Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Basu A, Zhou F. Adenocarcinoma in situ. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungtumoradenoinsitu.html. Accessed April 2nd, 2025.
Definition / general
- Preinvasive lung adenocarcinoma
- Size: ≤ 30.0 mm
- Pure lepidic growth pattern with no invasion (neoplastic cells along pre-existing alveolar structures)
- Diagnosed only when all tumor has been sampled
- Diagnosis cannot be made in small biopsy or cytology specimen
Essential features
- Lepidic growth with no stromal, vascular or pleural invasion
- Size: ≤ 30.0 mm
- Diagnosed only after complete sampling of a resected lesion
Terminology
- Bronchioloalveolar carcinoma (historical term, obsolete)
ICD coding
Epidemiology
- ~5% of nonsmall cell lung carcinomas (NSCLC)
- F = M (F slightly higher, in contrast to other NSCLC)
- References: J Clin Oncol 2005;23:8396, Lung Cancer 2004;45:137
Sites
- Peripheral lung (Cancer 1995;75:2844)
Pathophysiology
- Multistep progression model (Ann Oncol 2015;26:156, Int J Mol Sci 2018;19:1259)
- Adenocarcinoma in situ (AIS) is the step between atypical adenomatous hyperplasia (AAH) and minimally invasive carcinoma (MIA)
- Incidence of EGFR mutations increases from atypical adenomatous hyperplasia → adenocarcinoma in situ → minimally invasive carcinoma
- KRAS and BRAF mutations do not show same progression, suggesting other molecular alterations are also involved in tumor evolution
- EPPK1, KMT2C, KMT2D, NOTCH3 and NF1 mutations may present as early events in the progression of lung adenocarcinoma (Am J Respir Crit Care Med 2020;201:697)
Etiology
- Same as invasive lung adenocarcinoma
- #1 risk factor is tobacco smoking
- Possible risk factors in never smokers: secondhand smoke, radon, occupational exposures, air pollution
- Most cases of lung cancer in never smokers are idiopathic, with different mutational profile than smoking related lung cancer
- Reference: J Thorac Oncol 2012;7:1352
Clinical features
- Often incidental
- May occur alone or along with invasive adenocarcinoma as a separate focus
- Slow growing
Diagnosis
- May or may not be seen on CT or MRI, depending on size and association with scar
