Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Keow J, Cecchini MJ. Lepidic adenocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumoradenolepidic.html. Accessed March 31st, 2025.
Definition / general
- Lung adenocarcinoma with primarily lepidic growth pattern with at least one of the following (Arch Pathol Lab Med 2013;137:685, J Thorac Oncol 2011;6:244):
- > 0.5 cm of stromal invasion
- Measuring > 3 cm in greatest dimension with ≤ 0.5 cm of stromal invasion
- Lymphatic, vascular or pleural invasion
- Tumor necrosis
- Spread through airspaces
Essential features
- Tumor with noninvasive (lepidic) and invasive components
- Invasive component should total > 0.5 cm
- Invasive component can be defined as stromal invasion or the presence of any subtype other than lepidic
- Presence of lymphovascular invasion, tumor necrosis or pleural invasion also meets the criteria of an invasive component
- Tumors measuring > 3 cm with < 0.5 cm of invasive or nonlepidic components are also classified as lepidic adenocarcinoma
- In rare cases, a lepidic carcinoma with < 0.5 cm of invasion that has high risk features (lymphatic, vascular or pleural invasion, tumor necrosis or spread through airspaces) should also be classified as lepidic adenocarcinoma and not minimally invasive adenocarcinoma
Terminology
- Lepidic adenocarcinoma
- Lepidic predominant adenocarcinoma (for mixed patterns where lepidic growth pattern predominates)
- Older terminology was bronchoalveolar carcinoma; however, this is obsolete and should no longer be utilized
ICD coding
Epidemiology
- More common in Asian populations and not as strongly associated with smoking as other subtypes of adenocarcinoma (Am J Surg Pathol 2014;38:448)
Sites
- Generally peripherally located lung lesions (Lung Cancer 2000;29:179)
Pathophysiology
- Hypothesized to form after a multistep progression from atypical adenomatous hyperplasia to adenocarcinoma in situ to lepidic adenocarcinoma (J Thorac Oncol 2008;3:340)
Etiology
Clinical features
- Generally asymptomatic, discovered as incidental mixed solid and ground glass lesions on CT scans (N Engl J Med 2013;368:1980)
Diagnosis
- Slow growing ground glass opacity (see radiology description)
- Biopsies will show adenocarcinoma with lepidic growth pattern
- Diagnosis can only be made on the resection specimen and cannot be made with limited tissue sampling (Arch Pathol Lab Med 2013;137:668, Arch Pathol Lab Med 2007;131:1027)
Radiology description
