Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Guedj N, Beaufrère A. Combined hepatocellular carcinoma-cholangiocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livertumorcombinedHCCcholangio.html. Accessed April 2nd, 2025.
Definition / general
- Combined hepatocellular carcinoma-cholangiocarcinoma (cHCC-CC) is a rare primary liver malignancy
- cHCC-CC exhibits, unequivocally, both hepatocytic and biliary differentiation within the same tumor; collision tumors are excluded
- Primary liver tumor composed of homogenous biphenotypic tumor cells, called intermediate cell carcinoma, is considered a subtype of cHCC-CC
- Cholangiolocellular carcinoma (CLC) is now included in the cholangiocarcinoma classification in the 2019 WHO classification (5th edition); a tumor that exhibits a CLC component associated with a hepatocellular carcinoma component can be classified as cHCC-CC
- Diagnosis of cHCC-CC should be based on routine histopathology with hematoxilin and eosin; immunohistochemistry is used as a supplemental diagnostic tool
- Reference: J Hepatol 2021 Feb 2 [Epub ahead of print]
Essential features
- cHCC-CC is a specific entity within primary liver malignancies
- cHCC-CC is a primary liver carcinoma with unequivocal presence of both hepatocytic and cholangiocytic differentiation
- Diagnosis is based on H&E morphology
- Expression of immunohistochemical markers alone is not sufficient for diagnosis
Terminology
