Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Munkhdelger J, Yoshikawa A, Bychkov A. COVID-19. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumorcovid.html. Accessed March 27th, 2025.
Definition / general
- Coronavirus disease 2019 (COVID-19) is an infectious respiratory disease caused by novel coronavirus SARS-CoV-2 that emerged in Wuhan, China at the end of 2019, resulting in a worldwide pandemic
- Infection control guidance for healthcare professionals:
- CDC (CDC: Infection Control Guidance for Healthcare Professionals About Coronavirus (COVID-19) [Accessed 20 March 2023])
- Personal protective equipment (PPE) basics (CDC: Using Personal Protective Equipment (PPE) [Accessed 20 March 2023])
- Autopsy guidelines:
- Personal protective equipment (Pathol Res Pract 2020;216:153039)
- CAP (CAP: Amended COVID-19 Autopsy Guideline Statement from the CAP Autopsy Committee [Accessed 20 March 2023])
- CDC (CDC: Collection and Submission of Postmortem Specimens from Deceased Persons with Known or Suspected COVID-19 [Accessed 20 March 2023])
- Health and Safety Executive (HSE: Handling the Deceased with Suspected or Confirmed COVID-19 [Accessed 28 March 2023])
- Italian experience (Virchows Arch 2020;476:821)
Essential features
- COVID-19 is a viral infection caused by coronavirus SARS-CoV-2 that can progress to severe acute respiratory syndrome with pneumonia and acute respiratory distress syndrome
- The disease spread rapidly and became a pandemic with > 100 million confirmed cases and over 2 million deaths worldwide by end of January 2021
- Histologically, COVID-19 shows diffuse alveolar damage corresponding to the phase of the disease (acute to fibrotic), divided into 3 main injury patterns: epithelial, vascular and fibrotic
- Definite diagnosis is based on detection of viral RNA by RT-PCR
Terminology
- COVID-19 is also called novel coronavirus pneumonia
- Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is also called 2019 novel coronavirus (2019-nCoV)
ICD coding
Epidemiology
- COVID-19 pandemic
- In December 2019, cases of pneumonia with unknown etiology were reported from Wuhan, Hubei Province, China to WHO (WHO: Novel Coronavirus (2019-nCoV) Situation Report - 1 [Accessed 20 March 2023])
- In January 2020, the Chinese authorities identified a novel type of coronavirus, which was later named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
- At the beginning of February 2020, almost 10,000 cases of COVID-19 were confirmed in China and 100+ cases were detected outside of China (WHO: Novel Coronavirus (2019-nCoV) Situation Report - 11 [Accessed 20 March 2023])
