Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Wu R. Mucoepidermoid carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumormucoepidermoid.html. Accessed April 1st, 2025.
Definition / general
- Low grade or high grade salivary gland type tumor with mucous secreting cells, squamous cells and intermediate cells
- Distinguished from other lung cancers by central or peribronchial location, mucous cells, lack of keratinization, expression of p63 and MAML2 rearrangement (Mod Pathol 2014;27:1479)
Essential features
- Most common salivary gland type tumor in the lung, tends to arise centrally
- Similar morphology to mucoepidermoid carcinoma arising in the head and neck with a mixture of mucous cells, squamous cells and intermediate cells; must exclude metastasis
- Strong association with t(11;19)(q21;p13) and MAML2 rearrangement by fluorescence in situ hybridization (FISH)
- Squamous component stains with p63 and p40
Terminology
- Same diagnostic terminology as used in the salivary gland
ICD coding
Epidemiology
- 0.1 - 0.2% of primary lung tumors (J Thorac Cardiovasc Surg 1978;76:431) and 9 - 18% in the pediatric population (J Surg Res 2009;156:224, J Pediatr Surg 2015;50:1004)
- May occur in any age group; many cases reported in pediatric population
- Most common of the primary salivary gland type tumors of the lung but still rare
Sites
- Any lung lobe, usually in relation to large bronchi
Pathophysiology
- Usually considered to have low malignant potential with recurrences; more aggressive when high grade (Int J Clin Exp Pathol 2014;7:6792)
- Most tumors are low stage and low to intermediate grade rather than high grade (J Thorac Oncol 2013;8:1578)
Etiology
- May arise from submucosal bronchial glands
Clinical features
- Large central tumors cause obstructive symptoms such as dyspnea, cough, hemoptysis or pneumonia
- Peripheral lesions may be asymptomatic
Diagnosis
- Bronchoscopy may be used to directly visualize and sample an endobronchial tumor
- Diagnosis may be difficult in small biopsies; may mimic primary non small cell lung carcinoma