- Radiologic features that suggest indolence (Ann Am Thorac Soc 2015;12:1193):
- Small size
- Longer volumetric doubling time (> 400 days)
- Maximum standardized uptake value (SUV) < 1
- Definitive diagnosis requires excision and histopathologic evaluation
Radiology description
- Usually nonsolid
- May be partly solid or even solid (if tumor is mucinous or contains scar)
- References: Eur Respir J 2018;51:1800190, J Thorac Oncol 2016;11:1204
Prognostic factors
- Complete resection = 100% disease free and recurrence free survival rates (Am J Surg Pathol 2014;38:448, Lung Cancer 2019;129:16)
- If not resected, factors associated with growth of the lesions are initial tumor size, smoking and mutational status
- Reference: J Thorac Oncol 2012;7:1352
Case reports
- 39 year old nonsmoking woman with adenocarcinoma in situ coexisting with low grade fetal lung adenocarcinoma (Onco Targets Ther 2020;13:6675)
- 44 year old woman with papillary thyroid carcinoma metastasizing to adenocarcinoma in situ of lung (Korean J Pathol 2012;46:282)
- 72 year old man with adenocarcinoma in situ, detected on a thin walled lung cavity (Surg Case Rep 2022;8:60)
Treatment
- Complete resection is diagnostic and curative
- No adjuvant therapy
- Reference: Am J Surg Pathol 2014;38:448, Lung Cancer 2019;129:16
Gross description
- Ill defined nodule
- May appear grossly solid if collapsed, compressed or associated with scar
- Size: ≤ 30.0 mm
- References: J Thorac Oncol 2016;11:1204, Int J Mol Sci 2018;19:1259
Frozen section description
- Lepidic pattern adenocarcinoma with mild to moderate cytologic atypia
- Do not diagnose as adenocarcinoma in situ on frozen section; invasion may be present on deeper levels or in the remainder of the tumor that was not submitted for frozen section
- If no invasion is seen on frozen, one may call it adenocarcinoma with the lepidic pattern on 1 representative section, pending evaluation of permanent sections (or the remainder of the tumor)
- Reference: J Clin Pathol 2016;69:1076
Frozen section images
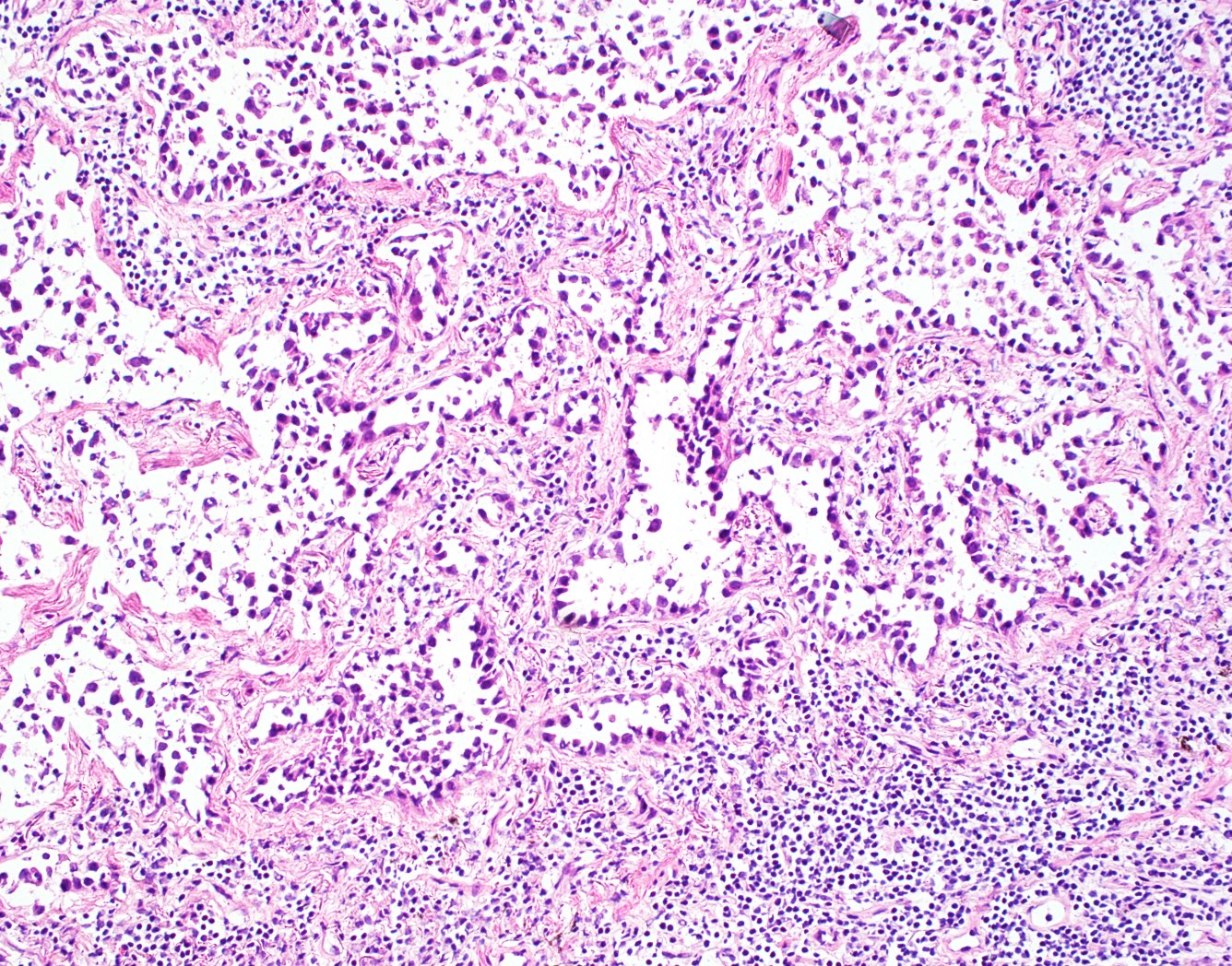
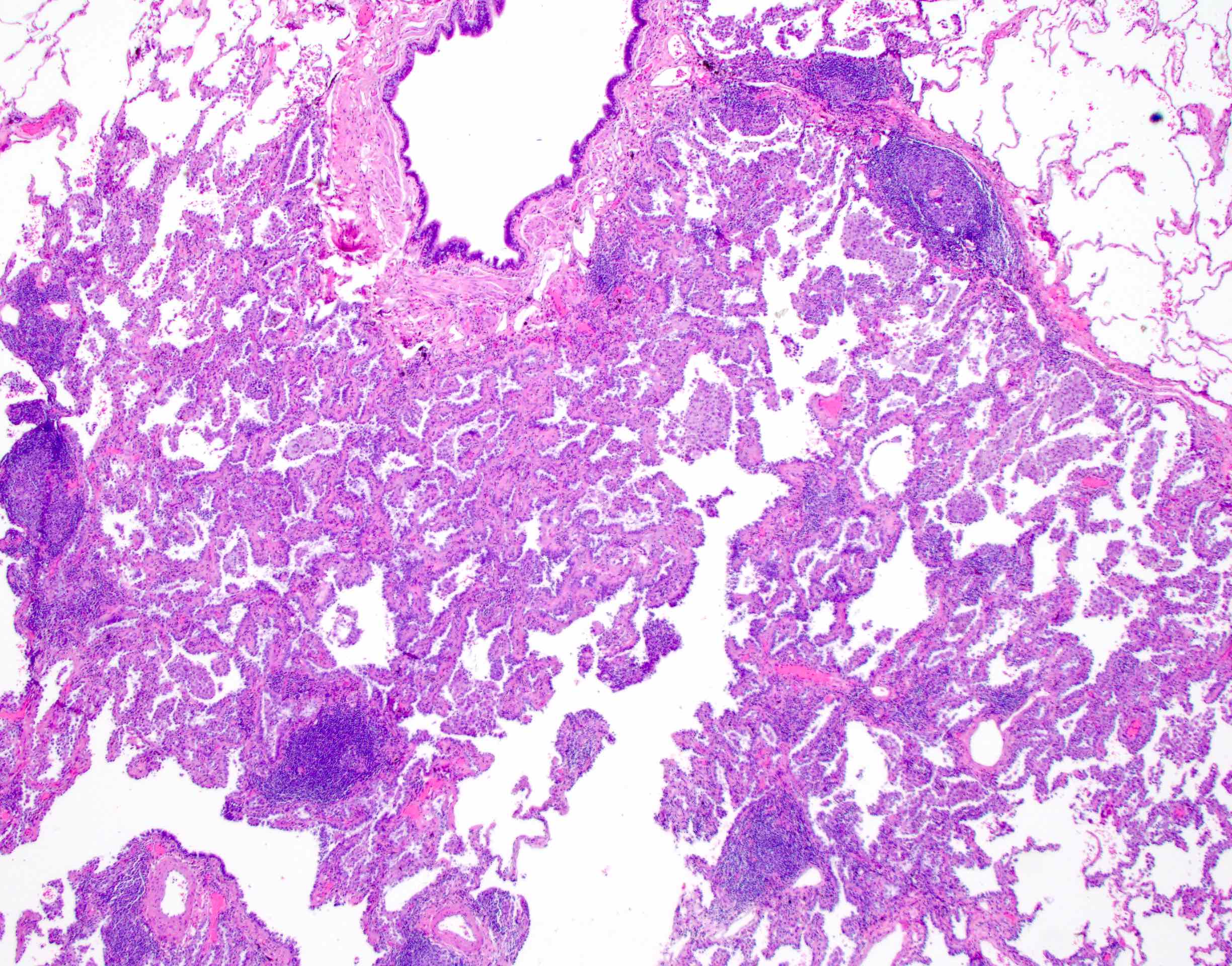
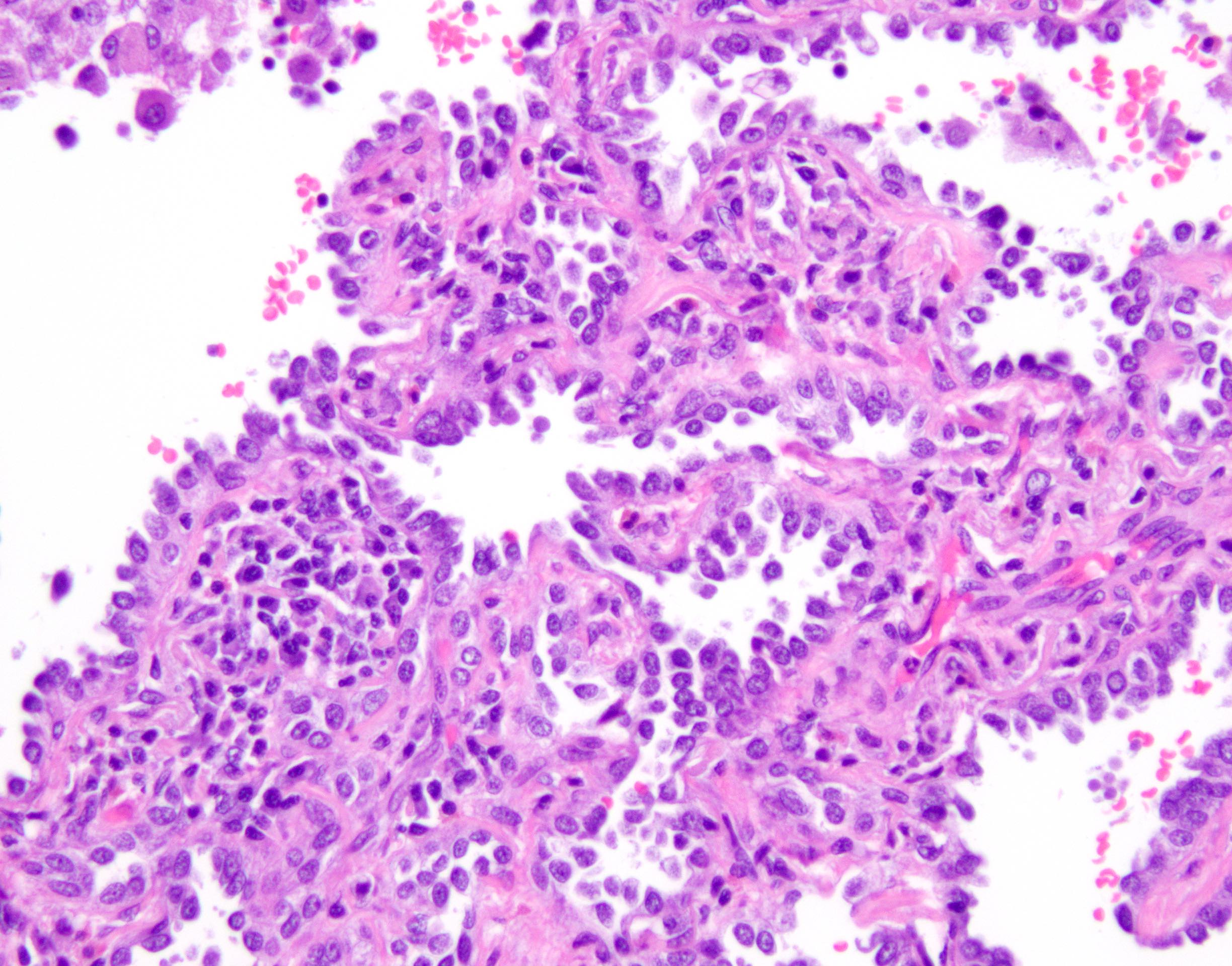
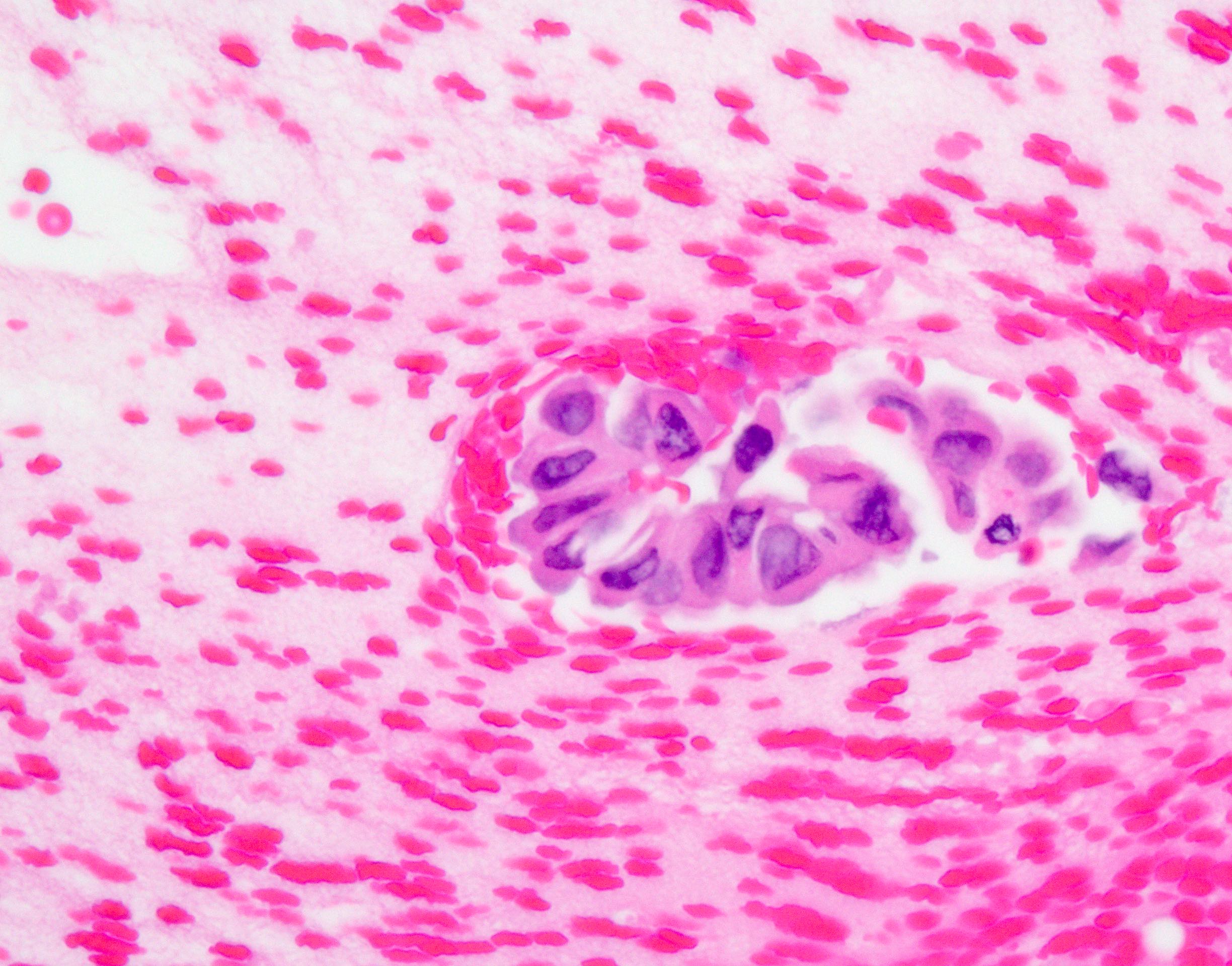
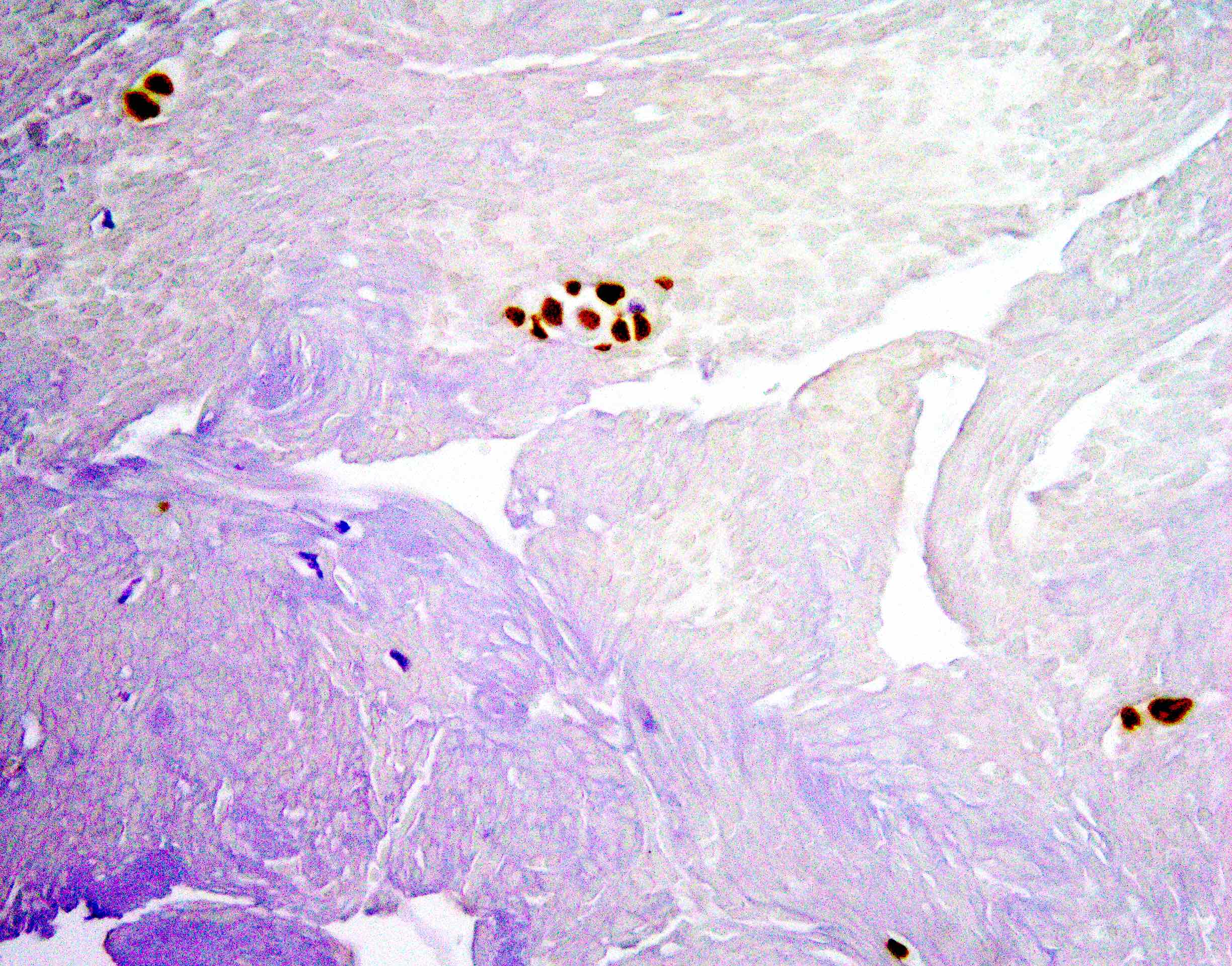
