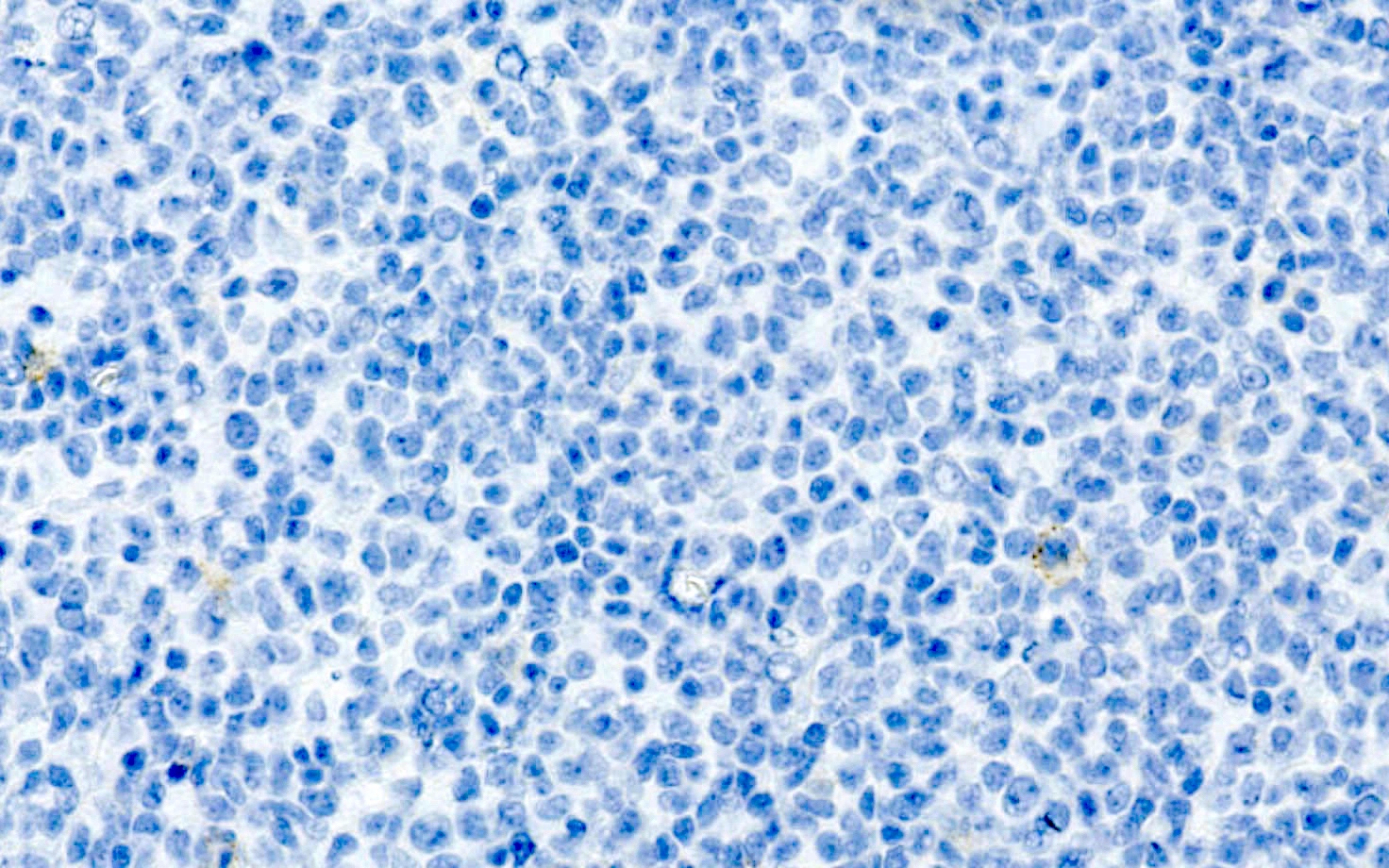
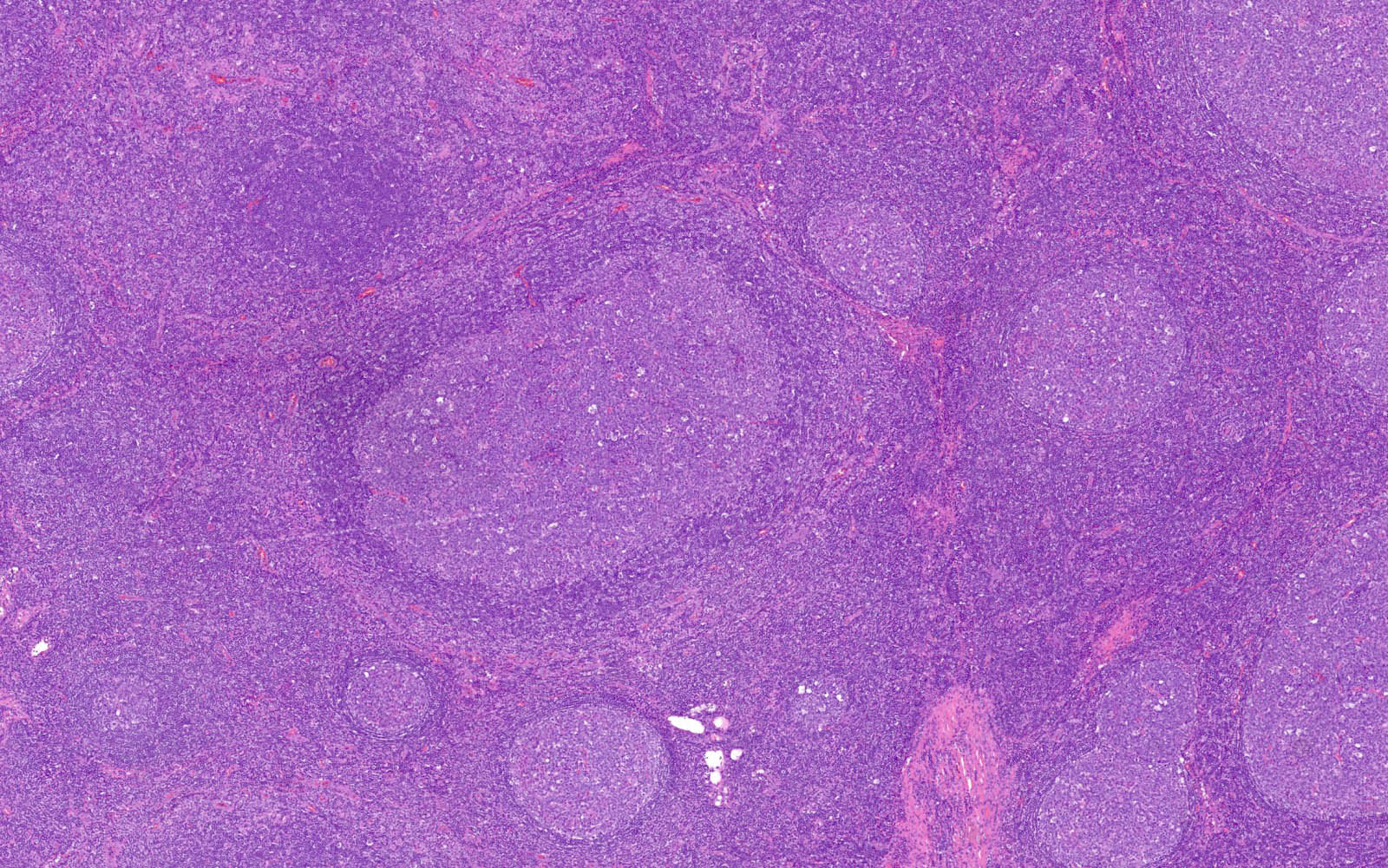
Microscopic (histologic) images
Contributed by Roaa Aljuaid, M.B.B.S.