- Ground glass opacity dominant, with foci of invasion represented by solid areas (Lung Cancer 2018;125:14, Hum Pathol 2016;51:41, Ann Oncol 2015;26:156)
Prognostic factors
- Early lepidic adenocarcinomas (pT1a) have a more favorable prognosis than other subtypes of adenocarcinoma (J Clin Oncol 2012;30:1438, J Thorac Oncol 2011;6:1496, Mod Pathol 2011;24:653)
Case reports
- 26 year old woman with a lepidic adenocarcinoma demonstrating aerogenous spread of mucin without evidence of invasion (Exp Mol Pathol 2014;96:400)
- 36 year old woman with a 33 week pregnancy in acute respiratory failure from a lepidic pulmonary adenocarcinoma (Case Rep Oncol 2018;11:822)
Treatment
- Associated with a lower risk of recurrence than other subtypes of adenocarcinoma; surgical excision with close follow up may be sufficient for early stage disease (Am J Surg Pathol 2014;38:448)
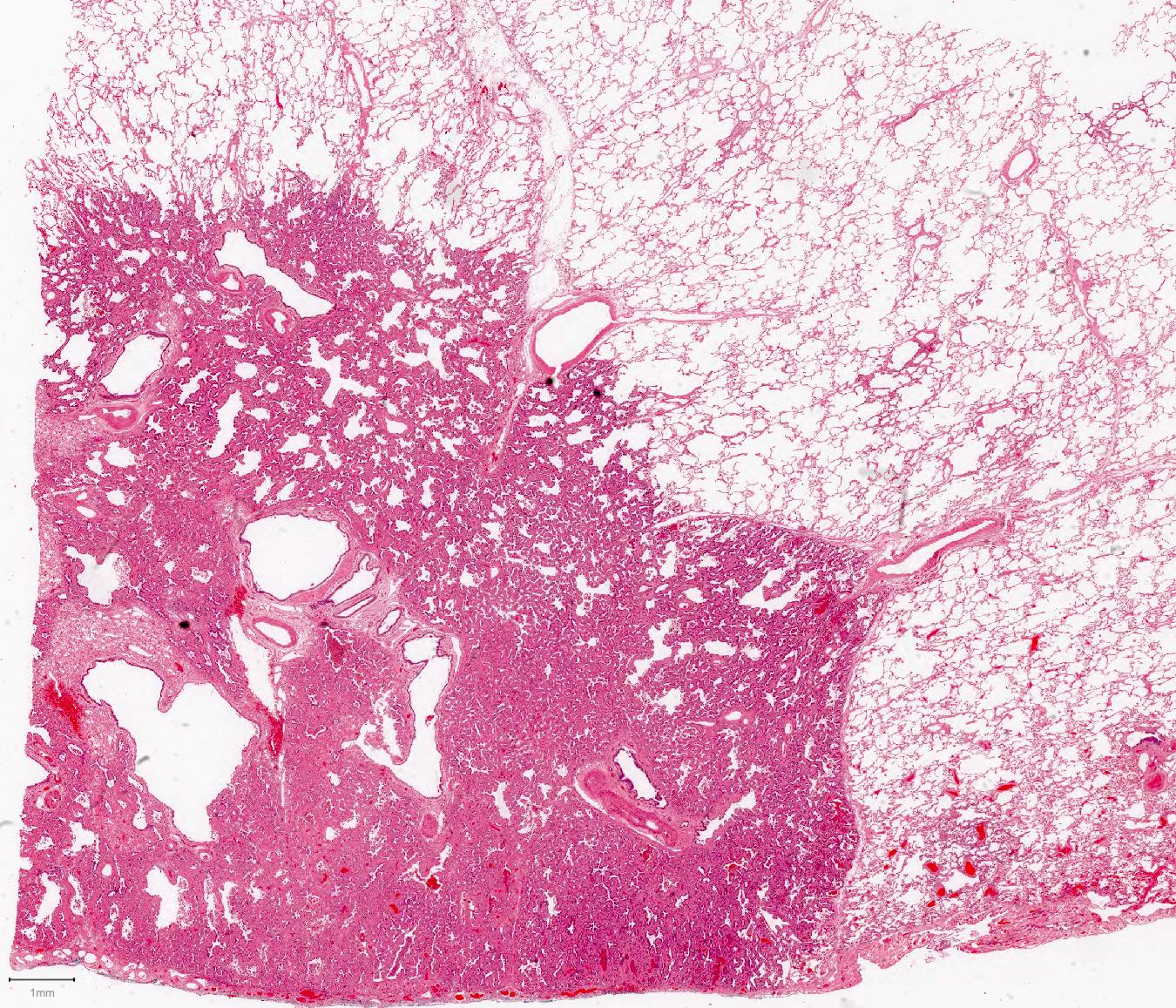
Gross description
- Peripheral ill defined firm white tumor with solid areas; ill defined areas correspond to lepidic growth pattern and the solid areas correspond to invasive component (Hum Pathol 2016;51:41)
- In rare cases, necrosis and frank pleural invasion may be present
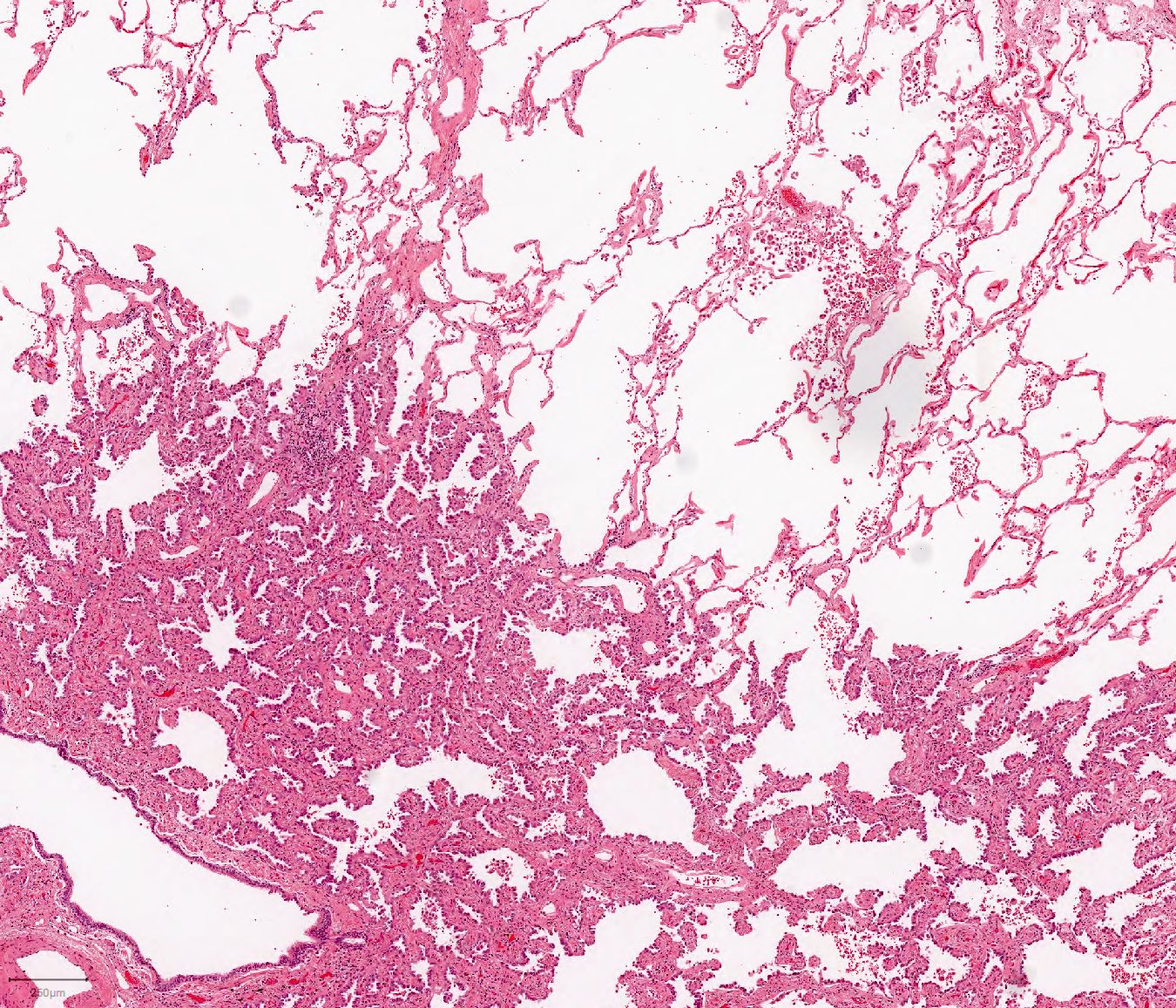
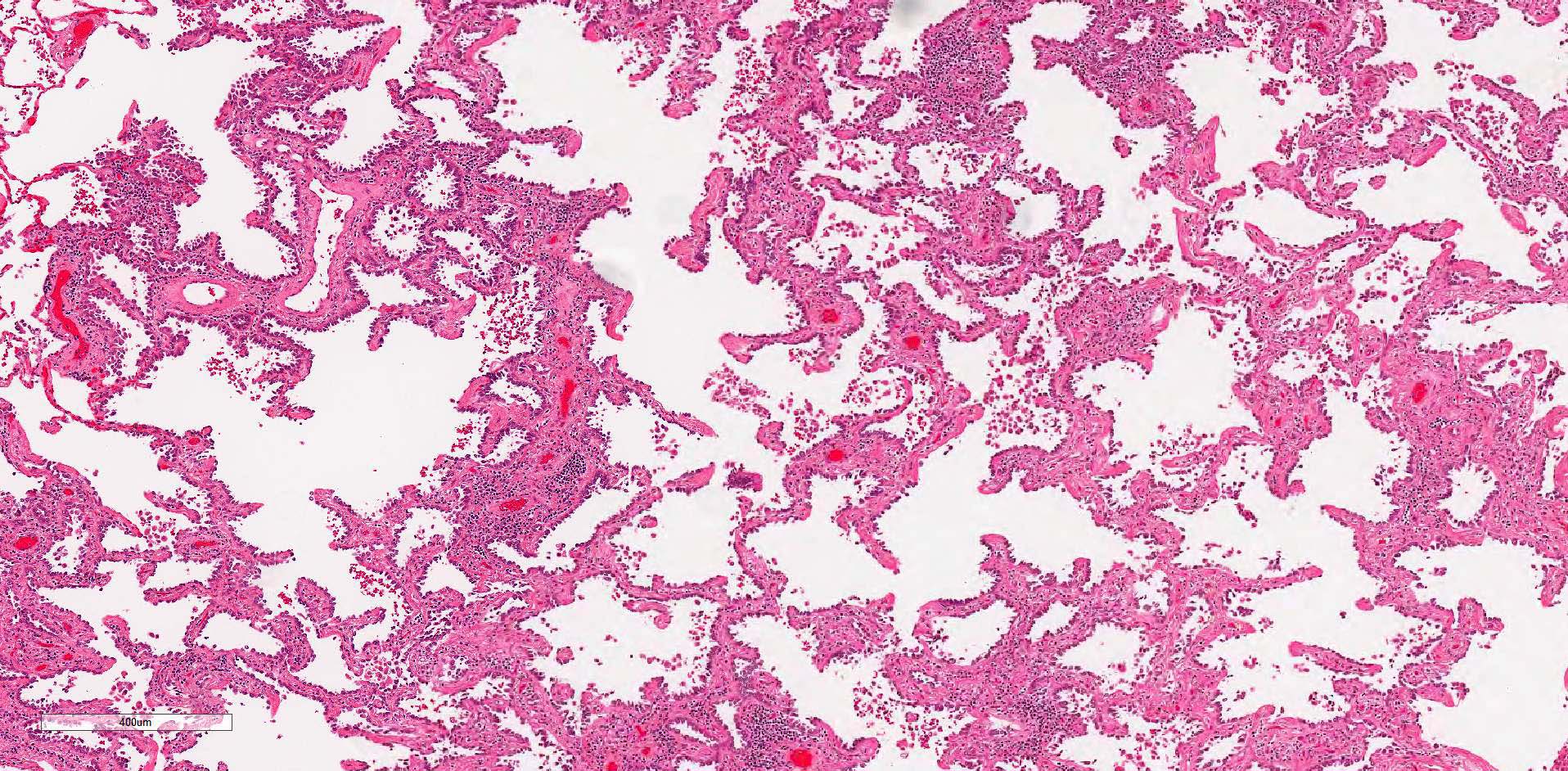
Microscopic (histologic) description
