Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sardana R, Zhang X. Hepatic infantile hemangioma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livertumorIHE.html. Accessed April 2nd, 2025.
Definition / general
- Benign vascular tumor with features similar to those of infantile hemangioma of the skin or superficial soft tissue in children
Essential features
- Numerous small and capillary-like vascular channels, especially the peripheral regions, lined by plump endothelial cells usually in a single layer
- Large cavernous vessels lined by flattened endothelial cells with fibrosis of the surrounding stroma in the center of large lesions
- Entrapment of hepatocytes and small bile ducts at the advancing edges of the lesion
Terminology
- Preferred: hepatic infantile hemangioma (HIH)
- Subtypes: single / focal HIH (SHIH), multifocal HIH (MHIH) and diffuse HIH (DHIH)
- Not recommended: hemangioendothelioma type 1 or type 2 (type 2 is currently classified as angiosarcoma), infantile hemangioendothelioma; juvenile hemangioma, hepatic small vessel neoplasm
ICD coding
Epidemiology
- Most common hepatic mesenchymal tumor in infants and children (Diagnostics (Basel) 2021;11:333, Pediatr Gastroenterol Hepatol Nutr 2020;23:72)
- F > M, up to 2:1 (J Pediatr Surg 2012;47:165)
- 90% are diagnosed at < 6 months of age (Pediatr Int 2014;56:304)
- Rarely can develop prenatally
- 10 - 15% have coexisting hemangiomas of skin and other sites
- Higher risk in patients with multiple cutaneous infantile hemangiomas (J Am Acad Dermatol 2021;84:1378)
- 50% are incidental findings at autopsy
- May coexist with hepatoblastoma, mesenchymal hamartoma and Beckwith-Wiedemann syndrome (Int J Surg Pathol 2023;31:485, Am J Med Genet A 2020;182:1972, J Surg Case Rep 2018;2018:rjx260, J Pediatr Surg 2012;47:448, Surg Case Rep 2022;8:161, J Formos Med Assoc 2007;106:S1, Am J Med Genet A 2024;194:88)
Sites
- Liver
Pathophysiology
- Pathophysiology of HIH is still unknown
- Aberrant response of pluripotent stem cells to stimuli, including hypoxia and the renin angiotensin system have been proposed (Arterioscler Thromb Vasc Biol 2007;27:2664, J Hematol Oncol 2014;7:13, Precis Clin Med 2022;5:pbac006, Clin Cancer Res 2013;19:3360)
Etiology
- No specific proven etiology
- Earlier considered to be associated with female gender, multigestational pregnancy, low birth weight and prematurity (Birth Defects Res 2017;109:809, World J Pediatr 2020;16:377)
Clinical features
- Most cases are asymptomatic and diagnosed incidentally
- Only 9.7% patients detected by regular screening are symptomatic (J Am Acad Dermatol 2021;84:1378)
- May grow progressively and then involute, especially SHIH
- Common symptoms: hepatomegaly, abdominal distension, failure to thrive
- Consumptive hypothyroidism: overexpression of type 3 iodothyronine deiodinase in tumor cells, inactivates thyroid hormone
- Congestive heart failure due to macrovascular (arteriovenous, arterioportal or portovenous) shunting (J Emerg Med 2021;60:107, BMC Cardiovasc Disord 2019;19:216)
- Abdominal compartment syndrome with compromised ventilation and poor inferior vena caval blood return to the heart
- Thrombocytopenia and coagulopathy
- DHIH is associated with more serious manifestations than MHIH (J Pediatr Surg 2012;47:165)
Diagnosis
- Imaging studies
- Histologic examination
- Tumor cells express endothelial cell markers (factor VIII related antigen, ERG, CD31 and CD34) and GLUT1 (except SHIH)
Laboratory
- Usually normal alpha fetoprotein (AFP); rarely elevated due to secretion from entrapped or uninvolved hepatocytes (Hum Pathol 2010;41:763)
Radiology description
- Generally not visualized on ultrasound beyond 18 - 24 months of age
- Ultrasound
- Well defined hypo or hyperechoic
- Multifocal or diffuse
- Hyperenhancement in arterial phase (AJR Am J Roentgenol 2020;214:658)
- MRI
- Homogeneously enhanced
- Hypointense relative to the liver on T1 weighted images
- Hyperintense on T2 weighted images (Eur J Radiol 2010;76:e24)
Prognostic factors
- Mortality as high as 16%, with up to 38% in DHIH (J Pediatr Surg 2015;50:837)
- Proliferative phase for > 2 years of age or new lesion after 1 year of age has worse outcome
- Poor prognostic factors: heart failure, diffuse HIH, abdominal compartment syndrome
Case reports
- Neonate girl with hepatic mass diagnosed in utero by ultrasonography (Cureus 2022;14:e25240)
