Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Lee W. Neuroendocrine carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livertumorNEcarcinoma.html. Accessed January 4th, 2025.
Definition / general
- Poorly differentiated neuroendocrine carcinomas are high grade, primary malignant epithelial neoplasms of liver or intrahepatic bile ducts with neuroendocrine differentiation
- Divided into small cell carcinoma (SCNET) and large cell carcinoma (LCNEC)
Essential features
- Exceedingly rare, virtually a diagnosis of exclusion after ruling out the possibility of metastasis
- Can be a component of mixed neuroendocrine - nonneuroendocrine neoplasm (MiNEN) with hepatocellular carcinoma or cholangiocarcinoma
- Ki67 proliferation index > 20% (typically > 50%) with abundant apoptosis and necrosis
Terminology
- Poorly differentiated neuroendocrine carcinoma, including small cell carcinoma (SCNEC) and large cell carcinoma (LCNEC)
- Mixed neuroendocrine - nonneuroendocrine neoplasm (MiNEN)
- Not recommended: carcinoid tumor of the liver, atypical carcinoid tumor of the liver
ICD coding
Epidemiology
- Exceedingly rare (0.3% of neuroendocrine neoplasms, < 0.5% of primary hepatic malignancies, < 100 cases reported) (Endocrine 2017;58:368, Endocr Relat Cancer 2010;17:909, Case Rep Oncol 2023;16:681)
- Usually not associated with chronic liver disease / cirrhosis
Sites
- Liver and intrahepatic bile ducts
Pathophysiology
- Not known; 2 hypotheses (Case Rep Oncol 2023;16:681)
- Originated from neuroendocrine cells in the intrahepatic bile duct epithelium
- Dedifferentiated from other malignant cells (malignant hepatocytes)
Etiology
- Not known
Clinical features
- Not well known due to rarity
- It is extremely important to rule out metastatic disease from other organs (e.g., gastrointestinal [GI] tract, pancreas and lung) by clinical workup (e.g., endoscopy, colonoscopy) and imaging study (e.g., gallium 68 dotatate scan and positron emission tomography / computed tomography [PET / CT])
Diagnosis
- Diagnosis of exclusion after ruling out metastasis (fluorodeoxyglucose [FDG] PET scan can be helpful)
- Due to its rarity and lack of characteristic imaging appearance, diagnosis is made by cytology / fine needle biopsy or on surgical specimens
Radiology description
- Large solitary mass with necrosis
- Hyperenhancement in the arterial phase and washout in the portal venous phase due to rich blood supply (similar to hepatocellular carcinoma [HCC]) (Case Rep Oncol 2023;16:681)
- Gallium 68 dotatate PET / computed tomography (CT) scan may show uptake in the lesion and can be used to rule out metastasis
Prognostic factors
- Not known; generally considered poor prognosis
Case reports
- 22 year old woman with primary hepatic NEC (Case Rep Oncol 2023;16:681)
- 39 year old man with mixed NEC and HCC (Front Surg 2021;8:678853)
- 76 year old man with poorly differentiated HCC and NEC (Am Surg 2016;82:1121)
