Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Basu A, Zhou F. Pulmonary artery intimal sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumorpais.html. Accessed April 2nd, 2025.
Definition / general
- Malignant mesenchymal tumor arising from large pulmonary blood vessels
Essential features
- Predominantly intraluminal growth in pulmonary arterial circulation
- Arises from intimal layer of elastic arteries, usually sparing media
- Causes obstruction of the vessel lumen leading to pulmonary embolism (PE) or pulmonary hypertension
- Causes embolic seeding to peripheral organs
- Microscopy: spindle cells with variable smooth muscle expression and variable atypia; however, may be completely undifferentiated with or without heterologous elements (osteosarcoma, chondrosarcoma)
- > 70% cases are positive for MDM2 (mouse double minute 2) amplification
- References: J Thorac Dis 2019;11:S9, Pathol Res Pract 2021;224:153548
ICD coding
- ICD-O: 9137/3 - intimal sarcoma
- ICD-11: 2C25.Y & XH36H7 - other specified malignant neoplasms of bronchus or lung & intimal sarcoma
Epidemiology
- Rare tumor
- Estimated prevalence: 0.001 - 0.003% (maybe be underestimated due to similar presentation as pulmonary thromboembolism)
- Found in 1 - 4% of pulmonary endarterectomy specimens in patients with clinical features of chronic thromboembolic pulmonary hypertension
- Females affected more than males (M:F = 0.7:1)
- Median age at diagnosis: 48 years
- References: CJC Open 2020;2:711, Aorta (Stamford) 2016;4:142, Korean J Radiol 2018;19:792, Cancer 1993;71:1761
