Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Evason KJ. Intraductal papillary neoplasm of the bile ducts. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livertumorintraductalpap.html. Accessed March 29th, 2025.
Definition / general
- Papillary neoplasm consisting of fibrovascular stalks within cystically dilated intrahepatic bile ducts
Essential features
- Papillary neoplasm within dilated intrahepatic bile duct(s)
- Lacks ovarian stroma
- High rate of associated invasive carcinoma (up to 74%) (Hepatology 2012;56:1352)
- WHO classification
- Premalignant: intraductal papillary neoplasm with low grade, intermediate grade or high grade intraepithelial neoplasia
- Malignant: intraductal papillary neoplasm with associated invasive carcinoma
Terminology
- Biliary papillomatosis
- Biliary papilloma
ICD coding
- ICD-O:
- ICD-11: 2E92.7 - benign neoplasm of liver or intrahepatic bile ducts
Epidemiology
- M > F; age: 50 - 70 years (Proc Bayl Univ Med Cent 2019;32:124)
- Most common in Far East (Taiwan, Japan, Korea) (World J Gastroenterol 2013;19:8595)
Sites
- Intrahepatic bile ducts
- Similar lesions can involve extrahepatic bile ducts, pancreas or gallbladder
- Often multifocal
Pathophysiology
- Stepwise progression from low grade dysplasia to high grade dysplasia to invasive carcinoma involving inactivation of TP53 and p16 (early), activating mutations in KRAS (early) and loss of SMAD4 / DPC4 (late) (Mod Pathol 2014;27:73)
Etiology
- May be related to hepatolithiasis and clonorchiasis (liver fluke infection) (Proc Bayl Univ Med Cent 2019;32:124)
Clinical features
- Symptoms resulting from biliary obstruction: jaundice, abdominal pain
Diagnosis
- Imaging (CT, MRI, ultrasound)
- Surgical resection: extensive histologic sampling required to exclude invasive component
Laboratory
- May have elevated bilirubin and alkaline phosphatase due to biliary obstruction
Radiology description
- Bile duct dilatation and intraductal masses can be seen on ultrasound, CT or MRI (Proc Bayl Univ Med Cent 2019;32:124)
Prognostic factors
- Presence of an invasive component is associated with shorter survival, related to depth and percentage of invasion (Mod Pathol 2014;27:73, World J Gastroenterol 2015;21:12498, Hepatology 2012;56:1352)
- Multiple / widespread lesions are difficult to treat and have a poorer prognosis
Case reports
- 38 year old woman with 1 week of acholic stools, jaundice, pruritus and dark colored urine (World J Gastroenterol 2015;21:12498)
- 58 year old man with mild prominence of the left hepatic biliary duct on MRI (Proc Bayl Univ Med Cent 2019;32:124)
- 59 year old woman with multiple episodes of abdominal pain and fever (Endosc Ultrasound 2016;5:274)
