Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Wu R. Epithelial myoepithelial carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumorepithelialmyo.html. Accessed April 1st, 2025.
Definition / general
- Low grade malignancy that arises from submucosal bronchial glands, mimics similar salivary gland tumor
- Very rare in lung, only case reports and small series
- Long interval to recurrence or metastasis
Essential features
- Rare, low grade, primary salivary gland-type carcinoma of the lung
- Typically arises in bronchial tree from submucosal glands
- Characterized by biphasic proliferation of duct-like epithelial cells with surrounding myoepithelial cells
Terminology
- Previous designations include adenomyoepithelioma, epithelial myoepithelial tumor, epithelial myoepithelial tumor of unknown malignant potential, pneumocytic adenomyoepithelioma (Hum Pathol 2009;40:366, Mod Pathol 2001;14:521)
ICD coding
- C33 Malignant neoplasm of trachea
- C34.00 Malignant neoplasm of unspecified main bronchus
- C34.01 Malignant neoplasm of right main bronchus
- C34.02 Malignant neoplasm of left main bronchus
- Code more peripheral lesions depending on specific lobe, laterality and extent
Epidemiology
- Extremely rare in lung, case reports mostly in adults, rare case report in child (J Pediatr Hematol Oncol 2009;31:206)
- No clear sex predominance
Sites
- Bronchial tree, usually endobronchial but a few cases peripheral / parenchymal
Pathophysiology
- Low grade malignancy with rare cases of metastasis to chest wall (Lung Cancer 2014;83:416), skull (Case Rep Oncol Med 2011;2011:610383) and lymph nodes (Hum Pathol 2009;40:366)
Etiology
- Arises from submucosal bronchial glands, the lung counterpart of the intercalated duct of the salivary gland (Oncol Lett 2015;10:175)
Clinical features
- Cough, hemoptysis, dyspnea or obstructive symptoms if endobronchial location
- Peripheral lesions may be asymptomatic
Diagnosis
- Challenging to diagnose with small biopsy specimens
- Exclude metastasis from salivary gland
Prognostic factors
- Complete surgical resection generally curative
