Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology description | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sathirareuangchai S, Glass C. Coccidioides. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumorcoccidio.html. Accessed March 31st, 2025.
Definition / general
- Lung infection caused by dimorphic fungi, Coccidioides spp.
Essential features
- Highly prevalent in the endemic areas (southwest U.S., Central and South America)
- Lower respiratory tract symptoms resembling bacterial pneumonia; mass lesion with cavity formation in chronic infection
- Necrotizing granulomatous inflammation with characteristic spherules
Terminology
- Pulmonary coccidioidomycosis
- San Joaquin Valley fever, valley fever
ICD coding
Epidemiology
- Endemic areas
- Southwest U.S.: California, Arizona, New Mexico, Texas
- Central and South America: northern Mexico, Argentina, Brazil (Ann N Y Acad Sci 2007;1111:19)
- Men: higher incidence of symptomatic and severe infection (Clin Microbiol Rev 2013;26:505)
- African Americans: higher risk of disseminated disease (Clin Microbiol Rev 2013;26:505)
Sites
- Primary lung infection
- Common extrathoracic sites: skin, joints, bones and meninges (Clin Microbiol Rev 2013;26:505)
Pathophysiology
- Acquired via inhalation of aerosolized arthroconidia (3 - 5 microns) from the soil
- A specialized structure called a spherule forms in the lung
- Endospores are released from the ruptured spherule and develop into new spherules
- Disseminate via hematogenous route
Etiology
- Dimorphic fungi in the genus Coccidioides, which contain 2 species
- Coccidioides immitis (central and southern California, San Joaquin Valley)
- Coccidioides posadasii (isolated outside California)
- No difference in clinical course and microscopic morphology between the 2 species
Clinical features
- Most infected individuals are asymptomatic or minimally symptomatic
- Symptoms include cough, fever, dyspnea, pleuritic chest pain
- Can be disseminated in 1 - 5% of cases, especially immunocompromised patients (Medicine (Baltimore) 2004;83:149)
- Desert rheumatism refers to the immunologic phenomena triad, including fever, arthralgia and erythema nodosum
Diagnosis
- Traveling history or residence in the endemic areas
- Fungal organism identification by histology, culture or serology
Laboratory