- 61 year old Asian man presented with severe right upper quadrant pain (BMJ Case Rep 2017;2017:bcr2016218139)
- 72 year old previously healthy man with right upper abdominal pain (Int J Surg Case Rep 2018;51:102)
Treatment
- Surgical resection is first line treatment
- Palliative approaches include chemotherapy and laser ablation
Gross description
- Soft, friable, villiform mass(es)
- May be pedunculated, sessile or polypoid
Microscopic (histologic) description
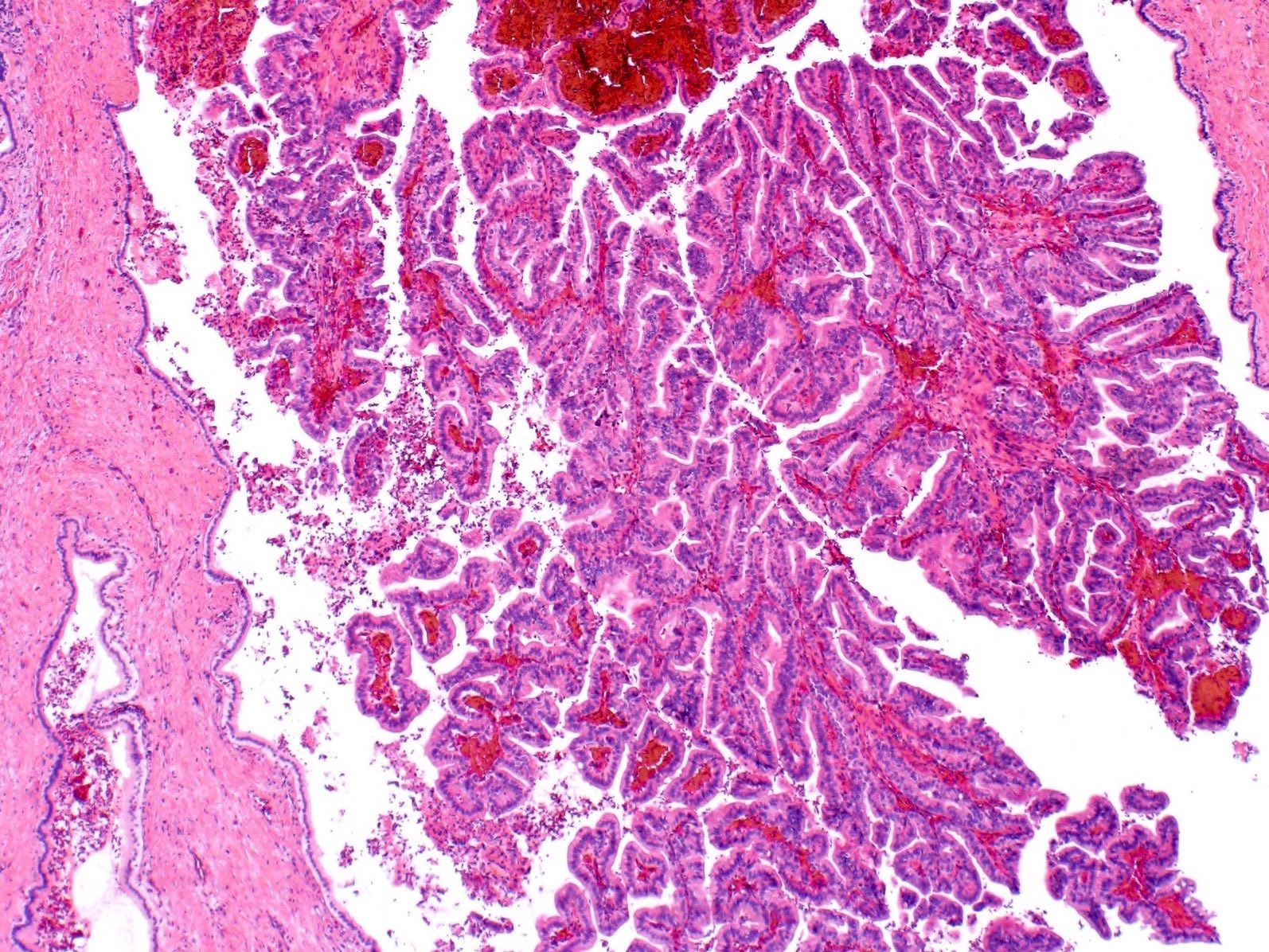
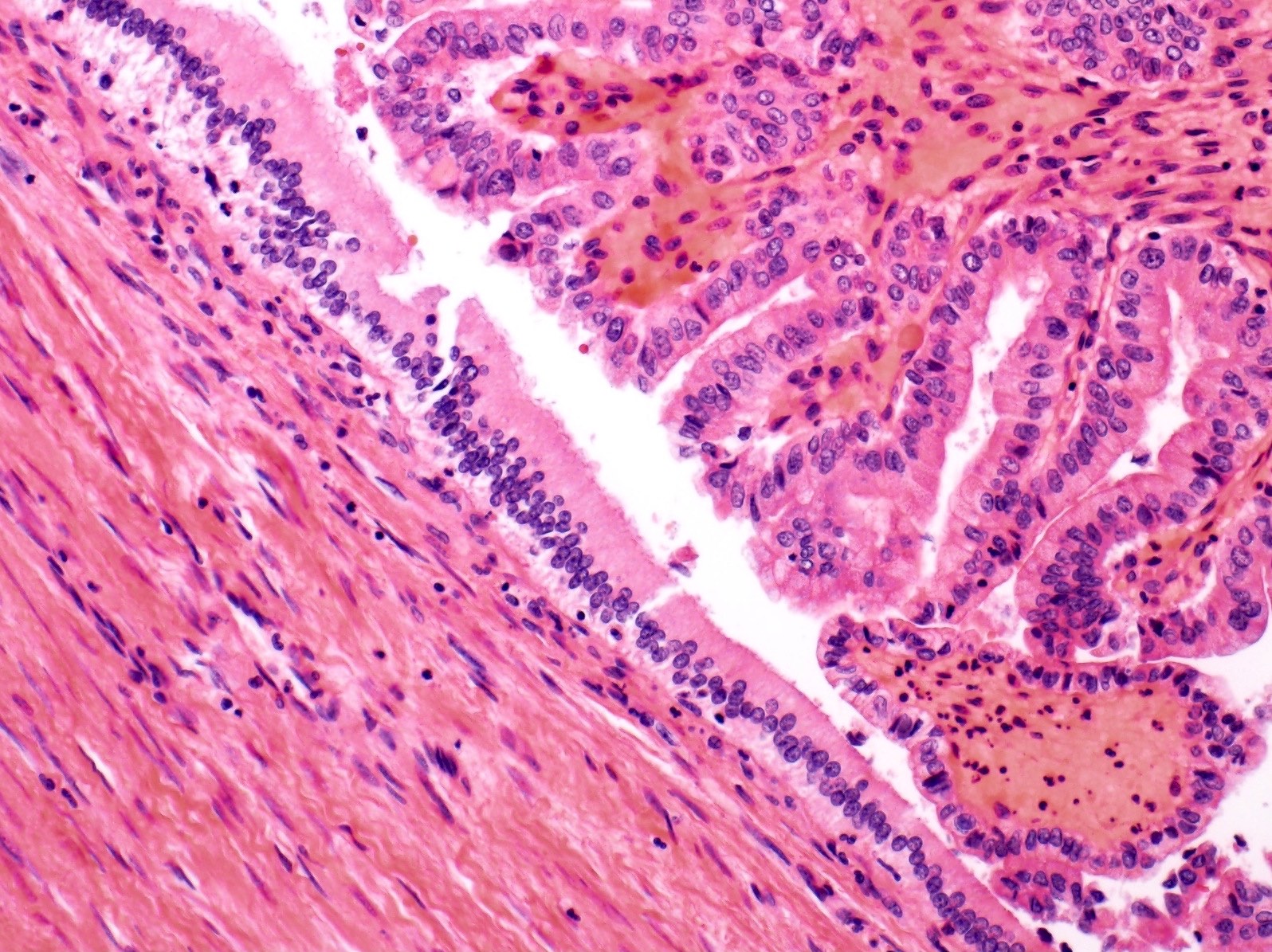
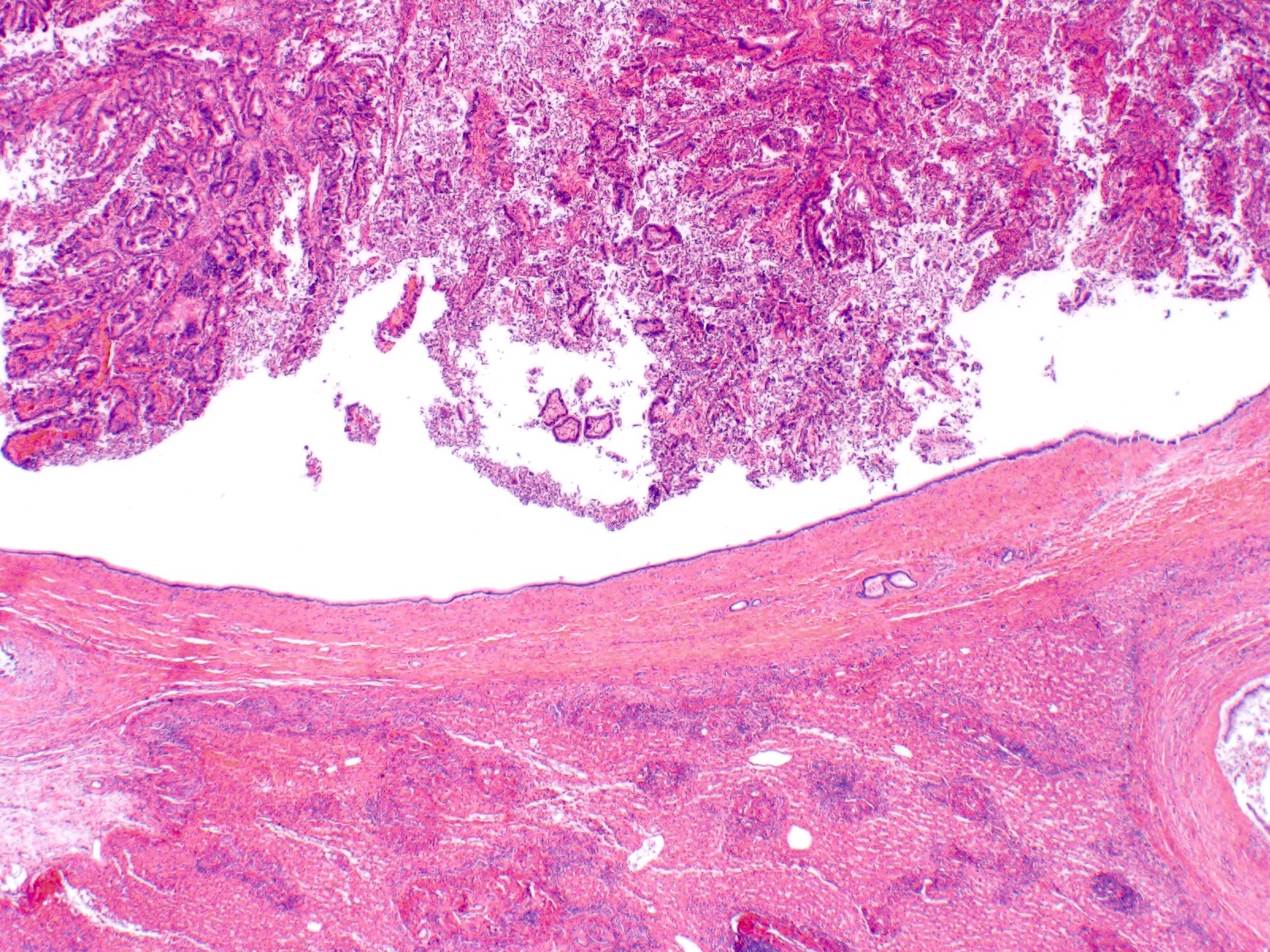
- Papillary neoplasm with complex tubulovillous or micropapillary architecture
- Grows within dilated bile ducts
- Lacks ovarian stroma
- May form large, multilocular cysts with thin fibrous septations
- Epithelium may be pancreaticobiliary (most common in European and North American patients), intestinal (more common in Asian patients), gastric (more common in Asian patients) or oncocytic
- Can be classified into type 1 (pancreatic type) and type 2 (nonpancreatic type) intraductal papillary neoplasms of the bile ducts (IPNBs) (Histol Histopathol 2017;32:1001, J Hepatobiliary Pancreat Sci 2018;25:181)
- Type 1 is similar to intraductal papillary mucinous neoplasms (IPMNs) of the pancreas