Sites
- Pulmonary arteries
- Anywhere from pulmonary valve to lobar branches
- Bilateral or unilateral
- Can also grow backwards into heart
- Rare reports of intimal sarcoma arising from other vessels and the heart
- Larger vessels: aorta (known as aortic intimal sarcoma, which is even rarer)
- Peripheral arteries: iliac and femoral arteries; or even more rarely, may arise from the renal arteries, carotid arteries or inferior vena cava
- Heart: undifferentiated pleomorphic sarcomas (UPS) of the heart is suggested to represent the cardiac analog of intimal sarcoma
- References: Case Rep Oncol 2016;9:267, Radiographics 2021;41:361, Cancer 1993;71:1761, J Thorac Oncol 2016;11:441 Mod Pathol 2021;34:2122
Pathophysiology
- Originates from subendothelial pluripotent cells within intimal lining
- Frequent amplifications and gains as well as other alterations, in 12q12-15, 4q12, 7p12 and others, where several genes, including MDM2, CDK4, PDGFRA, EGFR and other genes, are located
- References: Pathol Res Pract 2021;224:153548, Radiographics 2021;41:361
Etiology
- Not known
Clinical features
- Mimics pulmonary embolism and pulmonary hypertension
- Most common presentation: breathlessness
- Other symptoms: chest / back pain, cough, hemoptysis, fatigue, syncope, fever
- Clues to diagnosis:
- Absence of risk factors for pulmonary embolism (but half of patients with pulmonary embolism also have no risk factors)
- Patient fails anticoagulation therapy
- References: Radiographics 2021;41:361, Case Rep Oncol 2021;14:318, Intern Med 2019;58:3599
