Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Cevik L, Chen W. Simple biliary cyst. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liversolitarycyst.html. Accessed March 31st, 2025.
Definition / general
- Unilocular fluid filled intrahepatic cysts that do not communicate with the intrahepatic biliary tree
Essential features
- Most common hepatic cyst
- F > M; prevalence increases with age
- Diagnosis is based on radiologic and clinical findings; histologic evaluation is the gold standard but is usually not necessary
- Unilocular cyst lined by biliary type epithelium
Terminology
- Solitary bile duct cyst, simple hepatic cyst or benign hepatic cyst
Epidemiology
- Rare but is the most common type of hepatic cyst
- 1 - 2.5% of all individuals (Br J Radiol 1989;62:335)
- Occurs at all ages; prevalence increases with age (Br J Radiol 1989;62:335)
- F:M = 1.5:1 (Br J Radiol 1989;62:335)
Sites
- Anywhere in the liver but is more common in the right lobe
Pathophysiology
- Unknown; believed to be congenital and formed from bile ducts that do not connect to the biliary system
Clinical features
- Typically single and unilocular; rarely multilocular
- Family history and renal evaluation should be considered for autosomal dominant polycystic disease if the lesion is multilocular
- Mostly asymptomatic and incidental
- Symptomatic cysts are usually larger than asymptomatic cysts (Adv Surg 1997;31:127)
- Rarely causes abdominal discomfort, pain or distension and nausea due to mass effect
- Larger cysts can cause atrophy of adjacent hepatic tissue; complete atrophy of hepatic lobe causes compensatory hypertrophy of the other lobe
- Complications: spontaneous hemorrhage, infection, torsion of pedunculated cyst, rupture or local biliary obstruction (rare; associated with large cysts) (Adv Surg 1997;31:127)
Diagnosis
- Diagnosis is based on radiologic and clinical findings
- Histologic examination is usually not necessary, although it is the gold standard
Laboratory
- Laboratory findings are typically normal; increased gamma glutamyltransferase (GGT) in minority of cases (J Clin Gastroenterol 2010;44:289)
