Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Sagan OA, Huber AR. Focal nodular hyperplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livertumorFNH.html. Accessed March 30th, 2025.
Definition / general
- Common, benign, nonneoplastic mass forming lesion of the liver
- Widely accepted to be a hyperplastic and regenerative response of hepatocytes to local vascular abnormalities (Visc Med 2020;36:292)
Essential features
- Benign, nonneoplastic hepatocellular mass lesion predominantly affecting women
- Majority are solitary and have a central scar on imaging and gross examination
- Classic histologic features include fibrous septa, nodules of hepatocytes, abnormal thick walled vessels, bile ductular reaction and chronic inflammation
- Glutamine synthetase demonstrates characteristic map-like staining by immunohistochemistry
Terminology
- Focal nodular hyperplasia (FNH)
- Has also been known as focal cirrhosis, pedunculated adenoma, solitary hyperplastic nodule, mixed adenoma, hamartoma and hamartomatous cholangiohepatoma (Autops Case Rep 2014;4:5)
ICD coding
- ICD-10: K76.89 - other specified diseases of liver
Epidemiology
- Second most common benign liver tumor, with the incidence being between 0.3 and 3%
- Female predominance (F:M = 9:1)
- Most commonly occurs in adults between 30 and 40 years of age but has also been reported in children and older adults
- Reference: Visc Med 2020;36:292
Pathophysiology
- Not fully understood but accepted as a hyperplastic and regenerative response of hepatocytes due to abnormal perfusion by local vascular malformations (Autops Case Rep 2014;4:5, Visc Med 2020;36:292)
Etiology
- Local vascular malformations that have been associated with FNH include hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease), Budd-Chiari syndrome and hepatic hemangiomas (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
- Increased estrogen (oral contraceptive use and pregnancy) is not required for lesion development (Autops Case Rep 2014;4:5)
Clinical features
- Patients are typically asymptomatic and many lesions are diagnosed incidentally on imaging or at autopsy (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
- Patients with large lesions can experience vague symptoms, including abdominal discomfort or pain (Visc Med 2020;36:292)
- Enlargement of the lesion can occur with oral contraceptive use and pregnancy (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
Diagnosis
- Diagnosis is typically made on imaging
- Biopsy may be needed to rule out malignancy with noncharacteristic imaging
Laboratory
- Patients may have mild elevations in liver transaminases along with alkaline phosphatase and gamma glutamyl transpeptidase (GGT) but these are not diagnostic (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