- Standard fungal culture: no specific plate morphology; lactophenol cotton blue stains shows septate hyphae with alternating barrel shaped arthroconidia
- Biosafety level 3 pathogen: laboratory personnel should be aware of the diagnosis
- Serologic testing for anticoccidioidal IgG, IgM
- Increased serum (1→3)-β-D-glucan can be used to indicate invasive fungal disease, although not specific for coccidioidomycosis (J Clin Microbiol 2012;50:3060)
- Complete blood count: eosinophilia found in 27% of cases (West J Med 1993;159:153)
Radiology description
- Chest Xray and CT chest in acute infection: nonspecific, resembling acute bacterial pneumonia, including consolidation (75%), nodular opacities (20%), hilar adenopathy (20%), pleural effusion (15 - 20%); solitary pulmonary nodule may be seen (Radiographics 2014;34:912)
- Disseminated infection: miliary nodules from hematogenous spread (Radiographics 2014;34:912)
- Chronic cavitary lesion can be seen radiographically in 2% of cases, up to 11% by CT scan (Radiographics 2014;34:912)
- Grape skin sign: classic finding in chronic pulmonary coccidioidomycosis (AJR Am J Roentgenol 2014;202:479)
- Very thin walled cavitary lesion that develops in lung parenchyma previously affected by consolidation followed by central necrosis