- CEA and CA 19-9 may be elevated (J Clin Gastroenterol 2010;44:289)
- Increased cyst fluid and serum CA 19-9 levels due to expression in the inner epithelial lining of simple cyst (Liver 1996;16:255)
- Not useful to differentiate the types of hepatic cysts (J Hepatol 2022;77:1083)
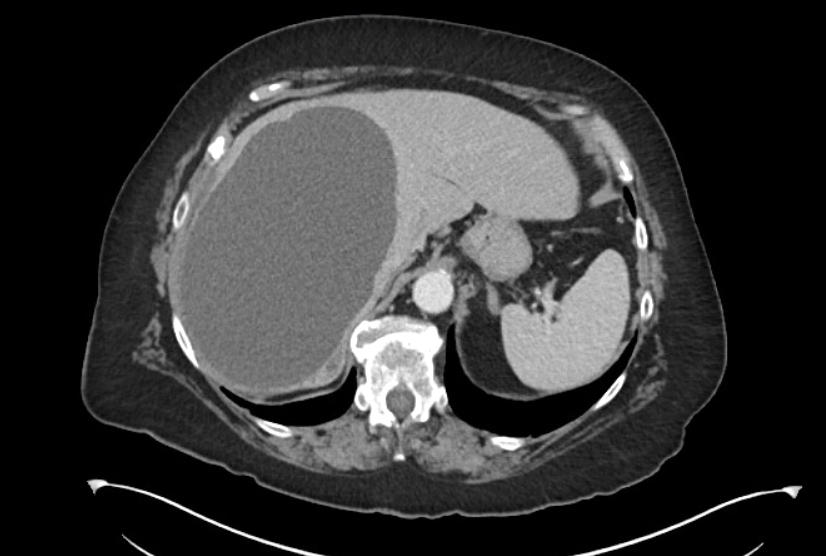
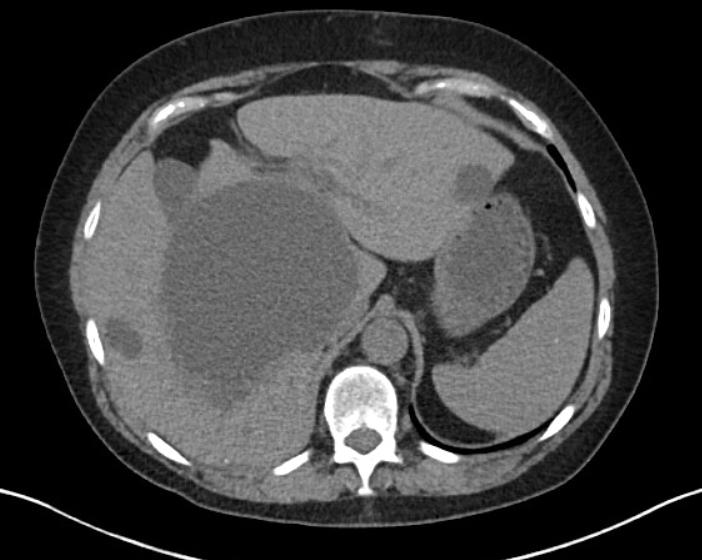
Radiology description
- Ultrasonography:
- Most helpful initial test for the differentiation
- Sensitivity and specificity of ~90% (Semin Roentgenol 1983;18:94)
- Anechoic (fluid filled), unilocular, oval or spherical shaped cavity with smooth borders, strong posterior acoustic enhancements (indicates a well defined fluid tissue interface) and no septations (World J Gastroenterol 2013;19:3543)
- Uncomplicated simple cyst is never septated
- CT scan:
- Well demarcated water attenuation lesion that does not enhance with intravenous contrast
- MRI:
- Well defined water attenuation lesion that does not enhance with intravenous gadolinium