- The disease spread rapidly and became a pandemic with > 100 million confirmed cases and over 2 million deaths worldwide by end of January 2021
- By late September 2022, confirmed cases approached 580+ million with over 6.5 million deaths worldwide
- The United States now has the most confirmed cases (> 89 million) and confirmed deaths (> 1,000,000) worldwide (WHO: Coronavirus (COVID-19) Dashboard - Table [Accessed 20 March 2023])
- Coronavirus maps:
- An early mutated variant of SARS-CoV-2, B.1.1.7 (Alpha) was identified in September 2020, followed by B.1.351 variant (Beta), first identified in South Africa, the P.1 variant (Gamma), first identified in Brazil, and the Delta strain, first reported in India (Immunotherapy 2022;14:351)
- In November 2021, the latest Omicron SARS-CoV-2 variant was designated by WHO and it had been identified in 149 countries by January 2022; the variant is currently the dominant variant circulating globally (WHO: Statement on Omicron Sublineage BA.2 [Accessed 20 March 2023])
- Person to person transmission is suspected to occur via respiratory droplets (cough, sneeze)
- The key to slowing the spread of this disease is widespread testing so that patients can be quickly identified / isolated and vaccination
- COVID-19 (SARS-CoV-2) testing
- By 2022, there are 11 WHO approved vaccines and the most commonly used ones are (Immunotherapy 2022;14:351, Front Immunol 2022;13:872683, COVID19 Vaccine Tracker: World Health Organization (WHO) [Accessed 20 March 2023])
- BNT162b2 (BioNTech / Pfizer)
- mRNA-1273 (Moderna)
- ChAdOx1 (AstraZeneca)
- Ad26.COV2.S (Janssen)
- BBIBP-CorV (Sinopharm)
- By mid 2022, approximately 66% of the world population had received at least one dose of a COVID-19 vaccine, 12.3 billion doses have been given globally and ~27 million new doses are administered daily (Our World in Data: Coronavirus (COVID-19) Vaccinations [Accessed 20 March 2023])
Sites
- Upper respiratory tract in mild disease
- Bilateral lobes of the lung in more severe disease
Pathophysiology
- Spike surface glycoprotein of the virus binds to the host via receptor binding domains of the angiotensin converting enzyme 2 (ACE2), which is most abundant in type II alveolar cells (J Virol 2020;94:e00127-20)
- 10 - 20 times higher binding affinity as compared with the SARS-CoV-1 virus (J Pathol 2020;251:228)
- After a SARS-CoV-2 attaches to a target cell, the virion releases RNA into the cell, initiating replication of the virus which further disseminates to infect more cells (Cell 2020;181:271)