- These terms should no longer be used:
- Mixed HCC-CCA
- Mixed hepatobiliary carcinoma
- Hepatocholangiocarcinoma
- HCC-CC with stem cell features
ICD coding
Epidemiology
- < 1% of liver primary malignancies (Liver Transpl 2014;20:952)
Sites
- cHCC-CC has an intrahepatic localization
Pathophysiology
- 3 different hypotheses have been postulated for the development of cHCC-CC (J Hepatol 2021 Feb 2 [Epub ahead of print]):
- Incidental coexistence of hepatocellular carcinoma (HCC) and intrahepatic cholangiocarcinoma (ICC) within the same tumor
- Malignant transformation of a hepatic progenitor cell
- Dedifferentiation of an HCC or ICC
Etiology
- Classical risk factors of hepatocellular carcinoma or intrahepatic cholangiocarcinoma also seem to predispose towards the development of cHCC-CC (Chin Clin Oncol 2016;5:66)
- Viral hepatitis
- Alcohol intake
- Nonalcoholic steatohepatitis
- Likelihood of liver cirrhosis in patients with cHCC-CC has been reported to be intermediate between the high proportion seen in patients with hepatocellular carcinoma and the lower prevalence in patients with intrahepatic cholangiocarcinoma
- Due to the rarity of the disease, the existence of specific risk factors to the development of cHCC-CC remains unknown
Clinical features
- cHCC-CC is predominantly observed in male patients
- No specific clinical symptoms; fatigue, obstructive jaundice, weight loss or abdominal discomfort may occur