Microscopic (histologic) description
- Lepidic growth pattern only: back to back neoplastic cells growing along pre-existing alveolar structures only
- No stromal, vascular or pleural invasion; no necrosis
- Diagnosed only in resections after complete sampling
- Cannot be diagnosed in small biopsies, cytology or frozen sections (differential diagnosis minimally invasive carcinoma and invasive adenocarcinoma)
- Size: ≤ 30.0 mm
- Nonmucinous adenocarcinoma in situ = mild to moderate cytologic atypia, consisting of various combinations of the following features: nuclear membrane irregularity, intranuclear pseudoinclusions, nuclear grooves, hyperchromasia, anisocytosis, small nucleoli, increased nuclear to cytoplasmic ratio, hobnailing
- Not all features may be present
- Mucinous type adenocarcinoma in situ = extremely rare; mucinous tumors are usually associated with invasion
- Mucinous cells show minimal atypia with abundant intracellular mucin and basally oriented nuclei
- References: J Thorac Oncol 2016;11:1204, Int J Mol Sci 2018;19:1259
Microscopic (histologic) images
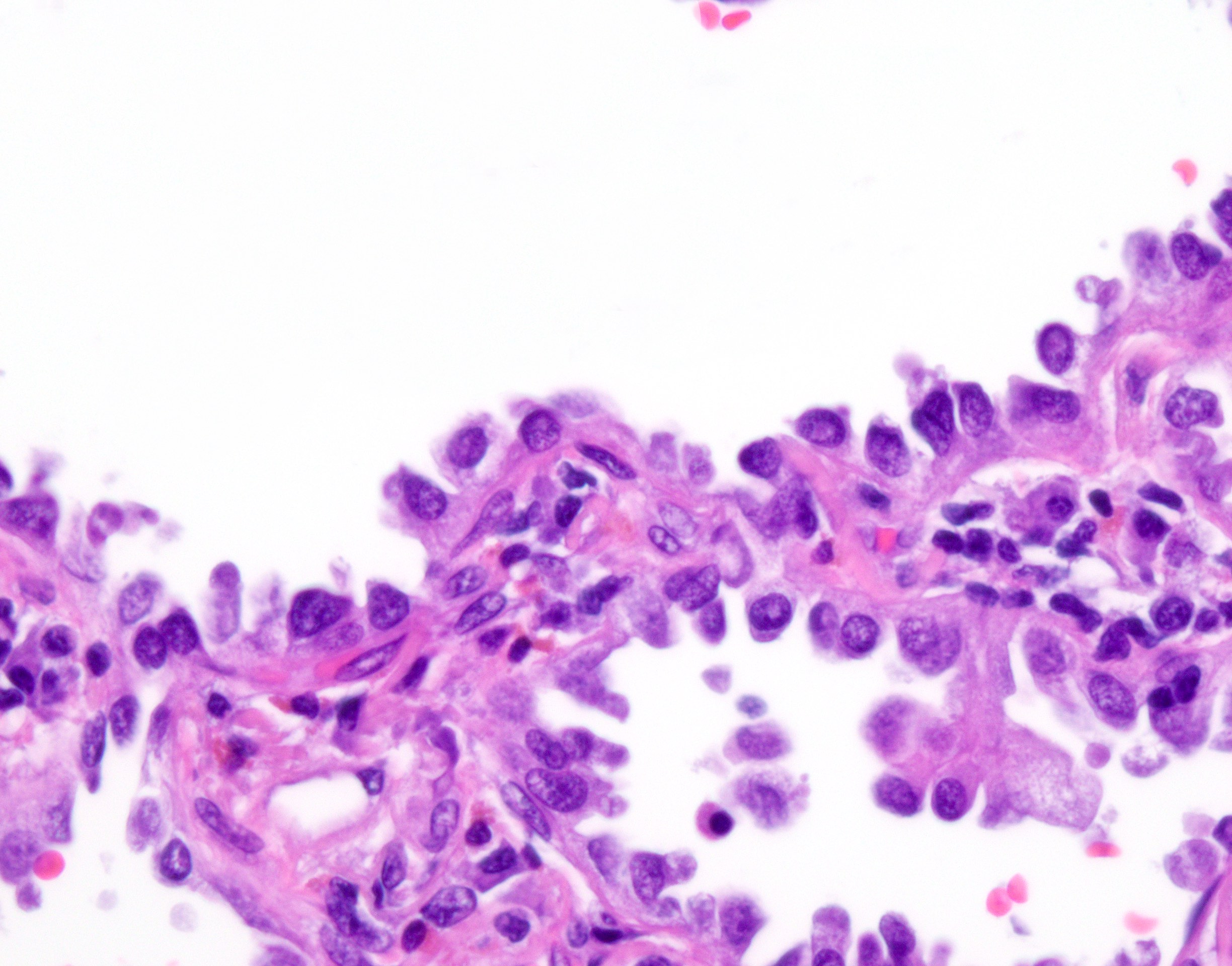