- 10 day old girl presented with high output failure (J Emerg Med 2021;60:107)
- 11 day old boy with giant hepatic infantile hemangioma causing postnatal respiratory arrest (Sisli Etfal Hastan Tip Bul 2020;54:108)
- 18 day old girl presented with jaundice and abdominal mass (Medicine (Baltimore) 2018;97:e12863)
- 2 month old girl with hepatomegaly and diffuse intrahepatic lesions (Front Oncol 2024;14:1336742)
Treatment
- Treatment strategies range from simple observation to a series of medical, surgical and radiological interventions
- Spontaneous involution in 5 - 10% by 6 - 8 months; resection if solitary, otherwise steroids, interferon, propranolol, radiation therapy, embolization or transplantation (World J Surg 2009;33:597, Pediatr Surg Int 2021;37:791, Pediatrics 2019;143:e20183475)
- Regular screening in patients with ≥ 5 cutaneous hemangiomas
- Routine thyroid hormone level monitoring and echocardiography (Semin Pediatr Surg 2020;29:150970)
Gross description
- Tumors can be single (~55%), multiple or diffuse (~45%) with mean size of 4 cm (range: 0.1 - 15 cm)
- Multifocal lesions usually progress to coalescent nodules diffusely replacing normal hepatic parenchyma (World J Hepatol 2021;13:1316)
- Individual lesions are well defined, noncapsulated, often with fibrotic scarring in the center and red-brown vascularized areas in the periphery; small lesions often appear spongy and red-brown on sectioning
- Hemorrhagic, infarcted and calcified areas can be seen
Microscopic (histologic) description
- Noncapsulated and irregular margins extending into surrounding hepatic tissue
- Small, capillary-like vascular channels lined by flattened or plump endothelial cells
- Vascular proliferation is more prominent in the periphery and in the proliferation stage
- Tumor cells have small, bland, hyperchromatic nuclei without marked atypia and may have very rare mitosis
- Rare foci of pseudopapillary proliferation
- Intervening stroma is loosely fibrotic and generally scant
- Stroma undergoes further expansion and becomes more fibrotic towards the center of the tumor
- Entrapped bile ducts and hepatocytes can be seen at the advancing edges of the tumor
- Extramedullary hematopoiesis can be seen
Microscopic (histologic) images
Cytology description
- Oval to spindle shaped cells with scant cytoplasm and wavy, kinked and indented nuclear outlines (Cytopathology 2010;21:398, Acta Cytol 2010;54:807)
Positive stains
- Factor VIII related antigen, CD31, CD34, ERG, GLUT1 (except SHIH) (Australas J Dermatol 2009;50:136, J Pediatr 2018:203:294, Hum Pathol 2004;35:200, Ann Diagn Pathol 2020:46:151506)
- Upregulation of GLUT1, an erythrocyte type glucose transporter protein, helps to differentiate tumor cells undergoing aerobic glycolysis from their benign counterparts (Nat Rev Cancer 2011;11:325)
- Positive in 95% of HIH with extensive staining involving > 90% of lesional vessels (Pathol Res Pract 2017;213:591)
- GLUT1 positive endothelial cells in HIH express properties of facultative stem cells (resembling blood barrier as seen in placenta), whereas other vascular lesions show GLUT1 negative endothelial cells with stable phenotype (Stem Cells 2015;33:133)
Negative stains
- HepPar1, cytokeratin, p53 (wild type), S100, CD117 and Ki67 (low proliferation index, generally ~1% except HIH with atypical features [type 2 infantile hemangioendothelioma, currently classified as angiosarcoma]) (Hum Pathol 2023:141:78)
Sample pathology report
- Liver, excision:
- Infantile hemangioma (see comment)
- Comment: The resection reveals multiple noncapsulated vascular lesions comprised of numerous small and capillary-like vascular channels lined by plump endothelial cells in a single layer. The lesional cells show strong, diffuse CD31, CD34 and GLUT1 positivity. Ki67 proliferative index is < 1%. The findings are consistent with infantile hepatic hemangioma (multifocal).
- Liver, biopsy:
- Benign vascular neoplasm, consistent with infantile hepatic hemangioma (see comment)
- Comment: Imaging study with multiple liver lesions was noted. The biopsy reveals a benign vascular neoplasm characterized by numerous small and capillary-like vascular channels lined by plump endothelial cells. There are no cytologic atypia, necrosis or other high grade morphologic features. The tumor cells show diffuse, strong CD34, CD31 and GLUT1 positivity. The findings are consistent with infantile hepatic hemangioma.