Diagnosis
- Diagnostic imaging modalities: CT angiography, fluorine 18-fluorodeoxyglucose PET (18F-FDG PET), MRI and echocardiography
- Biopsies are typically not performed
- Diagnosis is usually made on resection and histopathologic exam
- Reference: Radiographics 2021;41:361
Laboratory
- D dimer might be elevated (mimics thromboembolism) (Radiographics 2021;41:361)
Radiology description
- Heterogenous lobulated mass in an elastic artery (most often a pulmonary artery)
- Forms acute angle with vessel wall (versus pulmonary embolism)
- Possible imaging features:
- Tumor typically enlarges and molds to fill the central vascular lumen and its branches
- Can also grow backwards across the pulmonary valve, into the right ventricle, even into the right atrium and vena cava = continuous or multifocal appearance
- May occlude vascular lumen
- May invade through the vascular wall into surrounding tissue
- Intralesional blood flow suggests neoplasia
- CT: scan with contrast demonstrates a large filling defect
- PET: most intimal sarcomas are F-FDG avid
- MRI, T1 weighted: isointense to mildly hyperintense
- MRI, T2 weighted: isointense to highly intense
- Imaging differential diagnosis = more common cardiovascular lesions: thrombus, tumor embolism, valvular vegetation
- References: Case Rep Oncol 2016;9:267, Radiographics 2021;41:361
Radiology images
Contributed by Andre L. Moreira, M.D., Ph.D.
Images hosted on other servers:
Prognostic factors
- Generally poor survival
- Median survival, untreated: as a low as 1.5 months (range 1.5 - 5.5 months)