- SARS-CoV-2 produces several virulence factors that promote shedding of new virions from host cells and inhibit immune response
- Virus independent immunopathology in fatal COVID-19 (Am J Respir Crit Care Med 2021;203:192)
- Organ injury and death in COVID-19 is immune mediated rather than pathogen mediated
- Tissue inflammation and organ dysfunction in fatal COVID-19 do not correlate with the tissue and cellular distribution of SARS-CoV-2
Etiology
- Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a positive sense, single stranded RNA virus having close genetic similarity to bat coronaviruses (Nature 2020;579:270)
Diagrams / tables
Clinical features
- Average time from exposure to symptom onset is 5 days (Ann Intern Med 2020;172:577)
- 97.5% of people who develop symptoms do so within 11.5 days (JAMA 2020;324:782)
- Asymptomatic infection rate is 46% (J Med Virol 2020;92:2543)
- Rare in children, about ~2 - 5% of confirmed cases, with milder symptoms and very low hospitalization rate (< 7%) (JAMA 2020;324:782)
- Common symptoms in hospitalized patients (JAMA 2020;324:782):
- Fever (70 - 90%)
- Dry cough (60 - 86%)
- Shortness of breath (53 - 80%)
- Fatigue (38%)
- Myalgias (15 - 44%)
- Nausea / vomiting or diarrhea (15 - 39%)
- Headache, weakness (25%)
- Patients can present with nonclassical symptoms (JAMA 2020;324:782):
- Isolated gastrointestinal symptoms
- Isolated anosmia or ageusia (3%)
- COVID-19 can progress to severe acute respiratory syndrome and its major clinicopathological phenotypes include pneumonia and acute respiratory distress syndrome
- Distribution of severity (JAMA 2020;323:1239):
- Mild or no disease: 81%
- Severe disease: 14%
- Critical disease: 5%
- Overall case fatality rate: 2.3%
- 20 - 42% of hospitalized patients developed acute respiratory distress syndrome (JAMA Intern Med 2020;180:934, JAMA 2020;323:1061)
- Distribution of severity (JAMA 2020;323:1239):
- Patients who required ICU supportive care presented with acute respiratory distress syndrome, acute cardiac injury, acute kidney injury and shock; up to 15% of them had fatal outcomes (Travel Med Infect Dis 2020;34:101623)
- Common complications among hospitalized patients (JAMA 2020;324:782):
- Pneumonia (75%)
- Acute respiratory distress syndrome (15%)
- Acute liver injury (19%)
- Cardiac injury (7 - 17%): troponin elevation, acute heart failure, dysrhythmias, myocarditis (JAMA 2020;324:782)
- Prothrombotic coagulopathy resulting in venous and arterial thromboembolic events (10 - 25%)