- Primary lung adenocarcinoma with lepidic growth pattern measuring ≤ 3 cm in greatest dimension with > 0.5 cm area of stromal invasion or presence of necrosis, lymphovascular invasion, pleural invasion or spread through air spaces
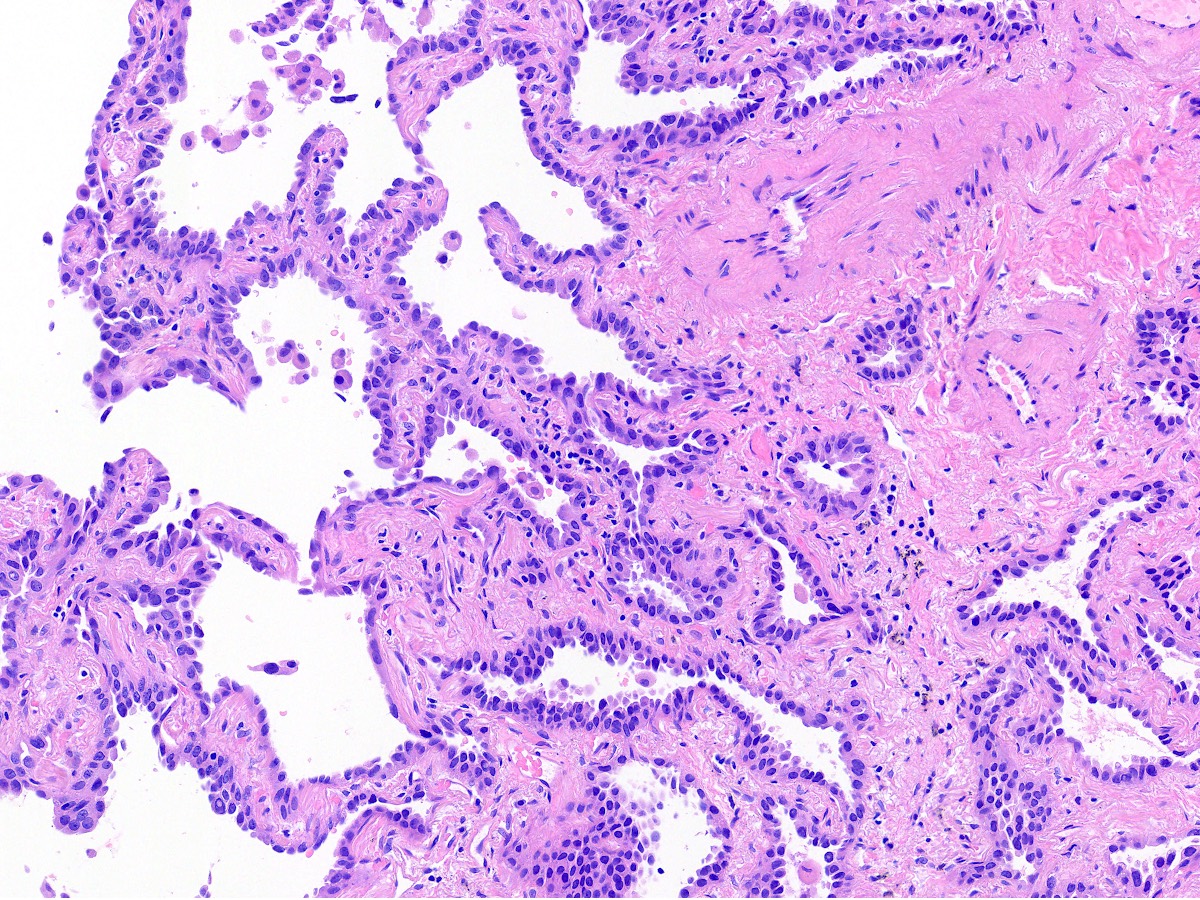
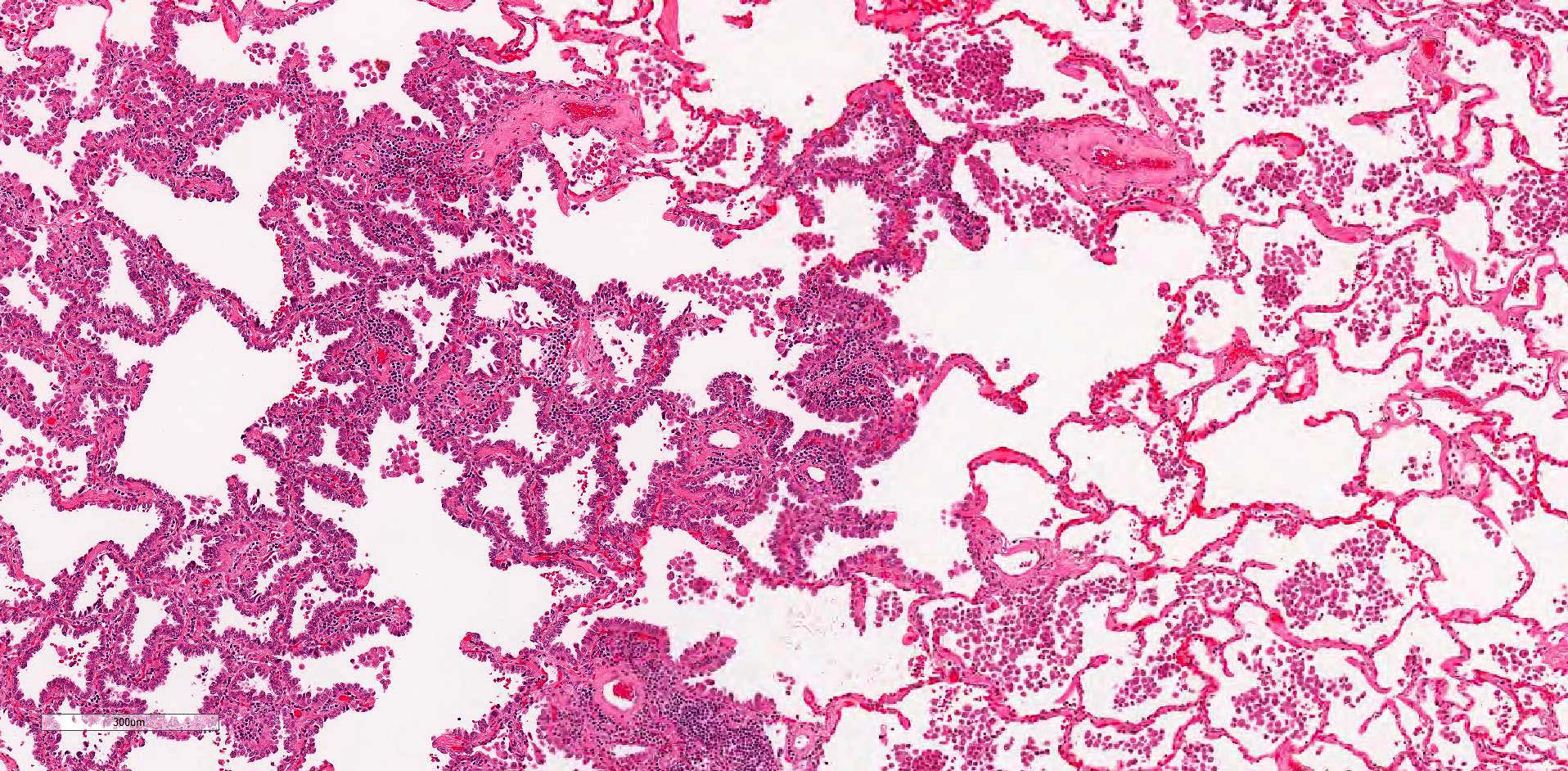
- Lepidic growth pattern: neoplastic cells resembling bland type II pneumocytes growing along the surface of the alveolar air spaces
- Foci of stromal invasion characterized by angulated glands, desmoplastic stroma and increased cytologic atypia (Cancer 1995;75:2844)
- Size of invasion should be measured as the largest focus of invasion (Am J Surg Pathol 2014;38:448, Arch Pathol Lab Med 2013;137:685)
- If there are multiple foci of invasion, the invasive size can be measured as a sum of the percentage of the invasive components in each section multiplied against the greatest tumor dimension (Am J Surg Pathol 2014;38:448, Surg Today 2019;49:828)
- Invasion may also be defined as presence of nonlepidic growth pattern (acinar, micropapillary, papillary, solid, colloid or fetal patterns) or the presence of necrosis, lymphovascular invasion, pleural invasion or spread through air spaces