- Reference: BMC Cancer 2016;16:158
Diagnosis
- Preoperative diagnosis of cHCC-CC is very complex since there are no specific noninvasive imaging features; however, the existence of overlapping features between hepatocellular carcinoma and intrahepatic cholangiocarcinoma is highly suggestive
- Gold standard diagnosis is based on histologic analysis of resected specimens after extensive tumor sampling (Hepatobiliary Pancreat Dis Int 2020;19:515)
Laboratory
- Alpha fetoprotein > 400ng/ml in 21.1% of cHCC-CC cases
- CA19-9 > hepatocellular carcinoma but < intrahepatic cholangiocarcinoma
- CEA elevated in 25% of cHCC-CC patients
- Reference: Hepatobiliary Pancreat Dis Int 2020;19:515
Radiology description
- Imaging features of cHCC-CC are heterogeneous and overlap with those of hepatocellular carcinoma and intrahepatic cholangiocarcinoma
- Amount of each component seems to be a key determinant of cHCC-CC radiological features
- If hepatocellular carcinoma predominates, an intense contrast uptake during the arterial phase with a washout in the venous phase is observed on CT
- If intrahepatic cholangiocarcinoma predominates, progressive centripetal enhancement, capsule retraction or peripheral rim enhancement is observed on CT
- Reference: Liver Int 2019;39:2386
Radiology images
Prognostic factors
- Main unfavorable prognostic factors are (J Gastroenterol Hepatol 2019;34:1074):
- Large tumor size (> 5 cm)
- Presence of satellite nodules
