Table of Contents
Definition / general | Clinical features | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Differential diagnosis | Additional referencesCite this page: Weisenberg E. Eosinophilic pneumonia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumoreosinophilic.html. Accessed April 1st, 2025.
Definition / general
- Acute eosinophilic pneumonia:
- Diagnosis of exclusion
- Lung disease associated with eosinophils in alveolar and interstitial spaces, usually with peripheral eosinophilia but excluding Langerhans cell histiocytosis
- Must exclude drug reactions (antibiotics, cytotoxic or anti-inflammatory drugs), immune disorders (Churg-Strauss syndrome, collagen vascular disease, asthma, hypereosinophilic syndrome, chronic eosinophilic leukemia NOS, myeloid and lymphoid neoplasms with eosinophilia and rheumatoid arthritis), infections (bacteria, Aspergillus, HIV, parasites - helminths, Dirofiliaria and filarial) or tobacco (flavored cigars, new onset of smoking (Chest 2007;131:1234, JAMA 2004;292:2997)
- Chronic eosinophilic pneumonia:
- Reaction to drugs, Aspergillus or other fungi, occurs with some malignancies and connective tissue diseases
- Prolonged (months) febrile illness with cough, weight loss, generalized fatigue, drenching night sweats and peripheral eosinophilia
- Associated with chronic asthma, usually in setting of allergic bronchopulmonary aspergillosis
- Xray: patchy infiltrates in peripheral lungs with central sparing
Clinical features
- Symptoms: fever, weight loss and shortness of breath
- Xray: peripheral infiltrate
- Classified as simple, acute or chronic
- Simple eosinophilic pneumonia (see Loeffler syndrome)
- Acute eosinophilic pneumonia: onset in 1 - 4 days, accompanied by fever, cough, dyspnea and chest pain; unknown cause, prominent eosinophils in bronchoalveolar lavage fluid and diffuse alveolar damage at biopsy (Am J Respir Crit Care Med 2002;166:1235)
Case reports
- 6 year old boy post chemotherapy for neuroblastoma with bilateral pulmonary infiltrates (Case #105)
Treatment
- Steroids cause dramatic response / complete resolution to acute or chronic forms
Gross description
- Chronic eosinophilic pneumonia: consolidation, mucus plugs in distal bronchi or bronchioles
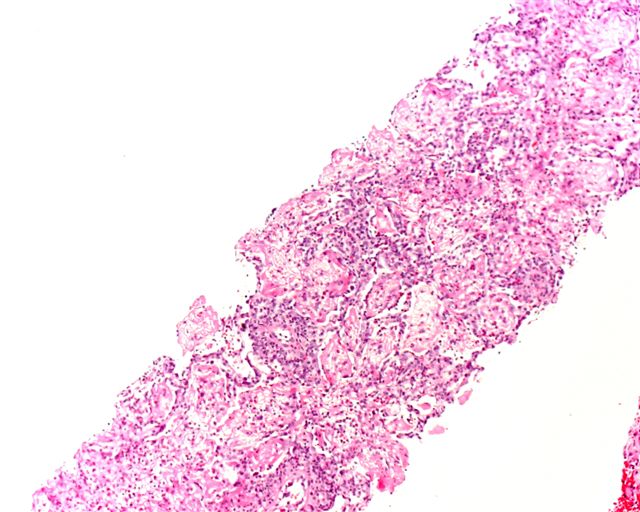
Microscopic (histologic) description
- Acute eosinophilic pneumonia:
- Acute form has diffuse alveolar damage
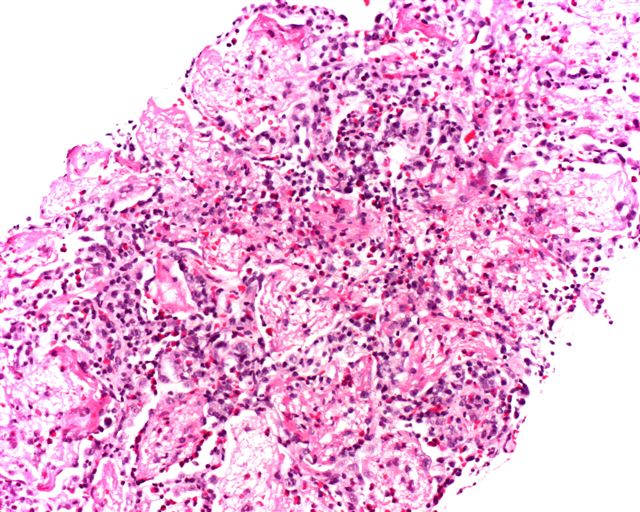
- Alveolar and interstitial infiltration by eosinophils, also plasma cells and histiocytes
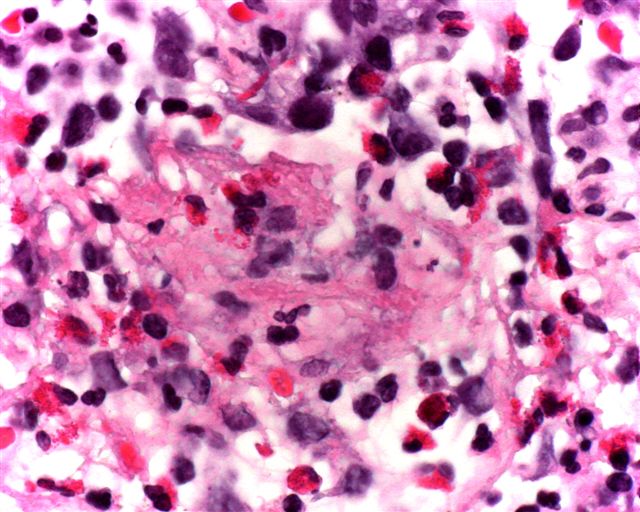
- May have Charcot-Leyden crystals
- Variable angiitis, granulomatosis, fibrosis, mucus plugging and bronchiolitis with necrosis
- Chronic eosinophilic pneumonia:
- Patchy intraalveolar edema, interstitial inflammation with giant cells and eosinophils with scattered histiocytes and plasma cells
- Mucus plugs composed of inflammatory cells and cellular debris
- Charcot-Leyden crystals may be present
- Often bronchiolitis obliterans
- Blood vessel infiltration by inflammatory cells is common but no vascular necrosis
- No diffuse alveolar damage
Differential diagnosis
- Desquamative interstitial pneumonitis (DIP):
- If extensive intra-alveolar macrophages
- Langerhans cell histiocytosis:
- Interstitial infiltrate, Langerhans cells
- Extrinsic allergic alveolitis:
- Less edema, more interstitial inflammation
- Parasites
- Fungal allergies
- Other causes of pulmonary eosinophilia must be excluded
Additional references