Radiology description
- Can be difficult to detect on imaging due to small size of tumor, endobronchial location, association with pneumonia or atelectasis (Arch Pathol Lab Med 2007;131:1400)
- On CT, markedly enhanced homogeneous central bronchial nodule / mass suggests low grade mucoepidermoid carcinoma (MEC); high grade MEC tends to be peripheral with poorly defined margins, lobular, heterogeneous with less enhancement (AJR Am J Roentgenol 2015;205:1160)
- Uncommon findings included cavitation, diffuse thickening or spiculation (Clin Imaging 2012;36:8)
Radiology images
Prognostic factors
- Excellent prognosis after surgical removal (Thorac Cardiovasc Surg 2014;62:140, Asian Cardiovasc Thorac Ann 2016;24:257)
- Age, stage, margin status and pathological grade related to overall survival and disease free survival (J Thorac Oncol 2013;8:1578 , Int J Clin Exp Pathol 2014;7:6792)
Case reports
- 22 year old man with tumor in the medial segment of the right lower lobe (Diagn Pathol 2012;7:137)
- 26 year old man with chronic cough and an endobronchial lesion (Respir Med Case Rep 2013;9:18)
- 38 year old woman with mild fever and dry cough (Oxf Med Case Reports 2015;2015:203)
- 40 year old man with dry cough (Asian Cardiovasc Thorac Ann 2015;23:988)
- 46 year old woman with dyspnea on exertion (Case Rep Oncol Med 2013;2013:625243)
- 58 year old man with shortness of breath, dysphagia and weight loss (Ann Clin Lab Sci 2015;45:219)
- 58 year old woman with mixed adenocarcinoma and mucoepidermoid carcinoma (Ann Thorac Surg 2014;98:695)
Treatment
- Complete surgical excision (Int J Clin Exp Pathol 2014;7:6792)
- High grade tumors may require additional treatment, although chemotherapy and radiation controversial (World J Surg Oncol 2014;12:33)
Gross description
- Polypoid, exophytic growth or sessile tumor in major bronchi, may be > 5 cm
- Generally well circumscribed and smooth with tan to yellow cut surface
- May be solid or cystic and potentially show glistening mucoid material