- Lymph node metastasis
- Vascular invasion
- Portal vein invasion
- High tumor stage
- Free surgical margin < 2 cm
- Prognosis is worse than hepatocellular carcinoma and similar to that of intrahepatic cholangiocarcinoma
- Recurrence rate after surgery is high (up to 80% at 5 years)
Case reports
- 27 year old Caucasian woman with a past medical history of imperforate anus, tetralogy of Fallot and Abernethy malformation (Hepatology 2016;64:1800)
- 31 year old Caucasian woman with persistent right sided rib pain (Gastrointest Cancer Res 2012;5:199)
- 51 year old man, HBV carrier, found to have high alpha fetoprotein (Int J Clin Exp Pathol 2013;6:737)
- 54 year old Japanese woman with abdominal distension (Pathol Res Pract 2020;216:152908)
- 68 year old man who presented with fluctuant fever, chills and sweating (Cell Biochem Biophys 2014;69:1)
Treatment
- Management of cHCC-CC is not standardized
- Surgical resection with lymph node dissection is the only curative option (Ann Surg Oncol 2009;16:623)
- Liver transplantation is contraindicated (Dig Liver Dis 2017;49:467)
- Locoregional therapies (arterial chemoembolization, radiofrequency) and systemic chemotherapy have been proposed for nonoperated patients
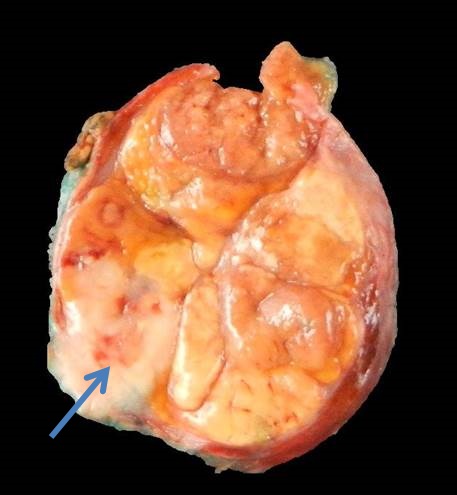
Gross description
- Lobular and firm mass
- Yellowish white pattern
- Well demarcated without capsule
- Reference: J Hepatol 2021 Feb 2 [Epub ahead of print]
Gross images