Case reports
- 34 year old man with left upper lobe pneumonia and cutaneous nodule (Am J Trop Med Hyg 2019;100:5)
- 42 year old man with cavitary lesion and fungal ball (Lab Med 2020;51:e12)
- 49 year old man with left upper lobe cavitary lesion (Hum Pathol 2018;71:55)
- 64 year old man with fever and respiratory failure (N Engl J Med 2020;382:276)
Treatment
- Oral azole antifungal
- Amphotericin B
- Surgical resection of the cavitary lesion if (Clin Infect Dis 2016;63:e112)
- Cavities are persistently symptomatic despite antifungal treatment
- Cavities have been present for more than 2 years and if symptoms recur whenever antifungal treatment is stopped
Gross description
- Mass lesion can be seen in chronic infection, usually well demarcated, often with central cavitation
- Fungus ball (mycetoma) was found in 28% of cases with cavity lesion (Hum Pathol 2014;45:153)
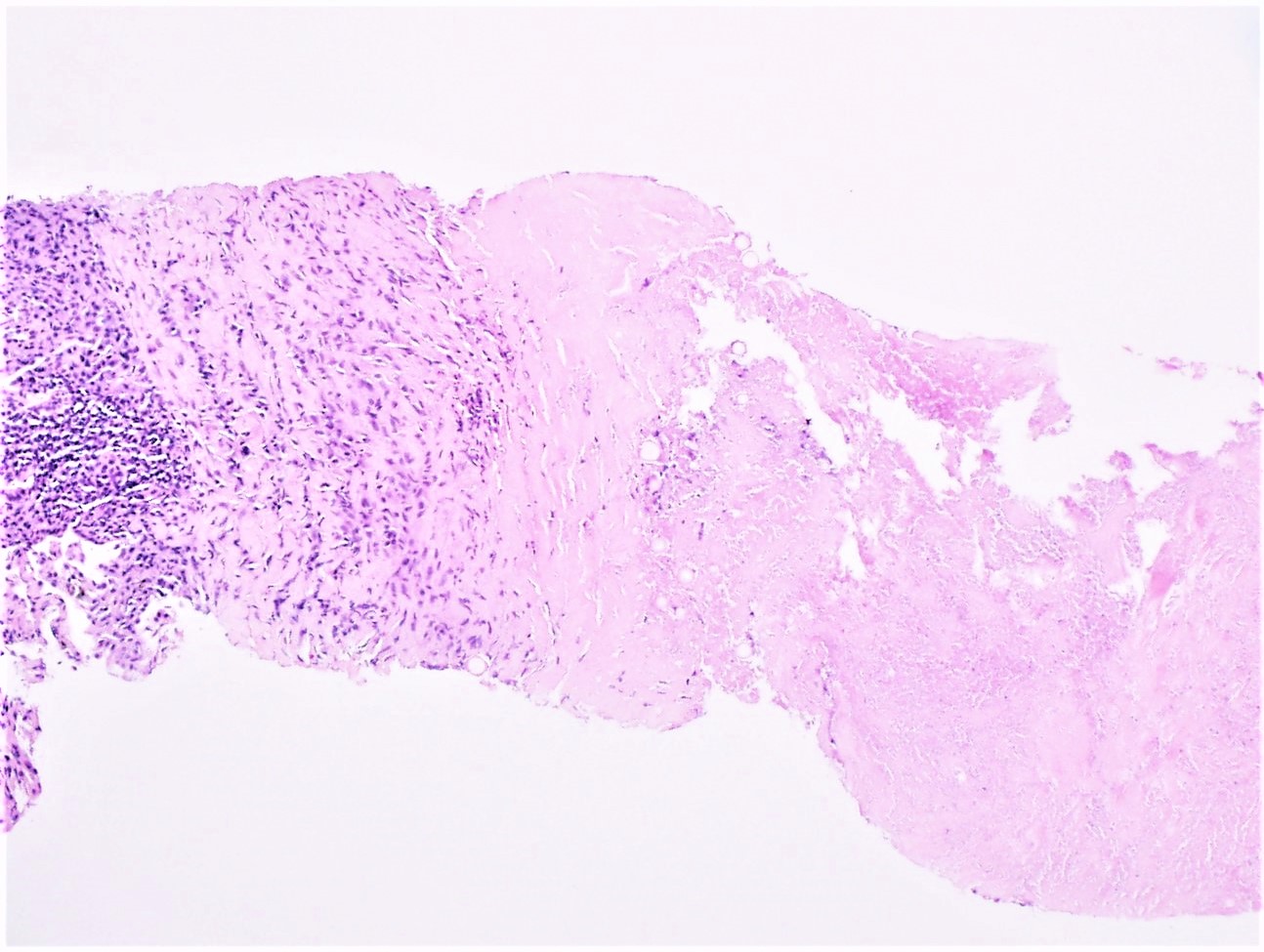
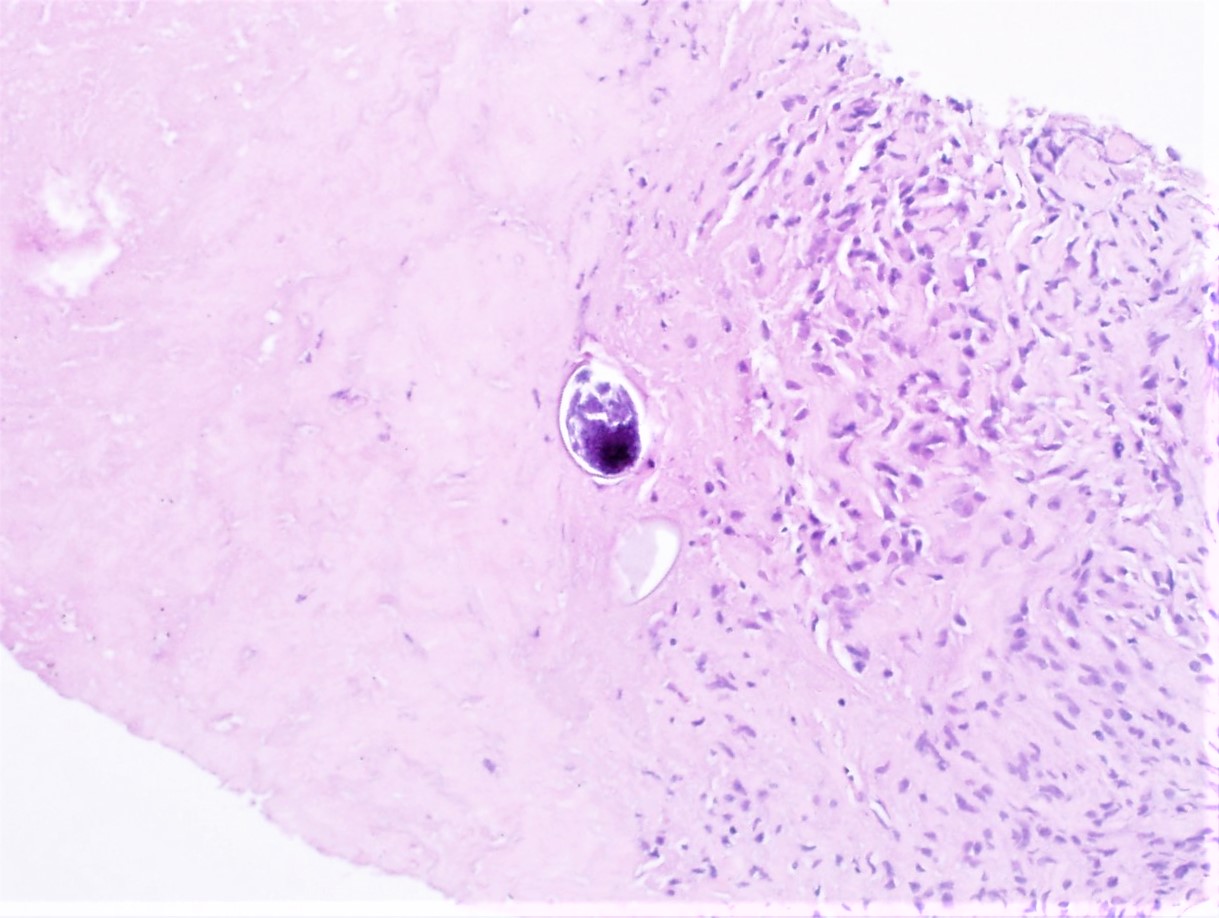
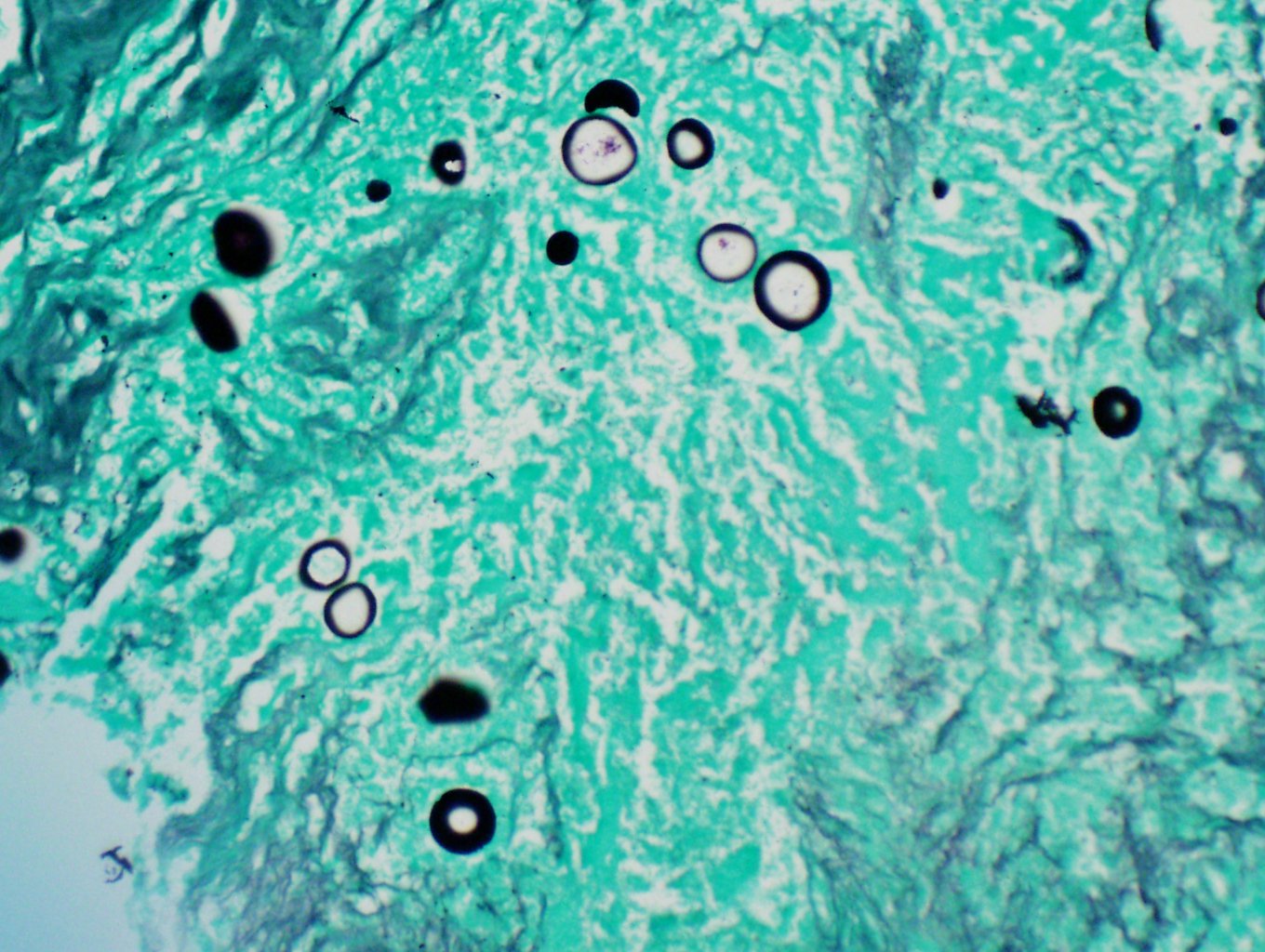
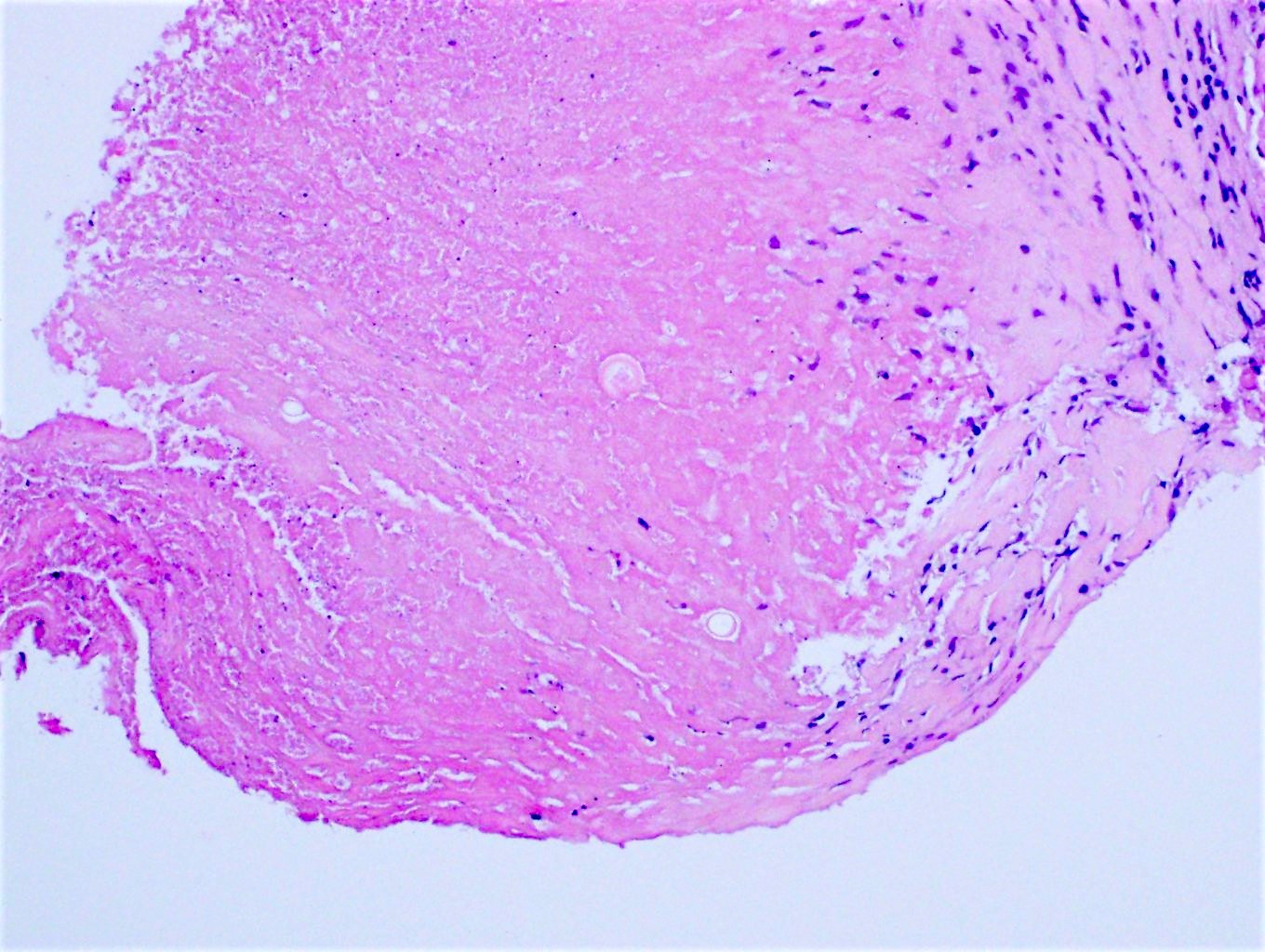
Microscopic (histologic) description
- Necrotizing, often suppurative, granulomatous inflammation