Differential diagnosis
- Hepatic angiosarcoma:
- Solid spindle areas with marked atypia
- Ki67 proliferation index > 10% (Pediatr Blood Cancer 2017;64:e26627)
- Irregular margins infiltrating into adjacent liver parenchyma
- Variable GLUT1 immunopositivity
- Mesenchymal hamartoma:
- Hypocellular fibromyxoid stroma with bland spindle cells
- Malformed bile duct in duct plate configuration
- Occasionally can have prominent vascular proliferation
- GLUT1 negative
- Cavernous hemangioma:
- Usually well circumscribed
- Variably sized, dilated and thin walled vessels lined by a single layer of flat endothelial cells
- No cytologic atypia or mitosis
- GLUT1 negative
- Hepatic small vessel neoplasm:
- Average patient age 54 years, more common in men (Hum Pathol 2016;54:143)
- Infiltration into adjacent liver parenchyma
- Anastomosing, closely packed vascular spaces lined by flat endothelial cells with occasional hobnailing
- GLUT1 negative
- Recurrent hotspot mutations of GNAQ, GNA11, GNA14 and PIK3CA
- Hepatic vascular malformation (HVM):
- Rare cause of liver mass lesions
- Thicker walled shunt vessels lead to a central area of vascular proliferation, congestion, large dilated blood filled spaces with areas of organizing thrombi, calcification and fibrosis
- The periphery of the lesion often consists of an irregular rim of loose, sometimes myxoid reactive stroma containing numerous capillary type vessels
- Unlike in HIH, the demarcation between HVM and normal liver tissue is indistinct (Hum Pathol 2004;35:200)
- The adjacent liver tissue often contains abnormally enlarged, dilated vessels in the portal area and dilated hepatic sinusoids (Hum Pathol 2004;35:200)
