Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Pathophysiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Wu R. Micronodular pneumocyte hyperplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumormicronodpneumohyper.html. Accessed November 30th, 2024.
Definition / general
- First recognized in 1991 by HH Popper (Histopathology 1991;18:347)
- Benign, hamartomatous, multinodular proliferation of type II pneumocytes
- Often associated with tuberous sclerosis complex
- May coexist with lymphangioleiomyomatosis (LAM)
Essential features
- Rare pulmonary manifestation of tuberous sclerosis complex that may occur in conjunction with LAM
- Composed of multiple nodules of enlarged but benign type II pneumocytes that may mimic atypical adenomatous hyperplasia
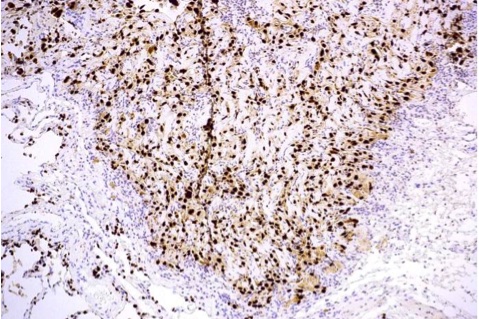
- Positive for cytokeratins and TTF1 by immunohistochemical stains, while negative for SMA
Terminology
- Also called multifocal micronodular pneumocyte hyperplasia (MMPH)
- Older terminology: acinar atypical adenomatoid proliferation of epithelium, multiple adenomatoid lesions, micronodular hyperplasia of type II pneumocytes
Epidemiology
- Young and middle aged adults, predominantly women
- Often associated with tuberous sclerosis complex but may be sporadic
Pathophysiology
- Functional loss of TSC 1 or TSC2 and hyperphosphorylation of mTOR related protein may cause this benign neoplastic proliferation of pneumocytes (Mod Pathol 2010;23:1251)
Clinical features
- Non-specific; may present with pneumothorax, shortness of breath, cough
Diagnosis
- Histologic examination
Radiology description
- Xray: multiple pulmonary nodules
- CT: multiple diffuse, small, solid and ground glass pulmonary nodules that remain stable in short term follow-up (J Comput Assist Tomogr 2012;36:518)
- Imaging may mimic miliary tuberculosis (Int J Clin Exp Pathol 2015;8:2165)
Prognostic factors
- Typically indolent with no clinical significance
- Rare case studies report respiratory failure
Case reports
- 13 year old girl with tuberous sclerosis, renal cell carcinoma, angiomyolipomas and multifocal micronodular pneumocyte hyperplasia (Chem Pharm Bull (Tokyo) 1990;38:498)
- 16 year old girl with respiratory failure (Histopathology 2002;41:263)
- 51 year old woman with tuberous sclerosis complex but no classical clinical findings (J Med Case Rep 2012 Oct 16;6:352)
Gross description
- Small (1 - 10 mm), well-demarcated, randomly distributed parenchymal lung nodules
Gross images
Microscopic (histologic) description
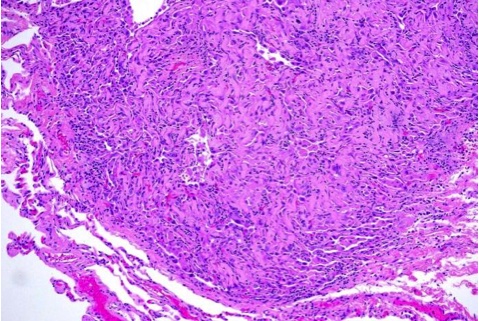
- Multiple, sharply demarcated or circumscribed nodules
- Tubulopapillary proliferation of type II pneumocytes lining fibrotic and thickened alveolar septa, moderate lymphocytic infiltration, no nuclear atypia (Int J Surg Pathol 2010;18:522)
- Enlarged type II pneumocytes with abundant eosinophilic cytoplasm, vesicular nuclei, distinct nucleoli, occasional eosinophilic inclusions
- Increased alveolar macrophages
Microscopic (histologic) images
Electron microscopy description
- Osmiophilic lamellar inclusions and surface microvilli of type II pneumocytes
Molecular / cytogenetics description
- Associated with loss of heterozygosity on TSC1 or TSC2 (Mod Pathol 2010;23:1251)
Differential diagnosis
- Atypical adenomatous hyperplasia
- Lymphangioleiomyomatosis
- Metastases
- Resolving miliary inflammatory / infectious processes
Additional references