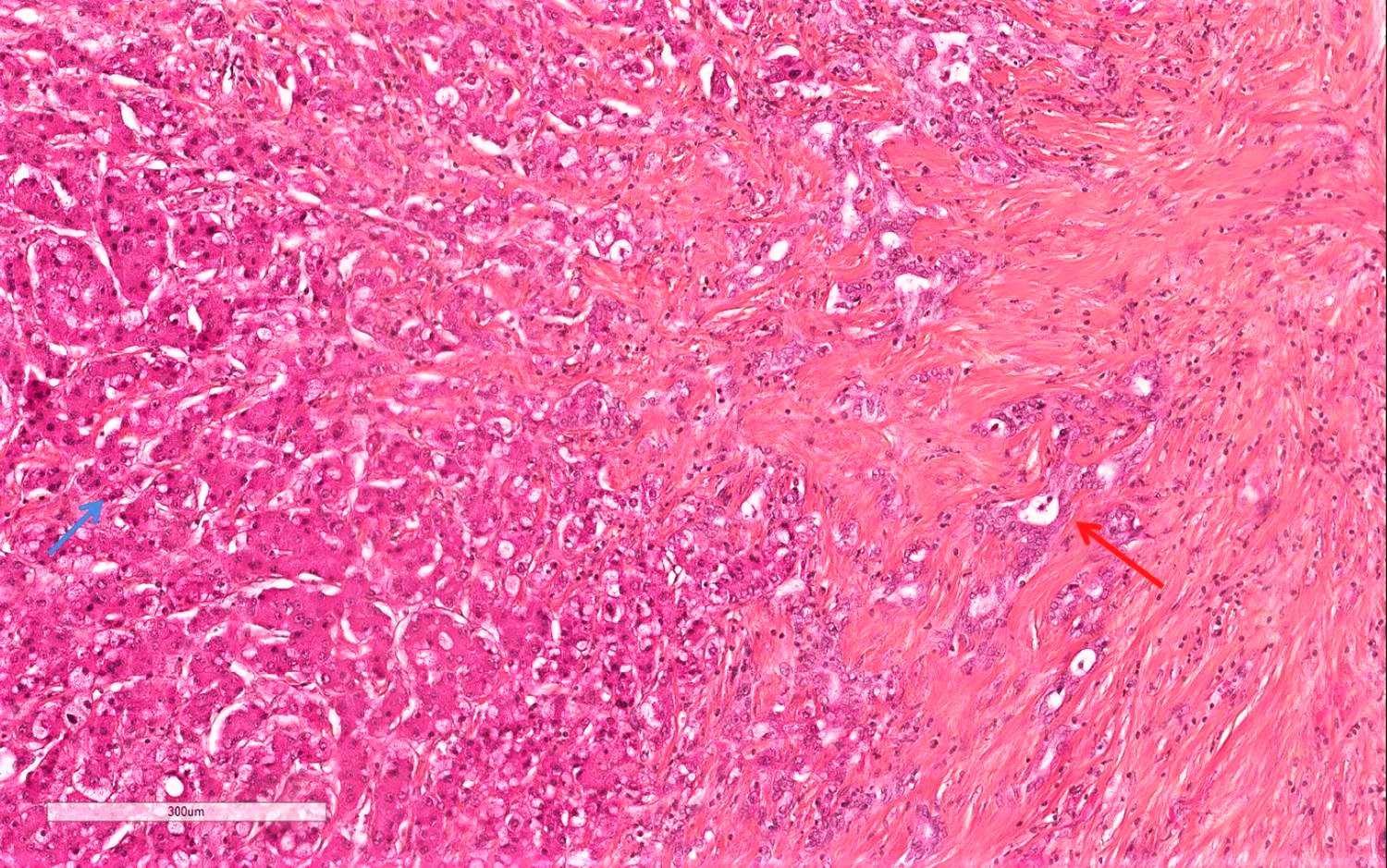
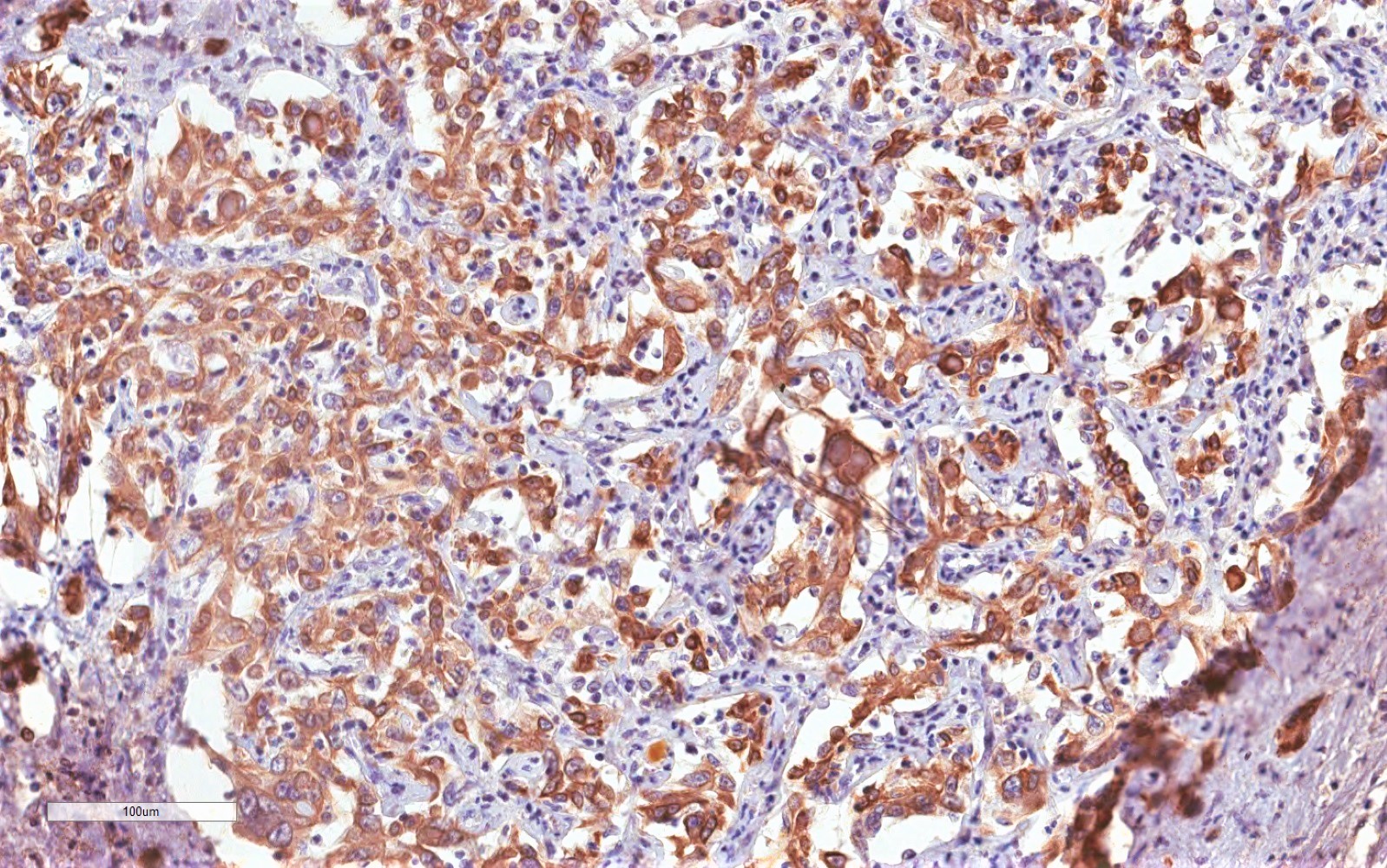
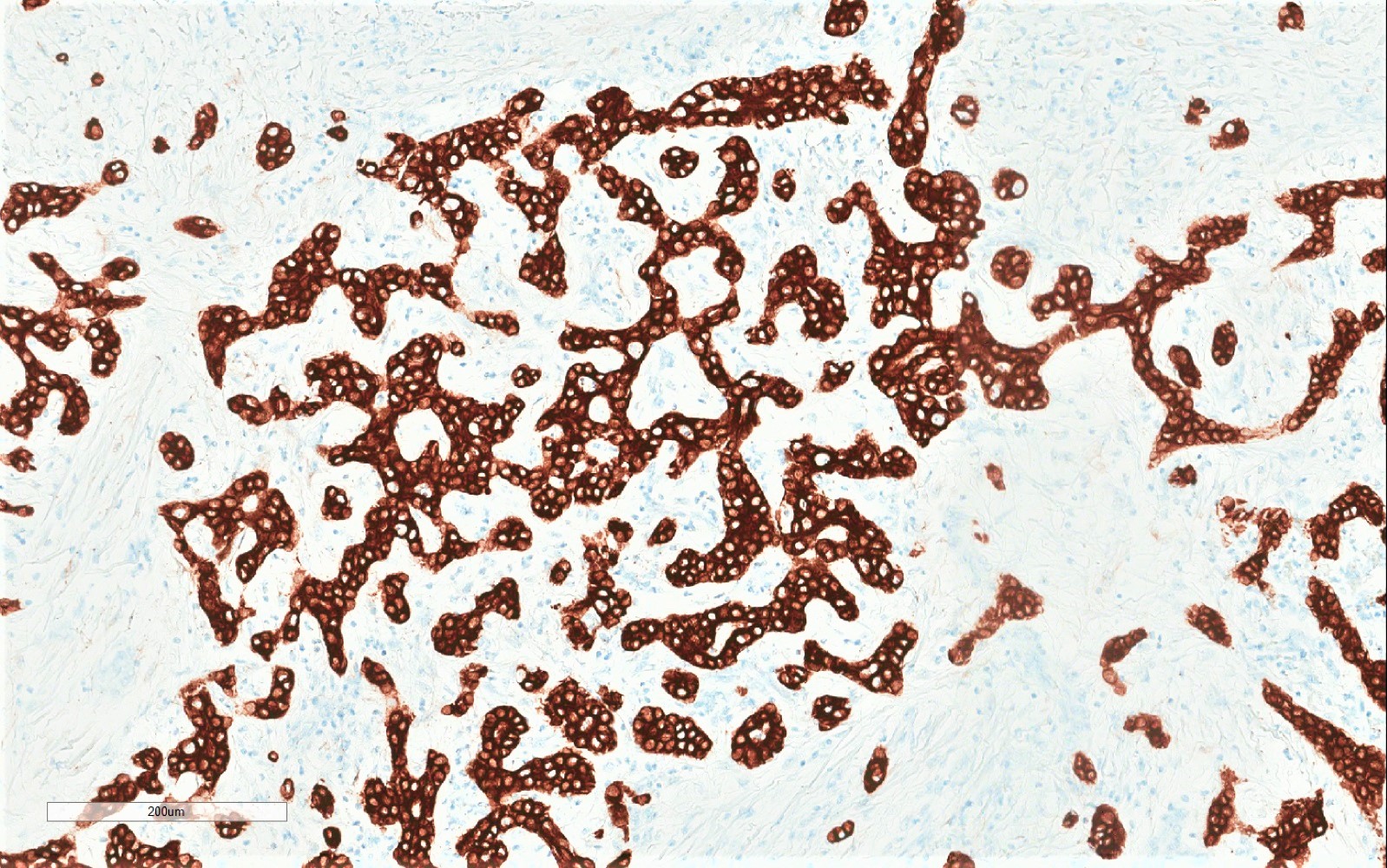
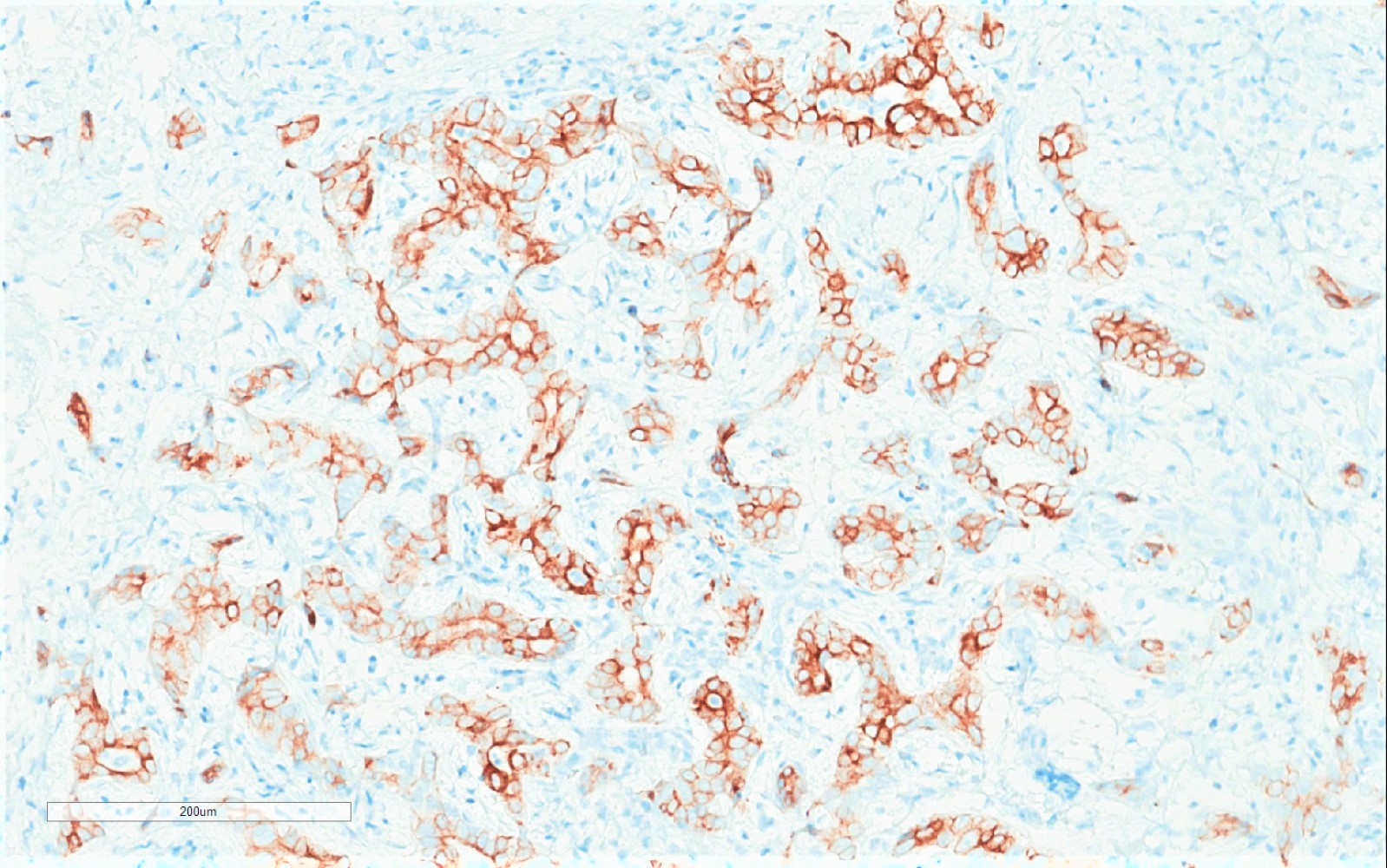
Microscopic (histologic) description
- Classical cHCC-CC contains areas of both typical hepatocellular carcinoma and typical intrahepatic cholangiocarcinoma, the former having any / all of the possible cytological and architectural features of hepatocellular carcinoma and the latter distinctly an adenocarcinoma with malignant glands, usually lying within a dense stromal background
- The components may be intermixed or lie in separate regions of a tumor, although focal areas of merging can often be discerned
- There are no published consensus guidelines for minimum amounts of hepatocellular carcinoma or intrahepatic cholangiocarcinoma to qualify for the diagnosis
- Intermediate cell carcinoma is composed of a monomorphic tumor with tumor cells smaller than normal hepatocytes but larger than the above described stem progenitor cell phenotype
- They have intermediate features between hepatocytes and cholangiocytes
- Tumor cells may be cuboidal to oval shaped, with pale or pink cytoplasm
- Tumor cells may be arranged in trabeculae or cords, solid nests or strands and set within a background of marked desmoplastic or acellular hyalinized stroma
- Elongated, ill defined gland-like structures may be present, suggestive of tubules but well defined glands are not observed