Positive stains
- Mantle zone B cells: express pan-B cell markers (CD19, CD20, PAX5 and CD79a) and IgD
- Germinal center cells: express pan-B cell markers as well as germinal center markers (BCL6, CD10, HGAL and GCET1)
- CD21 shows disruption of the follicular dendritic cell meshwork
- Reference: Pediatr Blood Cancer 2022;69:e29638
Negative stains
- EBV (EBER, LMP) negative; no large neoplastic cells on EMA, CD15 or CD30
- Mantle zone B cells: negative for BCL1, SOX11, CD5 and CD43
- Germinal center B cells: negative for BCL2
- Reference: Int J Pediatr Otorhinolaryngol 2002;65:195
Flow cytometry description
- Polytypic B cells
- No T cell immunophenotypic aberrancy
Molecular / cytogenetics description
- No evidence of B cell (IGH and IGK) or T cell receptor (TRB and TRG) gene rearrangement
- No BCL2 or BCL6 gene alterations
Sample pathology report
- Right cervical lymph node, excisional biopsy:
- Reactive lymphoid hyperplasia with progressive transformation of germinal centers (PTGC) (see comment)
- Negative for malignancy
- Comment: PTGC may precede, follow or coincide with nodular lymphocyte predominant Hodgkin lymphoma in certain patients.
Differential diagnosis
- Nodular lymphocyte predominant Hodgkin lymphoma:
- Nodular lymphocyte predominant Hodgkin lymphoma (WHO HAEM5), also known as nodular lymphocyte predominant B cell lymphoma (Blood 2022;140:1229)
- Lymph node architecture is partially or completely effaced
- Nodules contain lymphocytic and histiocytic (popcorn) neoplastic B cells
- Large lymphocytes express pan-B cell markers, BCL6, EMA (variable) and strong OCT2
- T cells rosette around lymphocytic and histiocytic cells and often express CD3, PD-1 and CD57
- Follicular lymphoma, floral variant:
- Partial or complete effacement of the lymph node architecture
- Follicles are fused, fragmented and back to back
- Neoplastic germinal centers may appear monotonous with various proportions of centrocytes and centroblasts and diminished tingible body macrophages and mitoses
- Monoclonal B cells typically express BCL6, CD10, HGAL, GCET1 and BCL2
- Lymphocyte rich Hodgkin lymphoma, nodular variant:
- Human immunodeficiency virus (HIV) associated lymphadenopathy:
- Affected lymph node in acute HIV infection can resemble PTGC
- Follicle lysis: small mantle zone B cells penetrate and disrupt the germinal centers
- Affected follicles are not as large as the PTGC follicles
- Hemorrhage with large monocytoid cell proliferation is common
- IgG4 related lymphadenopathy (Semin Diagn Pathol 2024;41:108, Am J Surg Pathol 2018;42:977):
- 5 distinct histologic patterns
- Progressive transformation of germinal centers is a hallmark of one of the variants
- Increased number of IgG4 positive plasma cells in affected nodes
- Epithelioid granulomas around PTGC is a rare and specific finding (Semin Diagn Pathol 2018;35:61)
- Pediatric nodal marginal zone lymphoma:
- Marginal zone expansion with interfollicular infiltration of lymphoma cells (Virchows Arch 2023;483:317)
- Follicular changes similar to PTGC
- Peripheral rims of the follicles are disrupted by the proliferation of the marginal zone (Adv Anat Pathol 2017;24:128)
Board review style question #1
Board review style answer #1
E. CD79a. The mantle cells express pan-B cell antigens, including CD79a. Answers A, C and D are incorrect because these markers are characteristically positive in mantle cell lymphoma but not in the nonneoplastic mantle cells of PTGC. Answer B is incorrect because BCL6 is immunoreactive on follicle center cells and not on mantle cells.
Comment Here
Reference: Progressive transformation of germinal centers
Comment Here
Reference: Progressive transformation of germinal centers
Board review style question #2
Which of the following lymphoid neoplasms is more commonly associated with progressive transformation of germinal centers (PTGC)?
- Follicular lymphoma
- Mantle cell lymphoma
- Mycosis fungoides
- Nodular lymphocyte predominant Hodgkin lymphoma
- Plasma cell neoplasm
Board review style answer #2
D. Nodular lymphocyte predominant Hodgkin lymphoma has been found to have the highest risk of being seen in association with PTGC. Answer C is incorrect because mycosis fungoides is associated with dermatopathic lymphadenopathy and not PTGC. Answers A, B and E are incorrect because these hematopoietic neoplasms are not known to occur with increased incidence in patients with PTGC.
Comment Here
Reference: Progressive transformation of germinal centers
Comment Here
Reference: Progressive transformation of germinal centers