- 84 year old woman with mixed NEC and HCC (World J Surg Oncol 2021;19:78)
Treatment
- Surgical resection
- Chemotherapy: platinum based regimen (not established)
Gross description
- Typically large solitary mass with areas of hemorrhage and necrosis; may be cystic
Frozen section description
- High grade malignant neoplasm with necrosis, apoptosis and mitotic activity
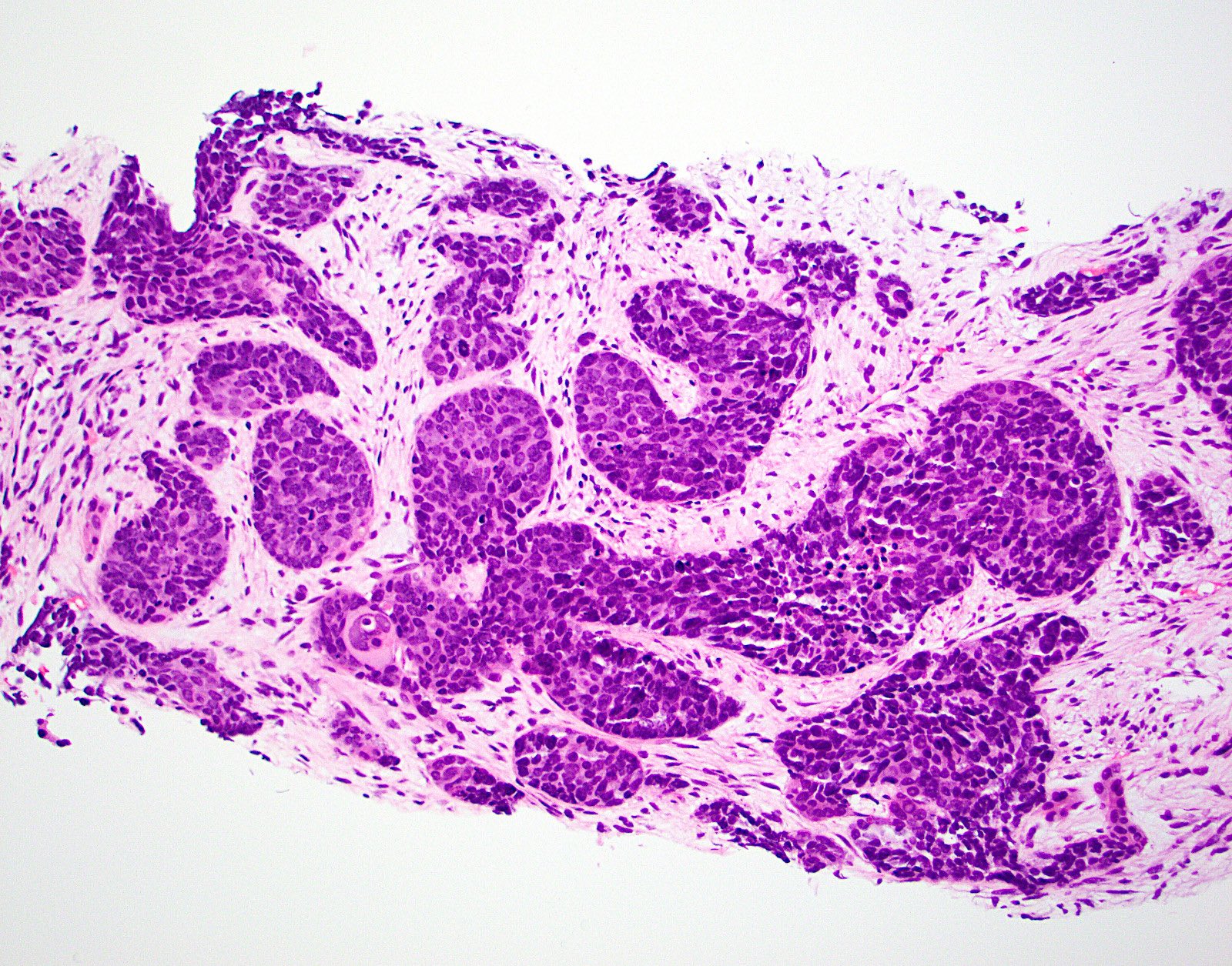
Microscopic (histologic) description
- Similar histomorphology of poorly differentiated neuroendocrine carcinoma of anywhere in the body
- Solid sheet-like proliferation of the tumor cells with geographic area of necrosis, high mitotic figures and abundant apoptosis (Front Oncol 2013;3:2)
- Small cell NEC: cellular pleomorphism with high N:C ratio, nuclear atypia, hyperchromasia, nuclear molding and frequent mitotic figures
- Large cell NEC: more rounded, marked nuclear pleomorphism with prominent nucleoli
- May have signet ring cell morphology with intracytoplasmic vacuoles negative for mucin but positive for neuroendocrine markers (Semin Liver Dis 2010;30:422)
- If mixed neuroendocrine - nonneuroendocrine neoplasm (MiNEN), 2 types have been reported (J Chin Med Assoc 2009;72:430)
- Collision type tumor: 2 simultaneous but histologically distinct tumors without histologic admixture
- Combined type tumor: both components intermingle with each other and cannot be separated in the transitional area
Microscopic (histologic) images
Cytology description
- High N:C ratio with nuclear molding, dark chromatin with inconspicuous nucleoli, background necrosis and typical crush artifact / nuclear streaming
Positive stains
- Cytokeratins (CK AE1 / AE3, CAM5.2, CK8 / CK18): may show perinuclear dot-like staining pattern
- Synaptophysin: usually positive; rarely weak or focal
- Chromogranin: usually positive; can be weak and patchy or can be almost absent
- INSM1: new marker of neuroendocrine differentiation; may have better sensitivity in neuroendocrine carcinoma (Am J Pathol 2015;185:3164)
- p53: aberrant expression, either overexpression or null type expression (PLoS One 2017;12:e0187667)
- No site specific IHC stain for hepatic NEC: panel still can be used to exclude metastasis (Torbenson: Tumors of the Liver (AFIP Atlas of Tumor Pathology), 4th Edition, 2018)
- Caveat
- Occasional HCCs can show aberrant staining for synaptophysin or CD56, which does not qualify as the combined HCC - NEC (Torbenson: Biopsy Interpretation of the Liver, 4th Edition, 2021)
- Neuroendocrine tumor can show focal arginase, HepPar1, glypican 3 and AFP staining (Torbenson: Biopsy Interpretation of the Liver, 4th Edition, 2021, Torbenson: Tumors of the Liver (AFIP Atlas of Tumor Pathology), 4th Edition, 2018)
- TTF1 can be positive in NEC regardless of the site of origin (Mod Pathol 2000;13:238)
Negative stains
- RB1: loss of Rb stain (Cancer Discov 2022;12:692)