- Low signal on T1 and very high intensity on T2 weighted images
- Microbubble contrast enhanced ultrasound (CEUS):
- Visualize vascular flow within septa or solid components of cysts (absent in simple cysts) (Ultrasound Q 2006;22:31)
- Helpful when ultrasound, CT or MRI shows ambiguous features
Radiology images
Prognostic factors
- Malignancy arising within a simple biliary cyst is thought to be extremely rare (Burt: MacSween's Pathology of the Liver, 7th Edition, 2017)
Case reports
- 57 year old woman with acute abdominal pain (Surg Case Rep 2015;1:71)
- 67 year old woman with acute abdominal pain (Surg Case Rep 2016;2:148)
- 67 year old man with anorexia and upper quadrant pain (World J Gastroenterol 2005;11:1881)
- 72 year old woman with abdominal pain for 24 hours (GE Port J Gastroenterol 2020;27:124)
- 84 year old woman with abdominal distention (World J Gastrointest Surg 2020;12:549)
Treatment
- Asymptomatic patients:
- No intervention or follow up until they become symptomatic
- Symptomatic patients:
- Large, symptomatic liver cysts might need intervention
- Cysts are usually > 4 cm
- Other causes for the symptoms should be excluded
- Several intervention types are available:
- Percutaneous aspiration:
- Needle aspiration with injection of a sclerosing agent (PAS, ethanol, ethanolamine or tetracycline)
- Without sclerosing agent recurrence is ~100% because the fluid reaccumulates due to continuous secretion by the epithelial lining
- High failure rate and recurrence even with sclerosing agent
- Surgical intervention:
- Laparoscopic cyst deroofing
- Deroofing is the excision of the cyst wall that extends to the surface of the liver
- The fluid secreted by the remaining cyst wall leaks into the peritoneal cavity
- Internal cyst drainage with cystojejunostomy
- Open surgical cyst deroofing
- Liver resection
- Laparoscopic cyst deroofing
- Recurrence and morbidity rate in open deroofing surgery and cyst resection is lower than laparoscopic surgery
- Percutaneous aspiration:
