Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alzeer A, Wu RI. Lymphangioleiomyomatosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumorlymphangioleiomyomatosis.html. Accessed April 1st, 2025.
Definition / general
- Lung mesenchymal neoplasm that arises from abnormal smooth muscle cells around lymphatic vessels and causes parenchymal damage
Essential features
- Rare cystic lung disease that causes progressive lung damage; mainly affects young females with tuberous sclerosis complex (TSC)
Terminology
- LAM
ICD coding
Epidemiology
- Overall rare (5 cases per 1 million) (QJM 2011;104:971)
- Almost exclusively seen in women of reproductive age (Semin Respir Crit Care Med 2020;41:256)
- Extremely rare in males; reported in males with tuberous sclerosis complex (Clin Radiol 2011;66:625)
- Associated with tuberous sclerosis complex; incidence increases with age in women with tuberous sclerosis complex (Chest 2013;144:578)
Sites
- Mainly lungs; usually in a bilateral fashion
- Can be found in retroperitoneal lymph nodes (Am J Respir Crit Care Med 2006;173:105)
Pathophysiology
- Proliferation of smooth muscle-like cells due to activation of the mTOR signaling pathway as a result of biallelic inactivation, loss of heterozygosity or somatic mutations in TSC1 or TSC2 genes (Lymphat Res Biol 2010;8:33, Am J Hum Genet 1998;62:810, Proc Natl Acad Sci U S A 2000;97:6085)
- Estrogen (ER) and progesterone (PR) receptors may have a role in disease development (Endocr Relat Cancer 2016;23:265)
Etiology
- Sporadic (Semin Respir Crit Care Med 2020;41:256)
- Associated with tuberous sclerosis complex (Semin Respir Crit Care Med 2020;41:256)
Clinical features
- Progressive exertional dyspnea is the most common symptom (Semin Respir Crit Care Med 2020;41:256)
- Pneumothorax (Semin Respir Crit Care Med 2020;41:256)
- Chylous pleural effusion (Am J Respir Crit Care Med 2016;194:748)
- Hemoptysis
- Extrapulmonary involvement of retroperitoneal lymph nodes or abdominal angiomyolipoma (AML) (Am J Respir Crit Care Med 2006;173:105)
Diagnosis
- Usually a clinical diagnosis
- Multiple bilateral round lung cysts on high resolution computed tomography (CT) scan