- Median survival, if resected: 10 months
- References: CJC Open 2020;2:711, Radiographics 2021;41:361
Case reports
- 25 year old Japanese woman presented with dyspnea and palpitations on exertion (Case Rep Oncol 2021;14:318)
- 36 year old man presented with chest pain and mild shortness of breath on exertion (CJC Open 2020;2:711)
- 37 year old Chinese woman presented with chest tightness and dyspnea (Medicine (Baltimore) 2021;100:e24699)
- 39 year old man experienced chest pain (World J Clin Cases 2021;9:3960)
- 42 year old woman with progressive shortness of breath and palpitation, pitting edema and fatigue (Respirol Case Rep 2020;8:e00530)
- 64 year old woman was referred to another hospital for syncope (Intern Med 2019;58:3599)
- 72 year old woman presented with a 2 month history of mild dyspnea on exertion (Case Rep Pulmonol 2021;2021:5573869)
- 79 year old patient with pulmonary arterial mass (Case of the month #535)
Treatment
- Surgical resection:
- Pulmonary endarterectomy (PEA)
- Full thickness resection
- Pneumonectomy
- Full thickness resection = complete excision of affected pulmonary artery depending on extent of tumor
- Neoadjuvant or adjuvant chemotherapy or radiation therapy may be considered
- Possible chemotherapy regimens: anthracyclines, ifosfamide, gemcitabine, taxanes, platinum based antineoplastic drugs
- Immunotherapy (not yet standardized)
- Reference: Radiographics 2021;41:361
Clinical images
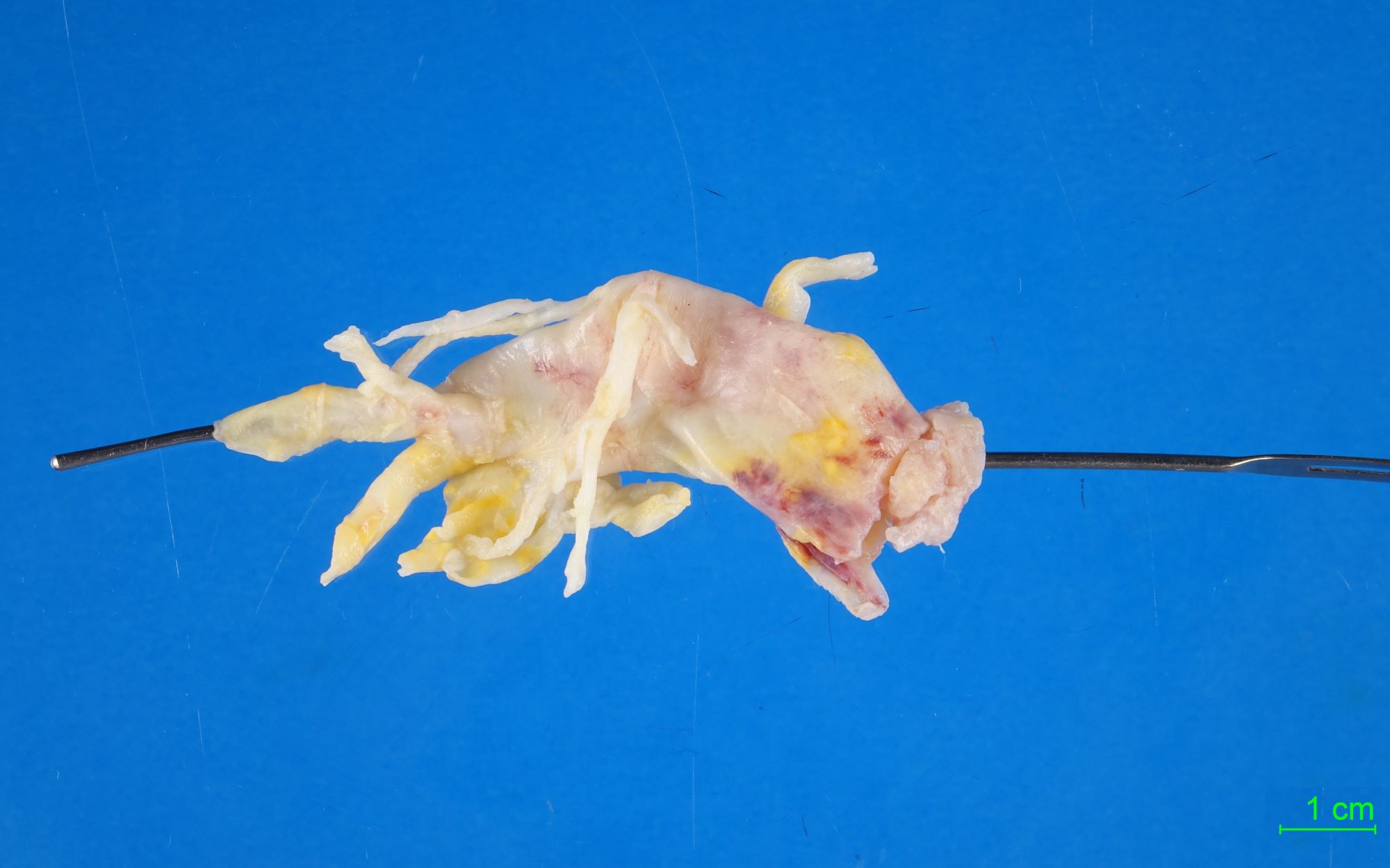
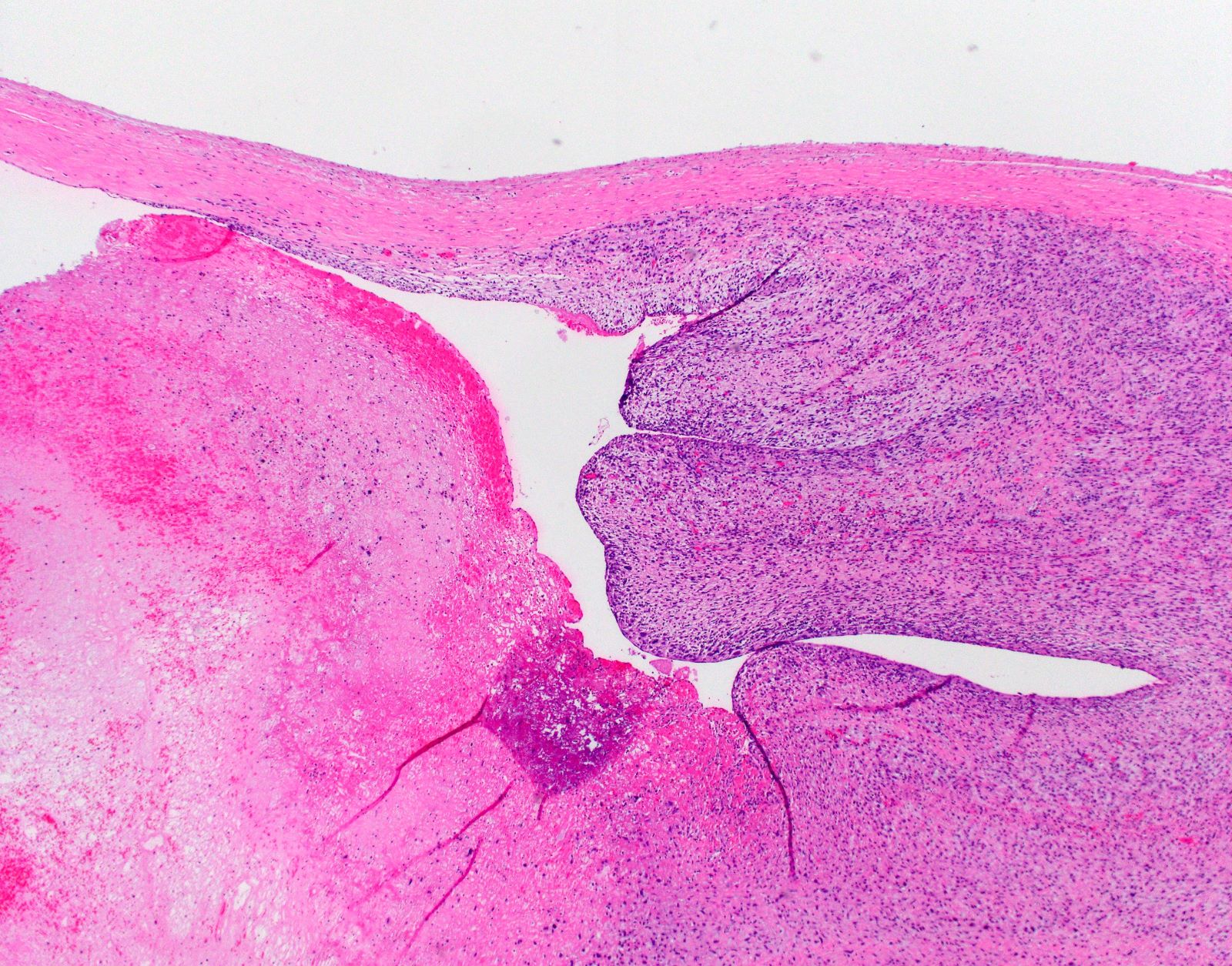
Gross description