- For the uncommon occurrence of a lepidic predominant tumor > 3.0 cm with either no invasion or ≤ 0.5 cm of invasion, it is recommended that such tumors be classified as lepidic predominant adenocarcinoma and staged as pT1a, since there is insufficient data to conclude they have the same prognostic features as ≤ 3.0 cm tumors meeting criteria for adenocarcinoma in situ or minimally invasive adenocarcinoma (J Thorac Oncol 2016;11:1204)
- Mucinous carcinoma can often display a prominent lepidic growth pattern; however, the majority of cases will have areas of invasion and should be classified as an invasive mucinous adenocarcinoma
Microscopic (histologic) images
Negative stains
Sample pathology report
- Lung, right lower lobe, lobectomy:
- Invasive adenocarcinoma, lepidic predominant, pT1a NX MX (see synoptic report)
Differential diagnosis
- Minimally invasive adenocarcinoma:
- < 3.0 cm in greatest dimension
- Invasive foci must be < 0.5 cm in aggregate
- No other high risk features
- Adenocarcinoma in situ / atypical adenomatous hyperplasia:
- < 3.0 cm in greatest dimension
- No invasive component
Additional references
Board review style question #1
Board review style answer #1
C. Noninvasive lepidic adenocarcinoma. In this image, the neoplastic cells extend along intact alveolar spaces. There are no architectural changes or features of invasive growth. There is a sharp cut off between these cells and a small amount of normal lung in the top left of the image. While challenging to see at this power, the cells are hyperchromatic with variably spaced overlapping cells that supports the classification as a lepidic adenocarcinoma.
Comment Here
Reference: Lepidic adenocarcinoma
Comment Here
Reference: Lepidic adenocarcinoma
Board review style question #2
What is the best diagnosis for a 4.0 cm tumor composed primarily of noninvasive lepidic adenocarcinoma and a 0.4 cm invasive acinar component?
- Acinar predominant adenocarcinoma
- Adenocarcinoma in situ
- Lepidic predominant adenocarcinoma
- Minimally invasive adenocarcinoma
Board review style answer #2
C. Lepidic predominant adenocarcinoma. This tumor is best classified as a lepidic predominant adenocarcinoma because the size is 4 cm which is above the 3 cm cut off for a lepidic adenocarcinoma. Note, the invasive component of 0.4 cm is insufficient to meet criteria for a lepidic adenocarcinoma. The T stage should be assigned based on the size of the invasive component.
Comment Here
Reference: Lepidic adenocarcinoma
Comment Here
Reference: Lepidic adenocarcinoma