- Screening CT scans are recommended for females with tuberous sclerosis complex (Am J Respir Crit Care Med 2006;173:105)
Laboratory
- Vascular endothelial growth factor (VEGF) D level of ≥ 800 pg/mL helps distinguish lymphangioleiomyomatosis from other cystic lung diseases (Semin Respir Crit Care Med 2020;41:256)
Radiology description
- Multiple bilateral round thin walled cysts on high resolution CT scan (Semin Respir Crit Care Med 2020;41:256, Am J Med Genet C Semin Med Genet 2018;178:326)
- Lung cysts vary in size (2 mm to > 2 cm) (Clin Radiol 2011;66:625)
- Discrete solid and ground glass nodules, typically ranging between 2 and 14 mm in size (Am J Med Genet C Semin Med Genet 2018;178:326)
- Pneumothorax or effusion (Semin Respir Crit Care Med 2020;41:256)
- Additional findings in other organs: abdominal mass (angiomyolipoma) (Am J Respir Crit Care Med 2006;173:105)
Prognostic factors
- VEGFD levels correlate with disease progression, severity and response to therapy (Semin Respir Crit Care Med 2020;41:256)
- Monitoring through periodic pulmonary function test (PFT) can be used as a tool to assess disease progression, severity and response to therapy (Semin Respir Crit Care Med 2020;41:256, Chest 2019;155:288)
- Respiratory decline slows with menopause and is accelerated by pregnancy or exogenous estrogen (Lymphat Res Biol 2010;8:9)
Case reports
- 22 year old man with sporadic lymphangioleiomyomatosis with multiple atypical features (Indian J Pathol Microbiol 2018;61:94)
- 29 year old woman with acute respiratory failure with gross hemoptysis and lymphangioleiomyomatosis as part of tuberous sclerosis complex (Intern Med 2004;43:755)
- 37 and 45 year old women with pelvic lymphangioleiomyomatosis treated successfully with everolimus (Medicine (Baltimore) 2017;96:e4562)
- 48 year old man with sporadic lymphangioleiomyomatosis as a result of extreme mosaicism for a TSC2 mutation (Ann Am Thorac Soc 2017;14:1227)
Treatment
- Relies on degree of lung function and extent of lung damage
- Supportive therapy with bronchodilators or oxygen therapy (Thorax 2019;74:999)
- Observation for patients with mild function impairment