Gross images
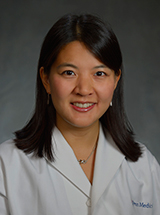
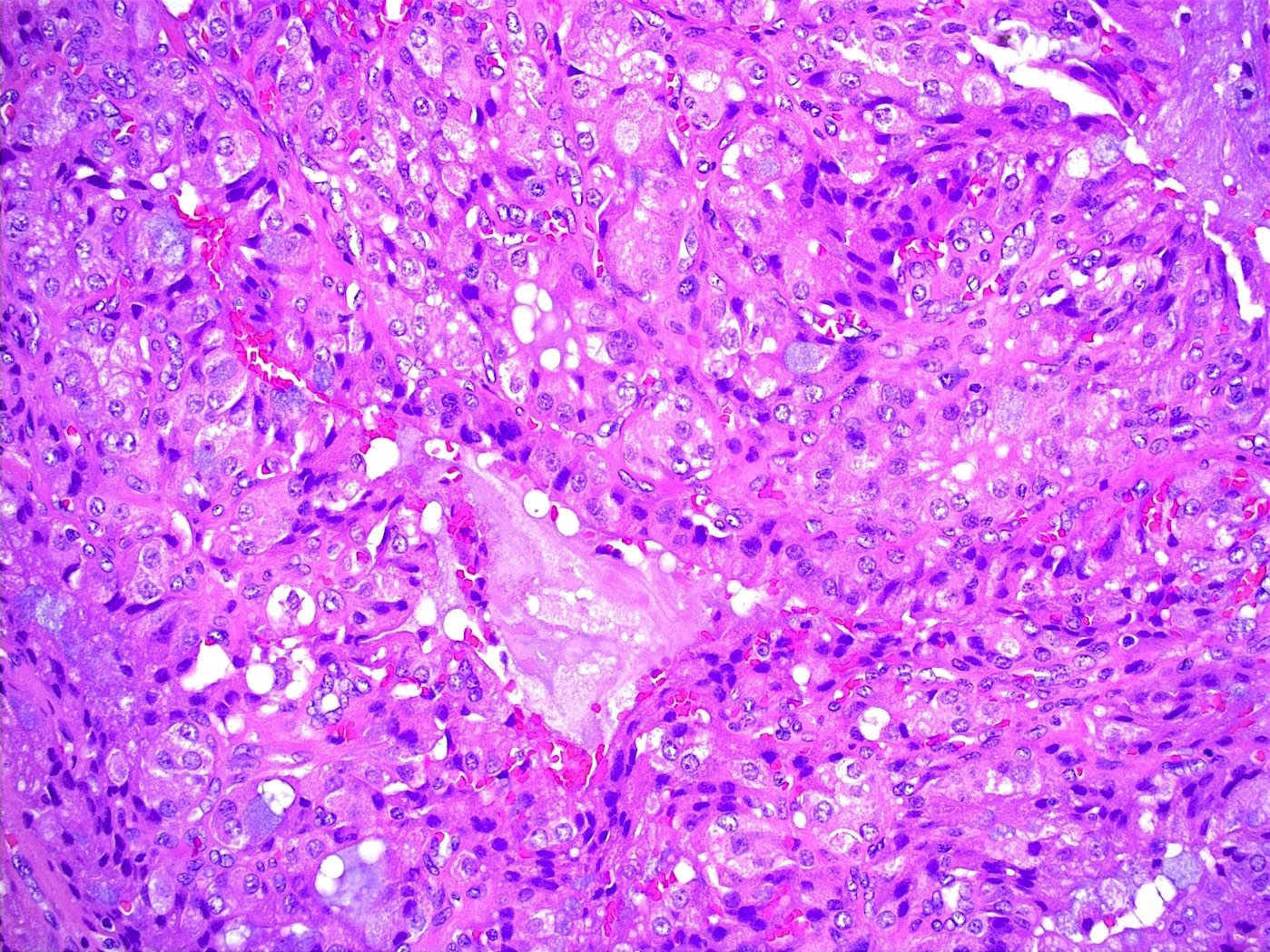
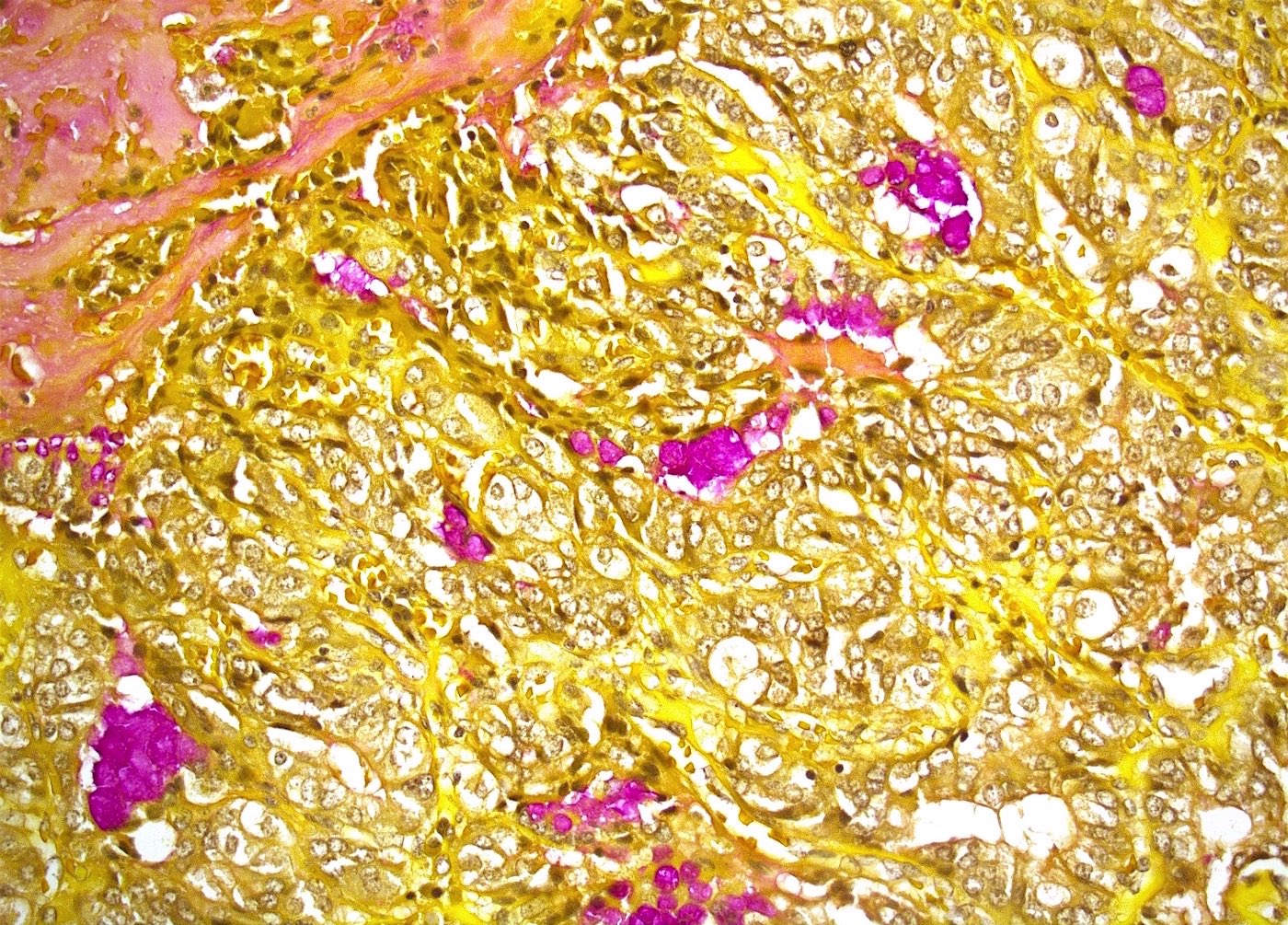
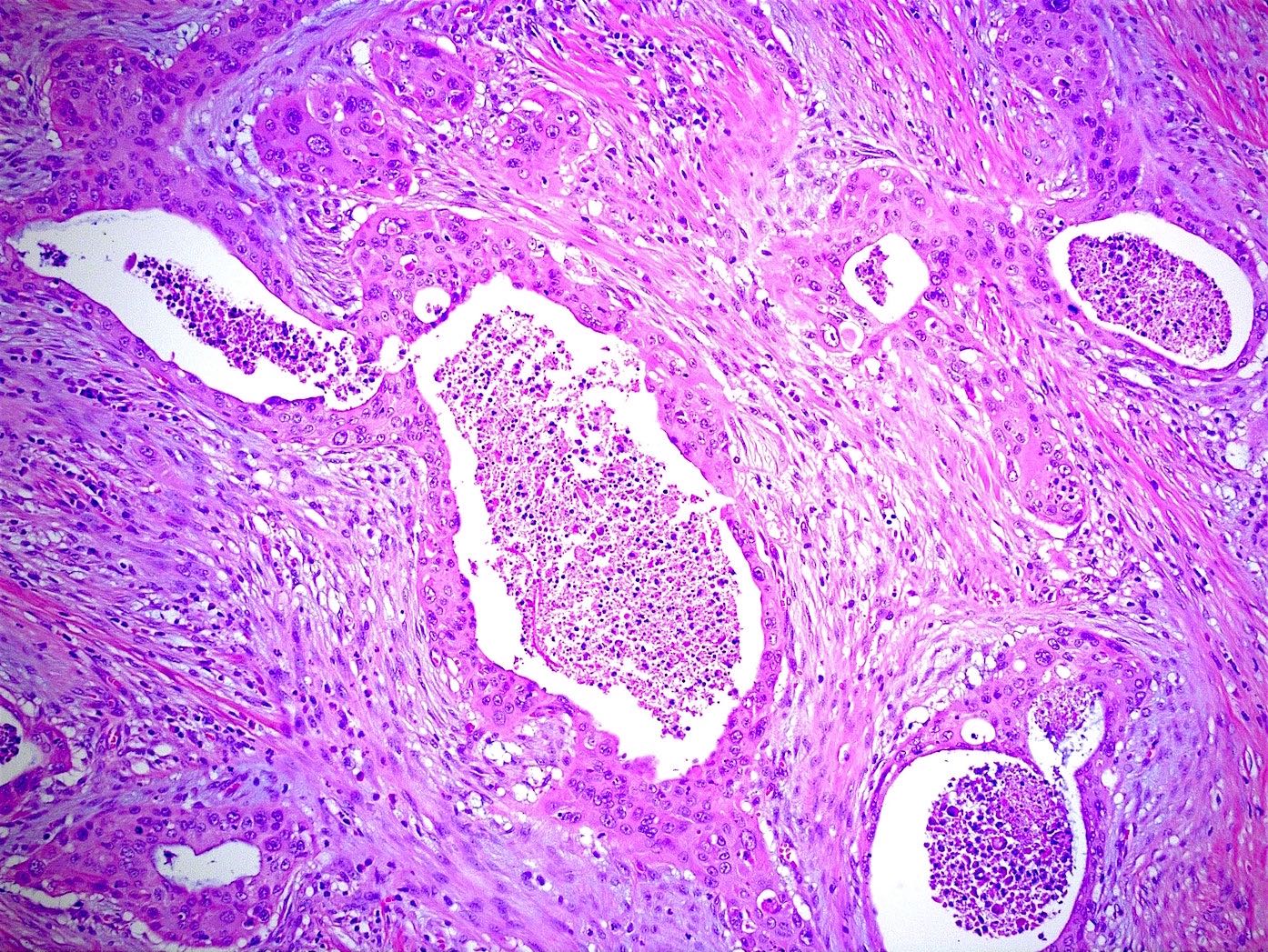
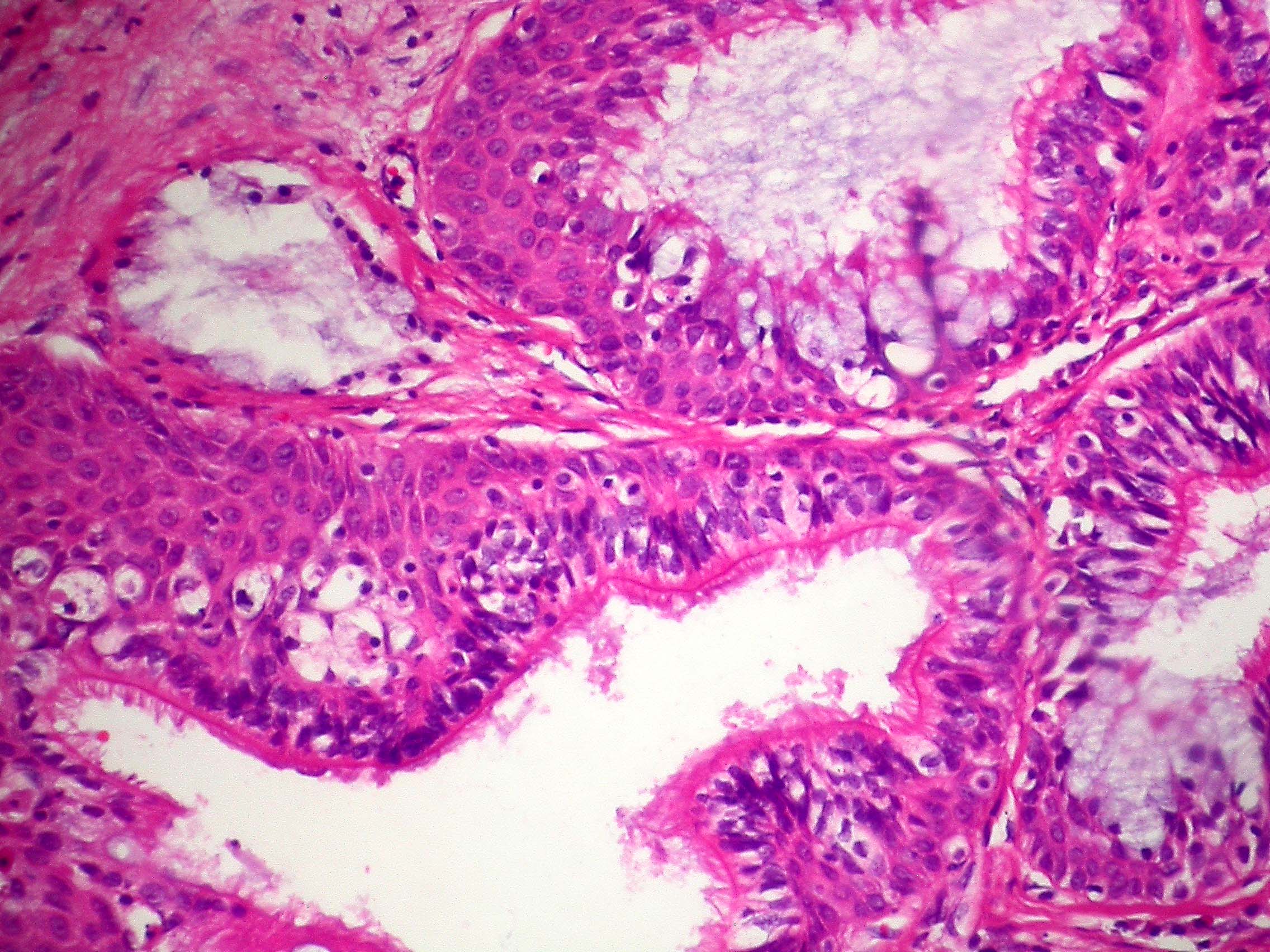
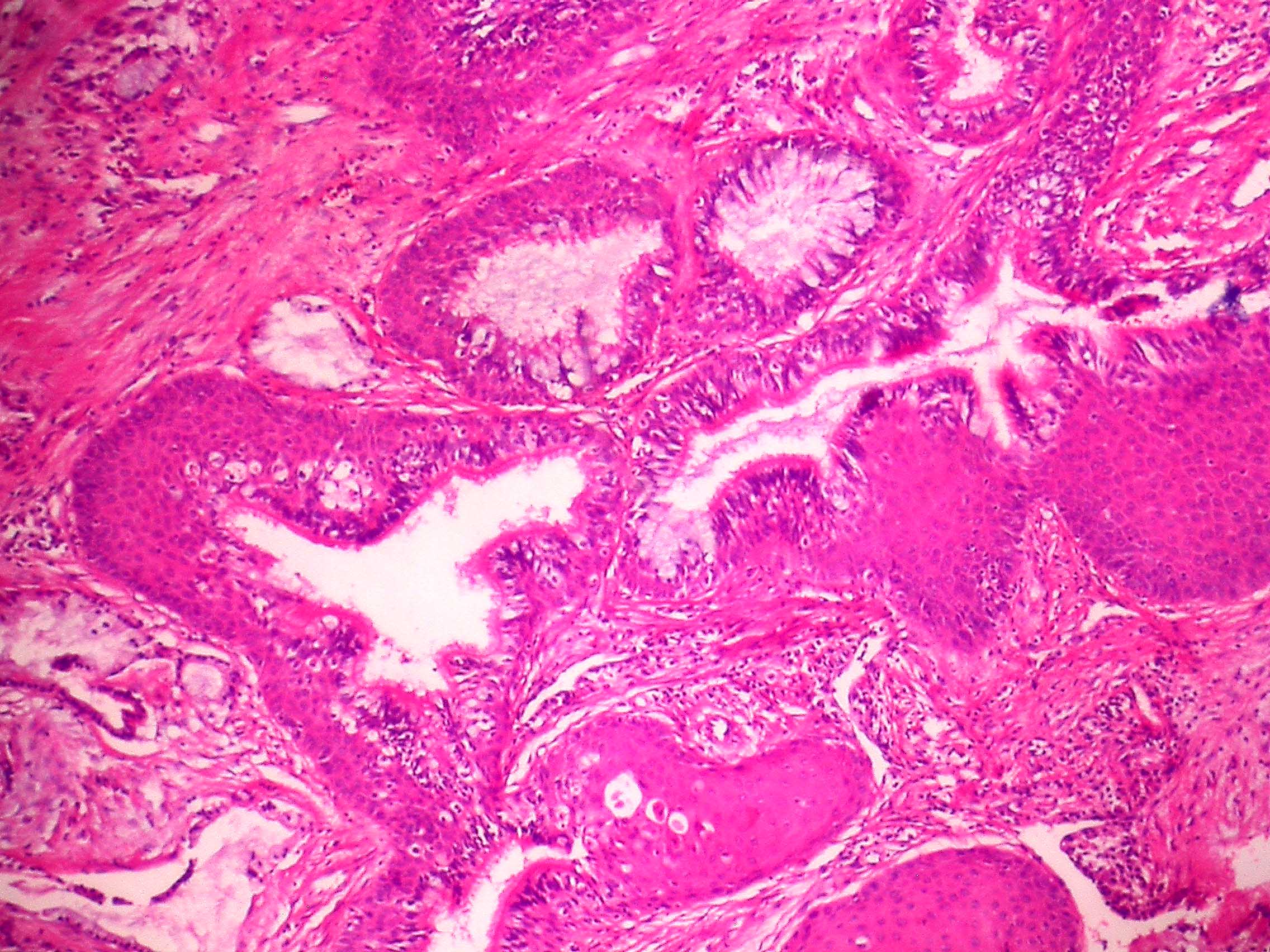
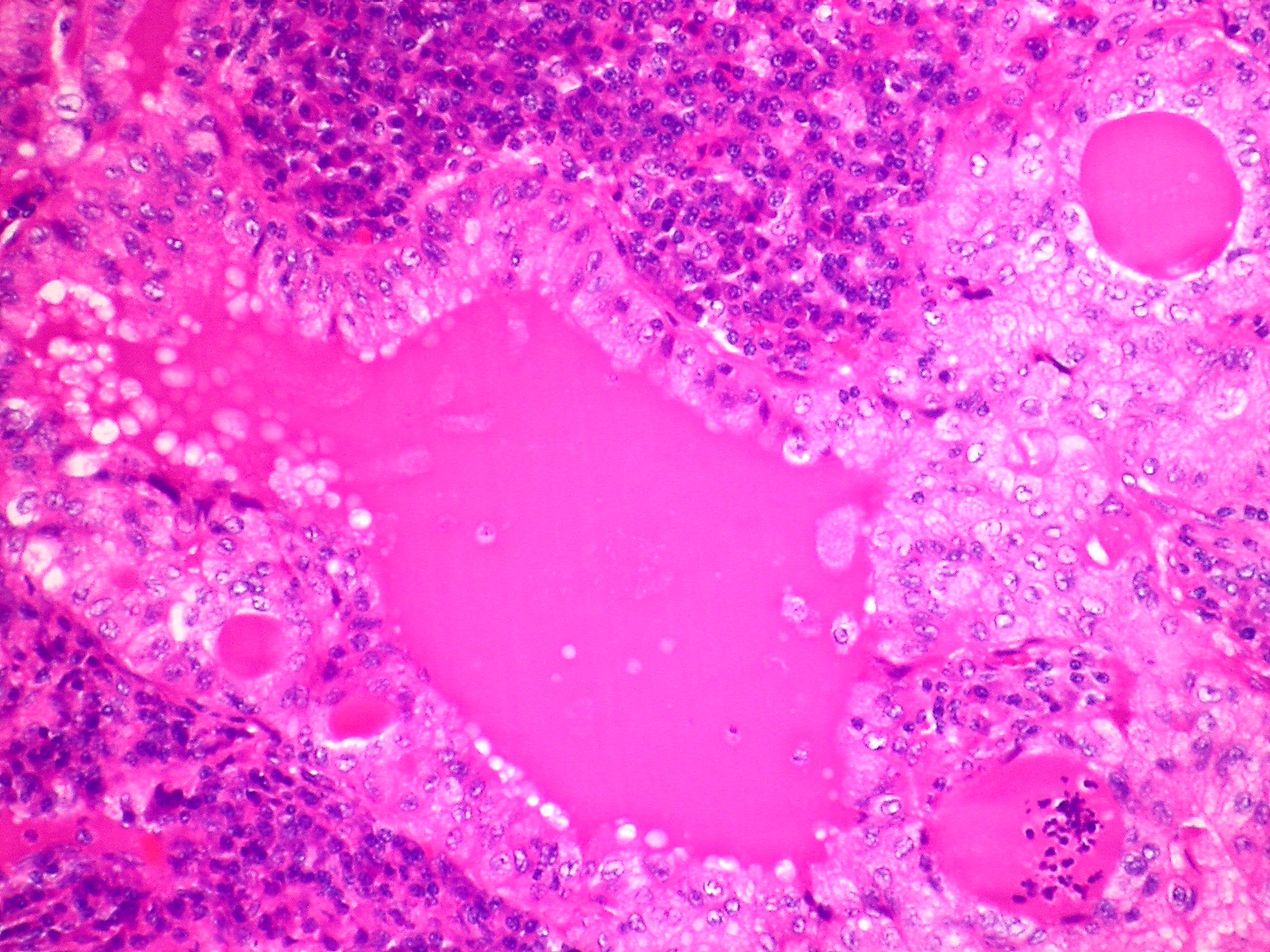
Microscopic (histologic) description
- Low grade has more cysts and mucous cells; high grade has more solid or nested growth, atypia, mitotic activity, necrosis, hemorrhage
- Mucus secreting cells, squamoid cells without significant keratinization, intermediate type cells
- Mucus secreting cells usually large with light blue-gray mucinous cytoplasm; variants include columnar, goblet, cuboidal, clear or oncocytic cells (Arch Pathol Lab Med 2007;131:1400)
- Squamous cells show intercellular bridges but no keratin whorls or pearls; intermediate cells usually polygonal with bland nucleus (Arch Pathol Lab Med 2007;131:1400)
- May show areas of papillary growth or spindled cells
- May have dense lymphoplasmacytic infiltrate (Am J Surg Pathol 2005;29:407)