- Large (20 - 200 microns) thick walled spherules, with or without granular basophilic endospores (2 - 4 microns)
- Eosinophilic infiltrate is common
- Thin, septate hyphae with arthroconidia formation may be seen, more often in diabetes mellitus patients (Eur J Clin Microbiol Infect Dis 2008;27:813)
- Cavitary lesion features (Hum Pathol 2014;45:153)
- Palisading fibroblasts and fibrosis with chronic inflammation
- Granuloma not seen in the cavity wall, while multinucleated giant cells occasionally present
- Squamous metaplasia in the lining of the cavity wall
- Hyphal forms identified in 62% of cases
- Blood vessel lesion: arteritis with fibrinoid necrosis and rupture, thrombus and mural chronic inflammation
- Surrounding lung parenchyma (Hum Pathol 2014;45:153)
- Lymphoid hyperplasia
- Chronic bronchiolitis
- Organizing pneumonia
Microscopic (histologic) images
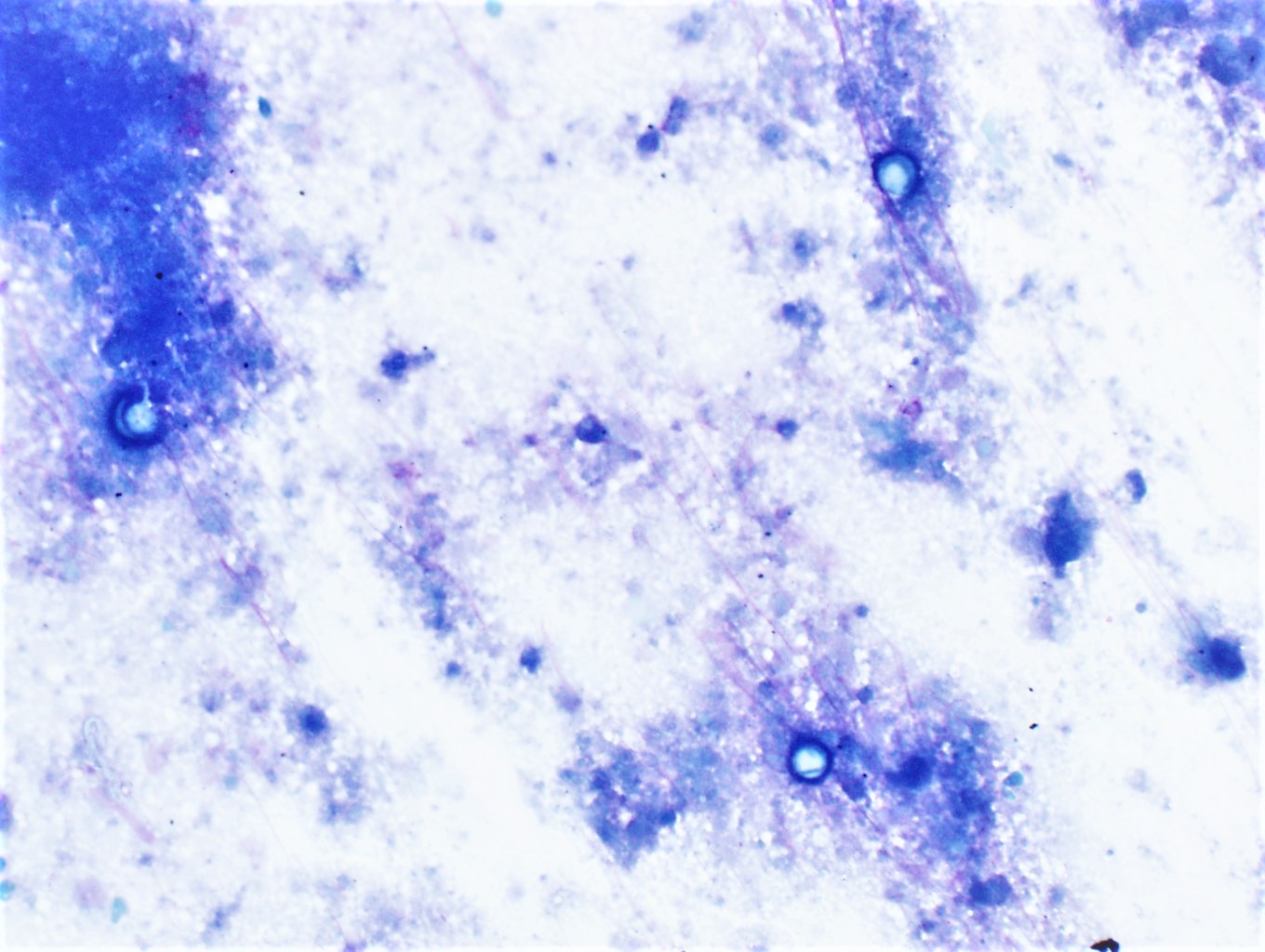
Cytology description
- Bronchoalveolar lavage (BAL) cytology (Diagn Cytopathol 2016;44:195)
- Various forms of spherules with associated acute inflammatory response
- Spherules can be immature (not adsorb any stains), smaller, larger, empty or fractured