- mTOR inhibitors (sirolimus, everolimus): for symptomatic patients with severe lung damage and disease progression (N Engl J Med 2011;364:1595)
- Lung transplantation for cases refractory to medical treatment
Gross description
- Multiple thin walled cysts (Semin Respir Crit Care Med 2020;41:256)
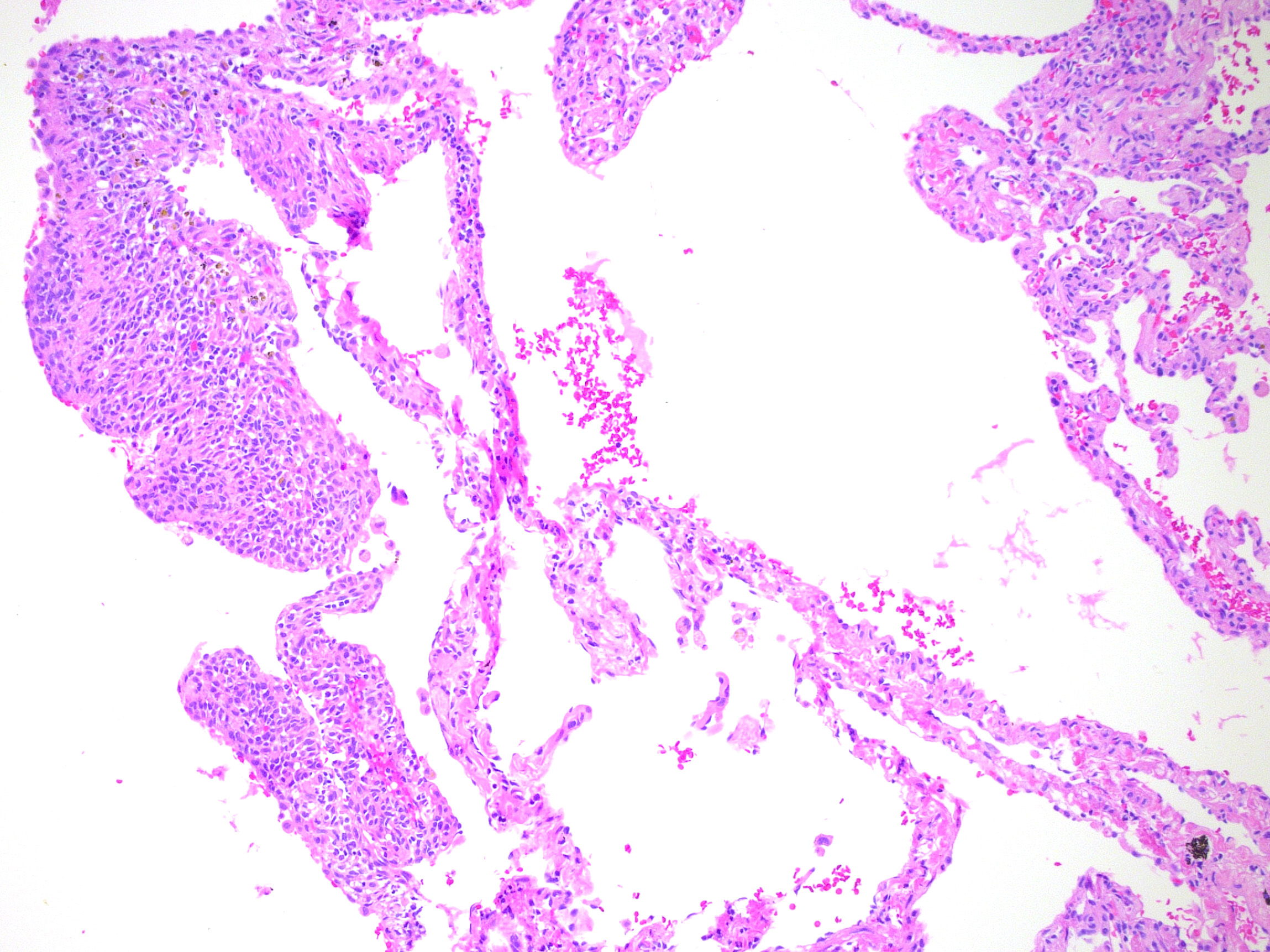
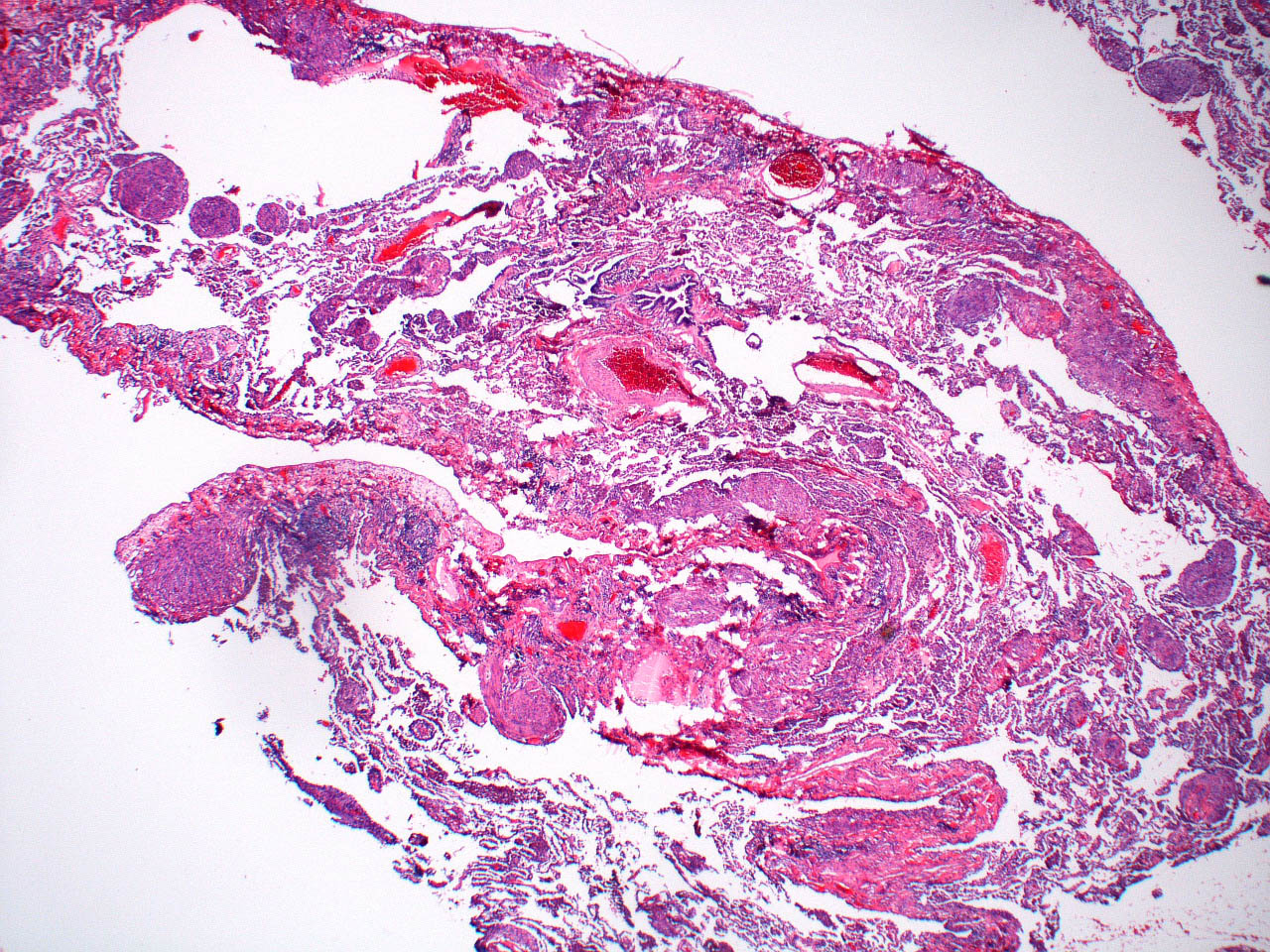
Microscopic (histologic) description
- Multiple thin walled cysts
- Cysts are lined or surrounded by nodules of rounded or spindled smooth muscle-like cells with mixed eosinophilic or clear cytoplasm, without cytologic atypia or mitoses
- Hemosiderin laden macrophages may be present as a clue to organized hemorrhage resulting from cysts infiltrating nearby vessels
- Multinodular pneumocyte hyperplasia around cysts (found in TSC LAM more than sporadic lymphangioleiomyomatosis)
- References: Semin Respir Crit Care Med 2020;41:256, Endocrinology 2016;157:3374
Microscopic (histologic) images
Cytology description
- Well organized, globular cluster consisting of lymphangioleiomyomatosis cells enveloped by lymphatic endothelial cells (Acta Cytol 2009;53:402)
Immunofluorescence description
- Lymphangioleiomyomatosis cells show strong reaction to matrix metalloproteinase 2 (MMP2) in research studies (Arch Pathol Lab Med 2000;124:1642)
Positive stains
Negative stains
Electron microscopy description
- Lymphangioleiomyomatosis nodules are lined by type II pneumocytes with short microvilli and electron dense cytoplasmic lamellar bodies (Arch Pathol Lab Med 2000;124:1642)
Molecular / cytogenetics description
- See Pathophysiology
Videos
Virtual slide review of a case of lymphangioleiomyomatosis
Overview of radiographic features of lymphangioleiomyomatosis
Sample pathology report
- Lung, right upper lobe, wedge biopsy:
- Lymphangioleiomyomatosis (see comment)
- Comment: Sections show cystic spaces replacing normal parenchyma. Some of the cystic spaces have mural nodules consisting of epithelioid and spindled cell proliferation. Lesional cells are immunoreactive with ER, SMA and MelanA. Control stains are satisfactory. The clinical presentation, morphology and immunohistochemical stains support the diagnosis above.