- Polypoid intraluminal masses attached to the arterial wall
- White to yellow solid mass
- Can resemble mucoid or gelatinous clots in vessel lumen
- Sometimes shows hemorrhage and necrosis
- References: Radiographics 2021;41:361, Case Rep Pulmonol 2021;2021:5573869
Gross images
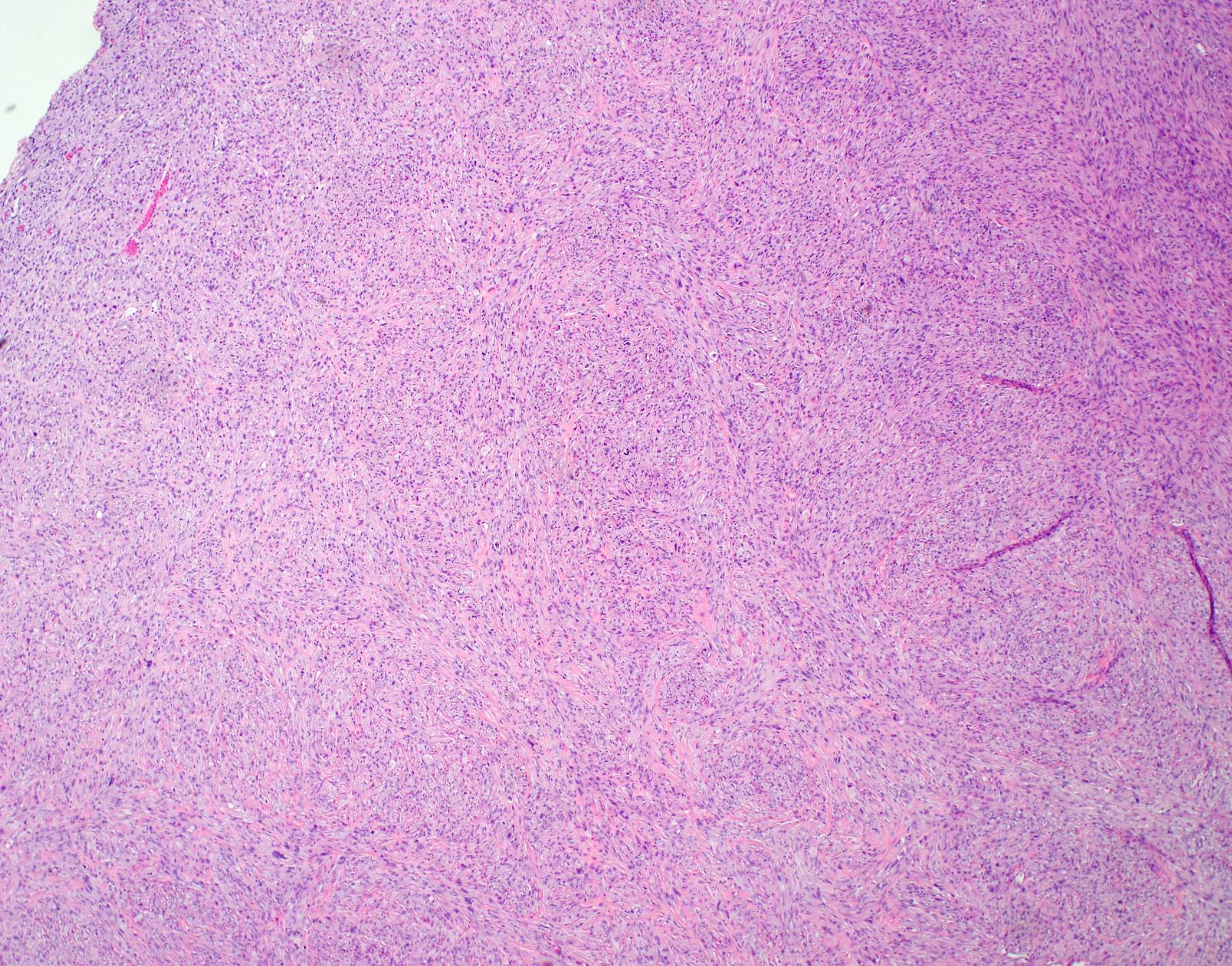
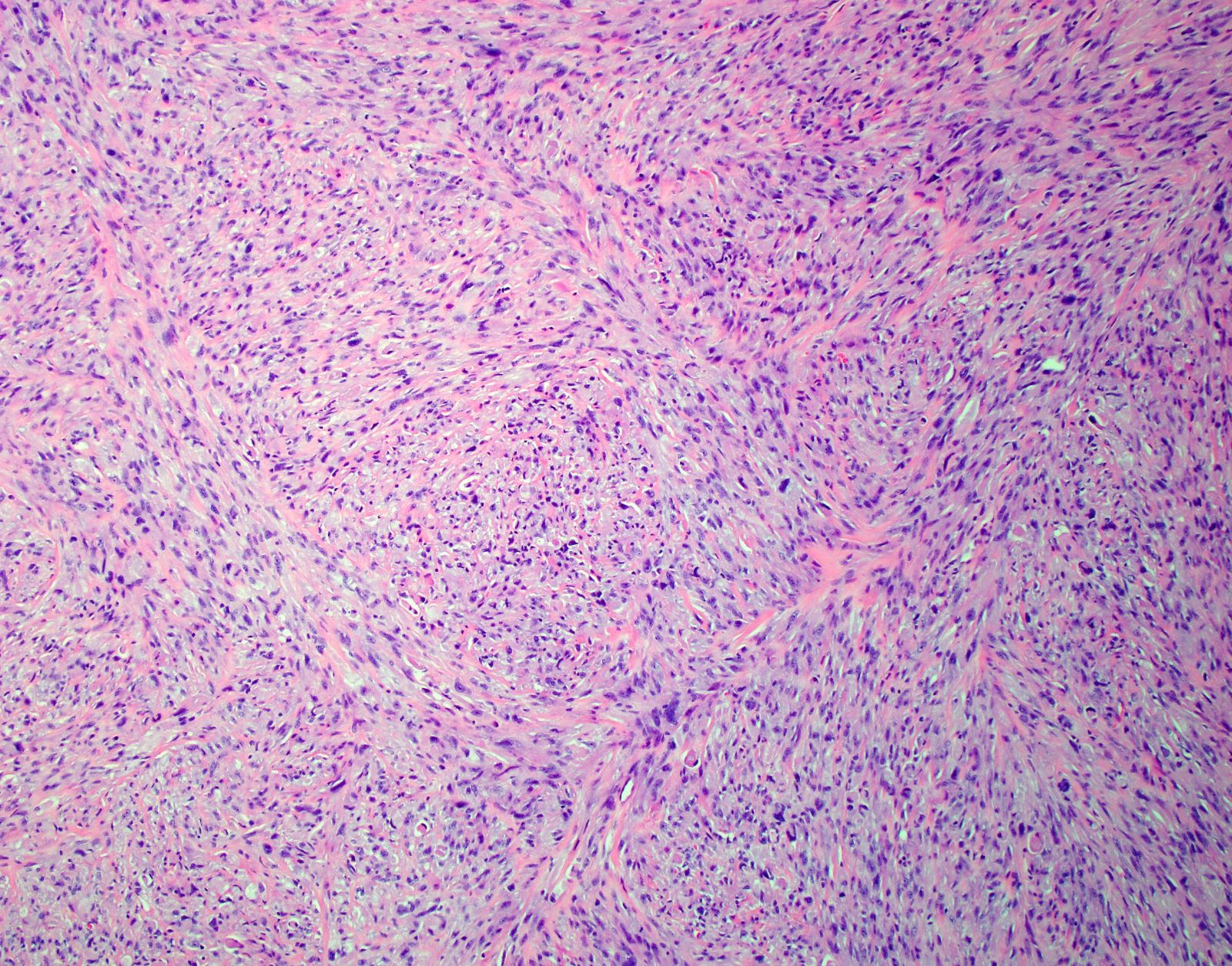
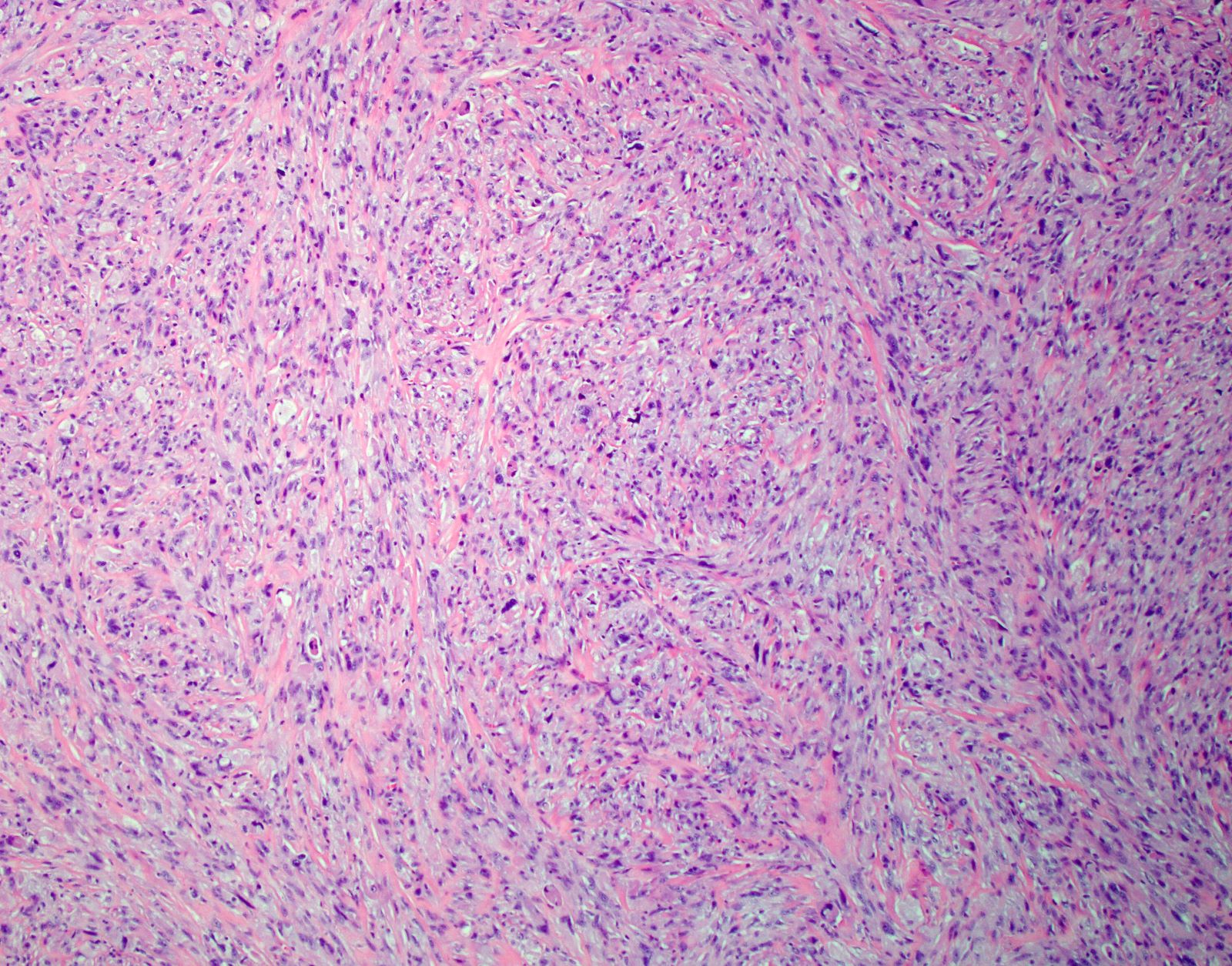
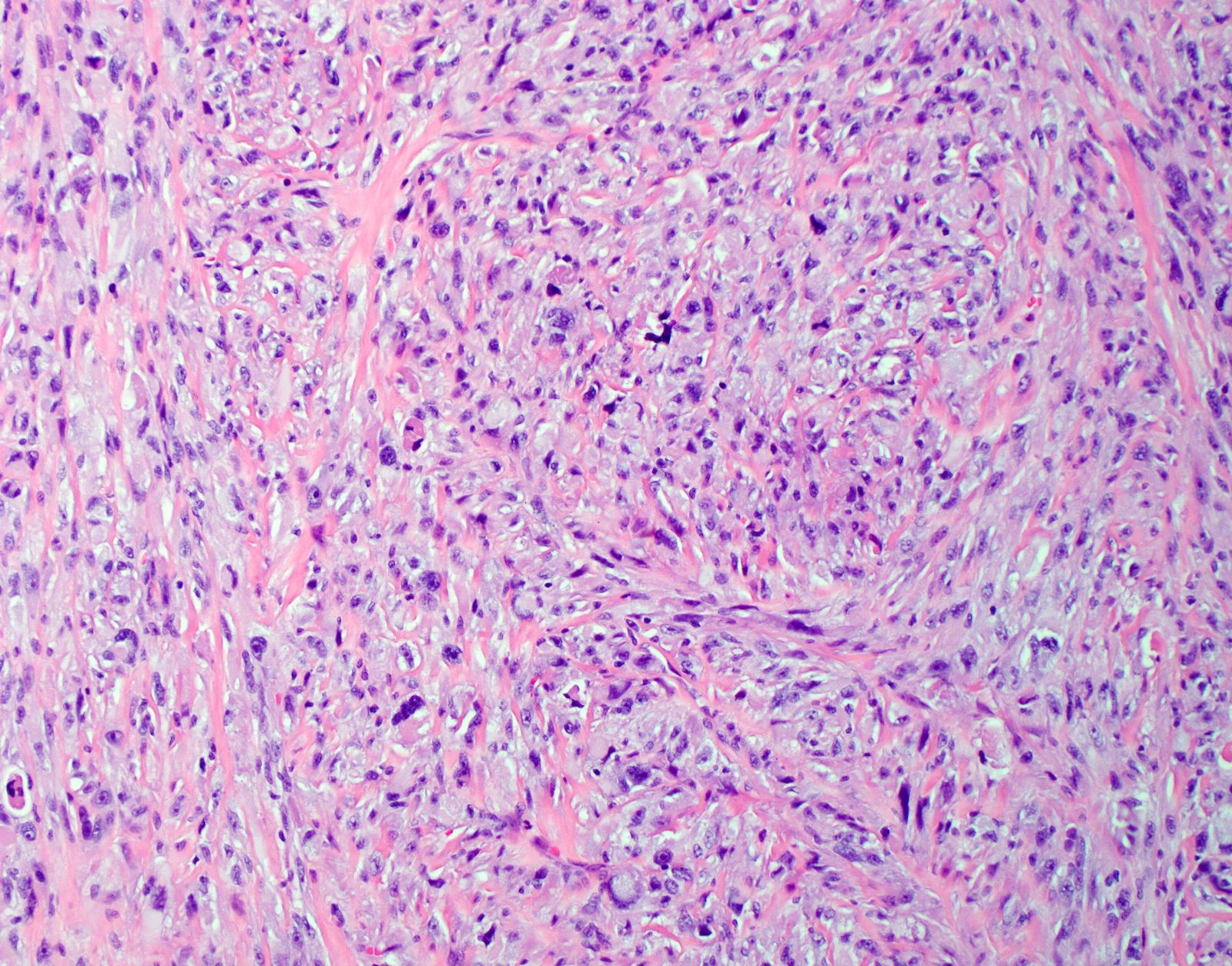
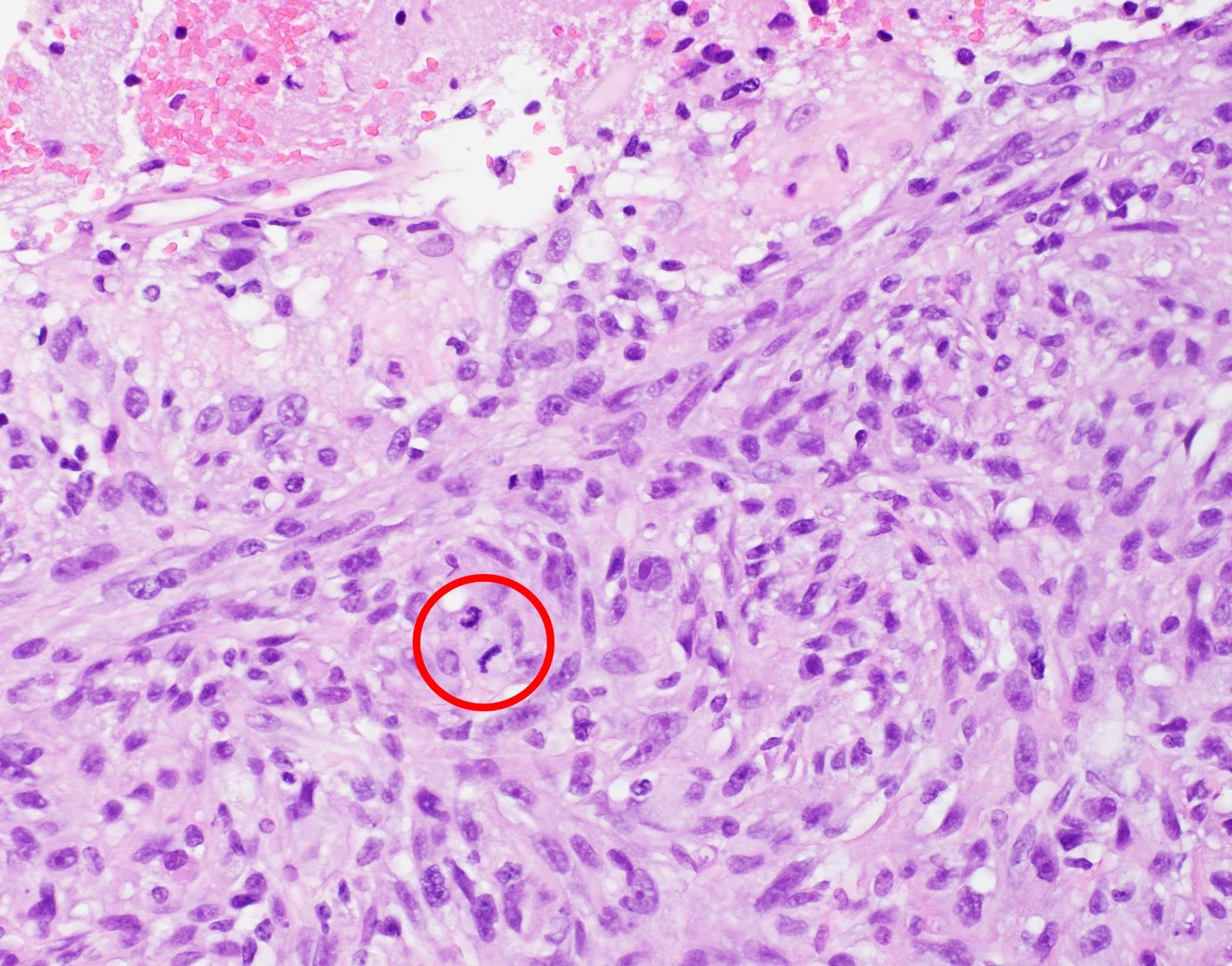
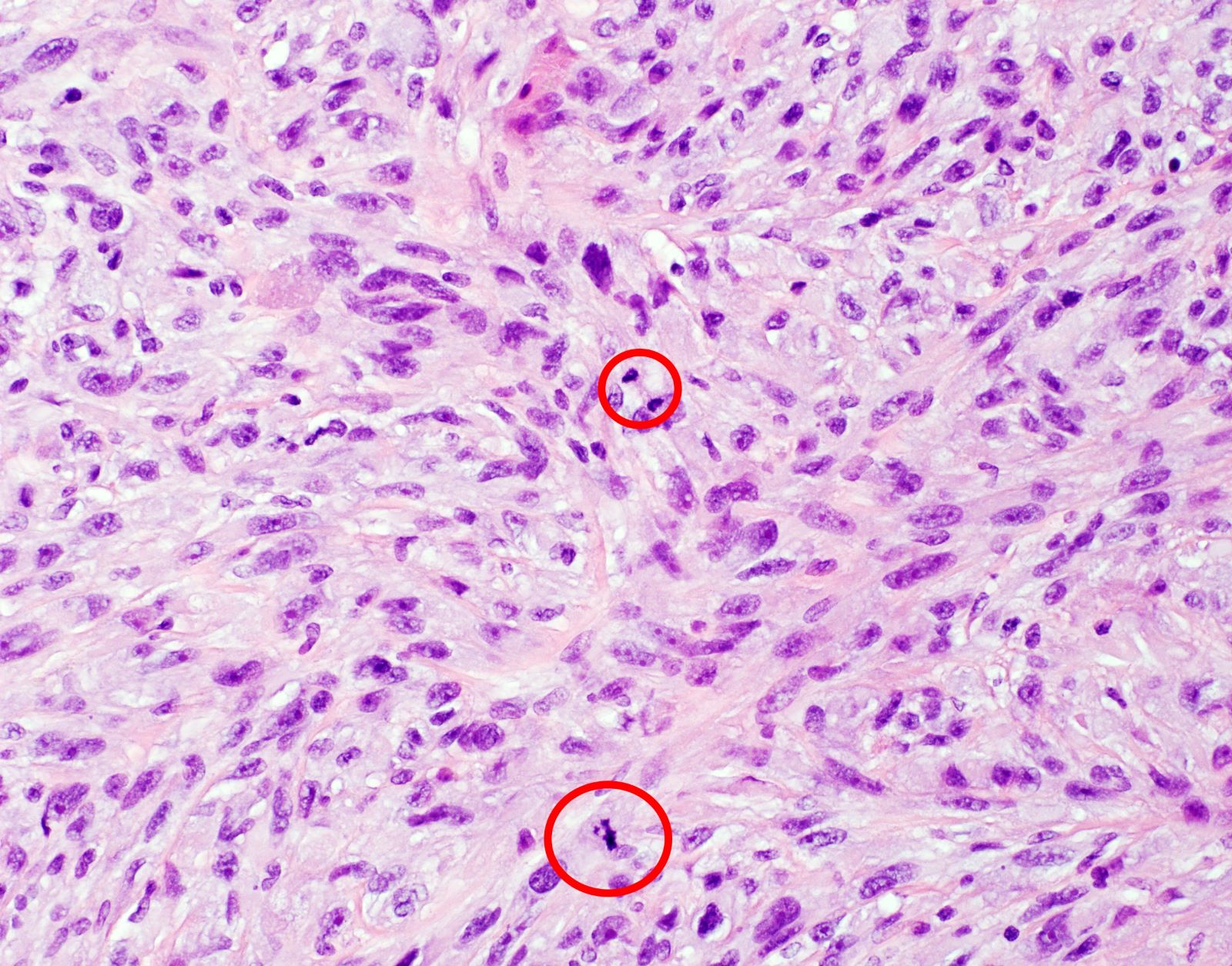
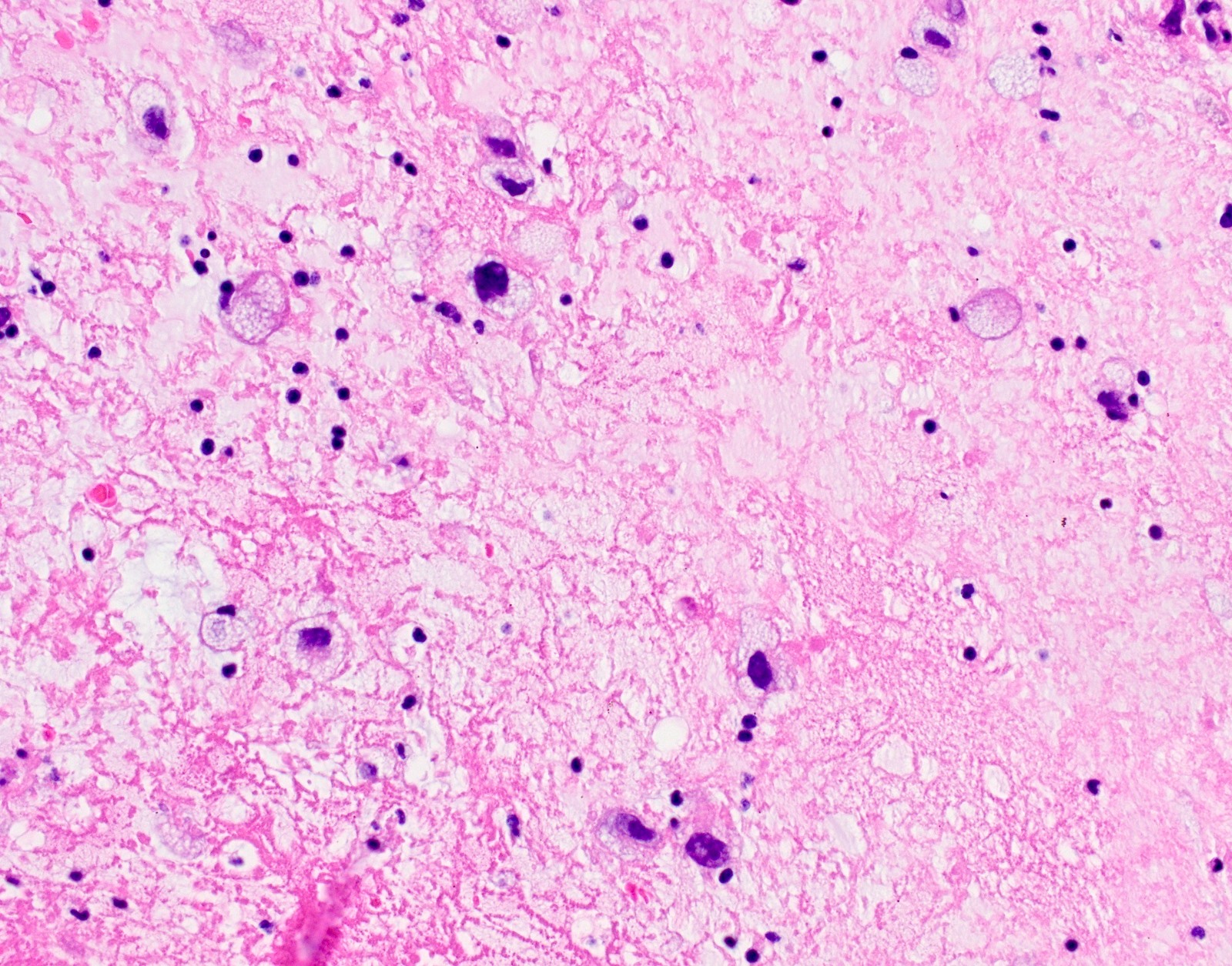
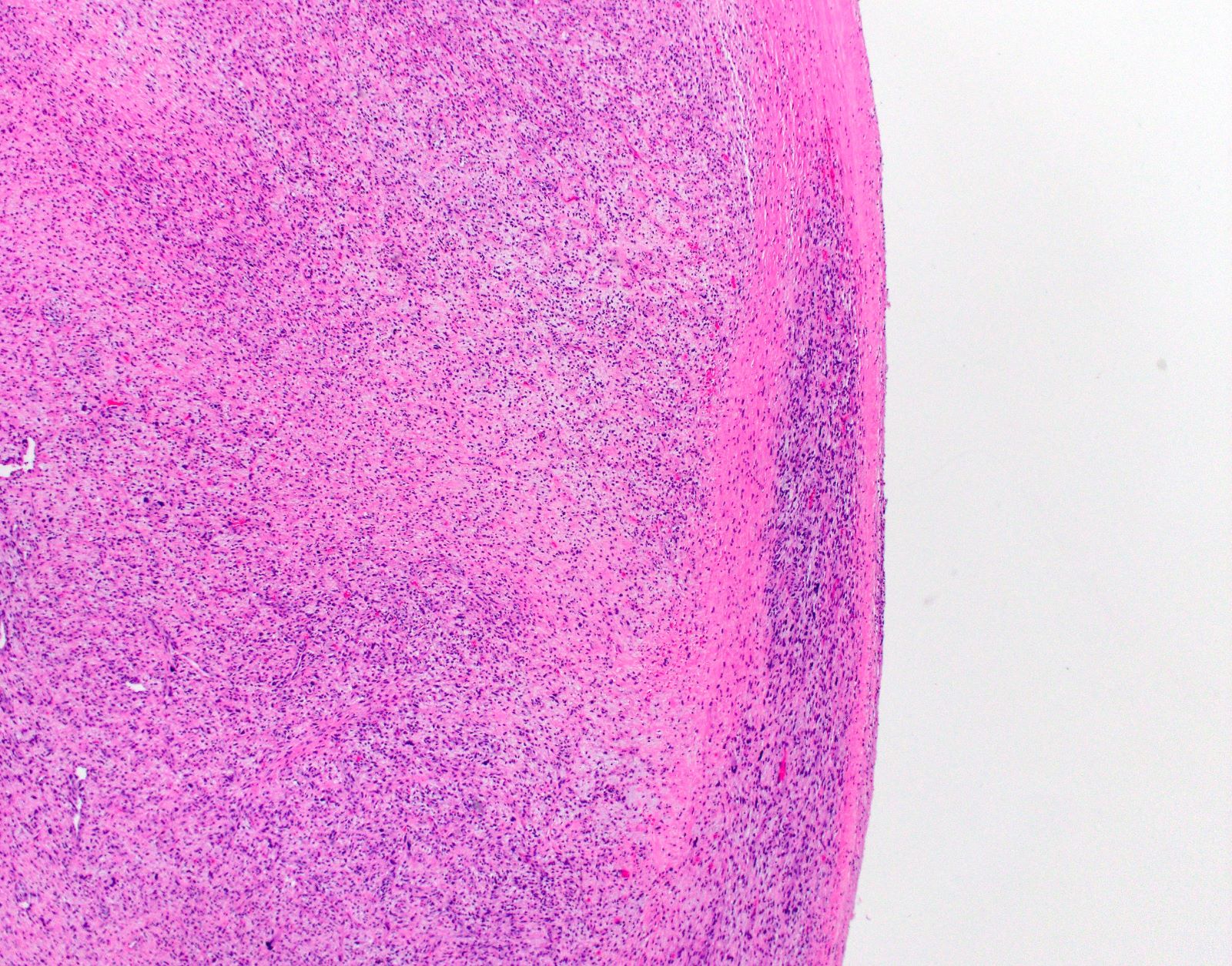
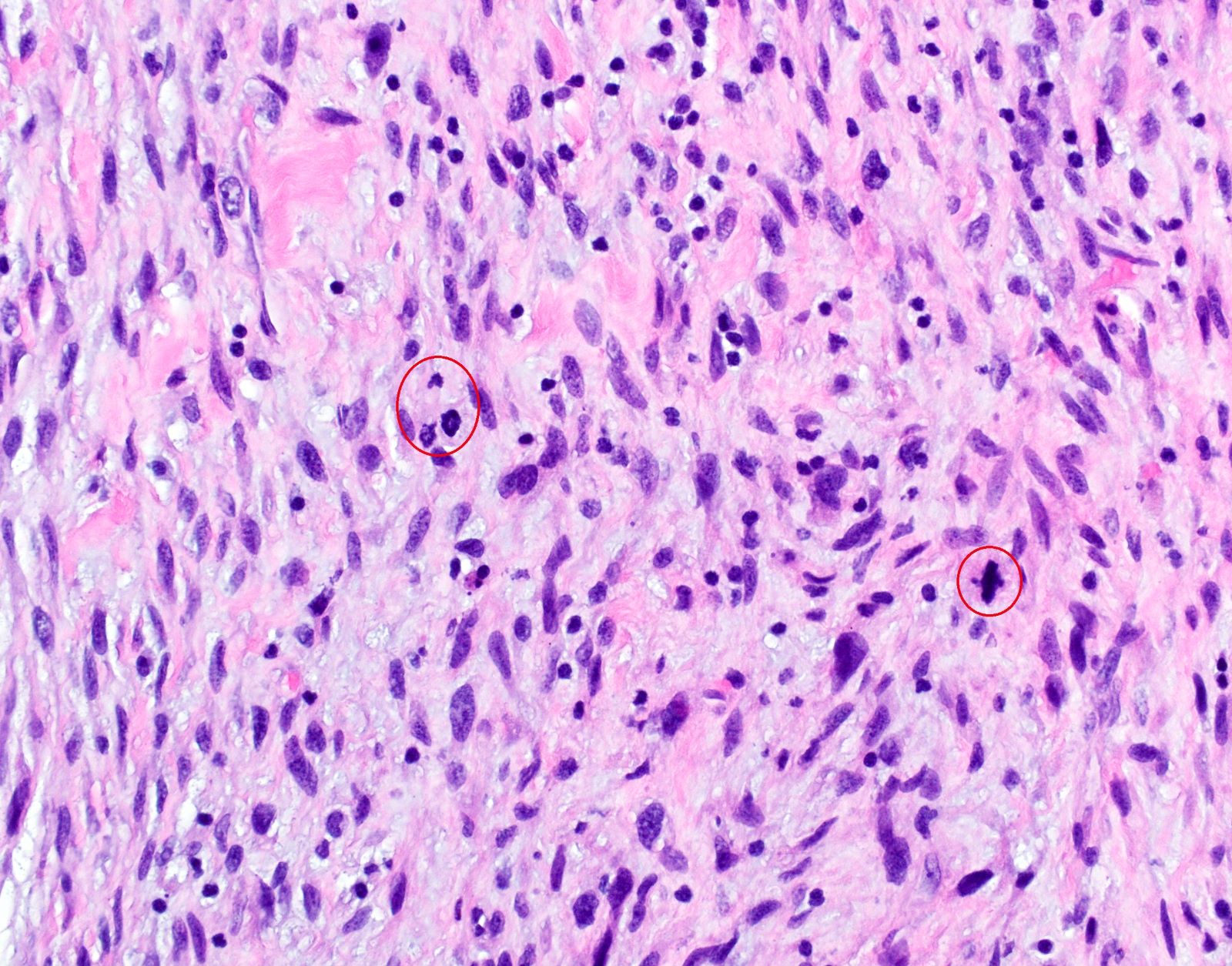
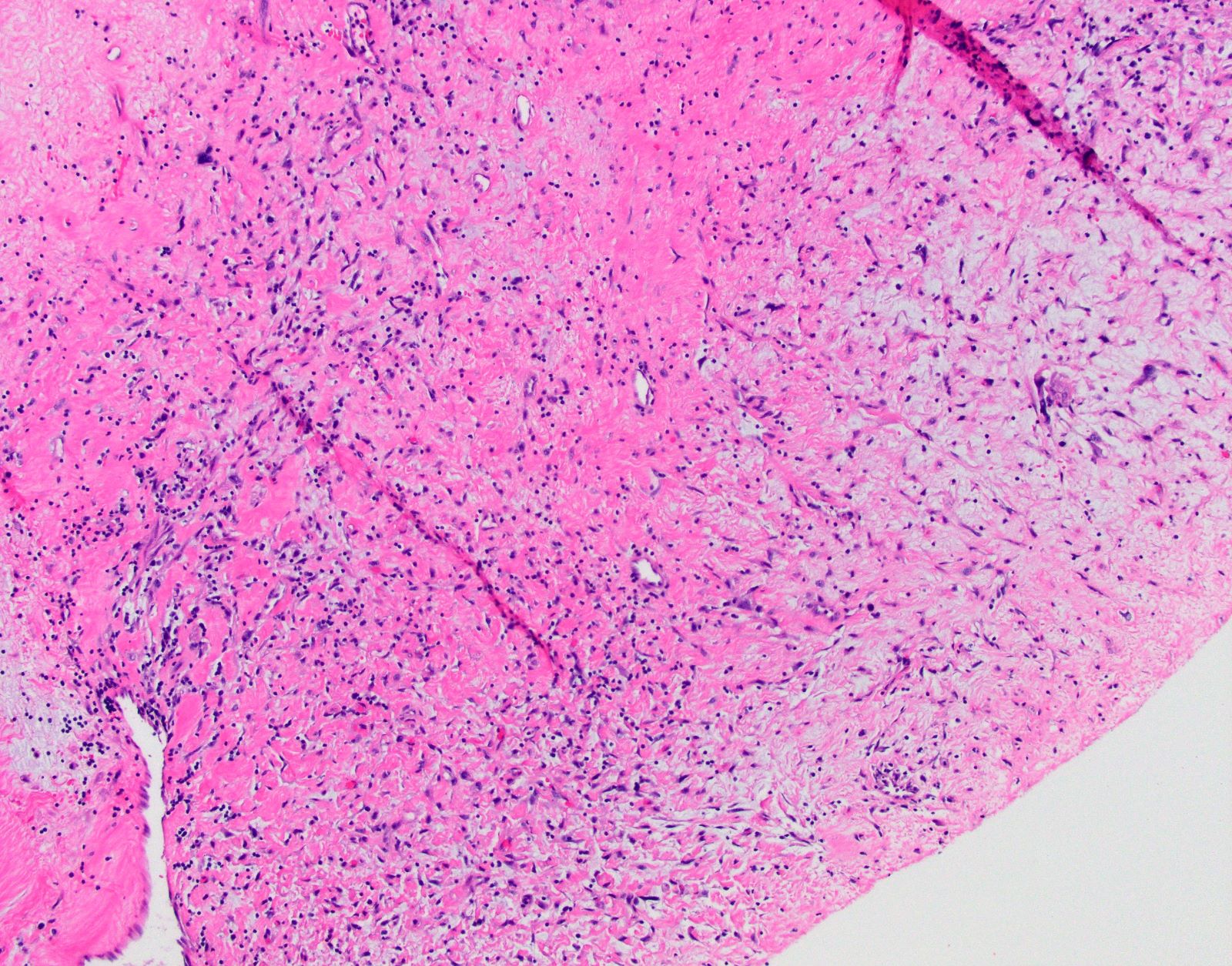
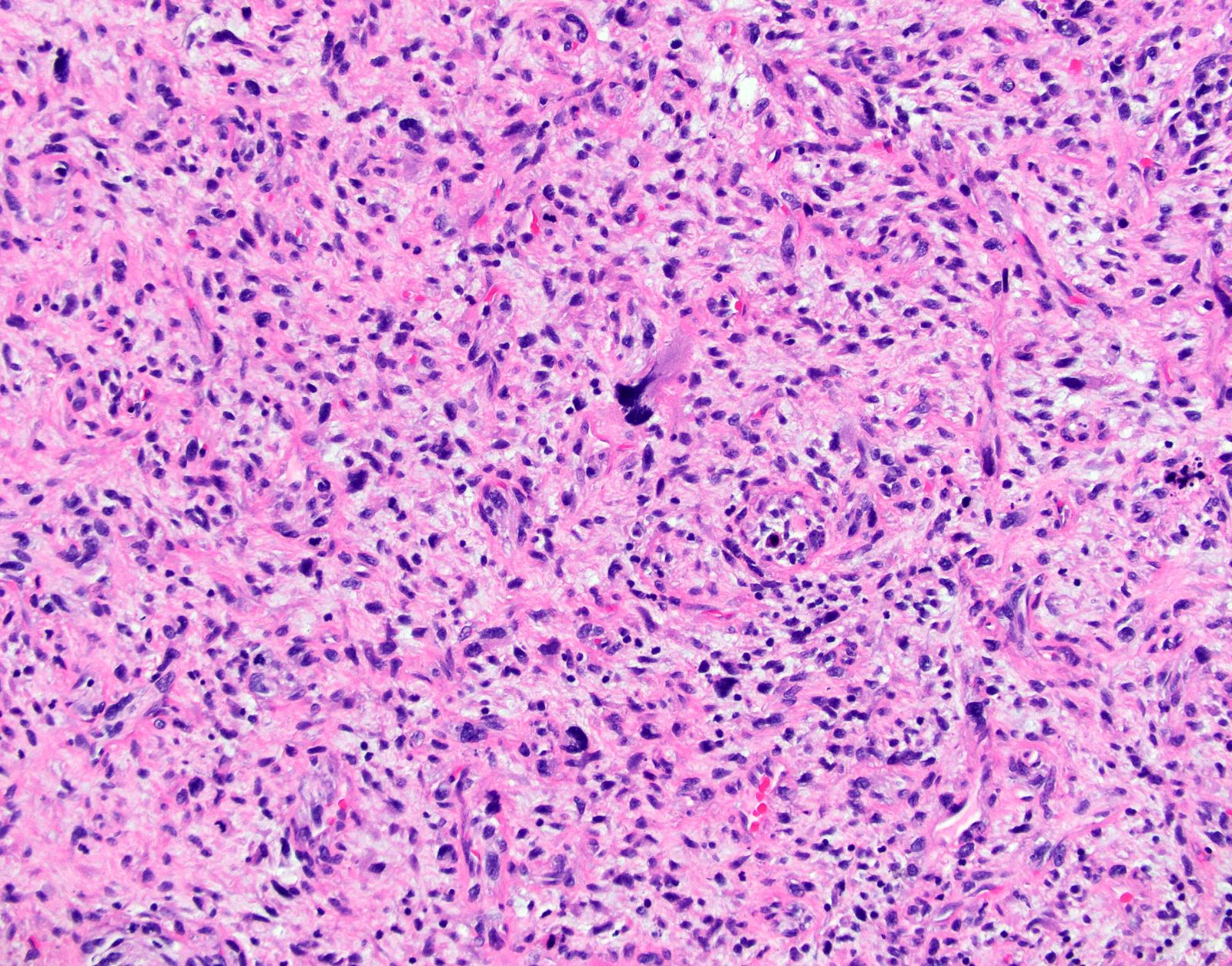
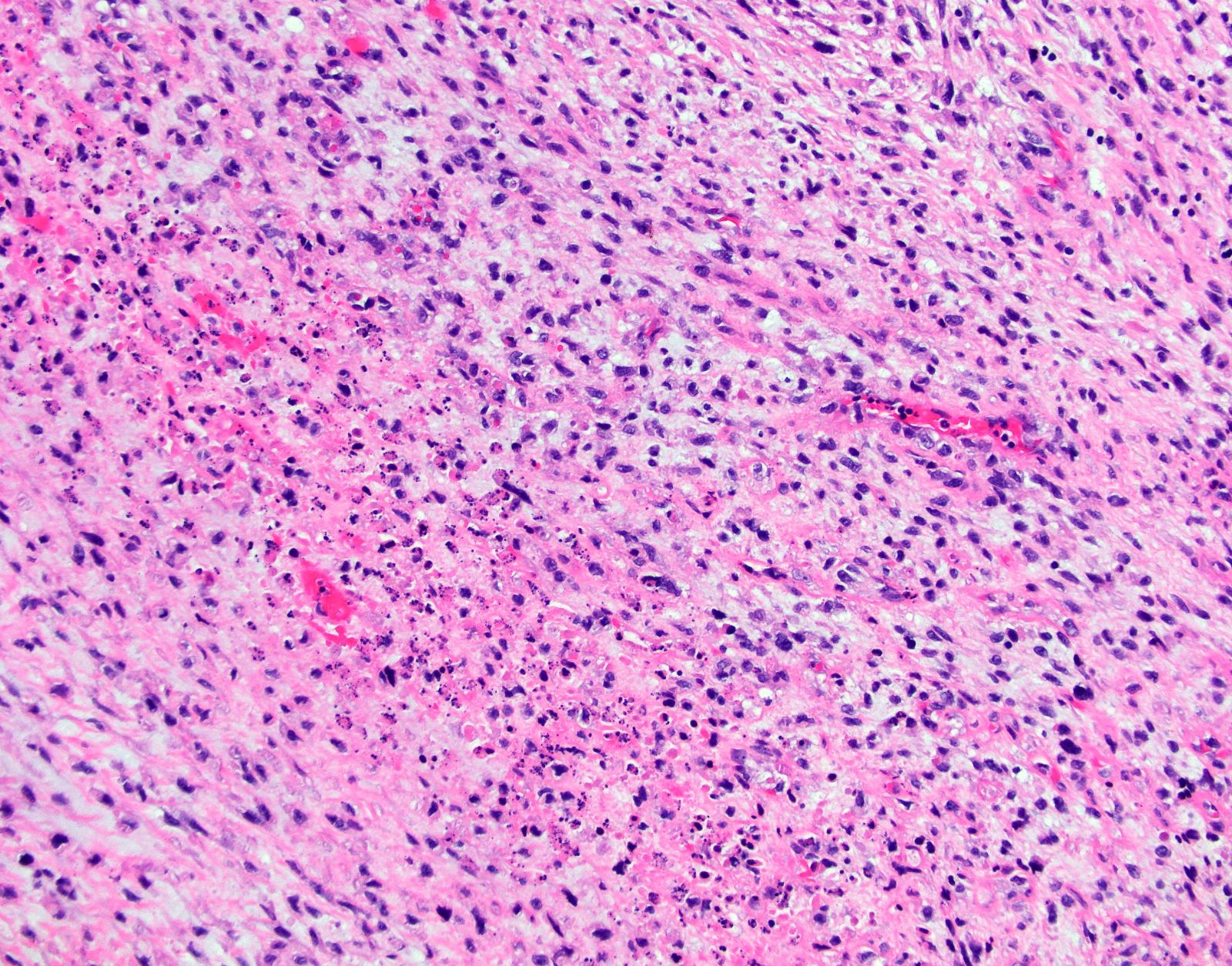
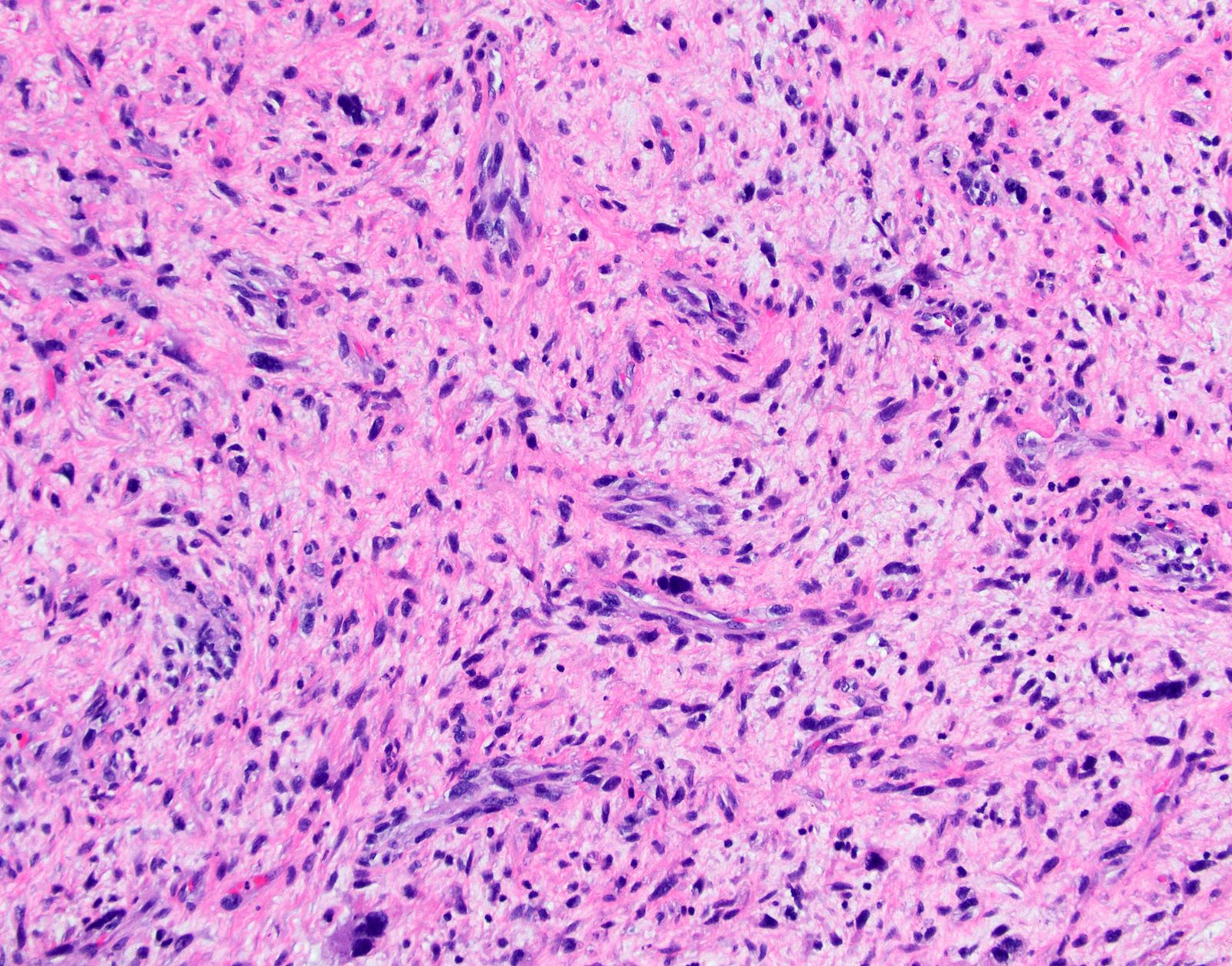
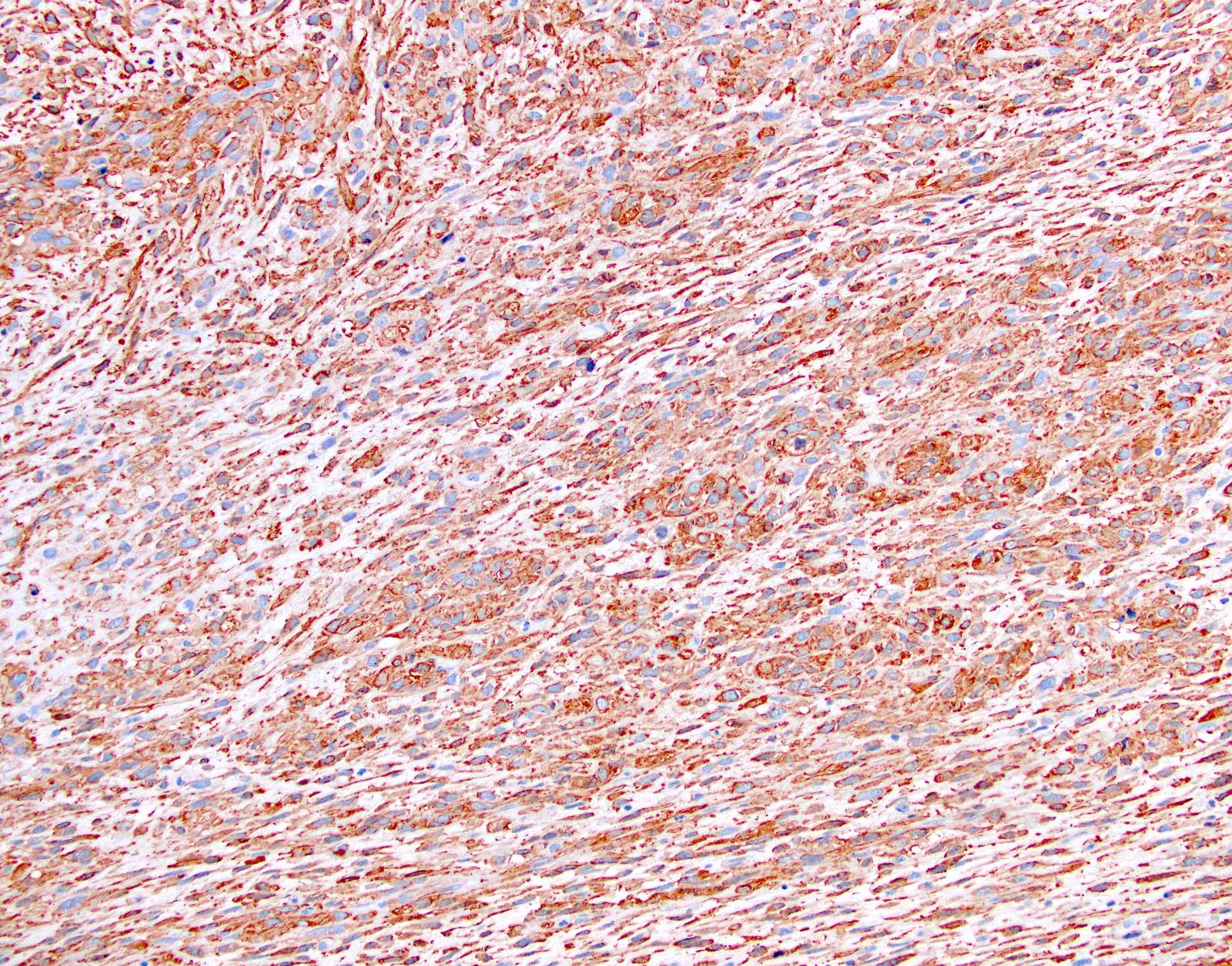
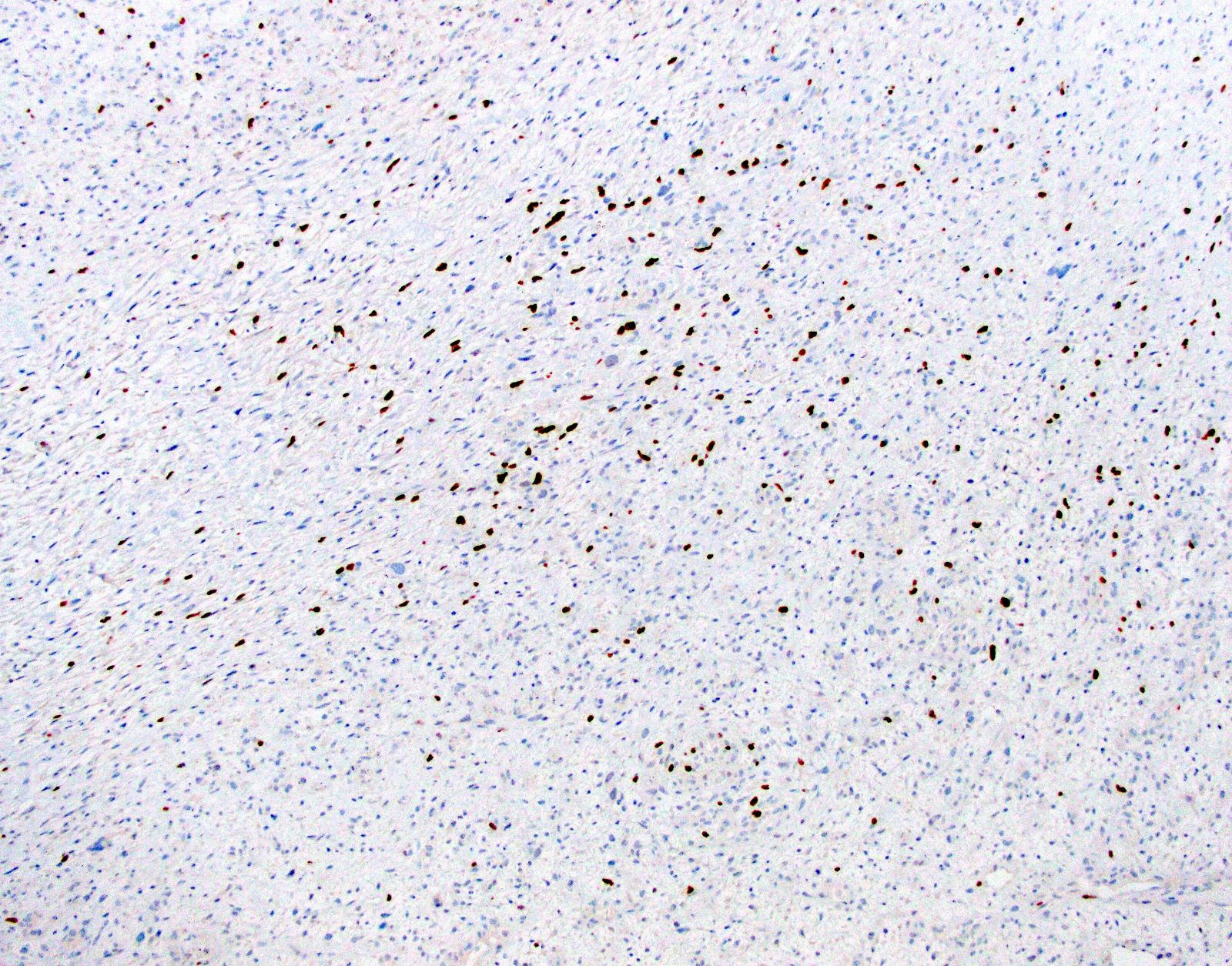
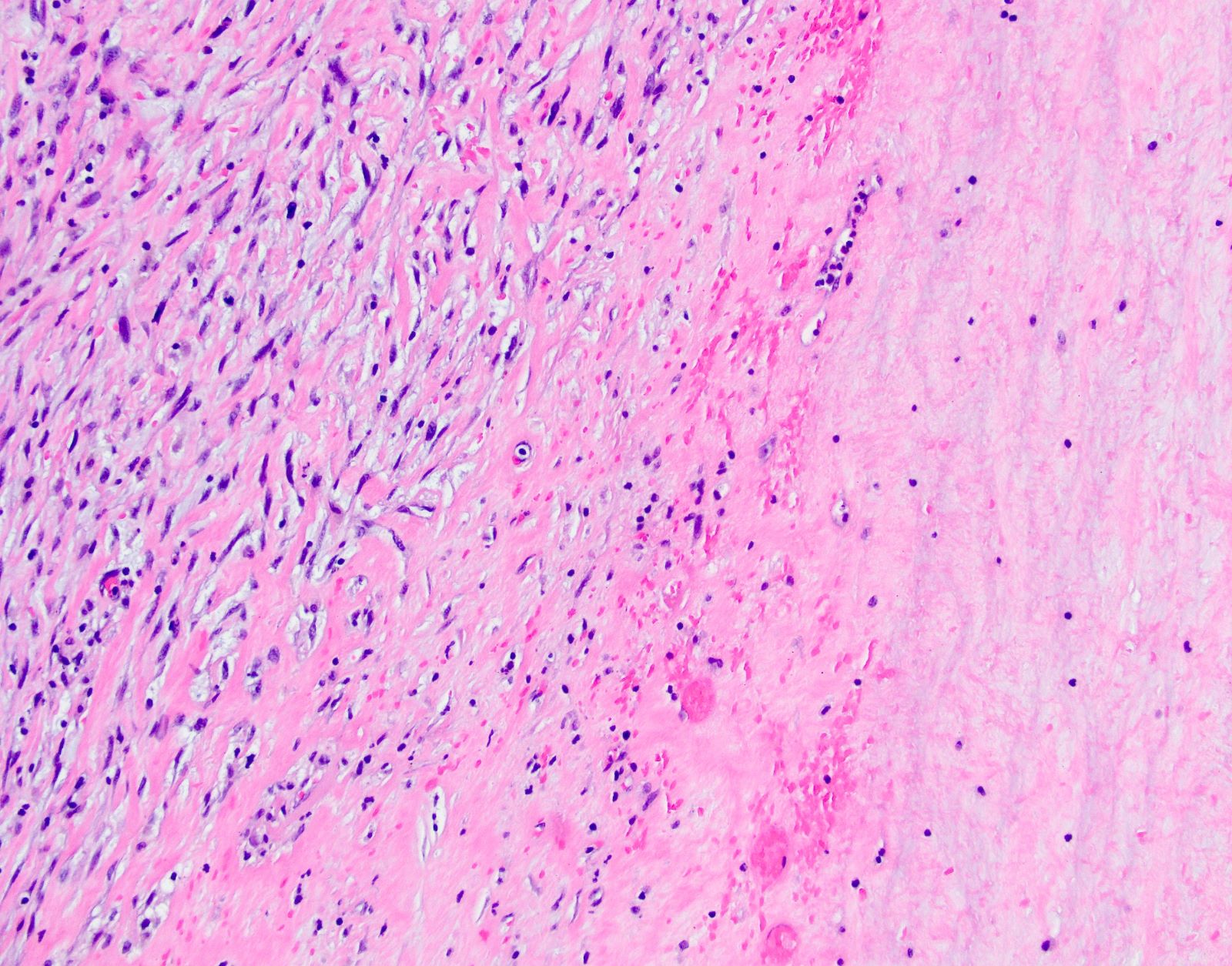
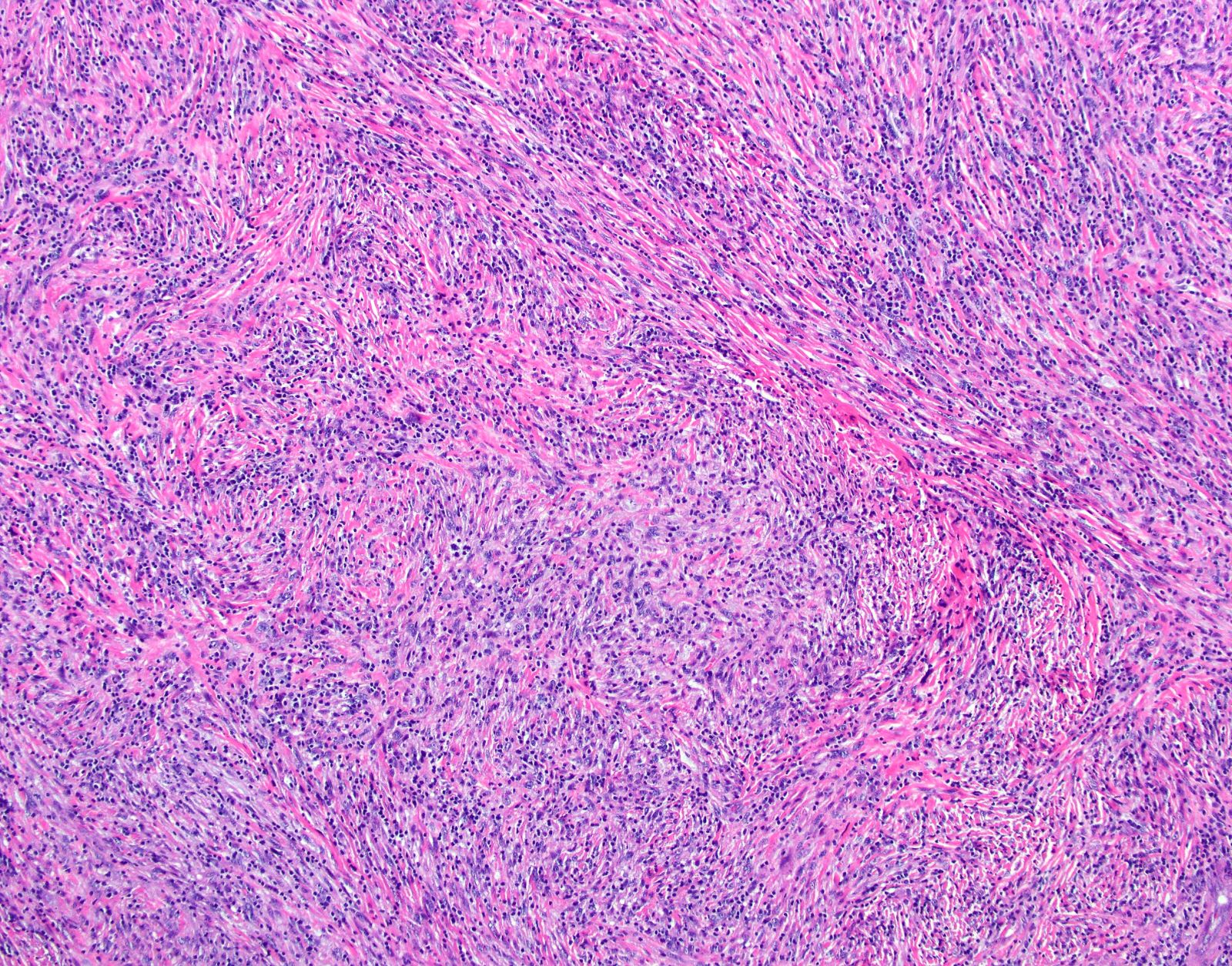
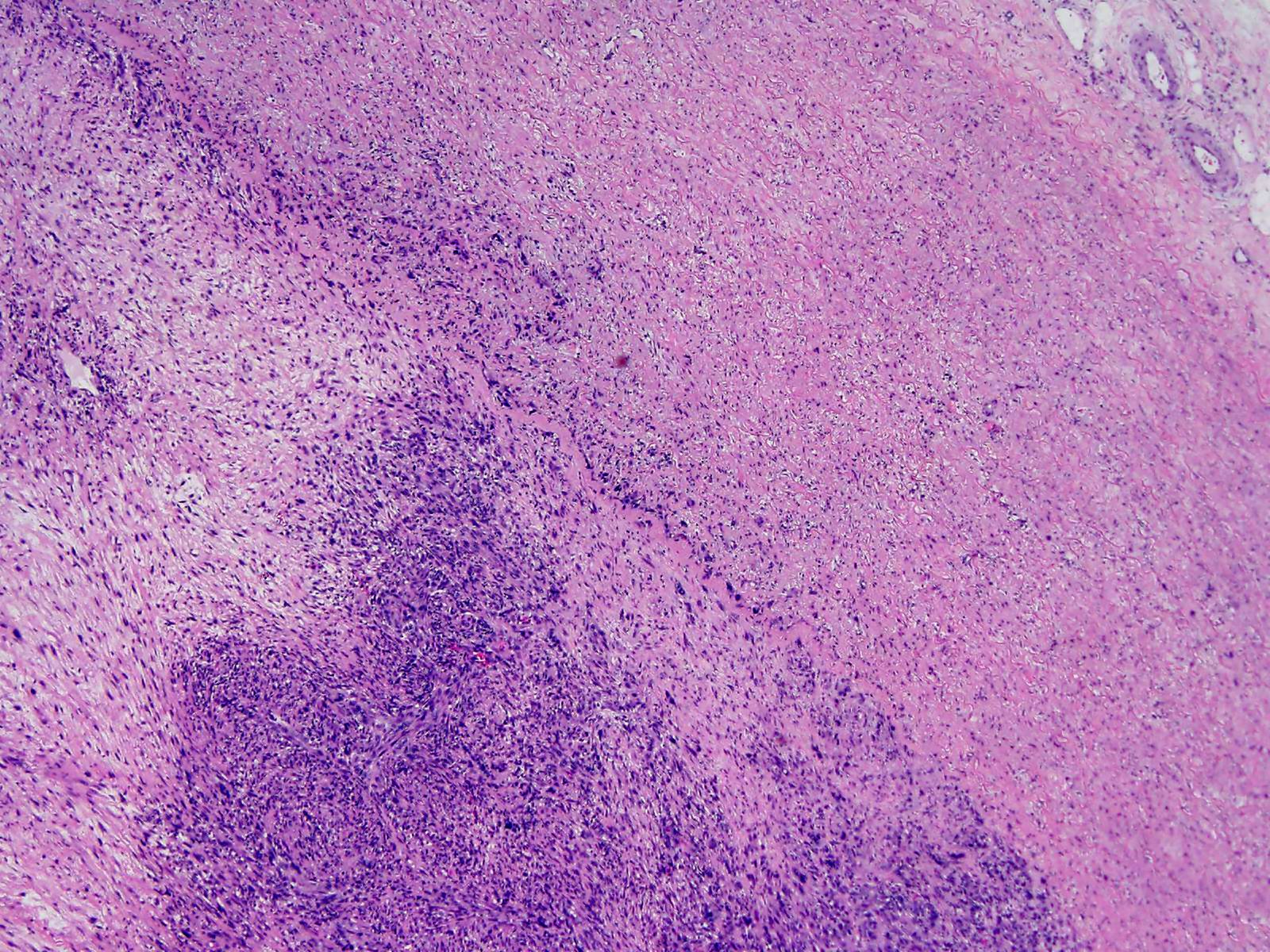
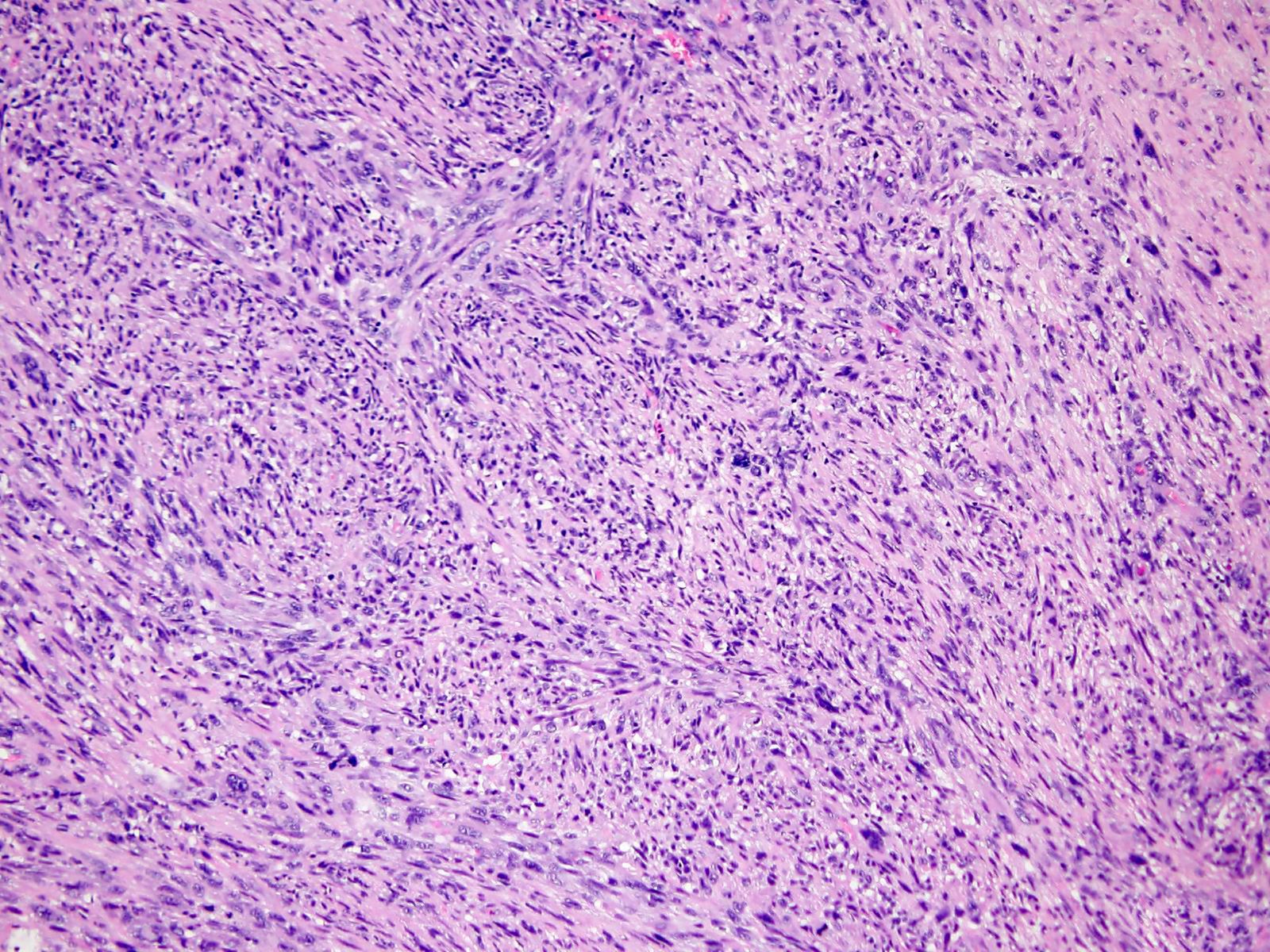
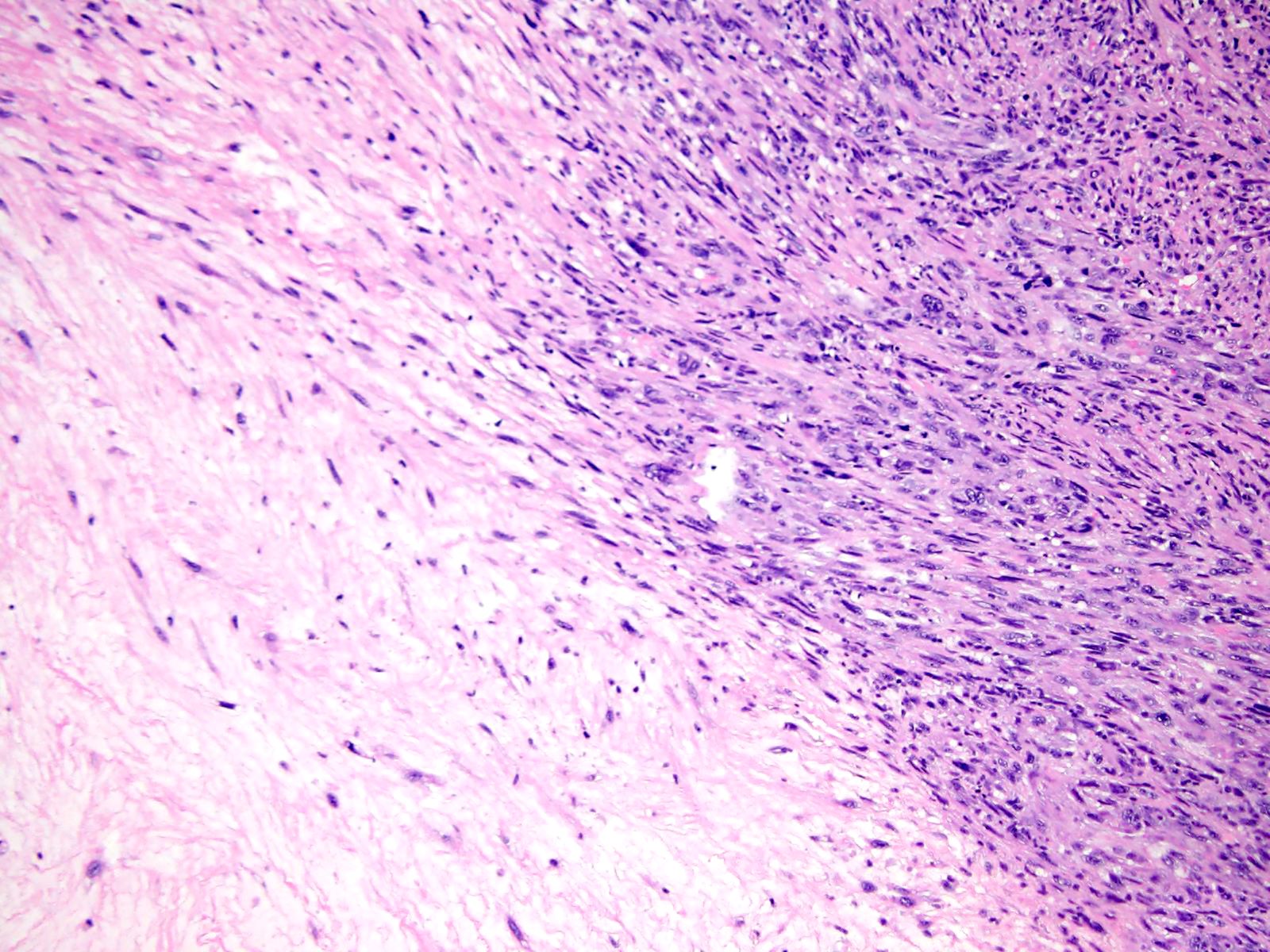
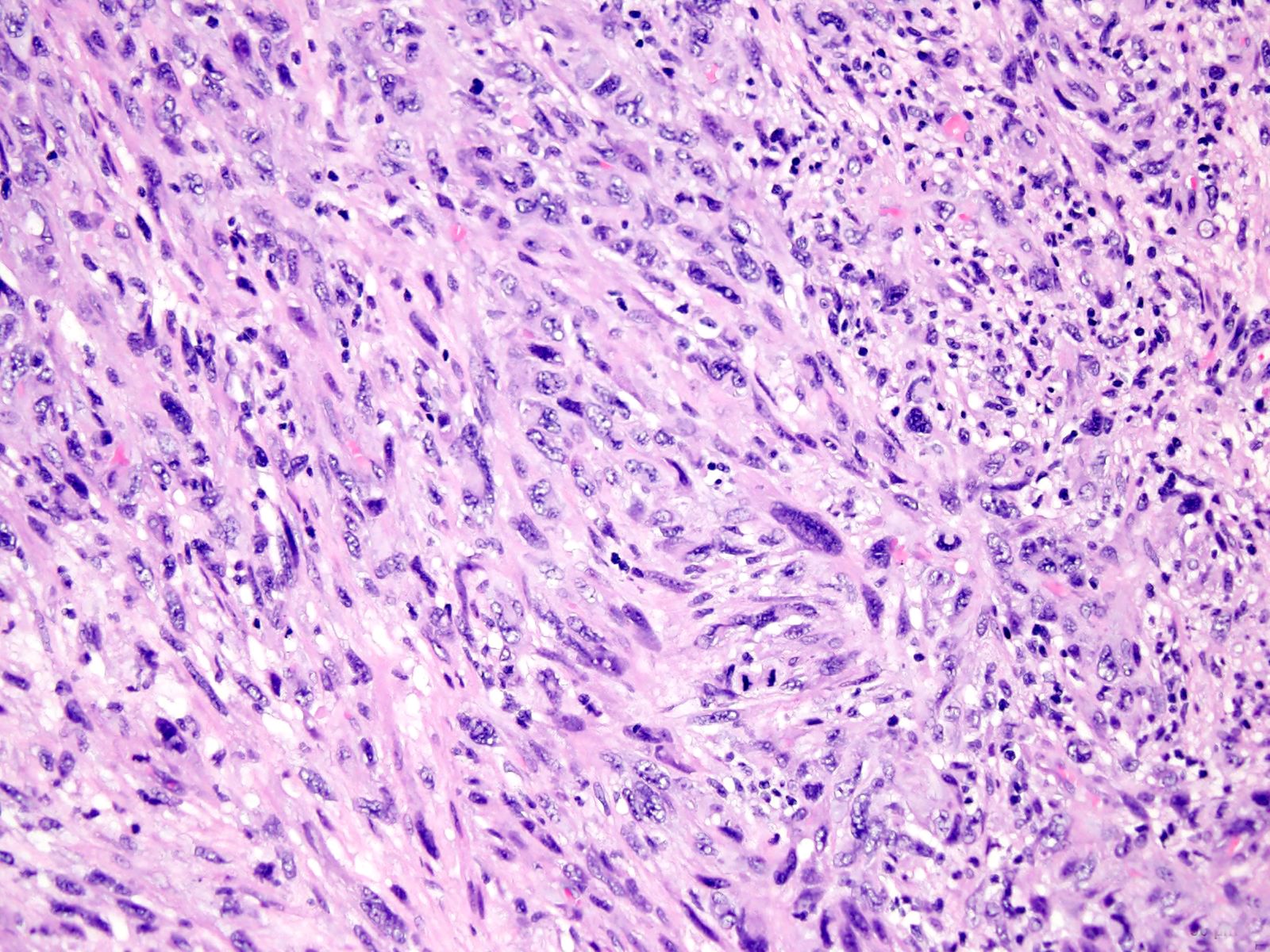
Microscopic (histologic) description
- Mesenchymal spindle cell neoplasm
- Variable atypia
- Variable cellularity
- Hyperchromatic nuclei
- Irregular nuclear membranes
- High grade component: high mitotic count, necrosis and more severe nuclear pleomorphism
- Low grade component: lower cellularity and myxoid areas
- With or without epithelioid morphology
- With or without heterologous element: osteosarcoma, chondrosarcoma, rarely rhabdomyosarcoma or angiosarcoma