- GLUT1 either negative or with focal staining but lacks the strong and diffuse staining as seen in HIH (Hum Pathol 2004;35:200)
Additional references
Board review style question #1
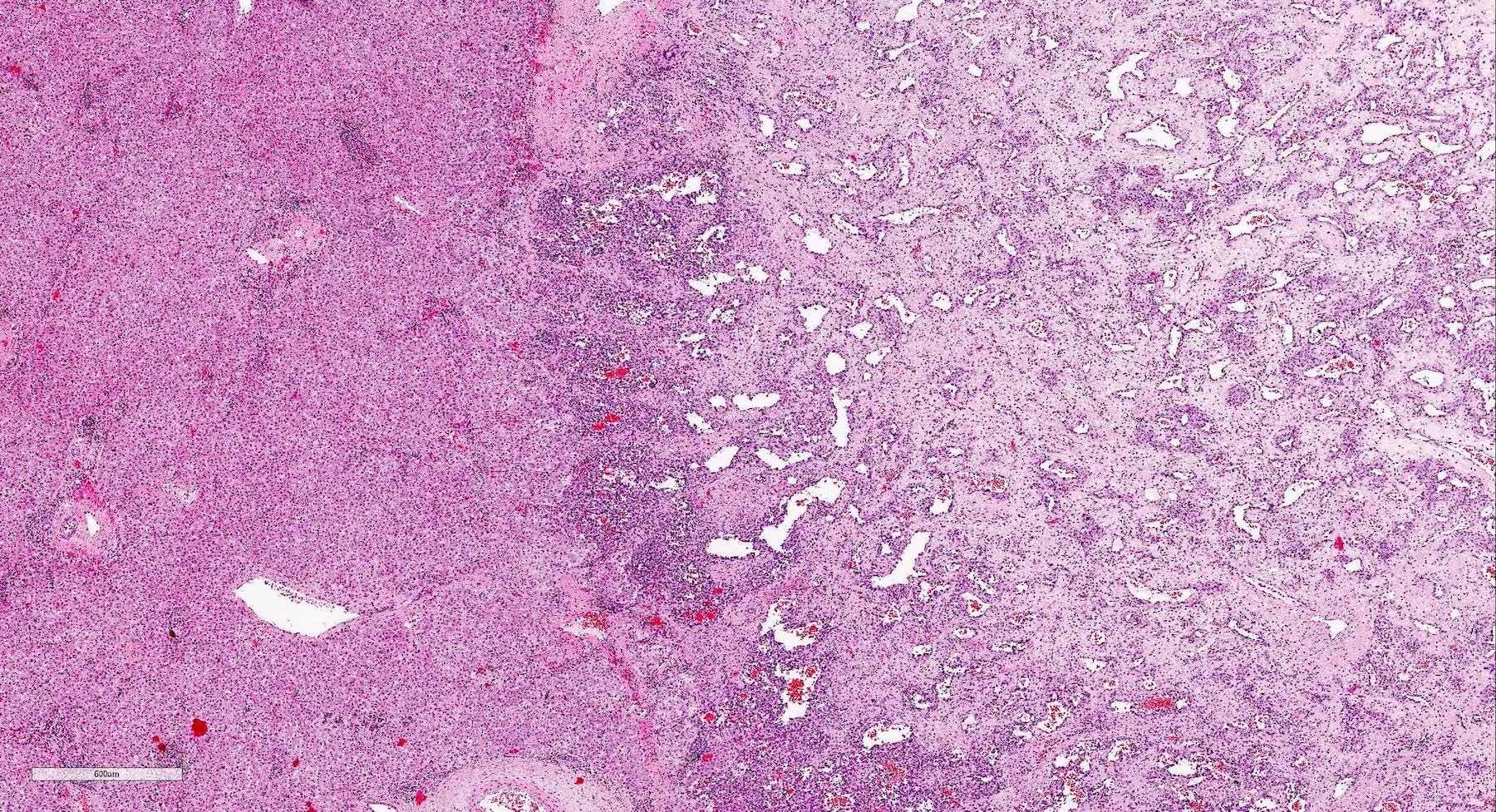
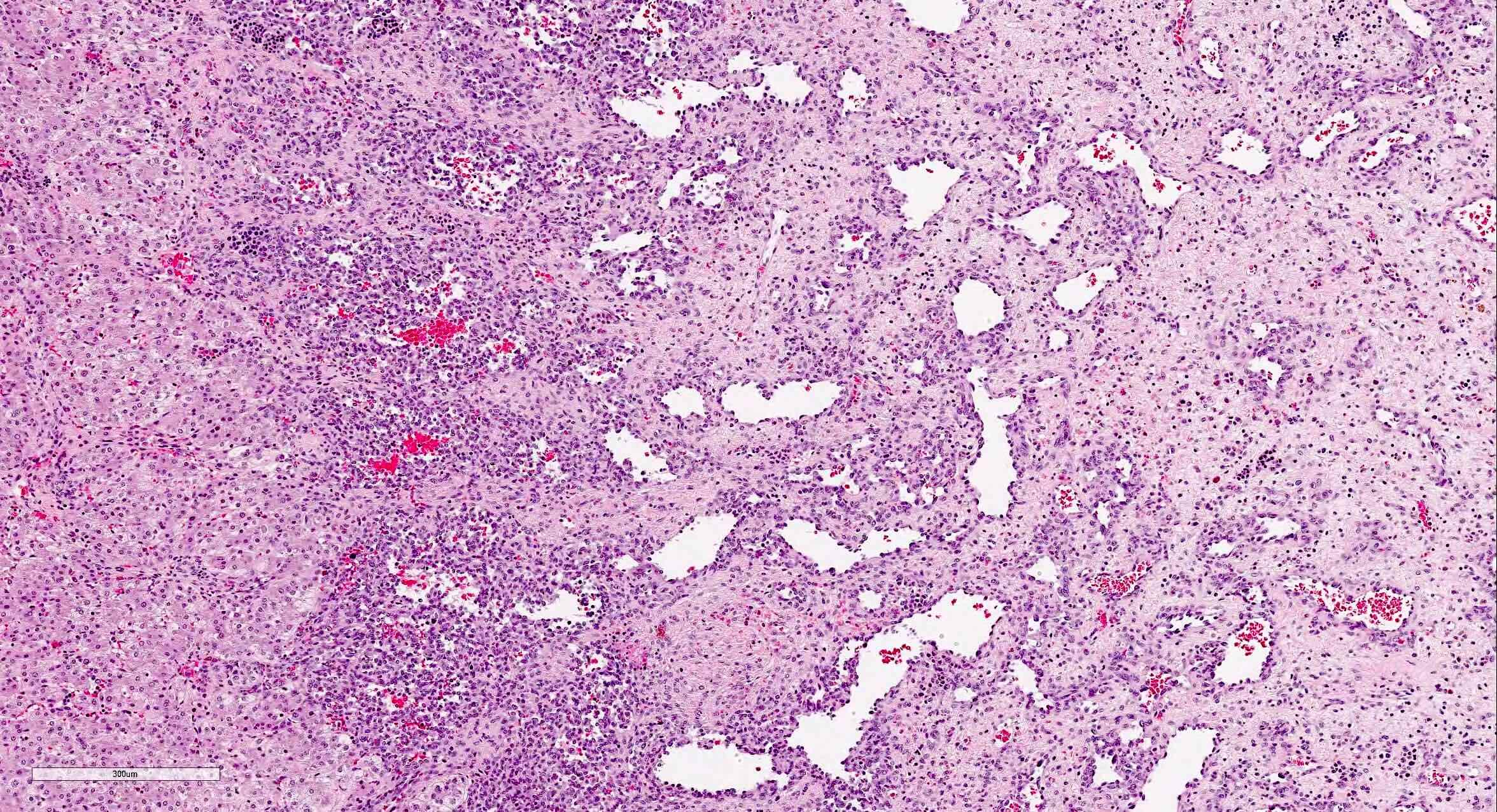
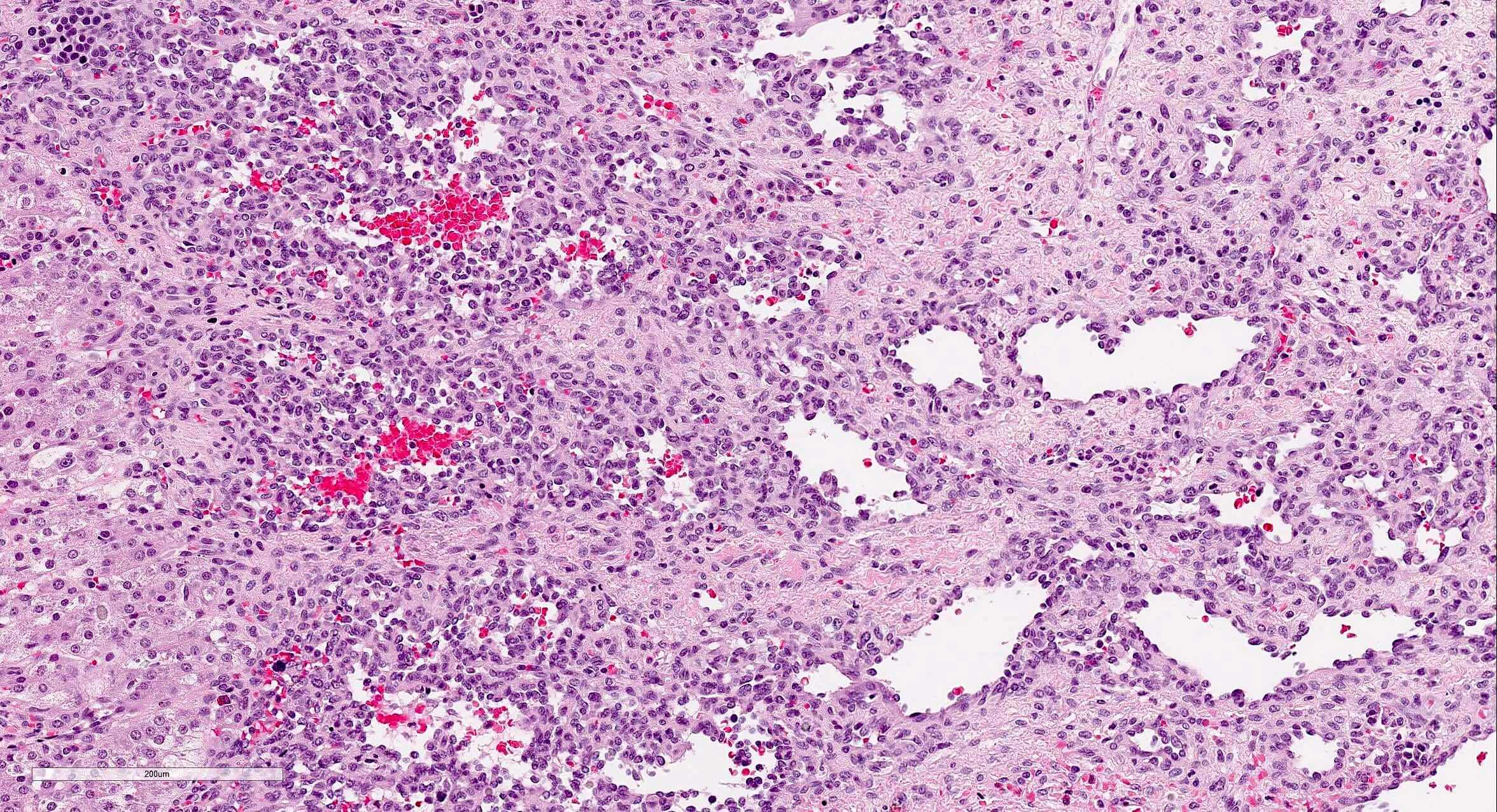
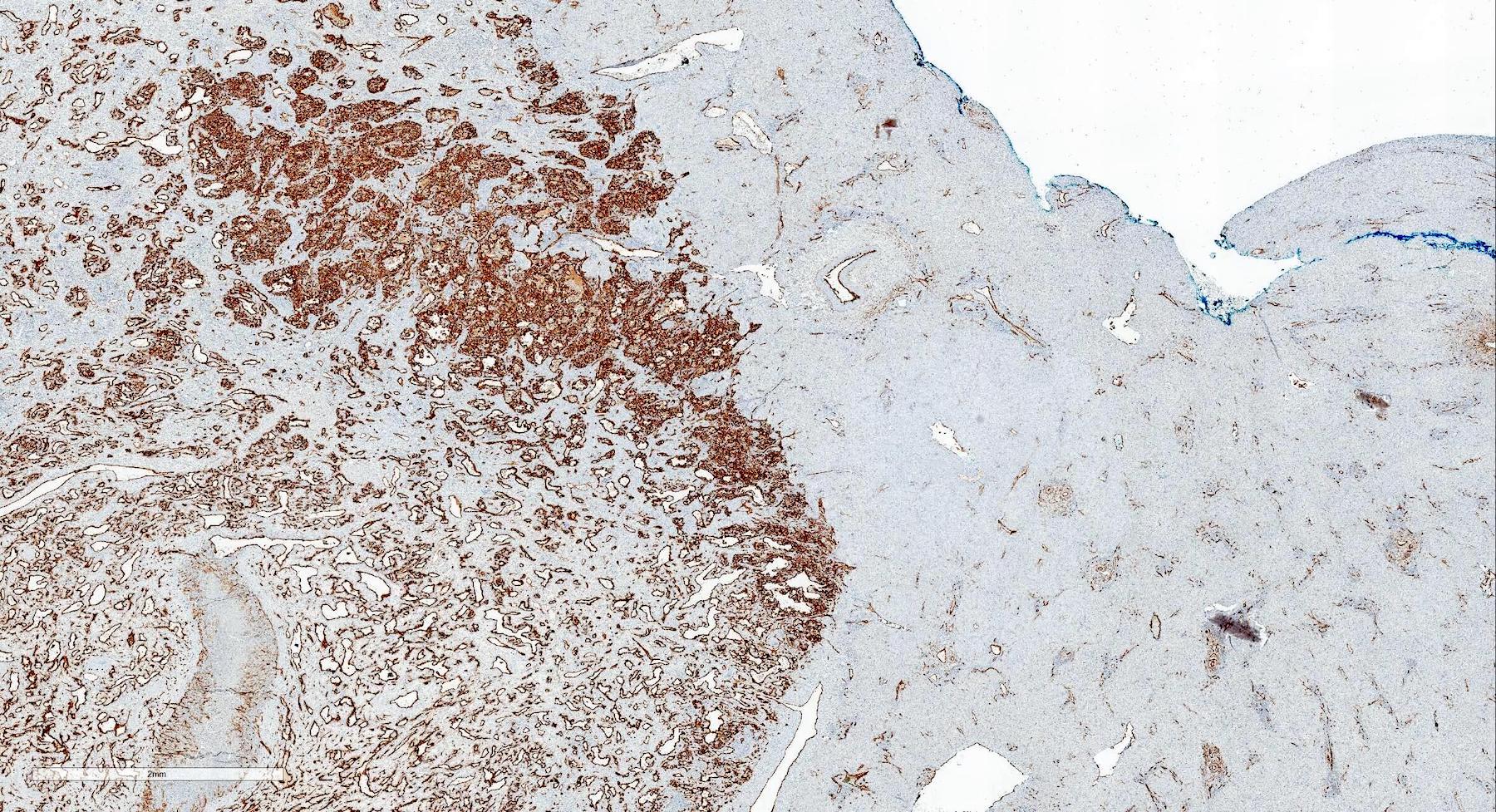
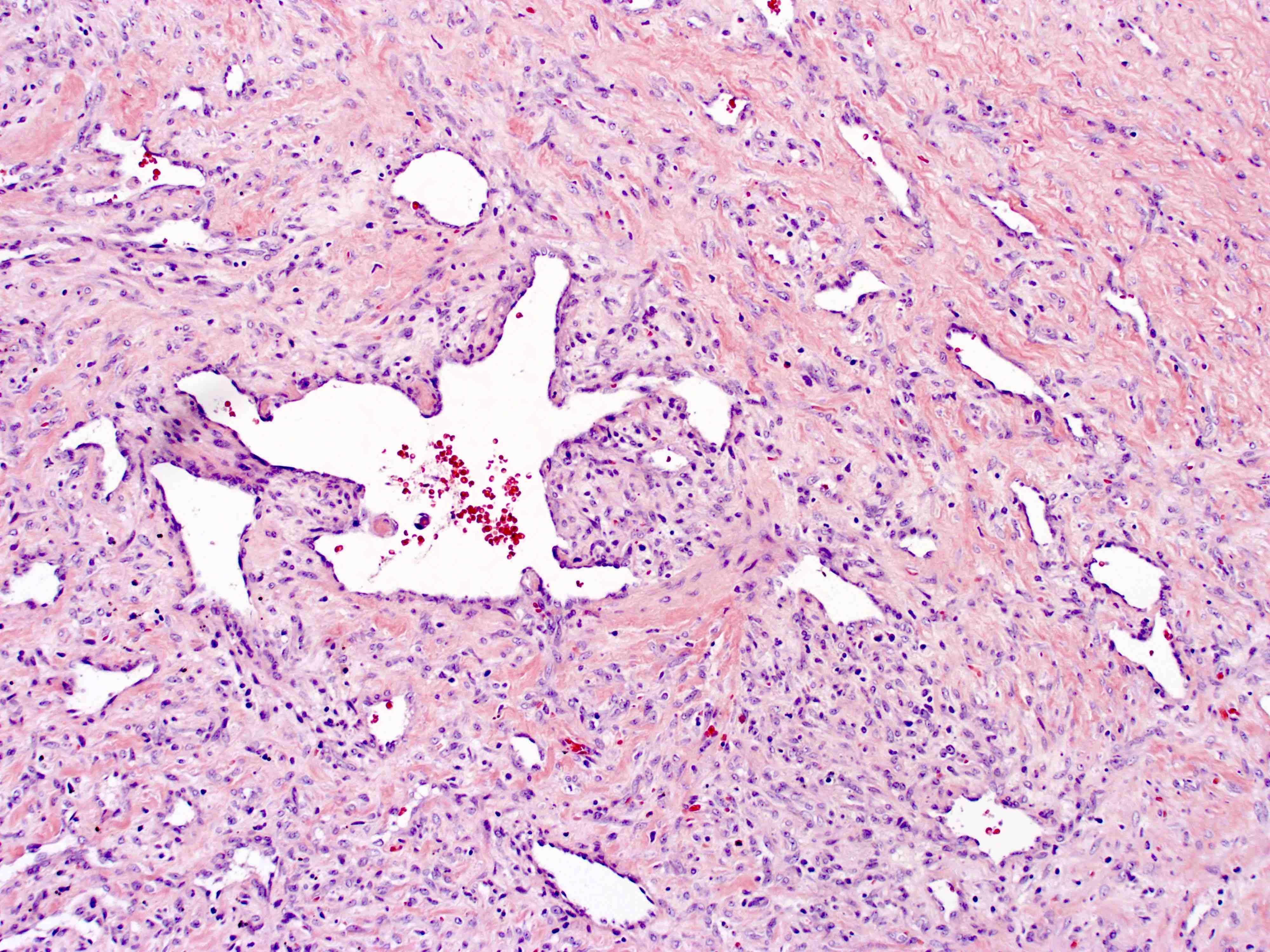
A 5.5 x 3.5 cm lesion in the liver (first image) is identified in the autopsy of a 10 month old girl. External examination reveals multiple cutaneous hemangiomas on the trunk and upper extremities. Microscopic examination of the liver lesion reveals a vascular neoplasm composed of numerous small and capillary-like vascular channels lined by plump endothelial cells with no cytologic atypia in the periphery region (second image). The tumor exhibits an irregular interface