- Reference: UpToDate: Diagnosis and Management of Cystic Lesions of the Liver [Accessed 26 January 2023]
Gross description
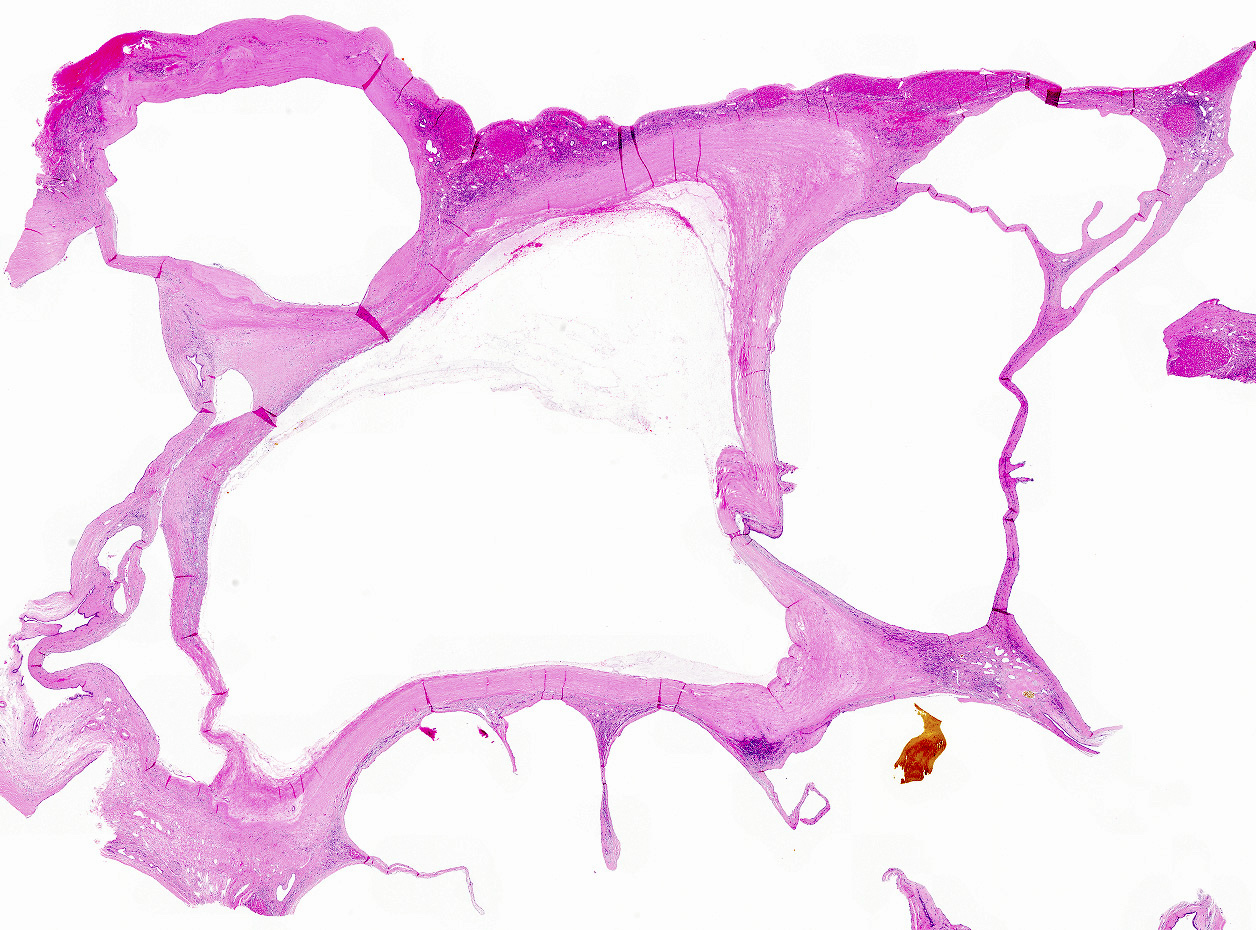
- Well circumscribed, fluid filled cavity, typically unilocular
- Cystic fluid is clear yellow but might be mucoid (mucoid lining), bloody (hemorrhage) or purulent (infection) (Histopathology 2022;81:402)
- Inner surface is smooth and glistening
- Size range: a few mm to tens of cm in diameter (UpToDate: Diagnosis and Management of Cystic Lesions of the Liver [Accessed 26 January 2023])
Frozen section description
- Unlike bile duct hamartomas and bile duct adenomas that may mimic metastatic carcinoma on intraoperative examination, large simple appearing biliary cysts are rarely sent for frozen section examination
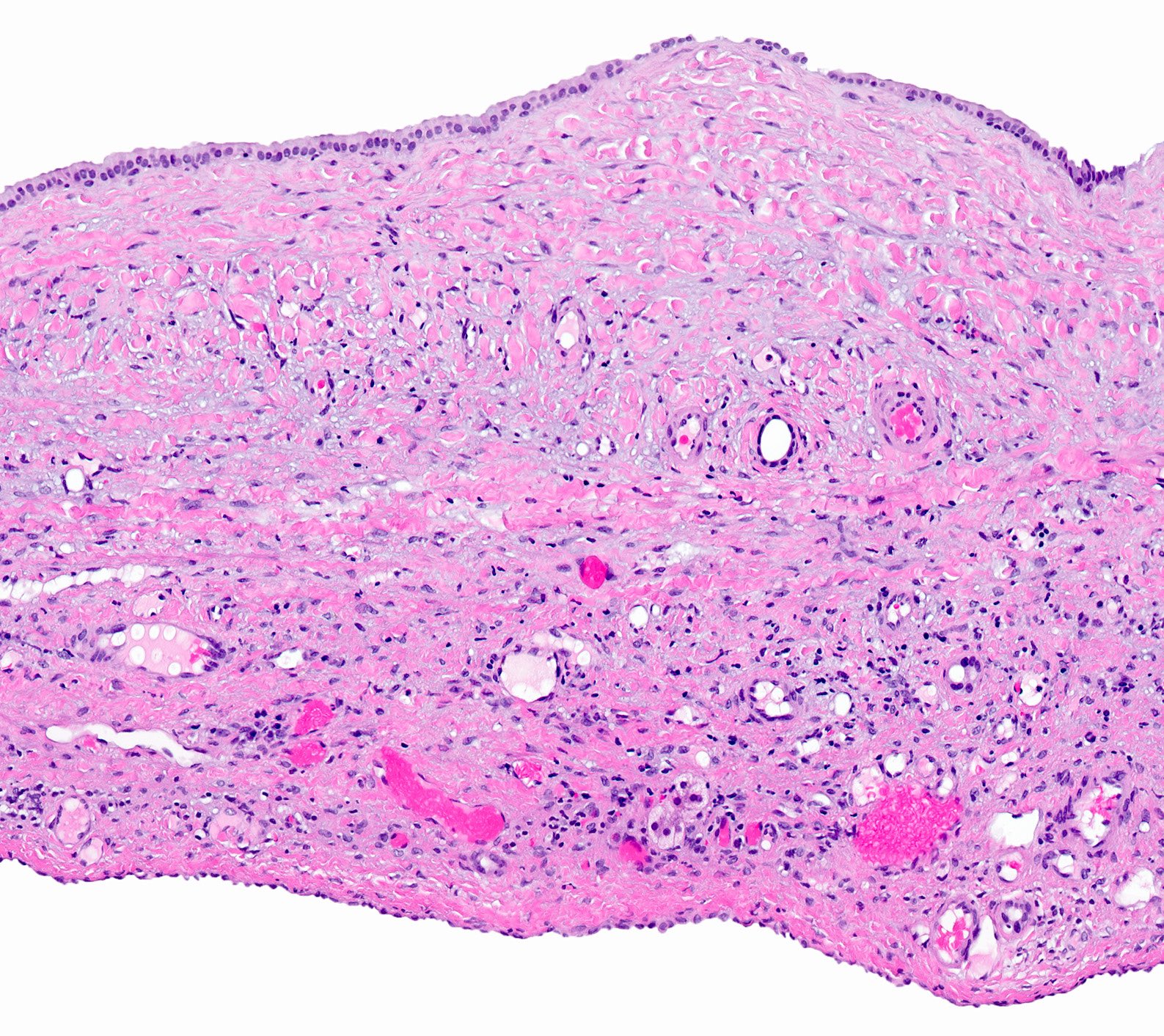
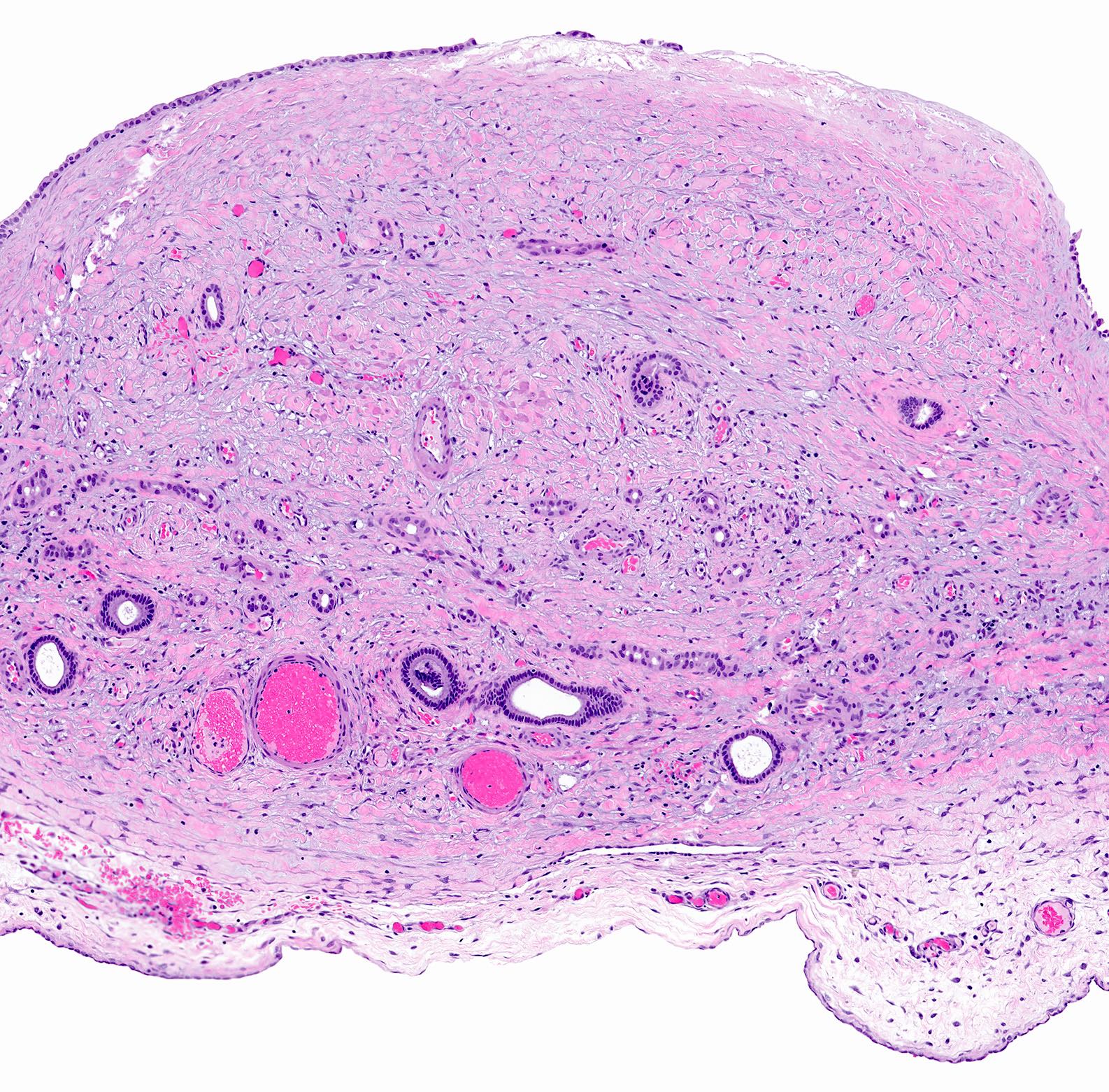
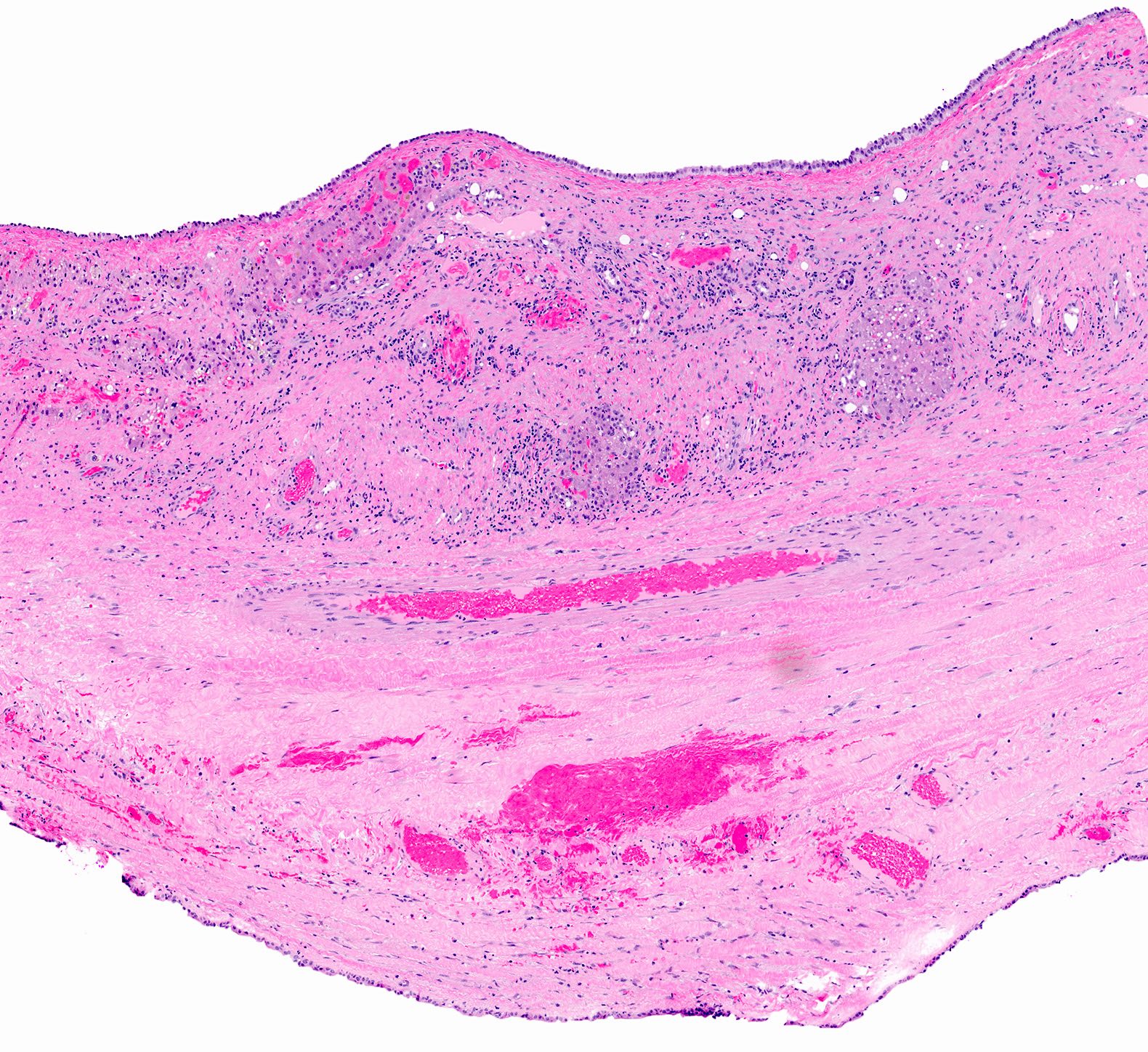
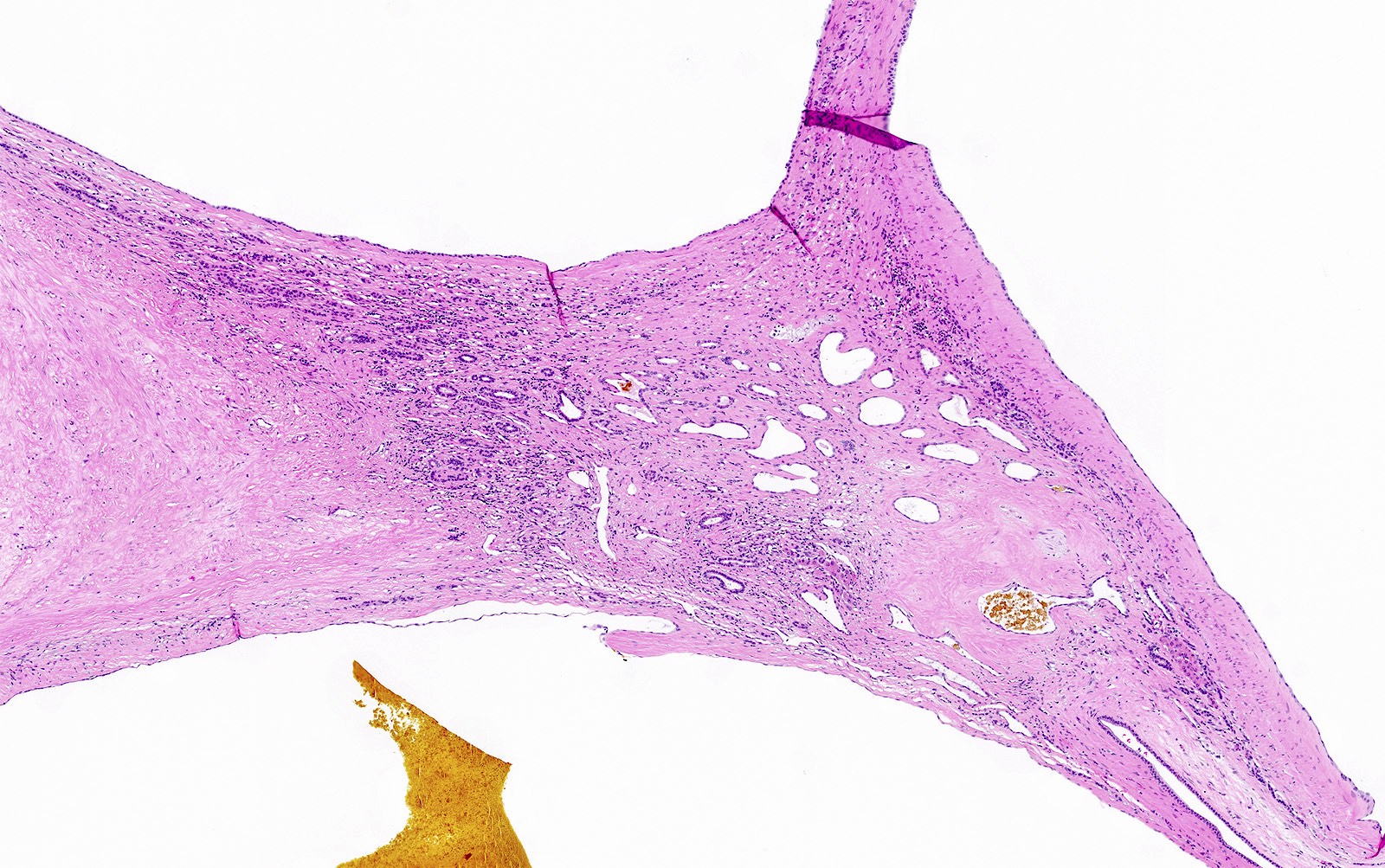
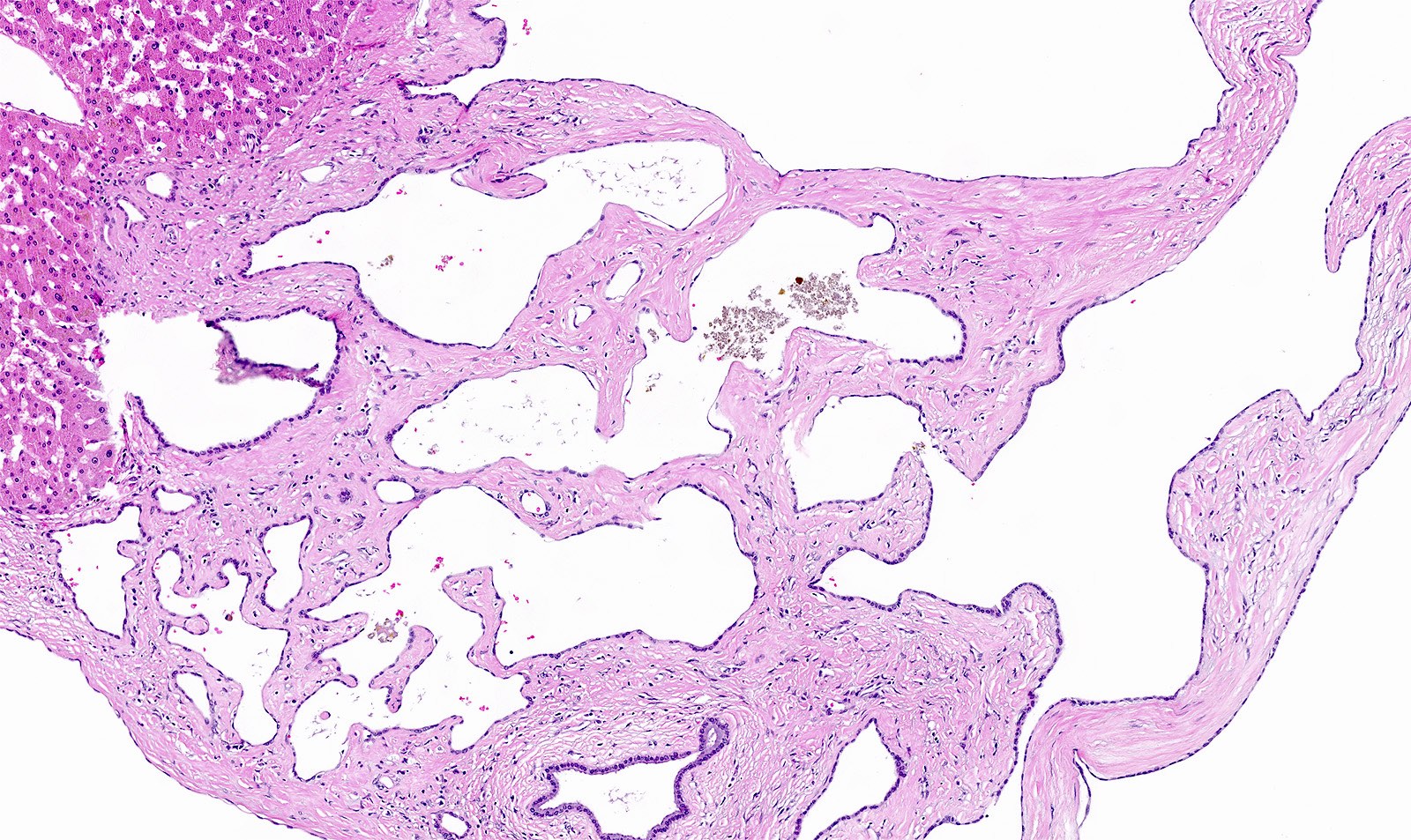
Microscopic (histologic) description
- Lined by biliary type epithelium (cuboidal to columnar cells)
- Epithelium might be attenuated or denuded
- Epithelial cells contain small amount of mucin or there can be focal mucinous epithelium due to metaplasia (Histopathology 2022;81:402)
- Cysts lack ovarian type stroma
- Cyst wall is usually fibrotic and can be hyalinized
- Cyst wall may contain islands of hepatocytes, bile ducts, hemorrhage and mild inflammation
- Other types of metaplasia (intestinal, pyloric, squamous) can be seen
- A biliary hamartoma is occasionally present in neighboring liver
- If multiple, polycystic liver disease should be considered
- Rarely, carcinoma is present
- Mostly adenocarcinoma, rarely squamous or adenosquamous carcinoma
Microscopic (histologic) images
Cytology description
- Aspiration is usually not required
Sample pathology report
- Hepatic cyst, excision:
- Benign biliary type cysts (see comment)
- Comment: The cyst wall is lined by biliary epithelium. No ovarian type of stroma is identified. No evidence of dysplasia or malignancy.