- Tumor cell atypia and mitoses are uncommon
- Mucin production is absent
- It is a biphenotypic tumor on immunohistochemistry
- Cholangiolocellular carcinoma (CLC) can be part of cHCC-CC if a hepatocellular carcinoma component is present; alone, CLC is now considered a subtype of intrahepatic cholangiocarcinoma
- CLC closely resembles the epithelial component of ductular reaction
- CLC consists of thin, malignant ductular-like structures that may appear to radiate from or surround a portal tract in a tubular, cord-like, anastomosing pattern (antler-like pattern) within dense, hyalinized stroma
- Tumor may show trabecular and replacing growth at its interface with the surrounding nontumorous liver
- CLC is mucin negative
- Reference: Hum Pathol 2020;96:48
Microscopic (histologic) images
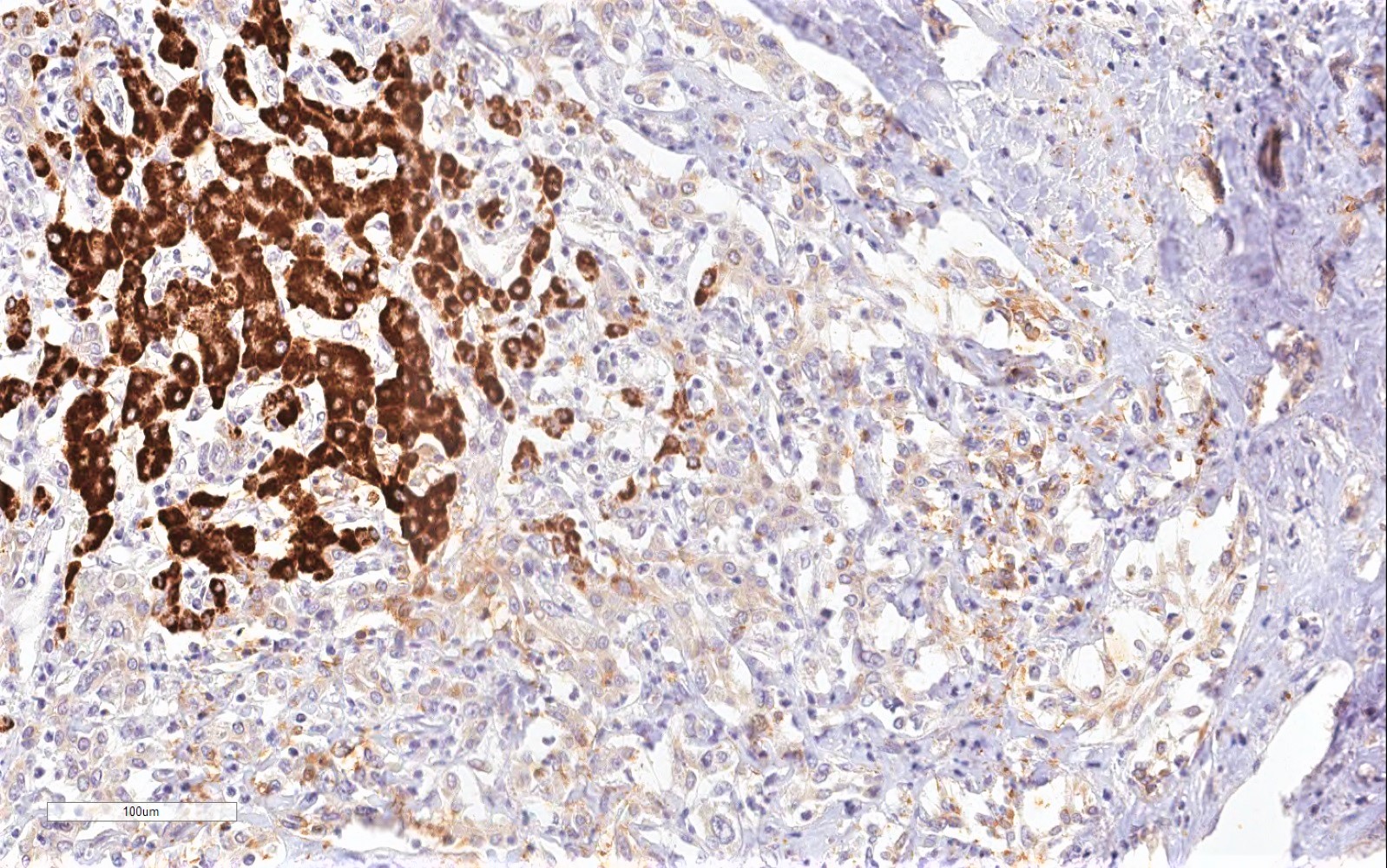
Positive stains
- Hepatocellular carcinoma component: HepPar1 (75 - 85%), arginase1 (85 - 95%), glypican 3 (50 - 80%), pCEA canalicular staining (50 - 80%), CD10 canalicular staining (50 - 75%)
- pCEA and CD10 are the most specific markers for confirming a hepatocellular carcinoma
- Intrahepatic cholangiocarcinoma component: CK7 (> 90%), CK19 (> 75%), EpCAM (> 90%)
- Reference: Hum Pathol 2020;96:48
Negative stains
- Hepatocellular carcinoma component: Alpha fetoprotein (AFP) (30%), CK7 (20 - 30%), CK19 (10 - 15%), EpCAM (10 - 20%)
- Intrahepatic cholangiocarcinoma component: HepPar1, arginase1, pCEA, CD10, AFP, glypican 3 (5%)