- Hepatocellular markers: HepPar, arginase1, glypican 3, unless mixed tumor (can show patchy positivity) (Torbenson: Biopsy Interpretation of the Liver, 4th Edition, 2021, Torbenson: Tumors of the Liver (AFIP Atlas of Tumor Pathology), 4th Edition, 2018)
- Beta catenin (J Hepatocell Carcinoma 2018;5:61)
Sample pathology report
- Liver, mass biopsy:
- Involved by poorly differentiated neuroendocrine carcinoma, consistent with small cell carcinoma (see comment)
- Comment: Primary neuroendocrine tumor of the liver is exceedingly rare. Radiologic and clinical correlation is recommended to exclude the possibility of metastatic disease.
Differential diagnosis
- Metastatic neuroendocrine carcinoma from other sites:
- Well differentiated neuroendocrine tumor (WDNET), grade 3:
- Organoid architecture
- Presence of low grade areas (tumor heterogeneity) favors WDNET
- Poorly differentiated hepatocellular carcinoma:
- Positive for hepatocellular markers
- Hepatoblastoma:
- Positive for beta catenin and hepatocellular markers
- Lymphoma:
- Negative for cytokeratin and neuroendocrine markers
- Melanoma:
- Positive for SOX10, HMB45, MelanA, PRAME
- Negative for cytokeratin and neuroendocrine markers
- Metastatic small round blue cell tumors: Ewing sarcoma, desmoplastic small round blue cell tumor, alveolar rhabdomyosarcoma, etc.:
- Negative for cytokeratin and neuroendocrine markers
Additional references
Board review style question #1
A large hepatic mass, shown in the image above, is biopsied. The tumor cells are positive for cytokeratin, synaptophysin and chromogranin. The Ki67 proliferative index is increased to more than 80%. Which of the following is characteristic of neuroendocrine carcinoma of the liver?
- Hepatic primary is more common than metastasis
- It can be seen as a component of hepatocellular carcinoma or cholangiocarcinoma
- It is a well differentiated neuroendocrine tumor
- It usually arises in the background of a cirrhotic liver
- Tumor cells are typically positive for arginase, HepPar1 or glypican 3
Board review style answer #1
B. It can be seen as a component of hepatocellular carcinoma or cholangiocarcinoma. This tumor is a high grade neuroendocrine carcinoma. Primary hepatic neuroendocrine carcinoma is exceedingly rare and the diagnosis should be made after carefully excluding possible metastatic disease. It can be a component of mixed neuroendocrine - nonneuroendocrine neoplasm (MiNEN) with hepatocellular carcinoma or cholangiocarcinoma.
Answer A is incorrect because metastatic lesions in the liver are more common than hepatic primary. Answer C is incorrect because it is a poorly differentiated neuroendocrine carcinoma (PDNEC). Answer D is incorrect because neither primary hepatic PDNEC nor metastatic neuroendocrine neoplasms are usually found in the noncirrhotic background. Answer E is incorrect because hepatic PDNEC does not typically express hepatocellular markers unless it is mixed HCC - PDNEC.
Comment Here
Reference: Neuroendocrine carcinoma
Comment Here
Reference: Neuroendocrine carcinoma