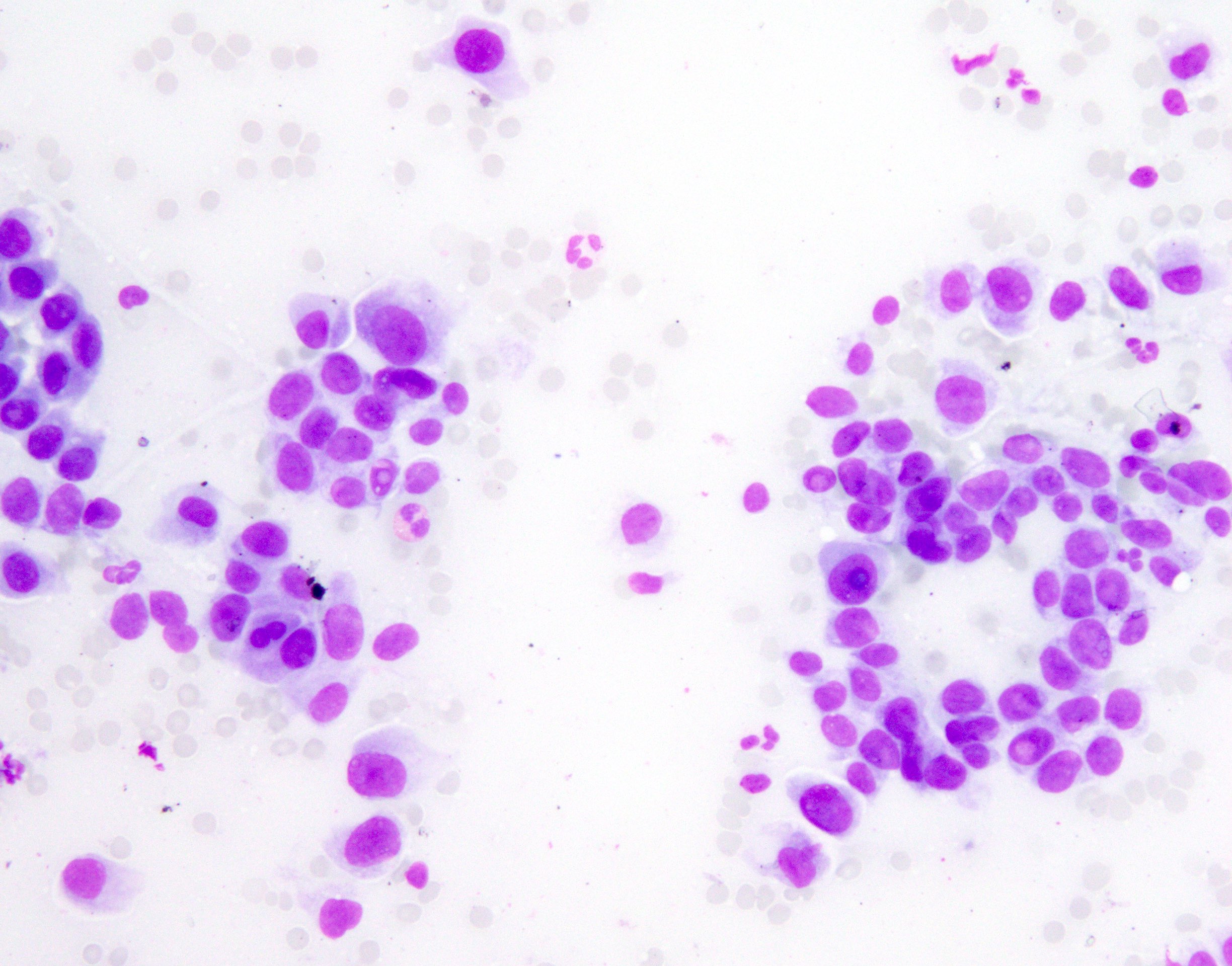
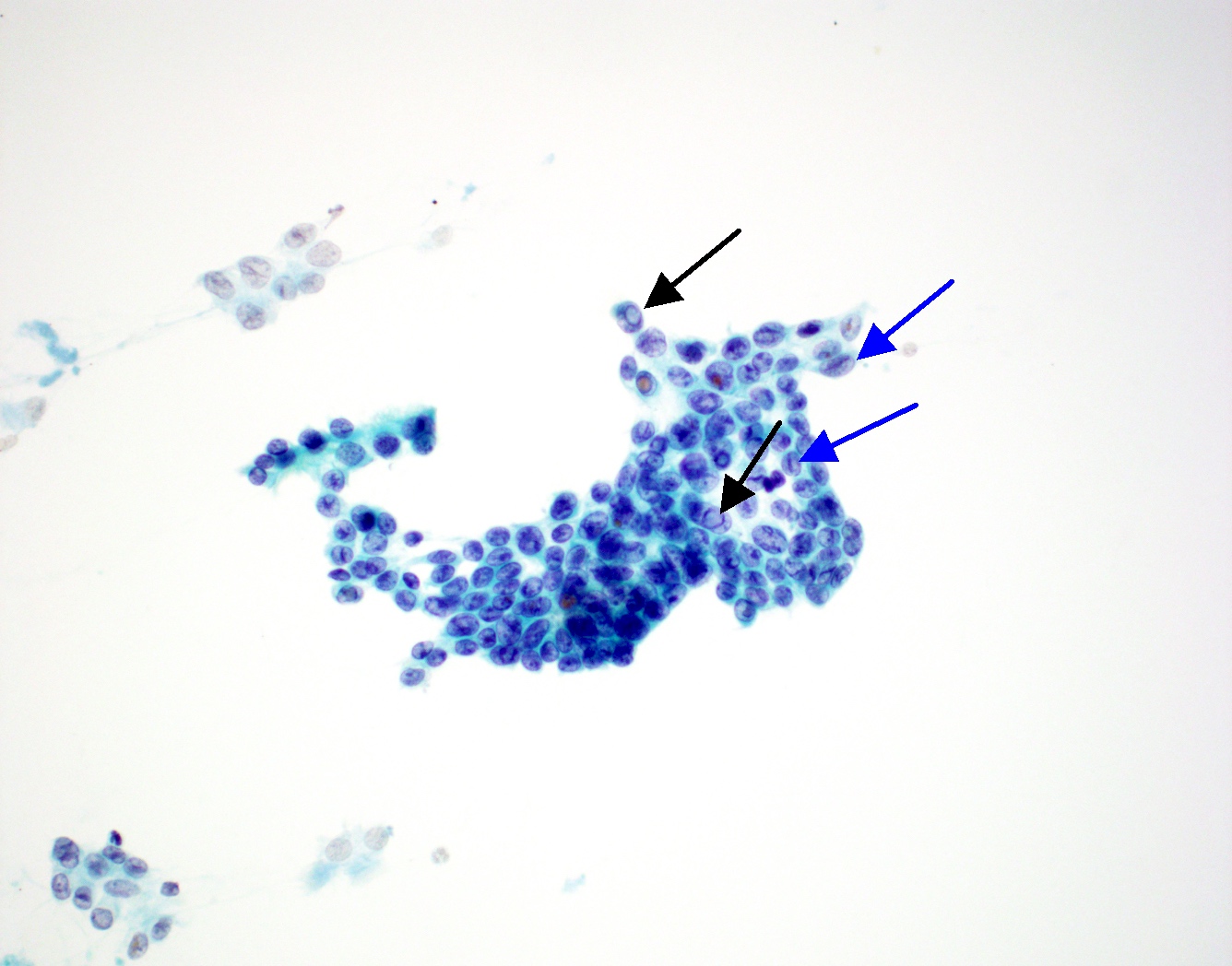
Cytology description
- Mild to moderate cytologic atypia
- Nuclear membrane irregularity, nuclear grooves and intranuclear pseudoinclusions (resembles papillary thyroid carcinoma cytology)
- Definitive diagnosis requires excision
Cytology images
Molecular / cytogenetics description
- About half of adenocarcinoma in situ cases harbor EGFR mutations (Ann Oncol 2015;26:156)
- EGFR mutation incidence is higher in Asian patients and KRAS mutation is seen more often in North American patients
- Ethnicity should not be considered in decision making; broad panel molecular testing is recommended for all patients who may benefit from targeted therapy (NCCN: NCCN Guidelines - Non-Small Cell Lung Cancer [Accessed 10 January 2022])
- Mutations of TP53 and NF1 were found to increase in frequency in adenocarcinoma in situ and minimally invasive adenocarcinoma (Am J Respir Crit Care Med 2020;201:697)