- References: Case Rep Oncol 2016;9:267, CJC Open 2020;2:711, World J Clin Cases 2021;9:3960, Respirol Case Rep 2020;8:e00530, Case Rep Oncol 2021;14:318, Radiographics 2021;41:361, Medicine (Baltimore) 2021;100:e24699, Intern Med 2019;58:3599, Case Rep Pulmonol 2021;2021:5573869
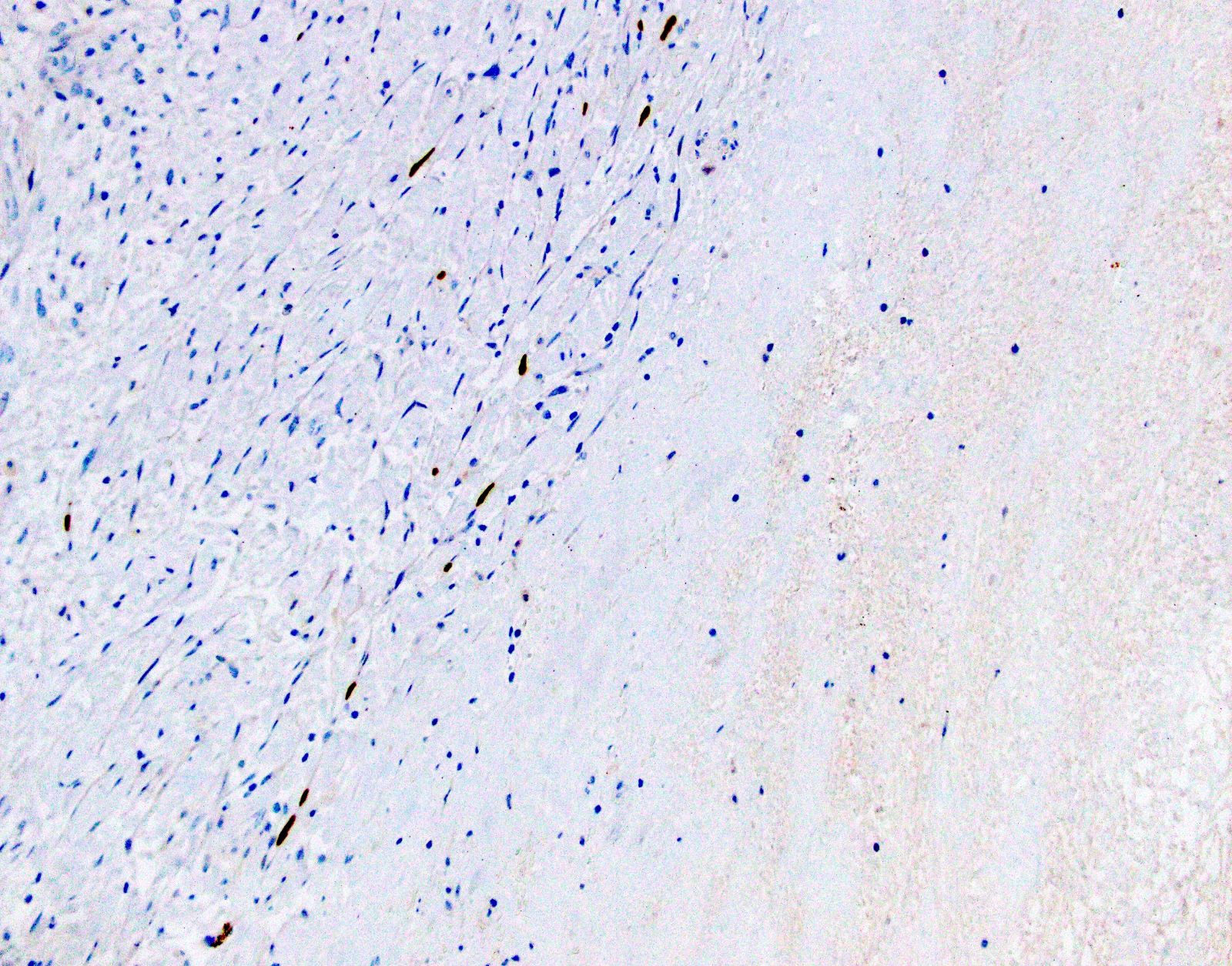
Microscopic (histologic) images
Cytology description
- Pleomorphic malignant spindle cells
- Loosely cohesive clusters of tumor cells
- Reference: Cytojournal 2015;12:3
Cytology images
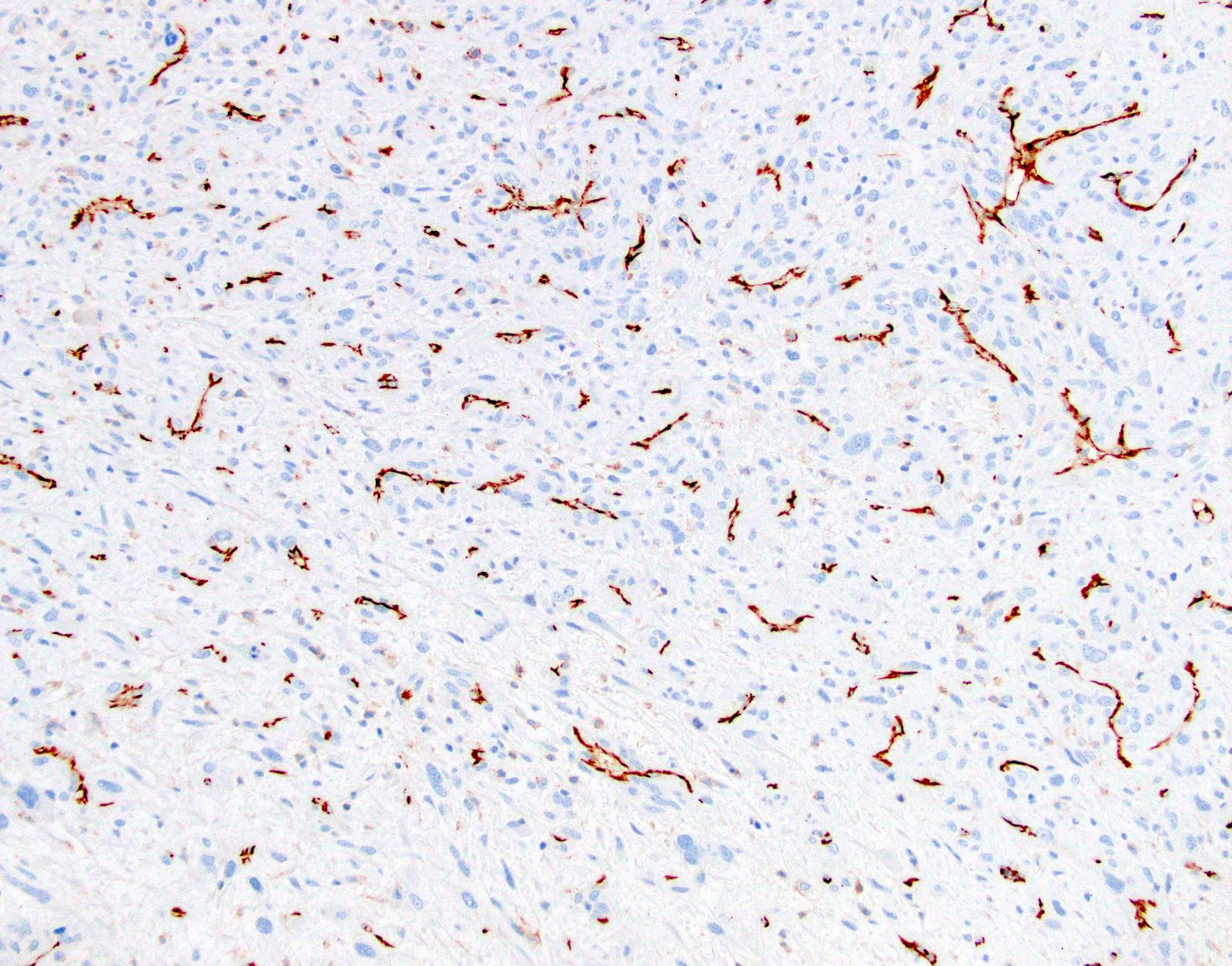
Positive stains
- Diagnosis does not require immunohistochemistry
- Variable expression:
- Elastic stain is helpful to identify invasion through arterial wall
- References: Case Rep Oncol 2016;9:267, CJC Open 2020;2:711, Respirol Case Rep 2020;8:e00530, Case Rep Pulmonol 2021;2021:5573869
Negative stains
- Keratin (AE1 / AE3, CAM5.2)
- S100
- Desmin
- CD68
- STAT6
- CD34
- Beta catenin
- ALK
- References: Medicine (Baltimore) 2021;100:e24699, Case Rep Pulmonol 2021;2021:5573869
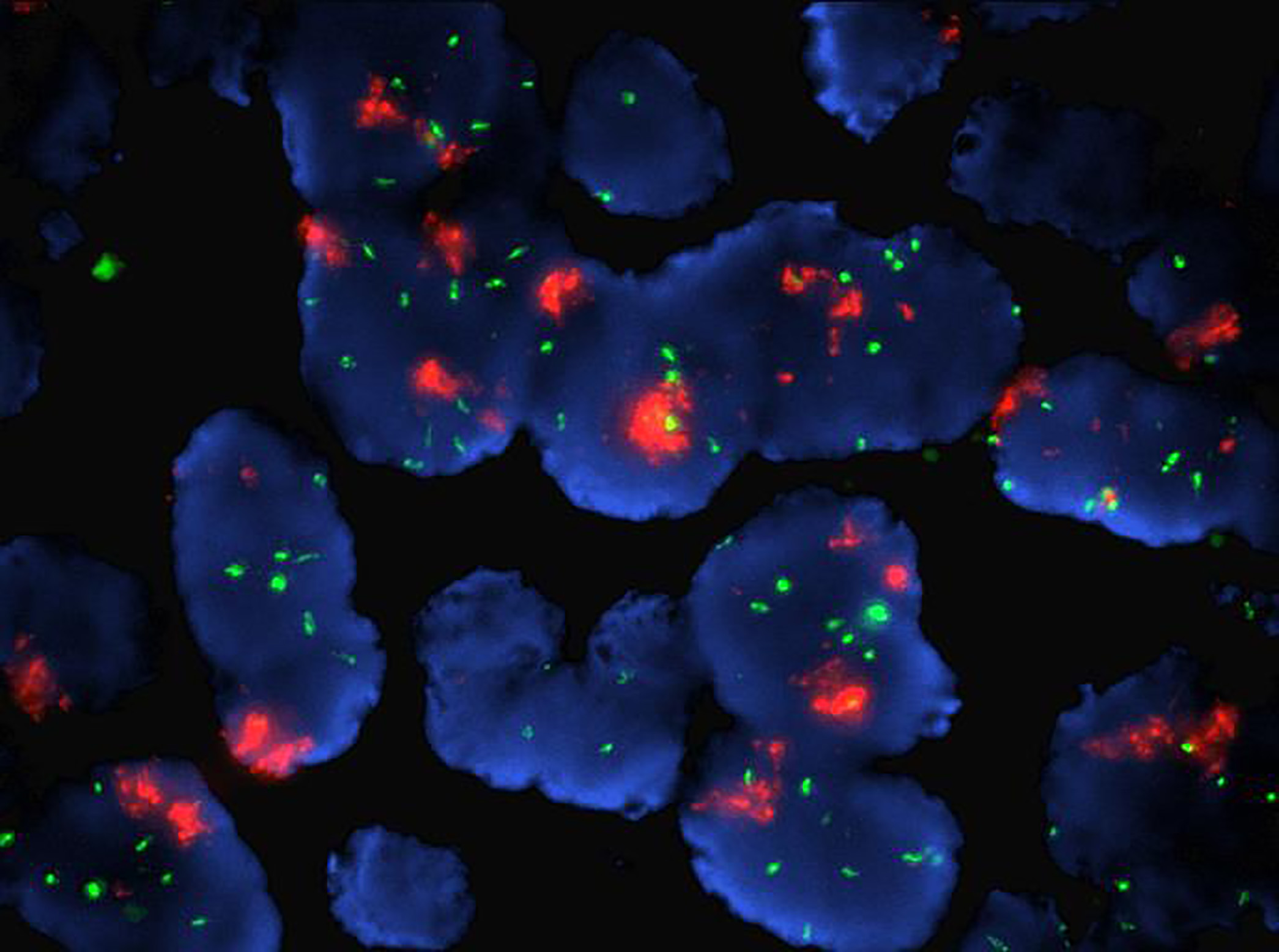
Molecular / cytogenetics description
- MDM2 gene amplification: most important in diagnosis
- Alterations have been reported in 12q12–15, 4q12, 7p12, 9p21, leading to changes or amplification of MDM2, CDK4, SAS, PDGFRA, EGFR, TERT, KIT, KDR, NOTCH2, ERBB3, GLI, VEGFR2, FBXW7, FAT3 or FANCM
- In one study, by FISH, 81% of intimal sarcomas had PDGFRA amplification, 65% had MDM2 amplification and 76% had EGFR amplification