- Acute kidney injury (9%)
- Acute cerebrovascular disease (3%)
- Shock (6%)
- A rare multisystem inflammatory syndrome similar to Kawasaki disease has recently been described in children (2 per 100,000 persons aged < 21 years) (JAMA 2020;324:782)
- Post acute COVID-19 syndrome: persistent symptoms, delayed or long term complications beyond 4 weeks
- Persistent ≥ 1 symptom was reported in 32.6 - 87.4% of cases (fatigue, joint pain, chest pain, dyspnea, cough, loss of taste / smell, headache, diarrhea) (Nat Med 2021;27:601)
Diagnosis
- Diagnostic testing of SARS-CoV-2 (COVID-19)
- Nasopharyngeal swab is recommended for the PCR specimen; oropharyngeal swab, sputum and bronchoalveolar lavage may be used alternatively based on the manufacturer's instructions (CDC: Interim Guidelines for Collecting, Handling, and Testing Clinical Specimens from Persons for Coronavirus Disease 2019 (COVID-19) [Accessed 20 March 2023])
- Positive rates of SARS-CoV-2 PCR testing by specimen types: bronchoalveolar lavage fluid (93%), sputum (72%), nasal swabs (63%), pharyngeal swabs (32%) (JAMA 2020;324:782)
- Definite diagnosis is based on detection of viral RNA by real time RT-PCR via many available laboratory tests (CDC: Information for Laboratories [Accessed 20 March 2023])
- False negative test results may occur in up to 20 - 67% of patients depending on the quality and timing of testing
- A modeling study estimated sensitivity at 33% 4 days after exposure, 62% on the day of symptom onset and 80% 3 days after symptom onset (JAMA 2020;323:1843)
- Number of SARS-CoV-2 antigen (rapid) tests are currently in use for point of care and at home test settings (FDA: In Vitro Diagnostics EUAs - Antigen Diagnostic Tests for SARS-CoV-2 | FDA [Accessed 20 March 2023])
Laboratory
- Meta analysis data (Travel Med Infect Dis 2020;34:101623):
- Decreased albumin
- High C reactive protein
- High lactate dehydrogenase (LDH)
- Lymphopenia
- High erythrocyte sedimentation rate (ESR)
- D dimer elevation (J Pathol 2020;251:228)
Radiology description
- Ground glass opacities, crazy paving pattern and consolidation in bilateral lobes are common findings (Radiology 2020;295:715)
- 15% of CT and 40% of chest radiograph findings are normal early in the disease (JAMA 2020;324:782)
- Evolution of abnormalities occurs in the first 2 weeks after onset
Prognostic factors
- Risks of acute respiratory distress syndrome development include age (> 65 years), underlying diseases (diabetes mellitus) and secondary infection (JAMA Intern Med 2020;180:934, Intensive Care Med 2020;46:846)