- High mitotic rate, tumor necrosis and nuclear pleomorphism appear to be adverse prognostic factors (Am J Surg Pathol 2001;25:1508)
Case reports
- 34 year old man with tracheal tumor (J Thorac Dis 2014;1:S194)
- 52 year old woman with progressive cough, dyspnea and wheezing (Case of the Week #357)
- 53 year old woman with tumor showing lobular solid growth and lymph node metastases (Tuberc Respir Dis (Seoul) 2015;78:428)
- 57 year old man with incidental endobronchial tumor (Case Rep Pathol 2012;2012:319434)
- 72 year old woman with tumor showing high grade transformation (Oncol Lett 2015;10:175)
- 73 year old man with bronchial tumor (Arch Pathol Lab Med. 2003 Apr;127:e177)
Treatment
- Complete surgical resection
- May recur after local therapy or incomplete excision (Clin Lung Cancer 2007;8:386)
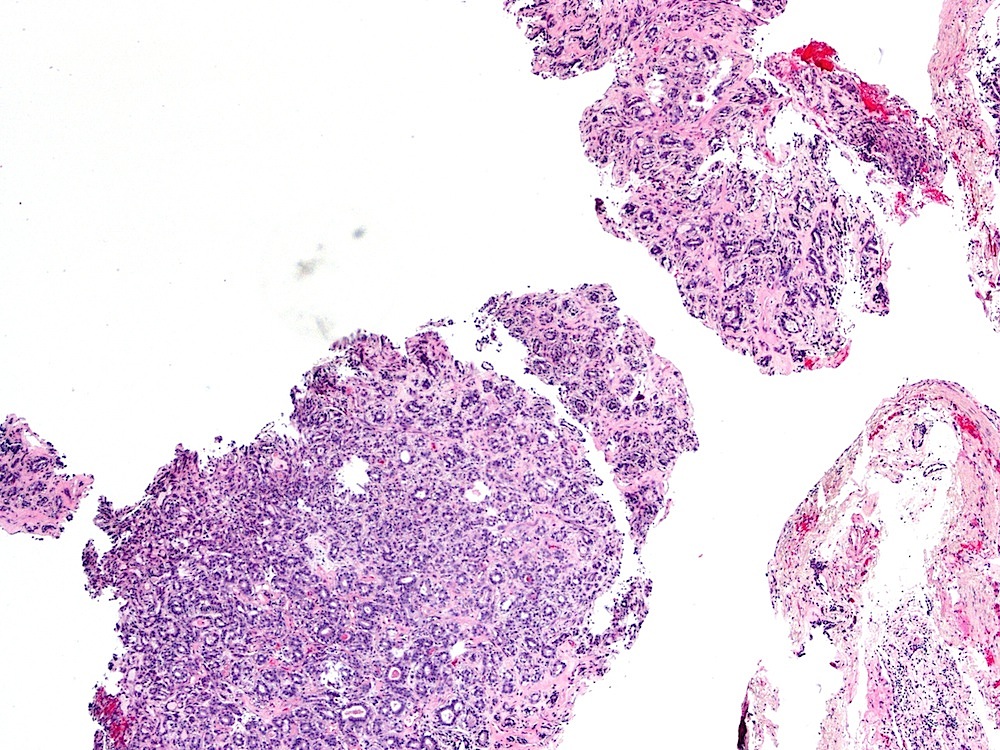
Gross description
- Intraluminal polypoid mass in bronchus; may invade parenchyma
- Well circumscribed, unencapsulated, tan, firm
- Variable size averaging a few centimeters
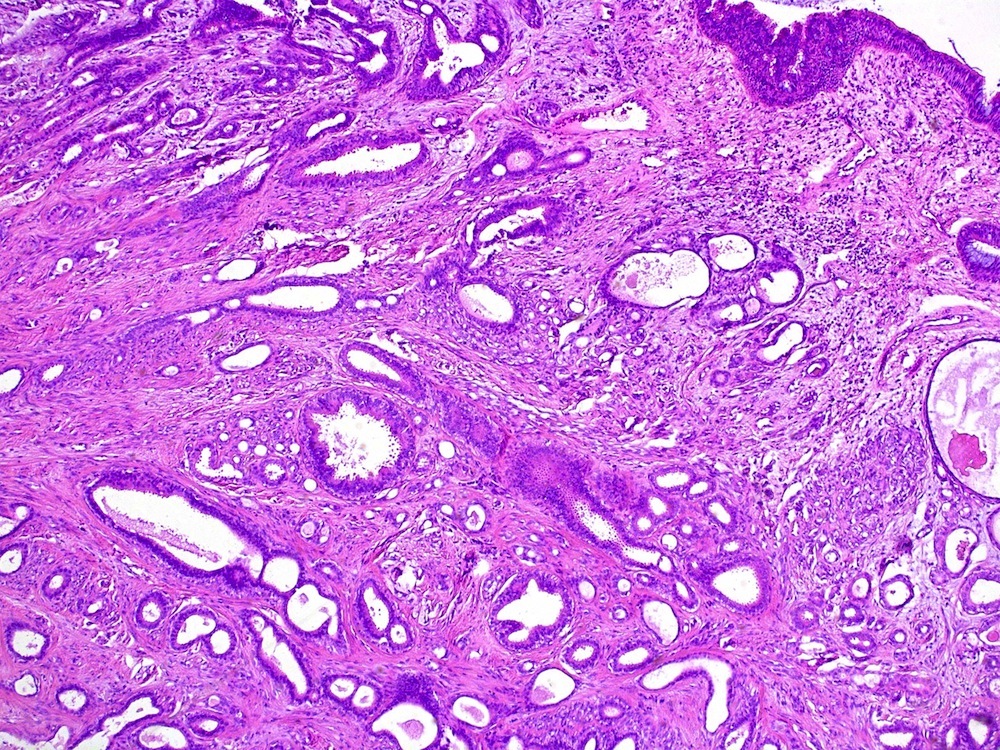
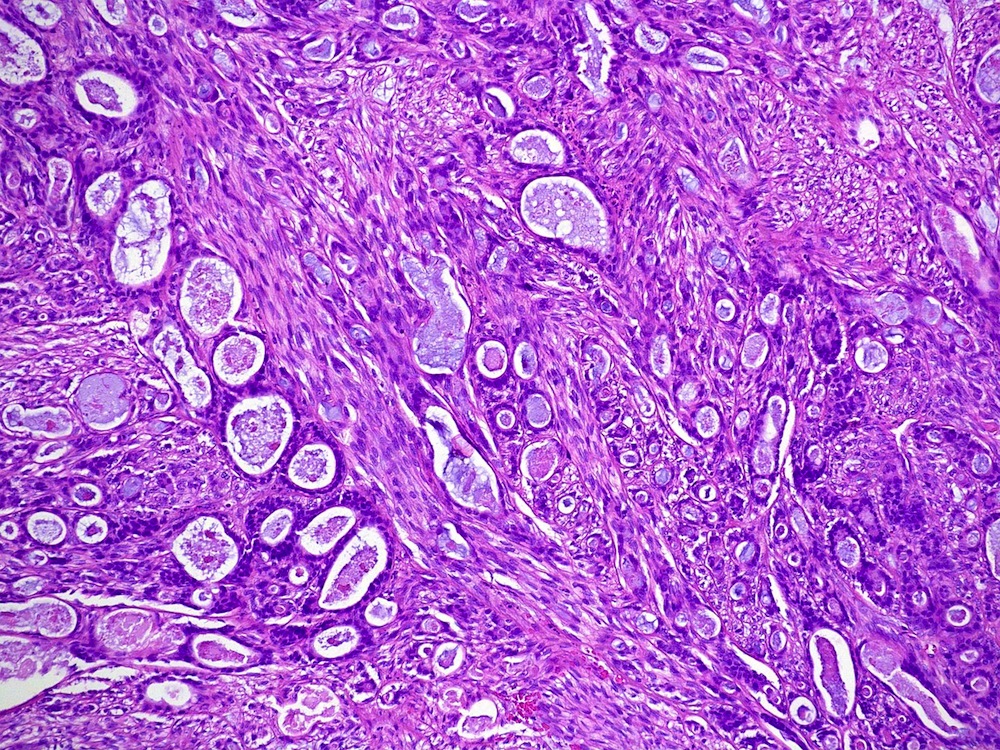