- Lack in situ carcinoma of overlying epithelium
Microscopic (histologic) images
Contributed by Roseann Wu, M.D., M.P.H. and Yale Rosen, M.D.
Images hosted on other servers:
Virtual slides
Cytology description
- Mixture of squamoid cells, mucous cells and intermediate cells
- Diff-Quik with numerous tight clusters of relatively small and bland cells with well defined but scant cytoplasm, central round and uniform nuclei with small nucleoli; second population of glandular appearing cells with cytoplasmic vacuoles with mucin, focal extracellular metachromatic mucinous material (Diagn Cytopathol 2013;41:1096)
Molecular / cytogenetics description
- MAML2 rearrangement most common molecular genetic event, found more in low grade tumors (PLoS One 2015;10:e0143169)
- May stain with epidermal growth factor receptor (EGFR) but does not show the mutation or alterations in copy number (Mod Pathol 2008;21:1168)
- Reciprocal translocations, including t(1;11)(p22;q13) with overexpression of cyclin D1, t(11;19)(q14-21;p12) and t(11;19)(q21;p13) which encodes MECT1-MAML2 (MECT1 also known as CRTC1) (Arch Pathol Lab Med 2007;131:1400)
Differential diagnosis
- Adenocarcinoma: lacks squamous and intermediate cells; TTF1+
- Adenosquamous carcinoma: usually peripheral in lung, not centered on bronchi; large tumors, no intermediate cells, contains adenocarcinoma component
- Metastatic renal cell carcinoma: more monotonous with foamy or eosinophilic cytoplasm; CK7-
- Mucous gland adenoma: confined to luminal aspect and not invasive; TTF1+
- PEComa: lacks mucin as well as squamous and intermediate cells; HMB45+
- Squamous cell carcinoma: may show more keratinization and lacks mucin
Additional references
- Cytomorphology of salivary gland type tumors in the lung and mediastinum (Diagn Cytopathol 2012;40:1062)
Board review style question #1
- Rearrangement of which gene would support the diagnosis of mucoepidermoid carcinoma of the lung?
- APC
- BRAF
- MAML2
- PIK3CA
- PLAG1
Board review style answer #1