- Reference: Hum Pathol 2020;96:48
Molecular / cytogenetics description
- Most frequently mutated driver genes in cHCC-CC are TP53, TERT promoter, AXIN1 and KMT2D (Cancer Cell 2019;35:932)
Sample pathology report
- Liver, tumor resection:
- Classical combined hepatocellular carcinoma-cholangiocarcinoma (see comment)
- Comment: This diagnosis is made based on morphological and phenotypical considerations. A tumor proliferation with 2 entangled components is observed: a well differentiated hepatocellular carcinoma component and a well differentiated intrahepatic cholangiocarcinoma component. The hepatocellular carcinoma component is composed of microtrabecular, massive and macrotrabecular architecture. Tumor cells are hepatoid and midsize with eosinophilic cytoplasm. The intrahepatic cholangiocarcinoma component is constituted of glandular, malformed and trabecular structures of small cuboidal cells. These tumor cells are accompanied by desmoplastic stroma. In the periphery of the tumor, we observed vascular and perineural invasion. There were no satellite nodules. Immunohistochemical staining showed cytoplasmic positivity of HepPar1 and glypican 3 in the hepatocellular carcinoma component and cytoplasmic positivity of CK7, CK19 and EpCAM in the intrahepatic cholangiocarcinoma component.
Differential diagnosis
- Hepatocellular carcinoma:
- Only features of hepatocellular carcinoma (no cholangiocarcinoma component)