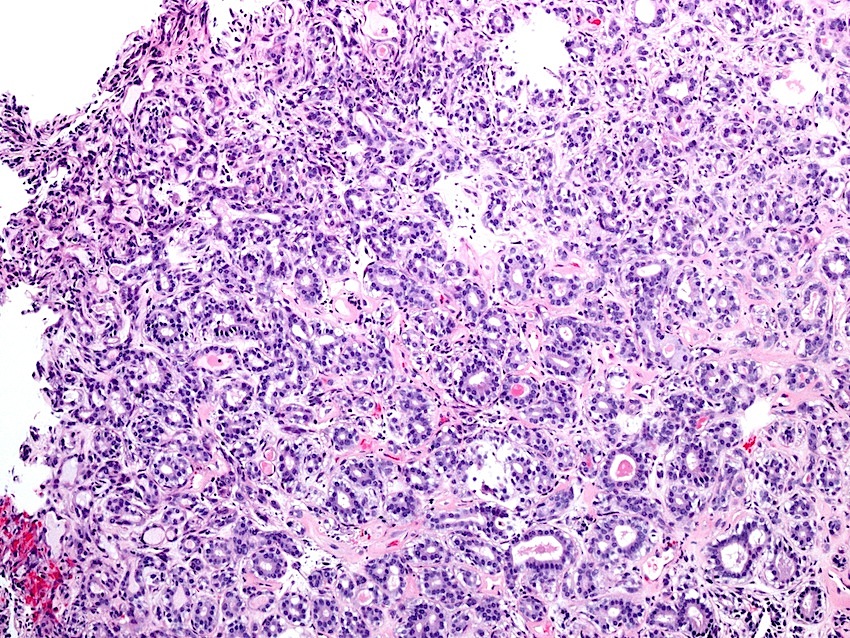
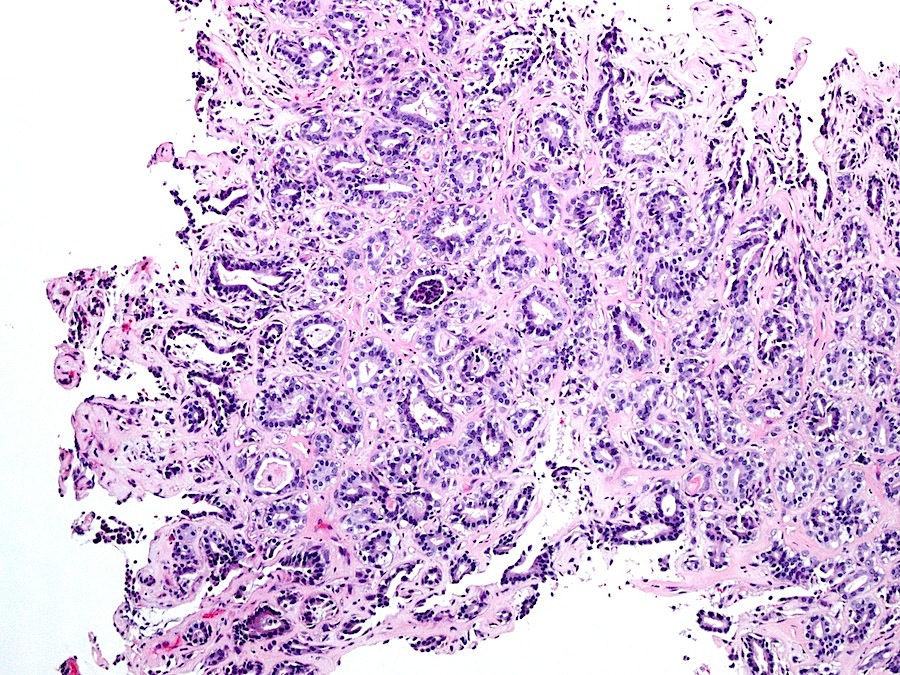
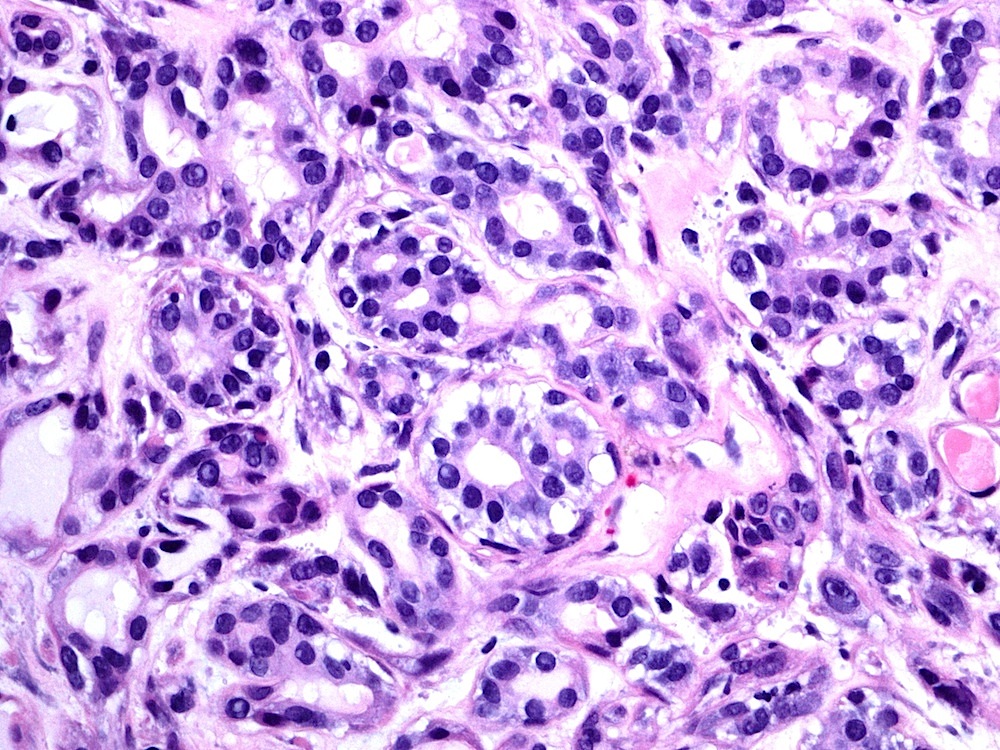
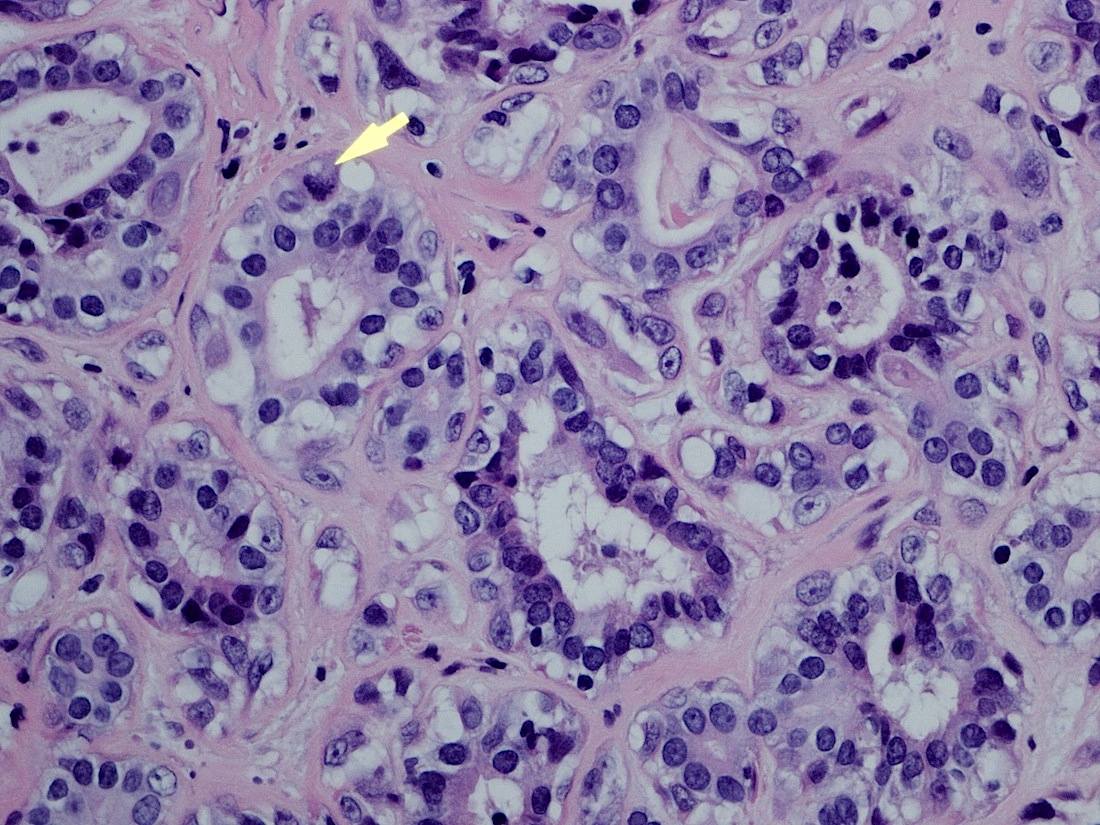
Microscopic (histologic) description
- Well circumscribed mass with pushing margin
- Thin fibrous septa with variable hyalinization or sclerosis
- Biphasic proliferation of inner epithelial and outer myoepithelial cells with formation of bilayered, duct-like structures
- Appearance and proportion of two cell types may be variable
- Epithelial cells flattened, cuboidal or columnar with somewhat clear to eosinophilic cytoplasm
- Myoepithelial cells may be indistinct, flattened, spindled or clear
- Lumens may contain pale to eosinophilic amorphous material or debris
- Scant inflammatory infiltrate may be present
- Mitoses, significant nuclear atypia, necrosis and hemorrhage typically absent
Microscopic (histologic) images
Contributed by Roseann Wu, M.D., M.P.H. and Case #357
Images hosted on other servers:
Positive stains
- Epithelial cells: CK7, pankeratin, EMA
- Myoepithelial cells: S100, muscle specific actin, p63, CK5/6
Molecular / cytogenetics description
- Potential role of p27 kip-1 protein (Diagn Pathol 2011;6:71)
Differential diagnosis
- Acinic cell carcinoma
- Adenoid cystic carcinoma with a tubular pattern
- Adenocarcinoma
- Clear cell ("sugar") tumor
- Metastatic clear cell carcinoma
- Metastatic epithelial myoepithelial carcinoma (usually parenchymal, not endobronchial)
- Mucoepidermoid carcinoma
- Myoepithelial carcinoma
- Myoepithelioma
- Pleomorphic adenoma
- Pneumocytic adenomyoepithelioma: has bronchial minor salivary gland origin; shows myoepithelial and pneumocytic differentiation (Am J Surg Pathol 2007;31:562)
Additional references
- Clinicopathological analysis of primary salivary gland type lung cancer (J Thorac Oncol 2013;8:1578)
Board review style question #1
- Epithelial myoepithelial carcinoma primary to the lung is believed to arise from what cell type(s)?
- Club cells
- Ciliated columnar cells
- Submucosal bronchial glands
- Type 1 pneumocytes
- Type 2 pneumocytes
Board review style answer #1