with the adjacent liver parenchyma. In the central region of the tumor, there are a few large, cavernous vessels lined by flattened endothelial cells, accompanied by fibrosis of the surrounding stroma (third image). The tumor cells are positive for CD31, CD34 and GLUT1 by immunohistochemistry. Which is the best diagnosis of this lesion?
- Angiosarcoma
- Cavernous hemangioma
- Hepatic infantile hemangioma
- Mesenchymal hamartoma
Board review style answer #1
C. Hepatic infantile hemangioma. The gross photograph and microscopic description identify the lesion as a benign vascular neoplasm. Micrograph shows a vascular neoplasm with numerous small and capillary-like vascular channels lined by plump endothelial cells with no cytologic atypia. In the center of the lesion shows stromal fibrosis and few large, cavernous vessels lined by flattened endothelial cells. CD31, CD34 and GLUT1 are positive in the lesional endothelial cells, confirming diagnosis of hepatic infantile hemangioma. Answer A is incorrect because angiosarcoma should show marked nuclear atypia, abundant atypical mitotic figures and solid spindled areas. Answer B is incorrect because cavernous hemangioma is a common subtype of hepatic hemangioma in adults showing circumscribed proliferation of variably sized, dilated and thin walled vessels lined by a single layer of flat endothelial cells. Answer D is incorrect because mesenchymal hamartoma, the second most common benign pediatric hepatic tumor after hepatic infantile hemangioma, is comprised of variable proportions of disorganized arrangements of primitive mesenchyme with benign dilated or branching bile ducts and clusters of normal appearing hepatocytes.