- Risk factors for disease progression: male, old age (> 65 years) and smoking (J Infect 2020;81:e16)
- Risk factors for critical / mortal states, in order of strength of association (Lancet 2020;395:1054):
- Cardiovascular disease
- Respiratory disease
- Diabetes
- Hypertension
Case reports
- Infant girl with COVID-19 hepatitis (Arch Pathol Lab Med 2020 Apr 17 [Epub ahead of print])
- 44 year old man and 62 year old woman with COVID-19 pneumonia (Diagn Pathol 2020;15:73)
- 65 year old man with multiorgan failure (Hum Pathol 2020;101:82)
- 71 year old man with COVID-19 acute respiratory failure; real time correlation with transbronchial biopsy (Virchows Arch 2021;479:827)
- 73 year old man and 84 year old woman with lung cancer and coincidental COVID-19 (J Thorac Oncol 2020;15:700)
- 76 year old woman with COVID-19 pneumonia (N Engl J Med 2020;383:380)
- 79 year old woman with residual SARS-CoV-2 in pulmonary tissues (Cell Res 2020;30:541)
- Autopsy case series (Lancet Respir Med 2020;8:420, Mod Pathol 2020;33:1007)
- Autopsy case series in COVID-19 vaccinees, high viral loads in organ systems in vaccinees with accentuation in incomplete vaccination (Mod Pathol 2022;35:1013)
- Biopsy proven myocarditis case series after COVID-19 vaccination (Int J Mol Sci 2022;23:6940, Clin Res Cardiol 2021;110:1855)
Treatment
- Home management is recommended for patients with mild symptoms
- Optimal duration of home isolation is under investigation but in hospitalized patients the virus is shed for an average of approximately 20 days after disease onset (Lancet 2020;395:1054)
- Antiviral drugs are recommended to patients who are at high risk of progressing to severe COVID-19 (paxlovid, remdesivir, molnupiravir) (NIH: Therapeutic Management of Nonhospitalized Adults with COVID-19 [Accessed 20 March 2023])
- Patients with severe disease require hospital care
- May need oxygenation support, ranging from low dose oxygen supplement to invasive ventilation and extracorporeal membrane oxygenation (ECMO)
- Among the antiviral drugs (ribavirin, favipiravir, remdesivir) undergoing clinical testing, remdesivir seems to be most promising (JAMA 2020;324:782)
- NIH COVID-19 Treatment Guidelines Panel recommends using dexamethasone in patients on ventilators and in those that require supplemental oxygen but not in other patients (Lancet 2020;395:1054, CDC: Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19) [Accessed 20 March 2023], WHO: Coronavirus disease (COVID-19) Technical Guidance - Patient Management [Accessed 20 March 2023], NIH: COVID-19 Treatment Guidelines - Corticosteroids [Accessed 20 March 2023])