- Granulomas were rare and mostly seen in lymph nodes and extra pulmonary sites (Diagn Cytopathol 2016;44:195)
- Mycelial form in BAL is uncommon but has been reported (Diagn Cytopathol 2007;35:535)
Negative stains
Molecular / cytogenetics description
- Real time PCR assay is available for various types of specimen (e.g., bronchoalveolar lavage, sputum, lung tissue, etc.)
- In situ hybridization for C. immitis ribosomal RNA has been described (Diagn Mol Pathol 2010;19:99)
Videos
Dimorphic fungi: coccidioidomycosis by Glenn D. Roberts, Ph.D.
Sample pathology report
- Left lung, core needle biopsy:
- Necrotizing granulomatous inflammation (see comment)
- Comment: Fungal organism identified on H&E and GMS stain, consistent with Coccidioides spp.
Differential diagnosis
- Histoplasmosis:
- Endemic in the central and eastern U.S. (Ohio and Mississippi River valleys)
- Small (2 - 5 microns) budding yeast within the histiocytes
- Blastomycosis:
- Endemic in the eastern U.S. (Ohio, Mississippi River valleys, Great Lakes region)
- Broad based budding yeast, smaller (8 - 15 microns) than Coccidioides sp.
- Paracoccidioidomycosis:
- Endemic in South America
- Large (10 - 60 microns) spherical yeast with circumferential budding, resembling mariner’s wheel
- Cryptococcosis:
- No specific endemic area
- Round, medium sized (4 - 7 microns), yeast with thick mucoid capsule
- Tuberculosis:
- Acid fast positive bacilli
Additional references
Board review style question #1
A 40 year old man presents with chronic cough, low grade fever and mild dyspnea for several months. CT scan of the chest shows a 3 cm mass lesion in the right upper lobe of the lung. The H&E image of the core needle biopsy is shown. Which one of the followings is the most likely exposure history?
- Cave diving in Ohio
- Military training in Arizona
- Parakeet breeder
- Traveling to Africa
- Camping in Colorado
Board review style answer #1
B. Military training in Arizona. The patient has coccidiomycosis.
Comment Here
Reference: Coccidioides immitis
Comment Here
Reference: Coccidioides immitis
Board review style question #2
What is the pathognomonic microscopic feature of coccidioidomycosis in a histologic section?
- Broad based budding yeast
- Round yeast with large mucoid capsule
- Acute angle, branching septate hyphae
- Large spherule with numerous endospores
- Oval yeast with pseudohyphae budding
Board review style answer #2