- Type 1 is more frequently intrahepatic or hilar, while type 2 is more frequently extrahepatic
- Type 2 is more aggressive, with more frequent associated invasive carcinoma
- Reference: Am J Gastroenterol 2012;107:118
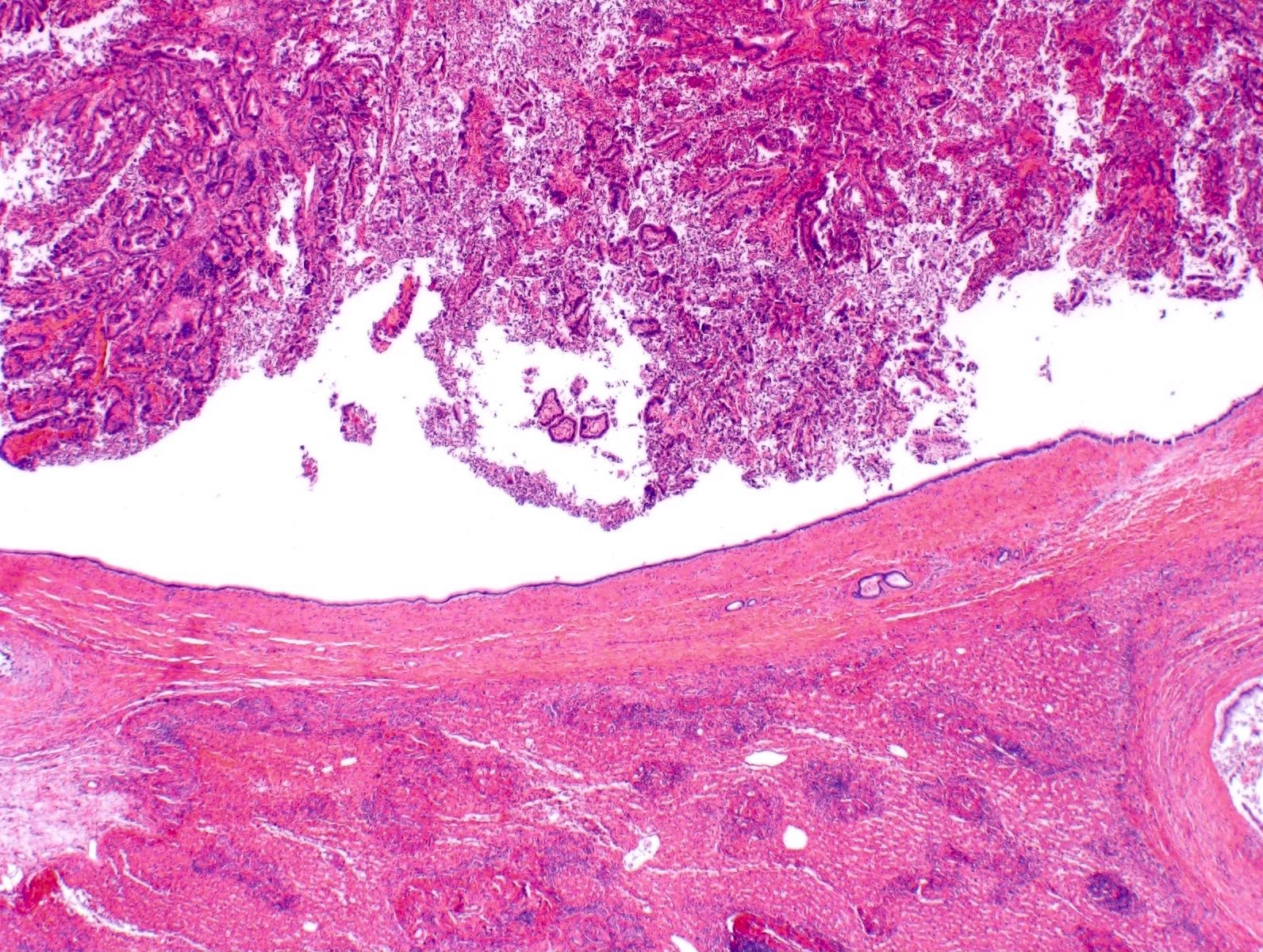
Microscopic (histologic) images
Cytology description
- Hypercellular, with broad and double layered sheets of columnar epithelial cells, fine stroma and complex, 3 dimensional branching papillary configurations
Positive stains
- Various mucins, depending on differentiation (Semin Diagn Pathol 2017;34:167)
- MUC5AC and MUC6: gastric type epithelium
- MUC2: intestinal type epithelium
- MUC1 (EMA): pancreatobiliary type epithelium
Negative stains
- ER / PR staining is negative in stroma cells (unlike mucinous cystic neoplasm)
- SMAD4 / DPC4 staining may be lost in invasive component
Sample pathology report
- Liver, left lobe, lobectomy:
- Intraductal papillary neoplasm with low and high grade dysplasia, involving left hepatic duct
- No invasive carcinoma
Differential diagnosis
- Mucinous cystic neoplasm:
- Also is a cystic hepatic lesion that may be lined by biliary type epithelium
- Has ovarian type stroma and does not communicate with biliary lumen
- Cholangiocarcinoma:
- May show areas of cystic degeneration
- Does not communicate with biliary lumen (Pathol Int 2005;55:206)