Gross description
- From pulmonary edema to lung consolidation (J Clin Pathol 2020;73:239)
- Increased lung weight
- Hemorrhagic changes (Mod Pathol 2020;33:2128)
- Macroscopic pulmonary emboli (Mod Pathol 2020;33:2128)
- Pleural inflammation with or without effusion may be seen
- Purulent inflammation, if secondary infection superimposed
Gross images
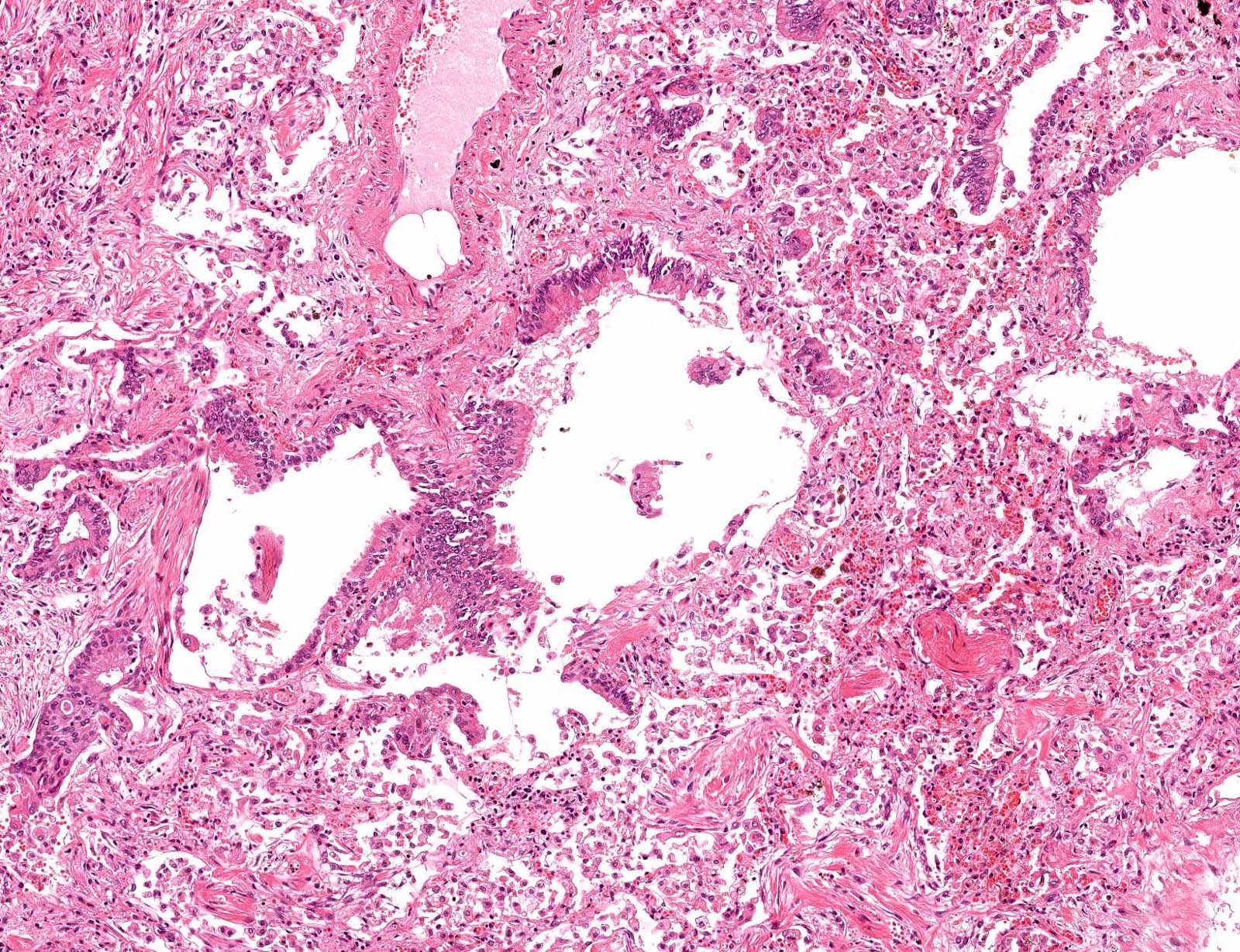
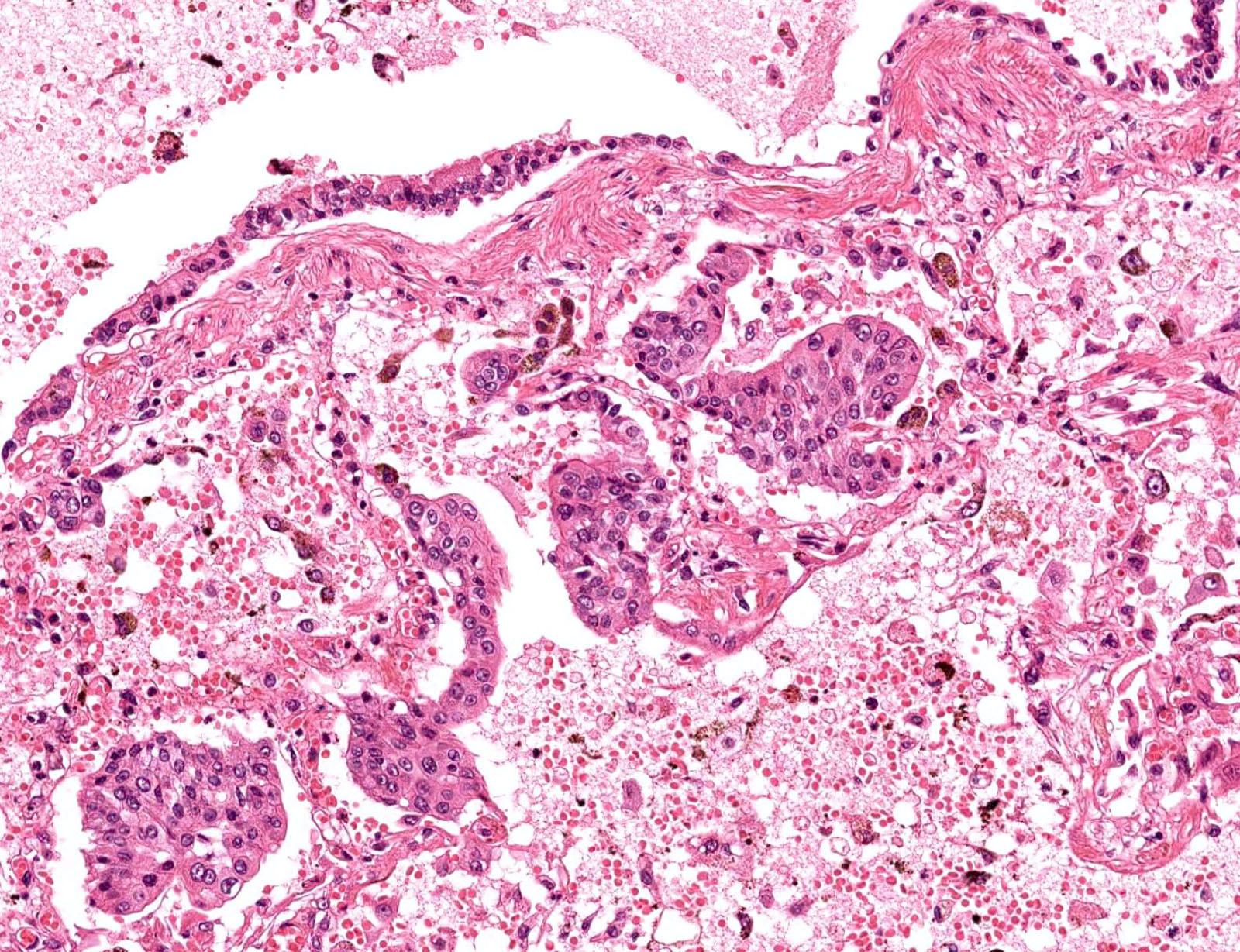
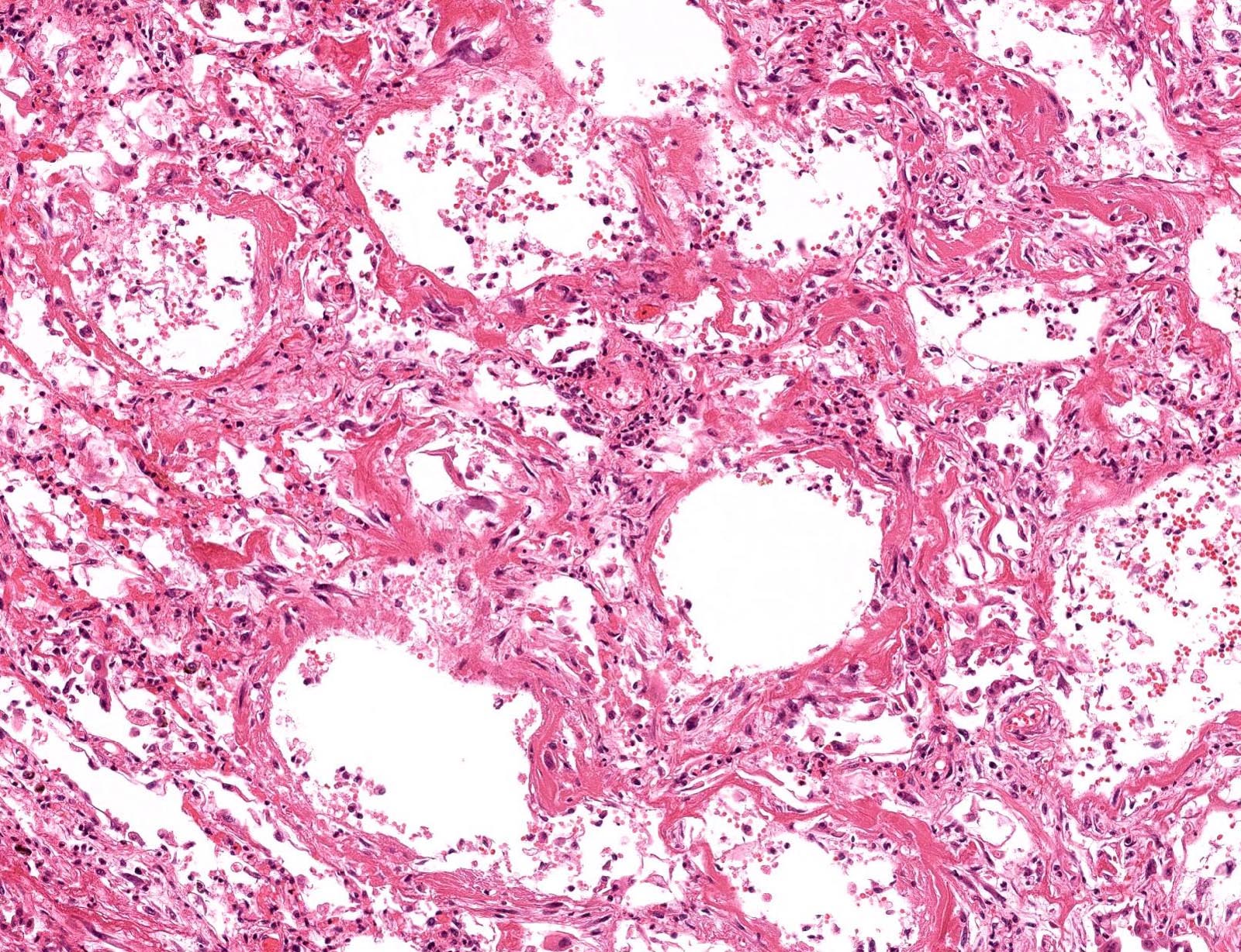
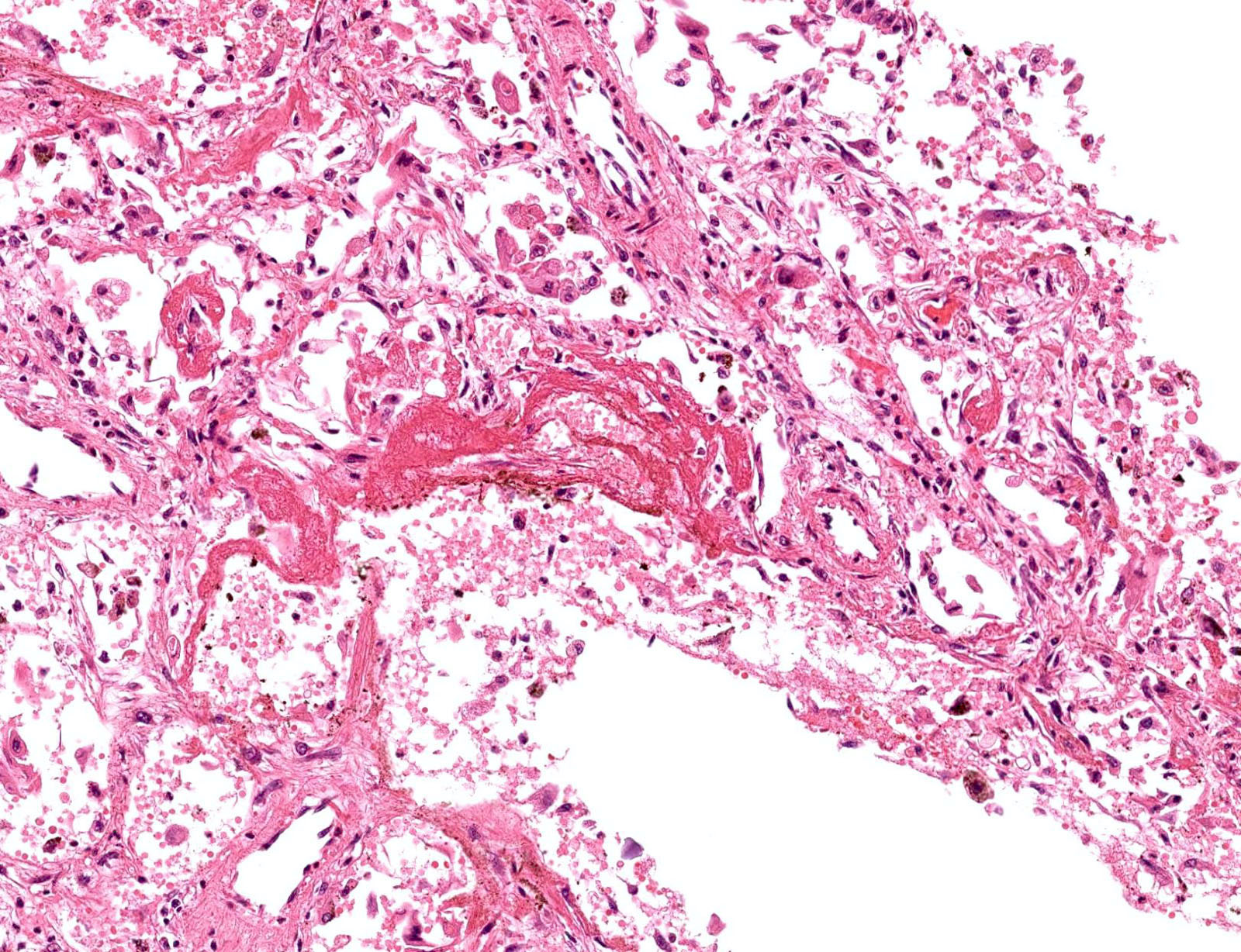
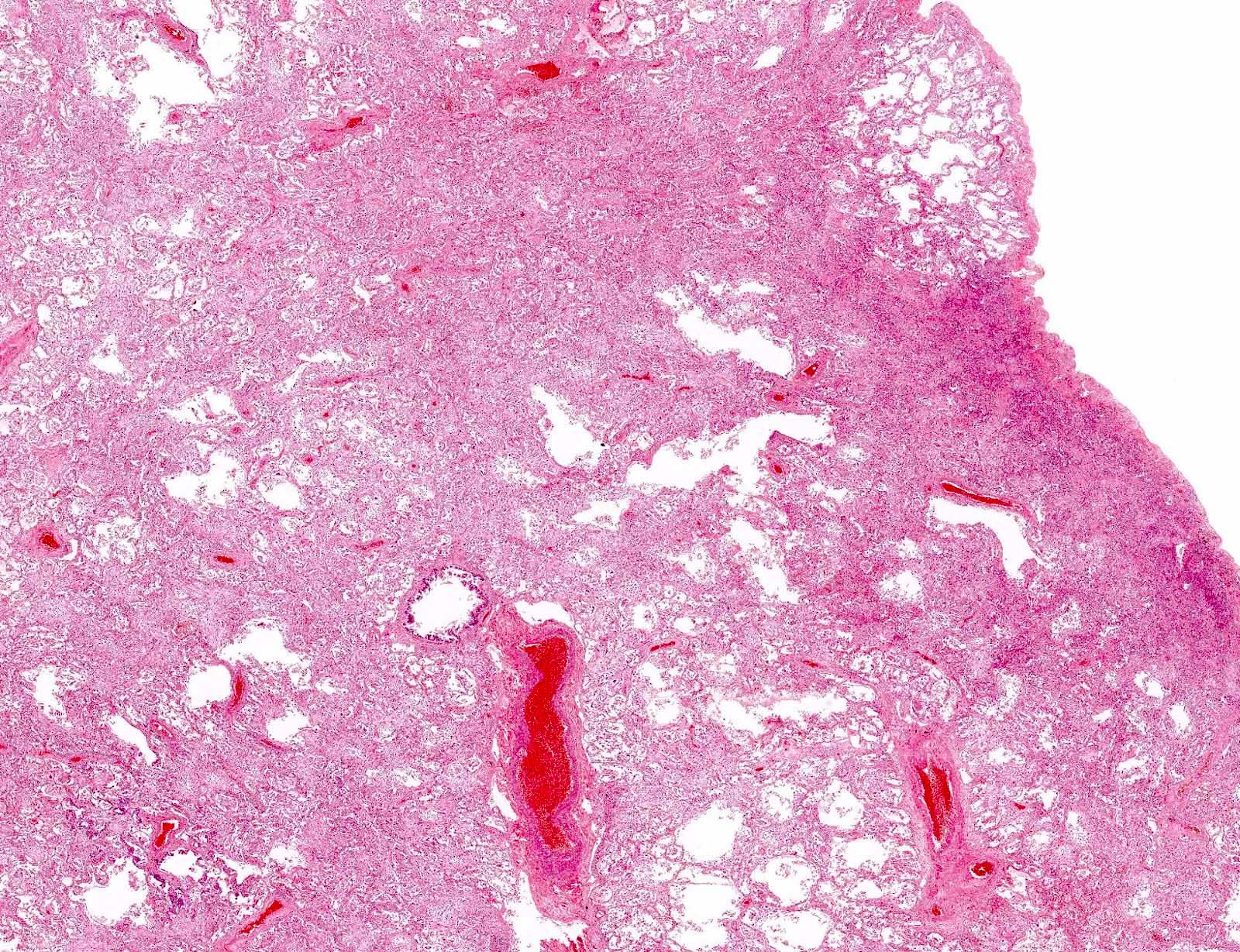
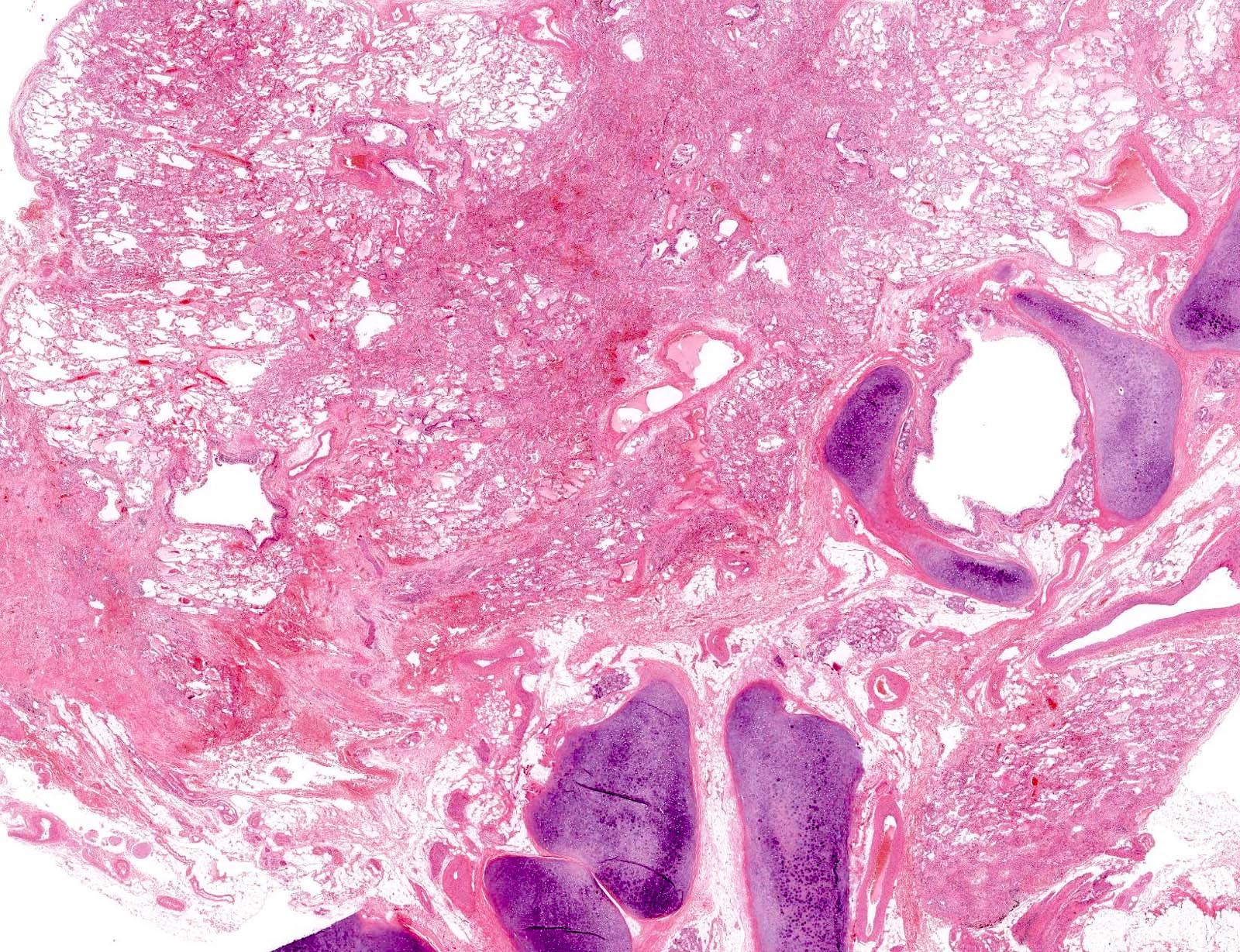
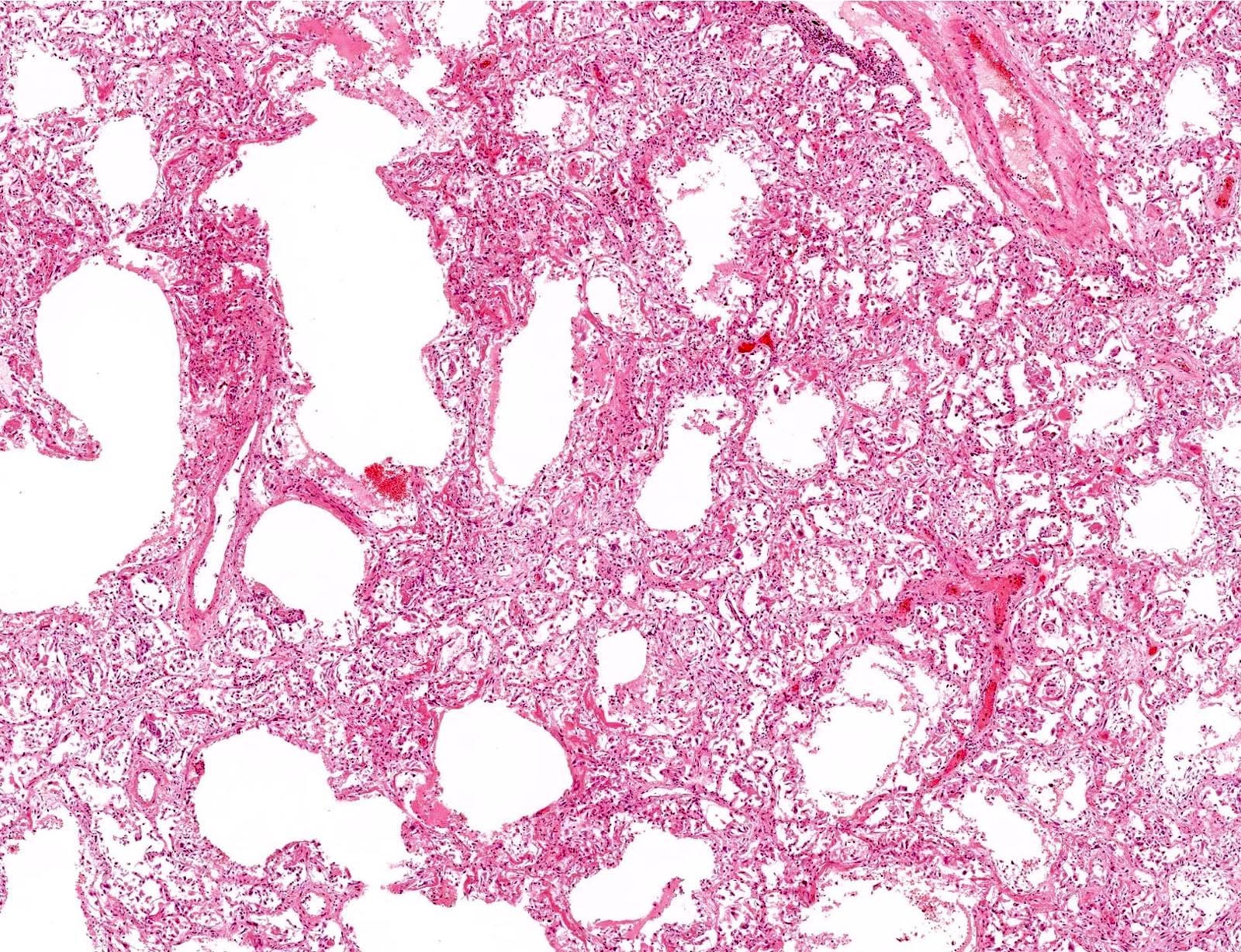
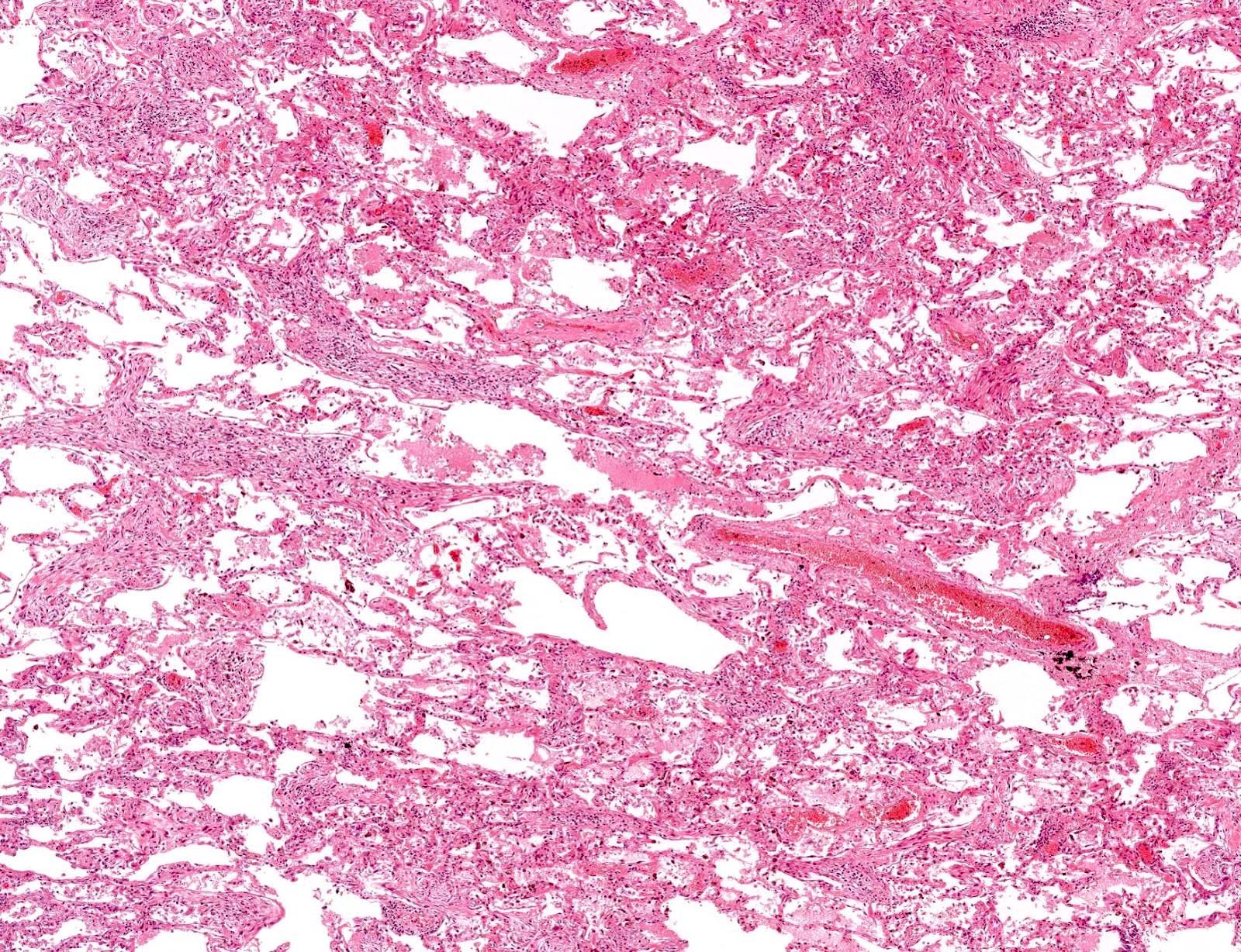
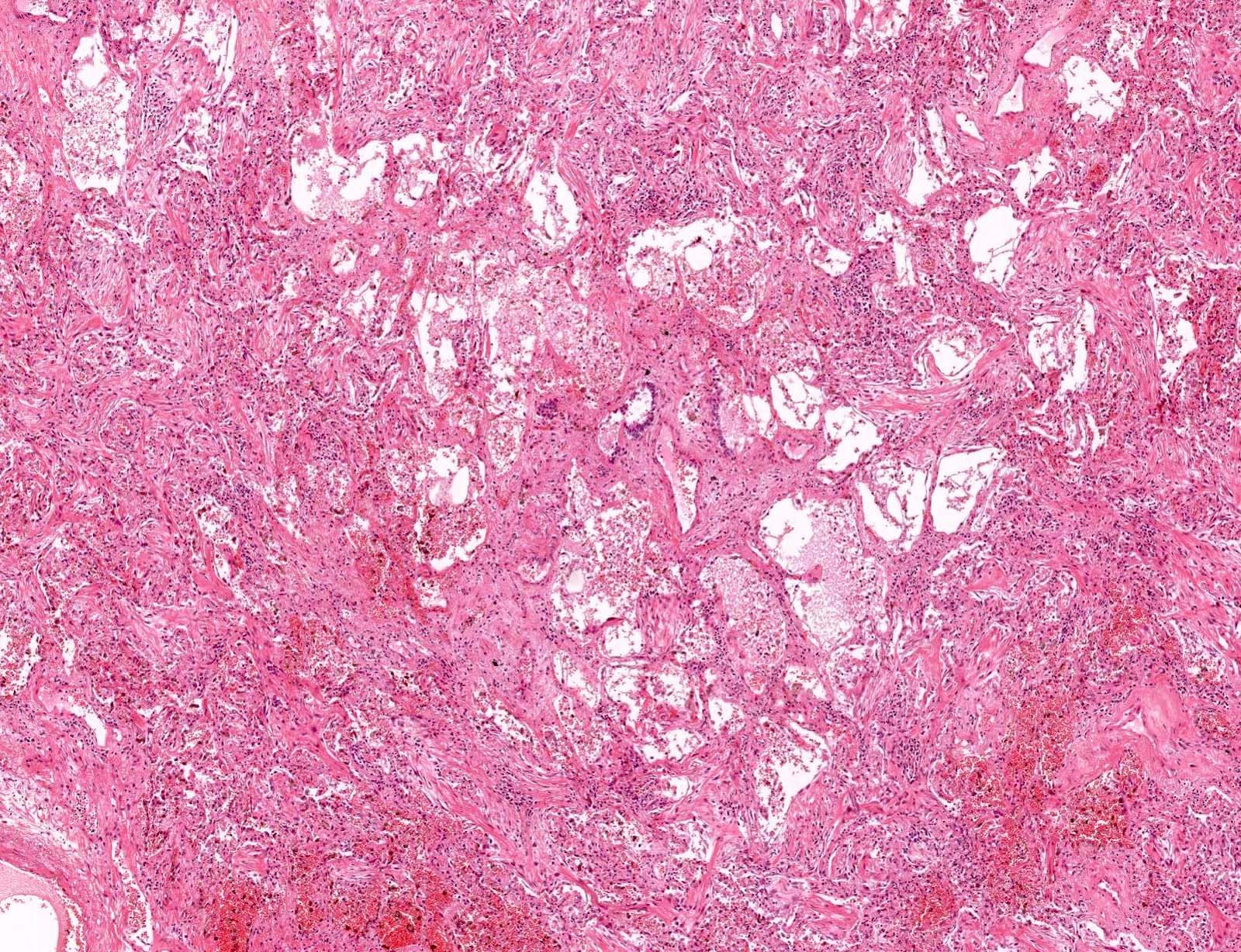
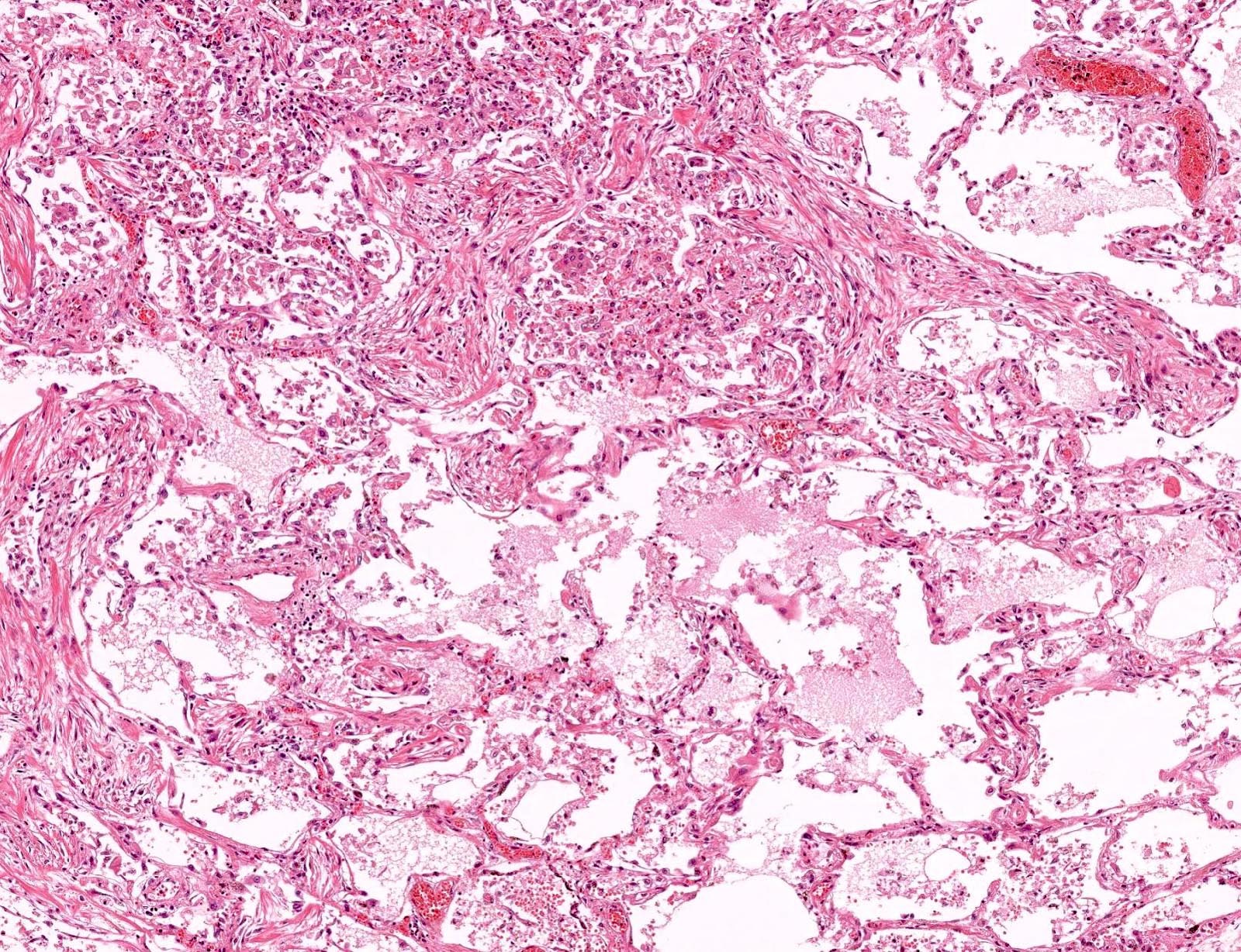
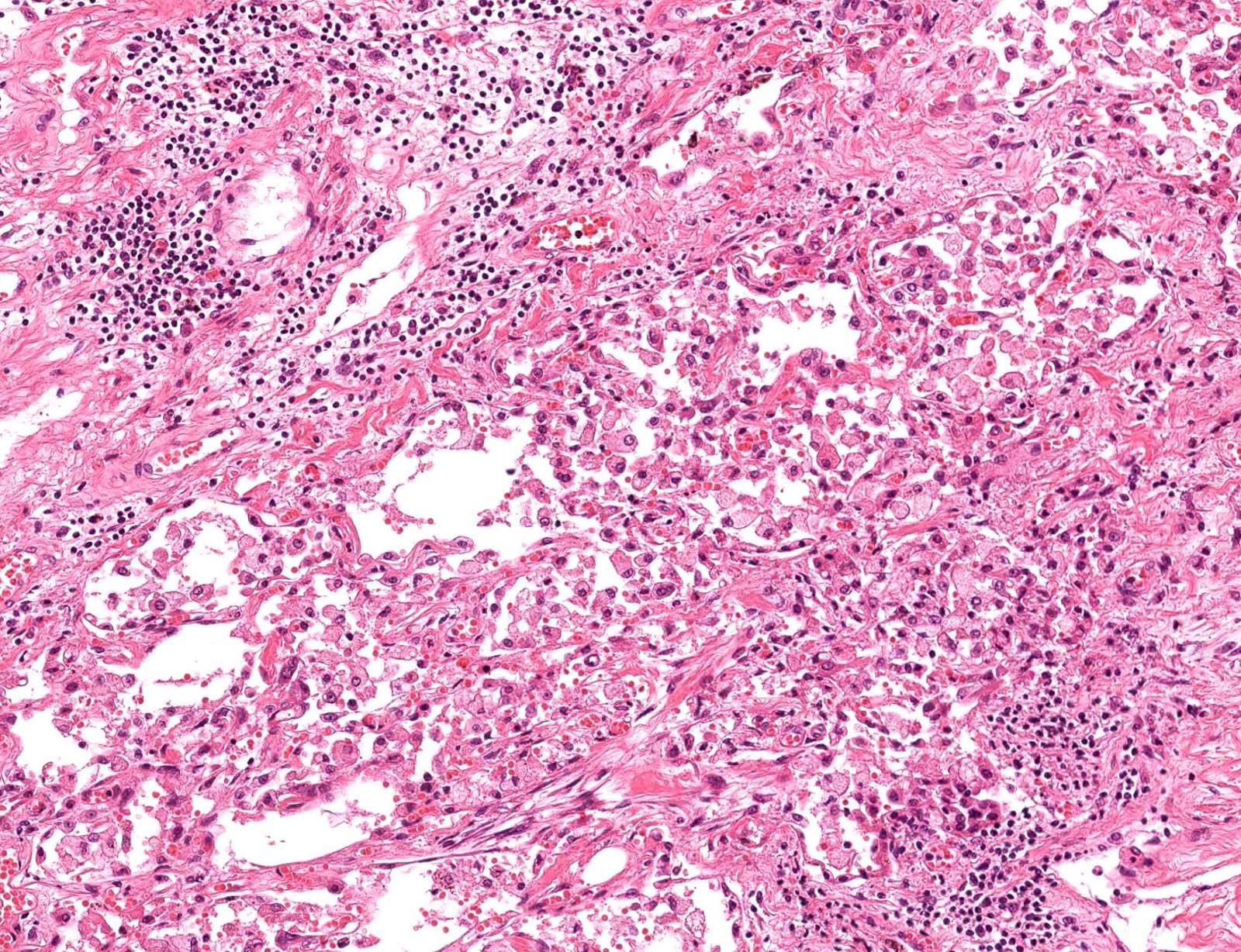
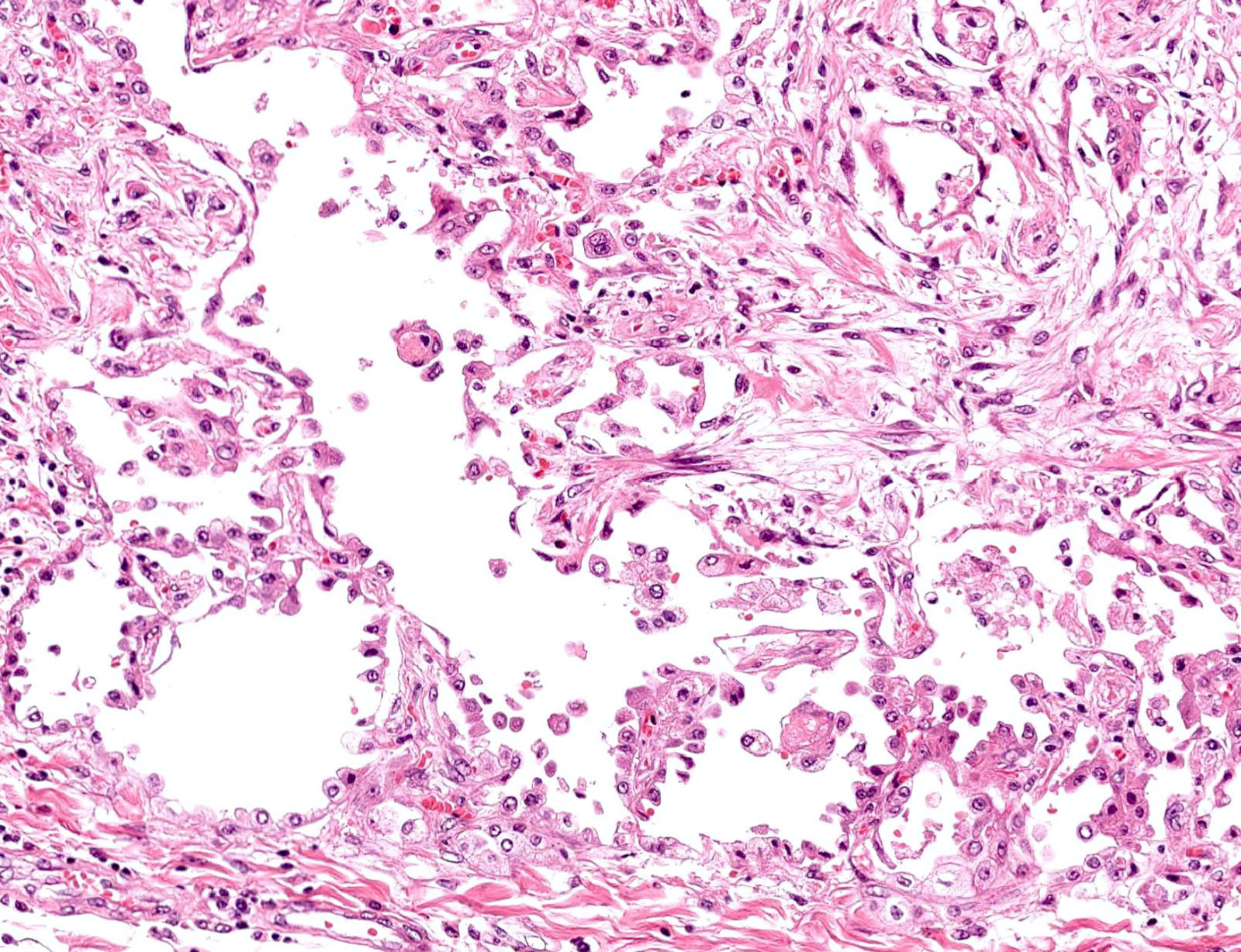
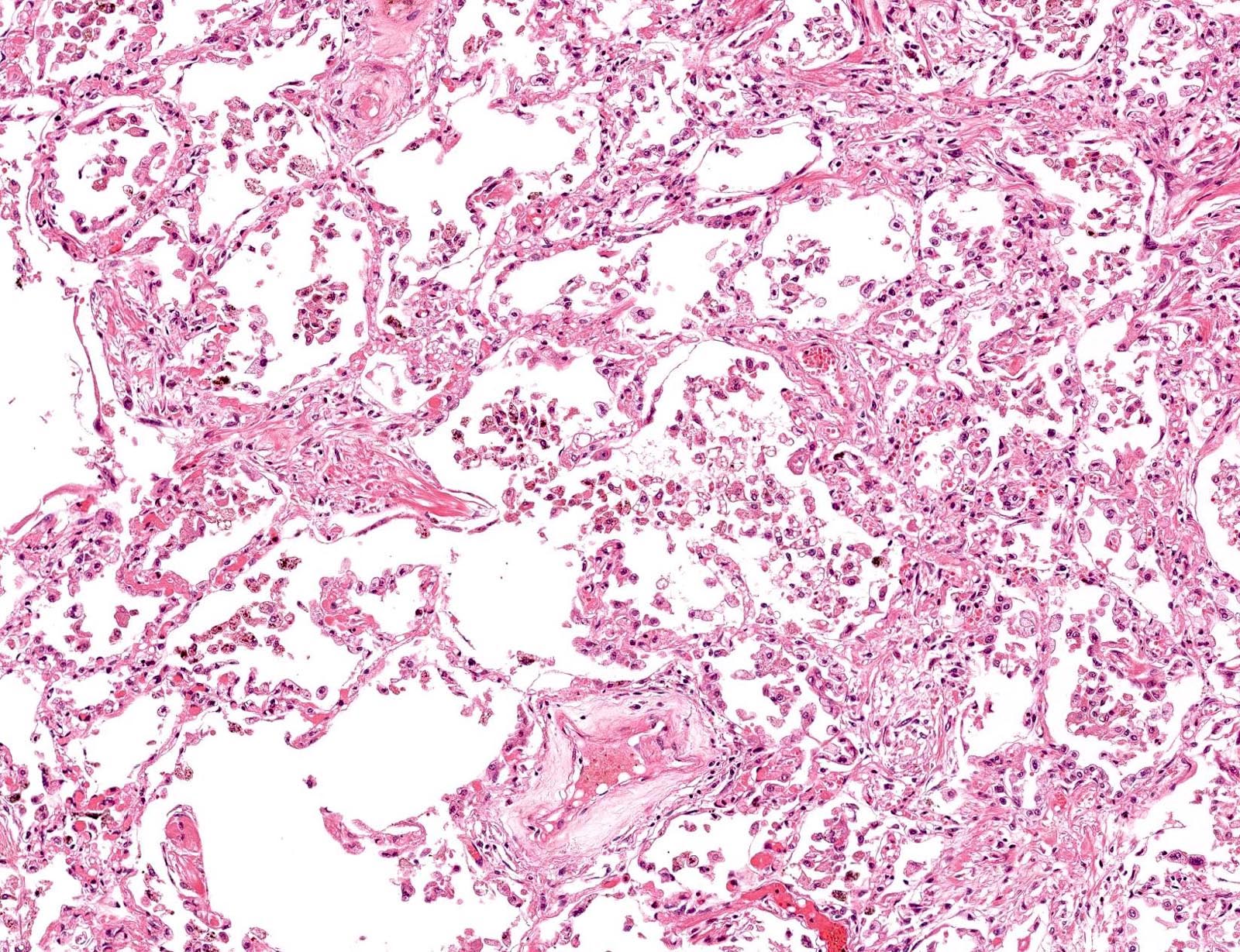
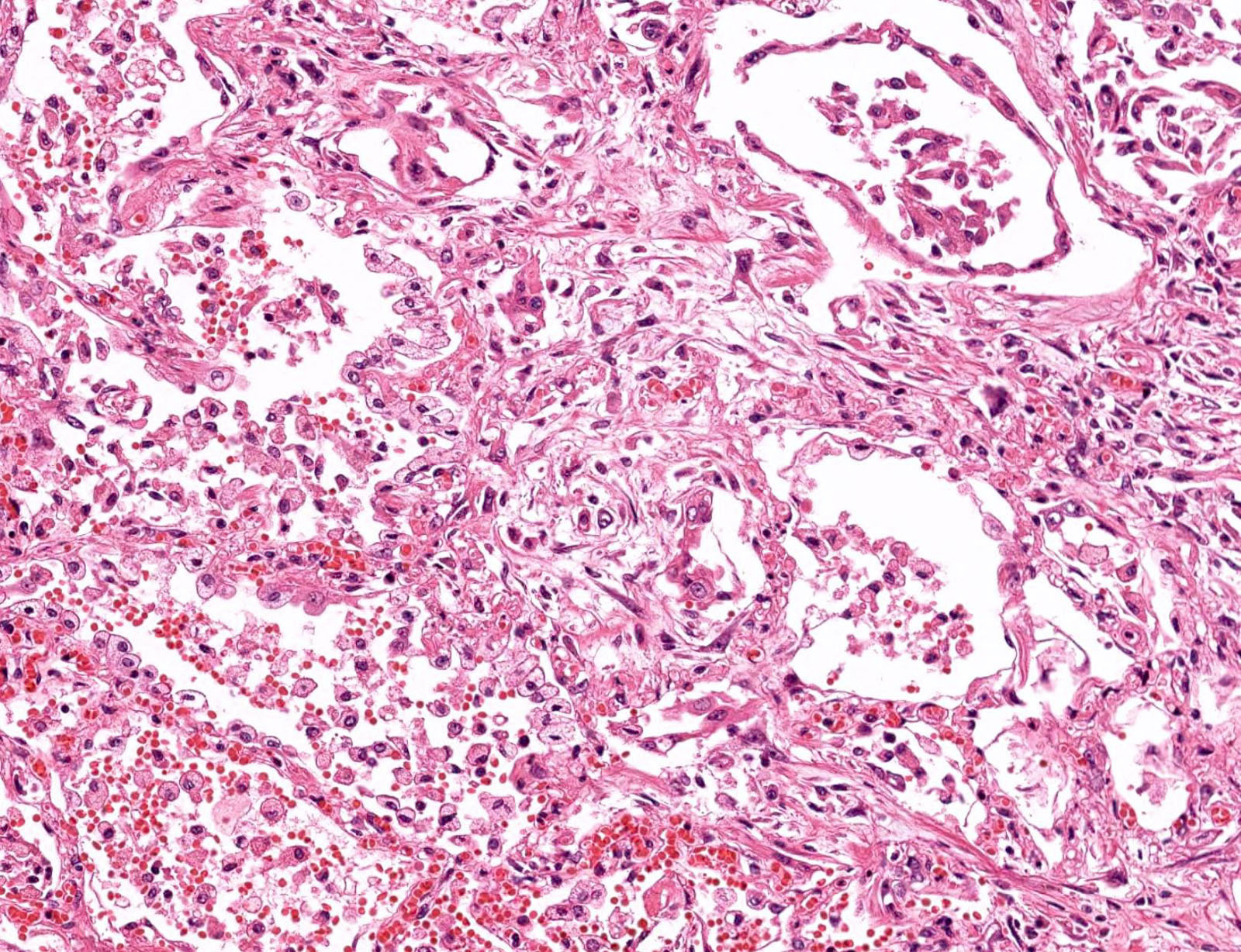
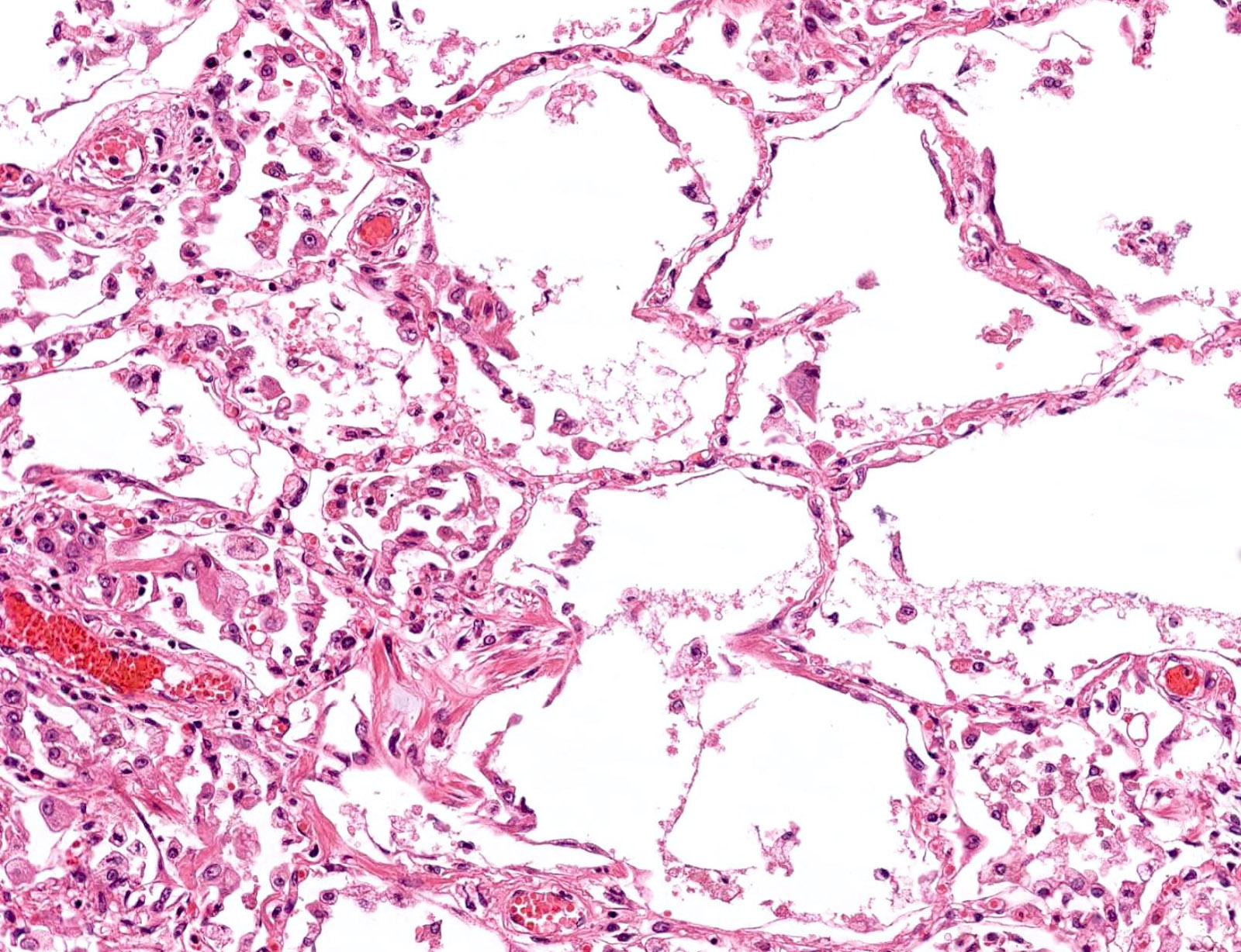
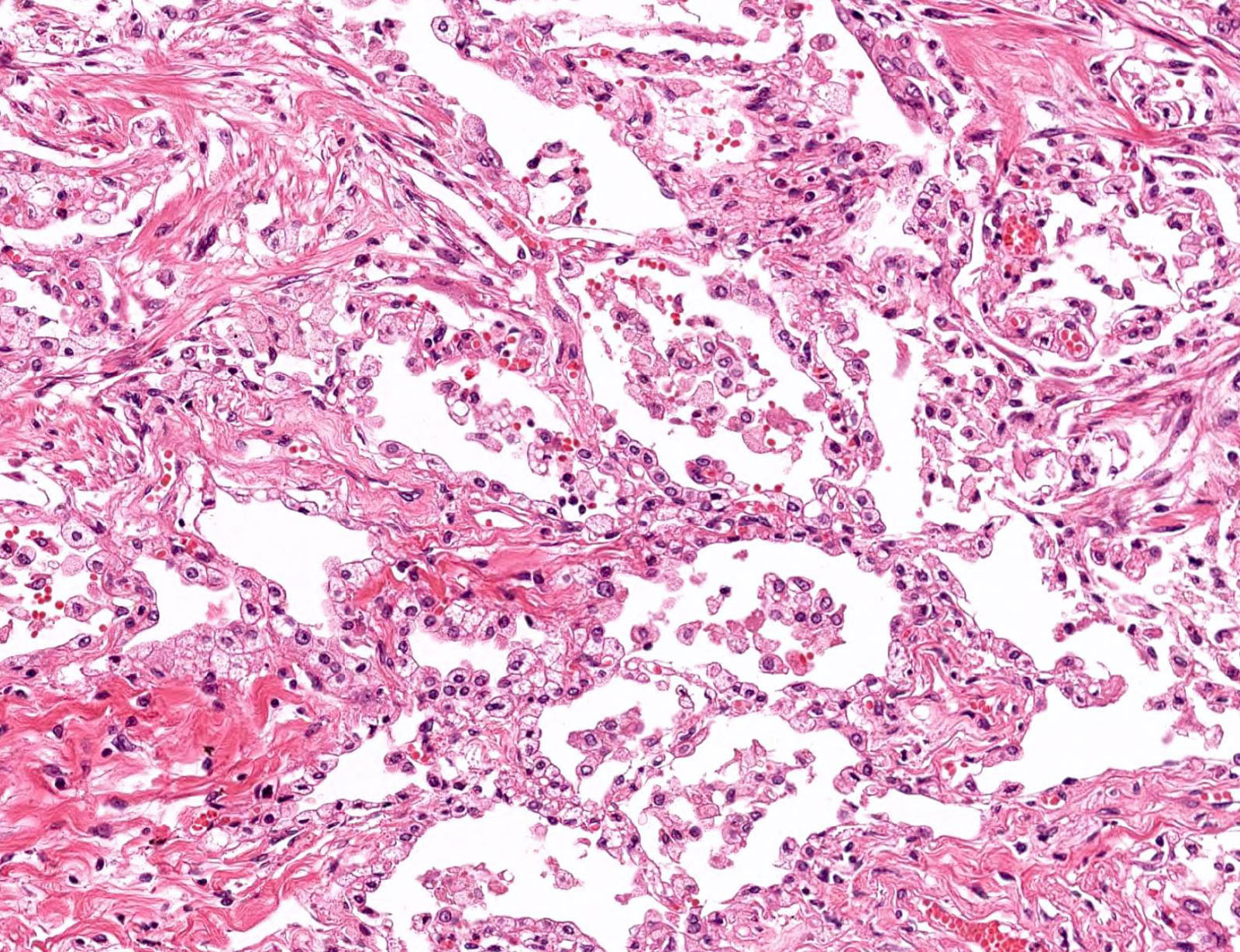
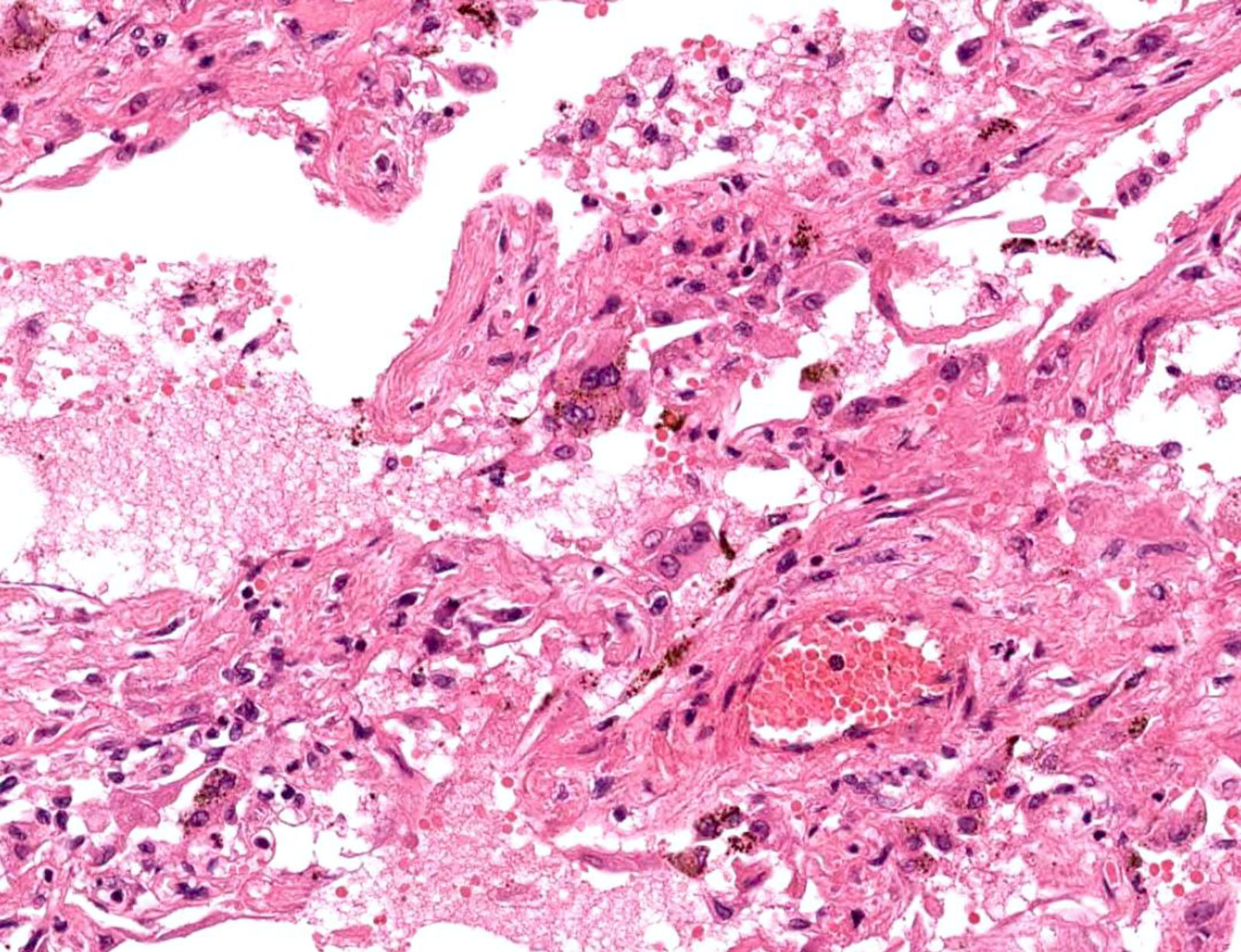
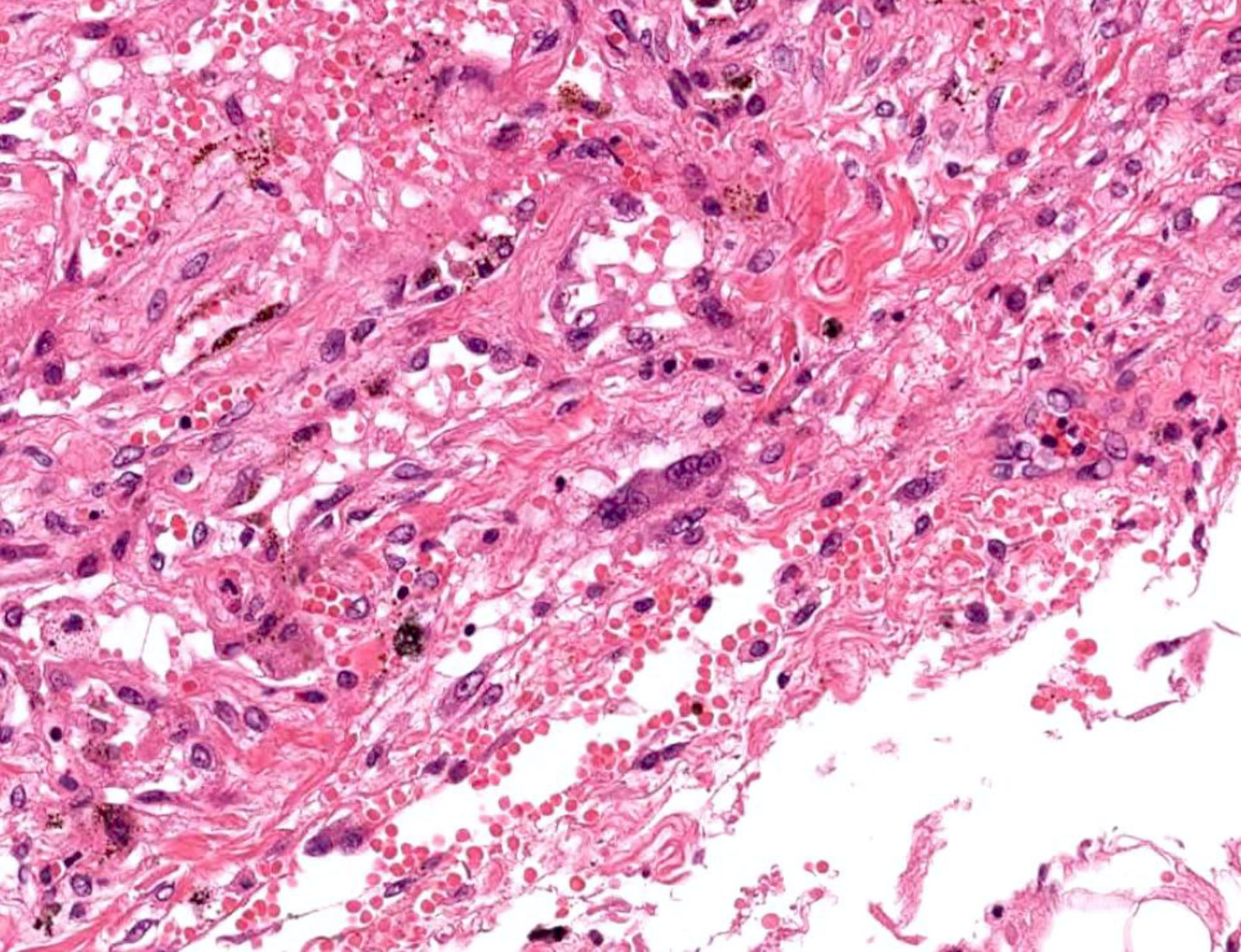
Microscopic (histologic) description
- Pulmonary changes are the most significant, although nonspecific (Lancet Respir Med 2020;8:420, J Thorac Oncol 2020;15:700, Mod Pathol 2020;33:1007)
- Findings of diffuse alveolar damage (DAD) corresponding to the phase of disease:
- Exudative phase: hyaline membrane formation, desquamation of pneumocytes, cellular or proteinaceous exudates, alveolar hemorrhage, fibrinoid necrosis of small vessels
- Organizing phase: interstitial and intra-alveolar proliferation of fibroblasts, lymphocytic infiltration, type II pneumocyte hyperplasia, fibrin deposition
- Fibrotic phase: dense collagenous fibrosis, architectural remodeling
- Lung injury patterns (Mod Pathol 2020;33:2128, Eur J Clin Invest 2020;50:e13259):
- Epithelial (85%): DAD with varying degrees of organization, denudation, hyperplasia of pneumocytes
- DAD in COVID-19 is as frequent as in SARS and H1N1 Influenza (Chest 2021;159:73)
- Vascular (59%): diffuse intra-alveolar fibrin, microvascular damage, (micro) thrombi, acute fibrinous and organizing pneumonia
- More vascular changes (hemangiomatosis-like changes, thromboemboli, pulmonary infarcts, perivascular inflammation) in fatal COVID-19 cases compared to DAD of other causes (Am J Respir Crit Care Med 2022;206:857)
- Fibrotic (22%): fibrotic DAD, interstitial fibrosis