- Pseudoglands in hepatocellular carcinoma should not be confused with the true glandular formation observed in intrahepatic cholangiocarcinoma
- Identification of bile can be very helpful
- There is no mucosecretion
- Importantly, marked bile ductular reaction with atypia adjacent to hepatocellular carcinoma due to mass effect is not an uncommon finding and one should be cautious not to overinterpret these atypical ductules as the cholangiocarcinoma component of a combined HCC‐CC
- Intrahepatic cholangiocarcinoma:
- Only features of intrahepatic cholangiocarcinoma with or without cholangiolocellular carcinoma component (no hepatocellular component)
- Mucin production
- Abundant desmoplastic stroma
Board review style question #1
Which of the following statements is correct regarding the liver neoplasm shown above?
- It is a cholangiolocellular carcinoma
- It is a hepatocellular carcinoma
- It is a poorly differentiated carcinoma
- It is an intrahepatic cholangiocarcinoma
- It shows unequivocal features of both hepatocytic and cholangiocytic differentiation
Board review style answer #1
E. It shows unequivocal features of both hepatocytic and cholangiocytic differentiation. It is, in fact, a combined hepatocellular carcinoma-cholangiocarcinoma.
Comment Here
Reference: Combined hepatocellular carcinoma-cholangiocarcinoma
Comment Here
Reference: Combined hepatocellular carcinoma-cholangiocarcinoma