Differential diagnosis
- Langerhans cell histiocytosis:
- Birt-Hogg-Dubé syndrome:
- Localized cystic lesions; lesional cells may show atypia
- Lack of immunoreactivity to melanocytic markers
- Lymphocytic interstitial pneumonia:
- Multiple cyst lesions in middle aged women
- Cysts are surrounded by lymphoplasmacytic inflammatory infiltrate
- Emphysema:
- History of smoking
- More localized process on imaging
Board review style question #1
A 44 year old woman who is a nonsmoker presented to the emergency department with acute chest pain after several months of progressive dyspnea. Physical examination was notable for diminished breath sounds on the right side. Computed tomography of the chest revealed a large pneumothorax and diffuse, intraparenchymal pulmonary cysts. The patient underwent mechanical pleurodesis and a wedge biopsy was performed. The biopsy specimens contained numerous thin walled cysts lined with spindle cells; on immunohistochemistry, the spindle cells coexpressed smooth muscle and melanocytic markers. What is the most likely diagnosis?
- Emphysema
- Lymphangioleiomyomatosis
- Metastasizing pulmonary leiomyoma
- Sarcoidosis
Board review style answer #1
B. Lymphangioleiomyomatosis. Answer A is incorrect because emphysema can present with pneumothorax and lung cysts on imaging but the process is usually more localized and most patients have a history of smoking. Additionally, cysts seen in emphysematous lung specimens represent lung parenchyma with cystic changes rather than lesional / neoplastic cells with the above mentioned immunophenotype. Answer D is incorrect because while sarcoidosis can present with shortness of breath and cystic changes in the lung, these changes are usually localized. Sarcoidosis patients usually have hilar adenopathy and fibrosis (not a finding in this patient). Answer C is incorrect because metastasizing leiomyoma is a diffuse process that can also be symptomatic and appear cystic; however, on immunohistochemistry, leiomyoma cells are not immunoreactive to melanocytic markers.
Comment Here
Reference: Lymphangioleiomyomatosis
Comment Here
Reference: Lymphangioleiomyomatosis
Board review style question #2
A 44 year old woman who is a nonsmoker presented to the emergency department with acute chest pain after several months of progressive dyspnea. Physical examination was notable for diminished breath sounds on the right side. Computed tomography of the chest revealed a large pneumothorax and diffuse, intraparenchymal pulmonary cysts. The patient underwent mechanical pleurodesis and a wedge biopsy was performed. The biopsy specimens contained numerous thin walled cysts lined with spindle cells; on immunohistochemistry, the spindle cells coexpressed smooth muscle and melanocytic markers. What other findings may be seen on this patient's physical examination?
- Characteristic skin changes
- Fever
- Lower extremity swelling
- Tobacco stains
Board review style answer #2
A. Characteristic skin changes. Most likely this patient also has TSC gene mutations as these contribute to the development of lymphangioleiomyomatosis (LAM). Skin changes / lesions such as angiofibromas or hypomelanotic macules are hallmarks / diagnostic features of tuberous sclerosis complex. Answer B is incorrect because fever has not been described for this disorder. Answer C is incorrect because lower extremity swelling and smoking history may raise suspicion for pulmonary embolism. Answer D is incorrect because tobacco stains would raise suspicion for complicated emphysema.
Comment Here
Reference: Lymphangioleiomyomatosis
Comment Here
Reference: Lymphangioleiomyomatosis