- More copy number loss was observed in adenocarcinoma in situ and minimally invasive adenocarcinoma rather than deleterious mutation burden, which was significantly greater in invasive adenocarcinoma (Am J Respir Crit Care Med 2020;201:697)
Videos
Adenocarcinoma in situ
by Dr. Thomas Colby
Sample pathology report
- Lung, middle lobe, right, lobectomy:
- Adenocarcinoma in situ (pTis) (see synoptic report)
- Tumor size: 25.0 mm
- Bronchial and vascular margins are negative for carcinoma
- Lung, right upper lobe; biopsy:
- Adenocarcinoma with lepidic pattern
- Note: Adenocarcinoma in situ cannot be definitely diagnosed until the entire tumor is examined and invasive adenocarcinoma ruled out. Thus, on small biopsy specimens, potential cases of adenocarcinoma in situ are signed out as above.
Differential diagnosis
- Atypical adenomatous hyperplasia (AAH):
- Atypical cells are not back to back
- Less cytologic atypia
- Size: < 5.0 mm
- Minimally invasive adenocarcinoma:
- ≤ 30.0 mm overall size and ≤ 5.0 mm focus of invasion
- Adenocarcinoma, lepidic predominant:
- > 30.0 mm overall size (see table 1) or > 5.0 mm focus of invasion
- Bronchiolar adenoma:
- Papillary growth pattern
- Has basal layer, ciliated cells and mucus cells
- Glandular papilloma:
- Usually central, endobronchial
- Papillary growth pattern
- Papillary adenoma:
- Papillary architecture, bland cytology
- Peribronchiolar metaplasia:
- Peribronchiolar ciliated cells are seen along alveolar septa
- Has basal layer
- Does not form mass
Table 1: Differential diagnosis of lepidic predominant lung tumors
| Overall size ≤ 30.0 mm | Overall size > 30.0 mm | |
Lepidic pattern only | Adenocarcinoma in situ | Adenocarcinoma, lepidic predominant (stage as pT1a) |
| Invasion ≤ 5.0 mm | Minimally invasive adenocarcinoma | Adenocarcinoma, lepidic predominant |
| Invasion > 5.0 mm | Adenocarcinoma, lepidic predominant | Adenocarcinoma, lepidic predominant |
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
On a resection specimen in which the tumor is entirely submitted, there is a 28.0 mm tumor with 2.0 mm of stromal invasion (acinar pattern). What is the diagnosis?
- Acinar predominant with lepidic adenocarcinoma
- Adenocarcinoma in situ
- Lepidic predominant with acinar adenocarcinoma
- Minimally invasive carcinoma
Board review style answer #2