Comment Here
Reference: Hepatic infantile hemangioma
Comment Here
Reference: Hepatic infantile hemangioma
Board review style question #2
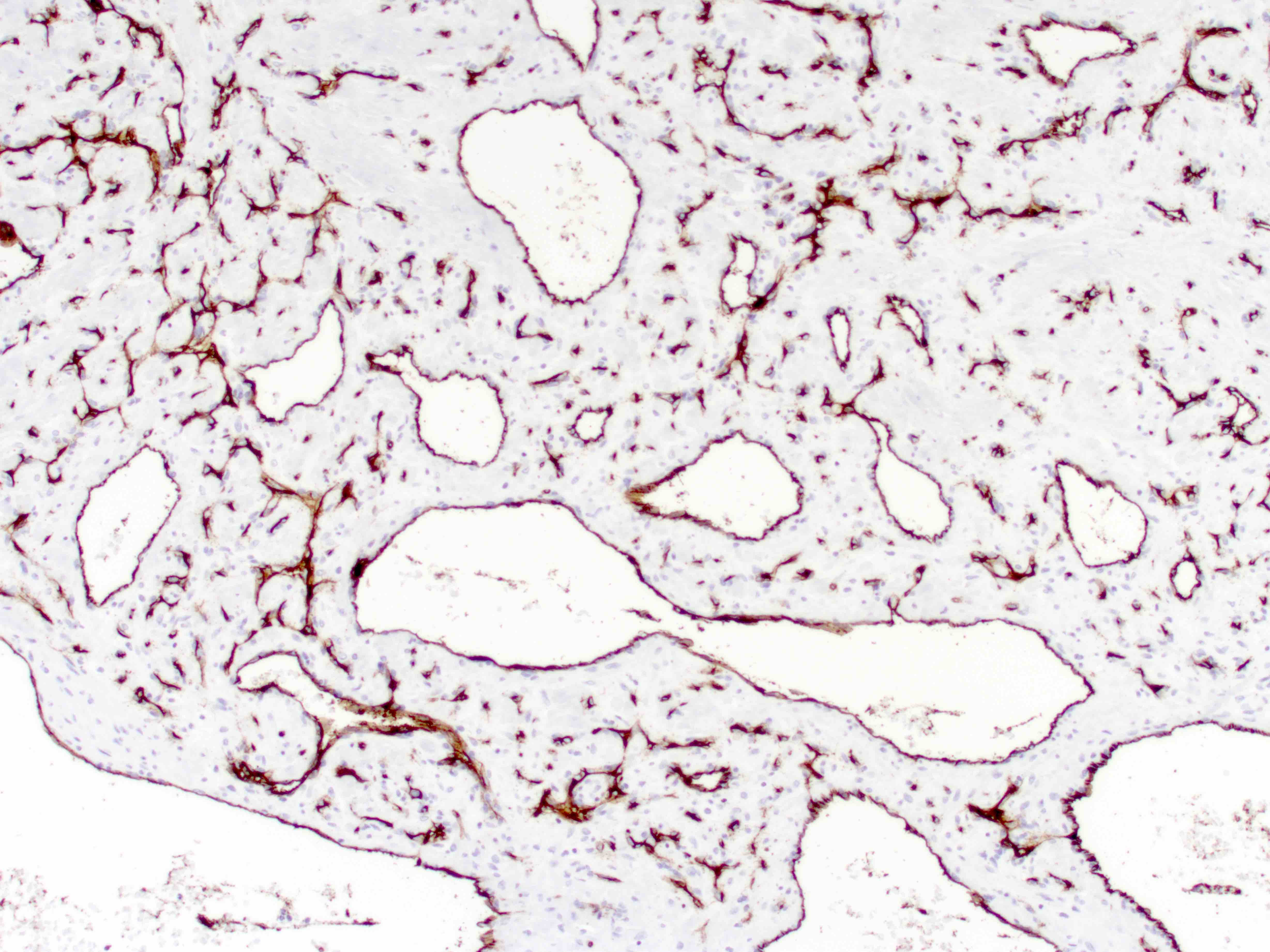
Multiple liver lesions (ranging from 0.5 to 3.5 cm) were incidentally identified on ultrasound of a 6 month old girl. A core biopsy was performed, which revealed a vascular neoplasm as illustrated in the micrograph (first image). The tumor cells are positive for CD34 (second image) and GLUT1 (third image) by immunohistochemistry. Which immunohistochemical stain is most characteristic for diagnosing this lesion?
- CD31
- CD34
- GLUT1
- HepPar1
Board review style answer #2
C. GLUT1. The microscopy shows a benign appearing vascular neoplasm. GLUT1 is strongly and diffusely positive in infantile hemangiomas and helps to exclude nonneoplastic vessels and vascular malformation as well as most of the other benign vascular neoplasms that do not express GLUT1. Answers A and B are incorrect because CD31 and CD34 are vascular markers that will be positive in all neoplastic or nonneoplastic vessels. Answer D is incorrect because HepPar1, a hepatocytic marker, is not helpful in characterizing a vascular lesion.
Comment Here
Reference: Hepatic infantile hemangioma
Comment Here
Reference: Hepatic infantile hemangioma