- Metastatic carcinoma, especially metastatic colorectal adenocarcinoma:
- May show areas of cystic degeneration
- Does not communicate with biliary lumen
- Biliary intraepithelial neoplasia (BilIN):
- Also is located within lumen of large intrahepatic bile ducts
- Typically is < 3 mm in height (not mass forming)
- Simple cyst, simple hepatic cyst, simple biliary cyst, bile duct cyst:
- Lacks papillary projections
- Intraductal tubulopapillary neoplasm of the bile duct (Mod Pathol 2015;28:1249):
- Predominantly comprised of densely packed, nonmucinous tubules
- < 30% papillary growth pattern
Additional references
Board review style question #1
A 72 year old man presented with jaundice. CT scan showed dilatation of the left bile duct, which contained a papillary lesion. An image from the resection specimen is shown. Which of the following is true about this entity?
- It is almost always unifocal
- It lacks ovarian type stroma
- The epithelium is most commonly oncocytic
- There is a strong male predominance
- There is a very low risk of associated invasive carcinoma
Board review style answer #1
B. It lacks type ovarian stroma. This is an intraductal papillary neoplasm, which has a relatively high risk of associated invasive carcinoma (up to 74%). Sex preponderance varies by geographic region but the lesion is more common in men than women in Western countries. The epithelium is most commonly pancreatobiliary in European and North American patients. Intestinal and gastric epithelium are common in Asian patients. Oncocytic epithelium is relatively uncommon. The differential diagnosis of cystic hepatic lesions includes mucinous cystic neoplasms, which do have ovarian type stroma.
Comment Here
Reference: Intraductal papillary neoplasm of the bile ducts
Comment Here
Reference: Intraductal papillary neoplasm of the bile ducts
Board review style question #2
Intraductal papillary neoplasms of the bile ducts in North American and European patients most often have which type of epithelium?
- Gastric
- Intestinal
- Oncocytic
- Ovarian
- Pancreaticobiliary
Board review style answer #2
E. Pancreaticobiliary. Intraductal papillary neoplasms of the bile ducts are most commonly lined by pancreatobiliary epithelium in North American and European patients. Intestinal and gastric epithelium are common in Asian patients. Oncocytic epithelium is relatively uncommon. Ovarian type stroma is associated with mucinous cystic neoplasms, a different type of cystic hepatic lesion.
Comment Here
Reference: Intraductal papillary neoplasm of the bile ducts
Comment Here
Reference: Intraductal papillary neoplasm of the bile ducts