- Cardiac intimal sarcomas from the left atrium tends to show MDM4 and CDK6 amplifications; they lack MDM2 amplification
- References: Mod Pathol 2021;34:2122, Pathol Res Pract 2021;224:153548, Zhonghua Bing Li Xue Za Zhi 2020;49:816, J Thorac Dis 2019;11:S9
Molecular / cytogenetics images
Sample pathology report
- Mass, pulmonary artery, excision:
- Intimal sarcoma (see comment)
- Comment: The sections show a spindle cell proliferation arranged in fascicles, with hyperchromatic pleomorphic nuclei. The lesion invades the media of the artery (supported by elastic stain). The sections also reveal areas of necrosis, consisting of > 50% of the submitted specimen. The mitotic activity is 12 mitoses/10 high power fields. The tumor cells are positive for SMA, vimentin and CD31; negative for cytokeratin, desmin, myogenin, CD34, beta catenin and STAT6. MDM2 immunohistochemistry shows positivity in the tumor nuclei. FISH study shows MDM2 and CDK4 amplification. The histologic, immunohistochemical and molecular findings are consistent with a diagnosis of intimal sarcoma.
Differential diagnosis
- Lung thromboemboli:
- Fibrin with or without organization, platelets (CD61+)
- Lines of Zahn
- History of risk factors for thromboembolism
- No atypical spindle cells, mitosis or necrosis
- Lung infarct:
- Gross: wedge shaped area of hemorrhagic or tan lung parenchyma
- Histology: no atypical spindle cells or mitosis
- Sarcomatoid carcinoma:
- Atypical spindle cells with mitoses or necrosis
- Epithelioid cells may be present
- Cytokeratin positive (may be focal)