- Liver, cyst, excision:
- Simple (biliary) cyst
Differential diagnosis
- Ciliated hepatic foregut cyst:
- Lined by ciliated columnar epithelium
- Cyst wall contains smooth muscle
- Subcapsular location, average 4 cm in size, unilocular in 90% of cases (Hepatobiliary Pancreat Dis Int 2008;7:581)
- Mesothelial cyst:
- Usually hilar location, subcapsular
- Lined by mesothelial cells (positive for calretinin and WT1 by immunohistochemistry)
- Mucinous cystic neoplasm:
- Large cyst lined by intestinal, pseudopyloric or gastric foveolar type epithelium surrounded by characteristic dense ovarian type stroma
- Hepatic abscess:
- Creamy, yellow, foul smelling pus filled mass in the liver
- Lack of true cyst epithelial lining
- Necrotic malignant tumor with cystic degeneration:
- Malignant cells with necrotic material in the center
- Choledochal cyst:
- Involves extrahepatic bile duct
- Younger patients
- Lymphocytic inflammation in the wall of the cyst
- Cyst wall fibrosis composed of dense collagen and smooth muscle bundles
- Adult patients
- Mucosal inflammation and hyperplasia
- Histology can vary depending on the type of choledochal cyst
- Type I and IV: absence or patchy distribution of biliary mucosa
- Type II: similar to gallbladder duplication
- Type III: frequently lined by duodenal mucosa, rarely lined by biliary mucosa
- Type V: usually shows hepatic fibrosis
- Hemangioma:
- Should be in the differential diagnosis of multiloculated cysts with hyalinized stroma and flattened epithelium
Board review style question #1
Board review style answer #1
D. Simple biliary cyst. Simple biliary cysts are usually incidental cysts recognized during autopsy or imaging for other causes. They are more common in women. They are well circumscribed and usually filled with yellow clear fluid if not infected (choice B is incorrect). Inner surface of the cyst is smooth and glistening. The cyst wall is lined by cuboidal to columnar epithelium similar to biliary epithelium with an underlying thin fibrous tissue (choice A is incorrect). The epithelium might contain mucinous metaplasia but the cyst wall does not have an ovarian type stroma (choice C is incorrect).
Comment Here
Reference: Simple biliary cyst
Comment Here
Reference: Simple biliary cyst
Board review style question #2
Which of the following is true regarding simple biliary cysts of the liver?
- Cyst lining is positive for calretinin and WT1 by immunohistochemistry
- Epithelial cells contain a small amount of mucin and ovarian type stroma is lacking
- Increased cyst fluid and serum CA 19-9 levels are diagnostic for simple biliary cysts
- Treatment is required in both asymptomatic and symptomatic patients
Board review style answer #2
B. Epithelial cells contain a small amount of mucin and ovarian type stroma is lacking. Increased cyst fluid and serum CA 19-9 levels might be increased but this feature is not specific to the diagnosis and not useful to differentiate the types of hepatic cysts (choice C is incorrect). Mesothelial cysts are lined by mesothelial cells which are positive for calretinin and WT1 by immunohistochemistry (choice A is incorrect). Treatment for asymptomatic patients is typically to follow up; however, symptomatic patients with large cysts might need intervention (choice D is incorrect).
Comment Here
Reference: Simple biliary cyst
Comment Here
Reference: Simple biliary cyst