- Prominent ongoing fibrosis in explanted lungs, accompanied by abundant macrophage infiltration, neoangiogenesis and persistent microvascular thrombosis (Am J Clin Pathol 2022;157:908)
- Epithelial (85%): DAD with varying degrees of organization, denudation, hyperplasia of pneumocytes
- Viral infection changes:
- Multinucleated enlarged pneumocytes with large nuclei, amphophilic cytoplasm and prominent nucleoli in alveolar spaces
- Intranuclear inclusions
- Bacterial pneumonia may be superimposed
- Findings of diffuse alveolar damage (DAD) corresponding to the phase of disease:
- Extrapulmonary changes (Mod Pathol 2020;33:2128):
- Cardiovascular: mild pericardial edema, some serosanguinous pericardial effusion, mild myocardial edema, low grade interstitial infiltration of mononuclear cells, endotheliitis
- Widespread systemic vasculitis with associated thromboemboli is not as common as initially thought (Lancet 2020;396:320)
- Hepatobiliary: hepatic congestion, mild steatosis, patchy hepatic necrosis, Kupffer cell hyperplasia, increased number of lymphocyte predominant inflammatory cells in the portal tracts and sinusoids, endotheliitis
- Renal: varying degrees of acute tubular injury, lymphocytic tubule interstitial infiltration, fibrin or hyaline thrombi in blood vessel, glomerular capillary dilatation, lymphocytic endotheliitis (Kidney Int 2020;98:219)
- Gastrointestinal: epithelial damage, prominent endotheliitis, ischemic enterocolitis
- Spleen: reduced number of lymphocytes with necrosis, atrophy, congestion, hemorrhage, infarction
- Bone marrow: histiocytic hyperplasia, hemophagocytosis (Mod Pathol 2020;33:2139)
- Other: cutaneous, prostatic manifestations, inflammation and clots in placenta with funisitis
- Cardiovascular: mild pericardial edema, some serosanguinous pericardial effusion, mild myocardial edema, low grade interstitial infiltration of mononuclear cells, endotheliitis
Microscopic (histologic) images
Contributed by Toru Igari, M.D., Jin Takahashi, M.D. and Shinyu Izumi, M.D.
Images hosted on other servers:
Cytology description
- Bronchoalveolar lavage (BAL):
- Inflammatory background (lymphohistiocytic, histiocytic, neutrophil predominant), virus related changes (atypical nuclei, nuclear cytoplasmic inclusion, multinucleation), nonspecific reactive changes (bronchial, alveolar, reserve cell hyperplasia) (Acta Cytol 2022;66:532)
- Abundant activated plasma cells, as per a single case report (J Thorac Oncol 2020;15:e65)
- Alveolar macrophages may feature nuclear clearing or intranuclear cytopathic inclusions