- Metastatic sarcoma from another organ:
- Atypical spindle cells with mitoses or necrosis
- History, immunohistochemical stains, molecular studies and previous pathology are helpful to differentiate
Additional references
Board review style question #1
A 50 year old woman, who completed a long distance flight the previous week, came to the ER with chest pain and breathlessness. D dimer level was elevated. CT scan with contrast showed a large filling defect in the left pulmonary artery. She was started on anticoagulation therapy but did not improve. PET / CT showed that the left pulmonary artery mass was FDG avid. The lesion was resected and the pathology revealed the findings shown above. Immunostains showed that the cells were positive for SMA and CD31 and negative for AE1 / AE3. What is the diagnosis?
- High grade sarcoma, consistent with intimal sarcoma
- Metastatic carcinoma
- Sarcomatoid carcinoma
- Thromboembolus
Board review style answer #1
A. High grade sarcoma, consistent with intimal sarcoma
Comment Here
Reference: Pulmonary artery intimal sarcoma
Comment Here
Reference: Pulmonary artery intimal sarcoma
Board review style question #2
A malignant spindle cell tumor is seen arising from the intimal layer of the pulmonary artery. Immunostains showed that the tumor cells were positive for SMA and CD31 and negative for AE1 / AE3. The provisional diagnosis was pulmonary artery intimal sarcoma. What is the most common molecular alteration seen in this entity?
- ETV6::NTRK3
- EWSR1::FLI1
- FUS::CREB3L2
- MDM2 amplification
Board review style answer #2