- High neutrophil proportions in mechanically ventilated critically ill patients (Clin Respir J 2022;16:329)
Cytology images
Positive stains
- IHC positive for SARS-CoV-2 antigen detected in pneumocytes, ciliated airway cells and upper airway epithelium in the acute phase (Mod Pathol 2020;33:2104)
Electron microscopy description
- Spherical particles sized 60 - 140 nm
- Distinctive spikes on the surface (9 - 12 nm) giving virions the appearance of a solar corona, consistent with the Coronaviridae family
- Inclusion bodies filled with virus particles in membrane bound vesicles in cytoplasm of the respiratory epithelium (N Engl J Med 2020;382:727)
Electron microscopy images
Molecular / cytogenetics description
- ISH, including RISH and FISH positive for SARS-CoV-2 antigen detected in pneumocytes, ciliated airway cells and upper airway epithelium in the acute phase (Lab Invest 2020;100:1485, JCI Insight 2020;5:139042)
- Guidelines from CDC (CDC: Information for Laboratories [Accessed 20 March 2023])
- Diagnostic testing of SARS-CoV-2 (COVID-19)
Videos
Pathology of COVID-19: a pulmonary pathologist explains
Sample management
Autopsy
SARS-CoV-2 detection in tissues
Pulmonary pathology
Cardiovascular pathology
COVID-19 autopsy pathology findings
Histology of acute respiratory distress syndrome
Sample pathology report
- Usually reported as part of autopsy findings:
- Diffuse alveolar damage due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection
- Diffuse alveolar damage with changes compatible with viral infection
Differential diagnosis
- Diffuse alveolar damage due to COVID-19 is morphologically indistinguishable from other DAD causes, including other viral pneumonias:
- Severe acute respiratory syndrome:
- Detection of SARS virus
- Acute respiratory distress syndrome of other etiology
- Acute interstitial pneumonia:
- Idiopathic by definition
Additional references
- WHO: Coronavirus Disease (COVID-19) Pandemic [Accessed 20 March 2023], CDC: Coronavirus (COVID-19) [Accessed 20 March 2023]
- General biosafety guideline protocol for histological and cytological samples from patients with suspected or proven COVID-19 infection (Cancer Cytopathol 2020;128:317)
Board review style question #1
Board review style answer #1
Board review style question #2
Board review style answer #2
Board review style question #3
Which of the following findings suggests viral infection of the lung?
- Alveolar hemorrhage
- Fibrin deposition
- Neutrophilic aggregation
- Nuclear inclusions
- Type II pneumocyte hyperplasia
Board review style answer #3