Radiology description
- Solitary, well circumscribed, unencapsulated and lobulated mass (Radiographics 2022;42:1043)
- Has variable echogenicity on ultrasound, so computed tomography (CT) and magnetic resonance imaging (MRI) may be preferred (Cureus 2020;12:e6813)
- Color and power Doppler ultrasound improve visualization by demonstrating the central feeding artery and characteristic spoke wheel pattern of branching vessels in the radiating septa (Radiographics 2022;42:1043)
Prognostic factors
- Overall excellent prognosis
- No evidence for malignant transformation (Visc Med 2020;36:292)
- Rupture, bleeding or necrosis is rare (Visc Med 2020;36:292)
- Larger and more symptomatic lesions have been observed among patients taking oral contraceptives (Autops Case Rep 2014;4:5)
Case reports
- 3 year old girl with a right sided abdominal mass (Proc (Bayl Univ Med Cent) 2018;31:97)
- 30 year old man with liver lesion concerning for hepatocellular carcinoma (Diagnostics (Basel) 2021;12:44)
- 33 year old woman with a liver lesion within an accessory lobe (Medicine (Baltimore) 2020;99:e21357)
- 43 year old man with acute abdominal pain due to hepatic tumor rupture (Front Oncol 2022;12:873338)
- 44 year old woman using oral contraceptives with liver mass (Am J Case Rep 2019;20:1124)
- 89 year old man with past medical history of kidney cancer and growing liver lesion (Clin J Gastroenterol 2020;13:413)
Treatment
- If a definitive diagnosis of FNH is made through imaging or biopsy, no long term follow up is necessary
- Patients can be reimaged after 6 months to confirm stability of the lesion
- Surgery should be reserved for symptomatic patients or highly suspicious lesions where malignancy cannot be excluded
- Transcatheter arterial embolization (TAE) has been successful in patients with large FNH where surgery would be high risk
- Reference: Visc Med 2020;36:292
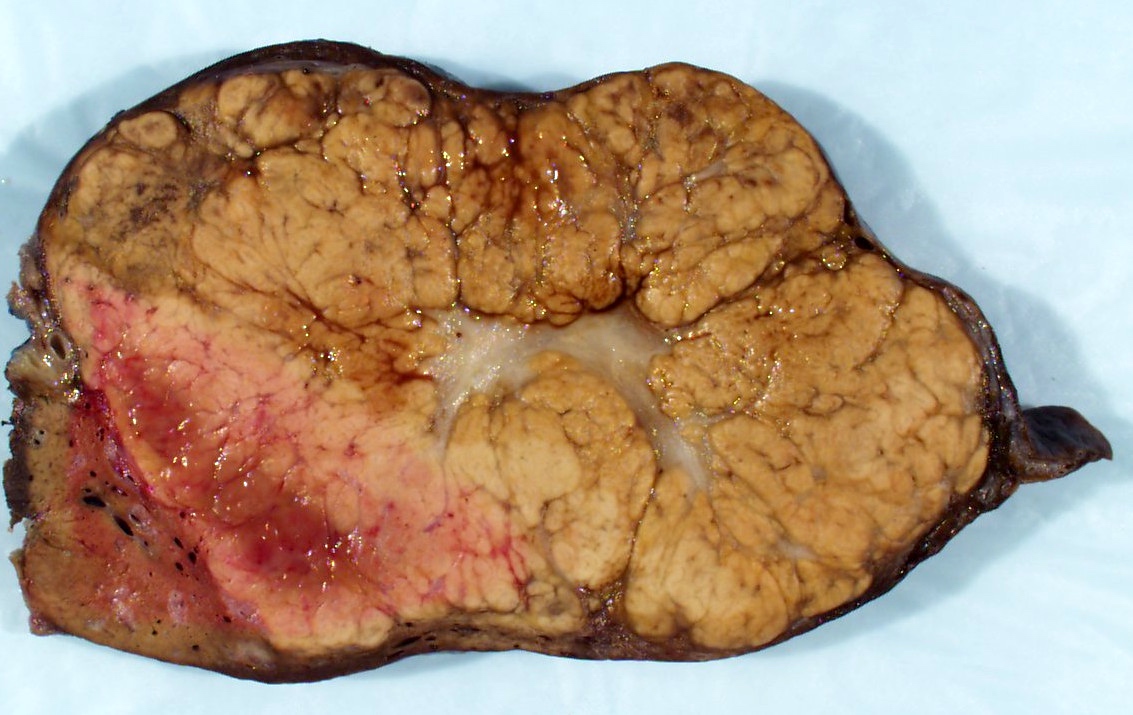
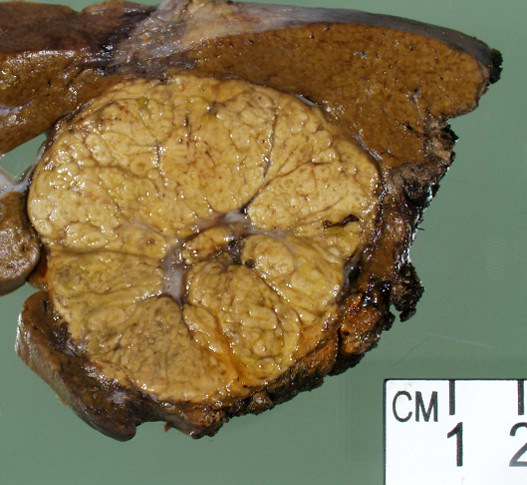
Gross description
- Well defined, nonencapsulated, lobulated and firm lesion, slightly lighter in color than the surrounding parenchyma (Visc Med 2020;36:292)
- Most commonly a solitary lesion (~66% of cases) (Liver Int 2009;29:459, Clin Liver Dis (Hoboken) 2021;17:244)
- Characteristic central, stellate fibrovascular zone (also described as a central scar, fibrous scar or scar-like fibrosis), which occurs in up to ~60% of lesions (Autops Case Rep 2014;4:5, Clin Liver Dis (Hoboken) 2021;17:244)
- Lesions typically measure between 4 and 8 cm but can measure up to 20 cm in greatest dimension (Autops Case Rep 2014;4:5)
- Can be associated with other lesions, including hemangiomas and hepatocellular adenomas (Visc Med 2020;36:292)
- Pedunculated forms are very rare (J Clin Med 2023;12:6034)
Gross images
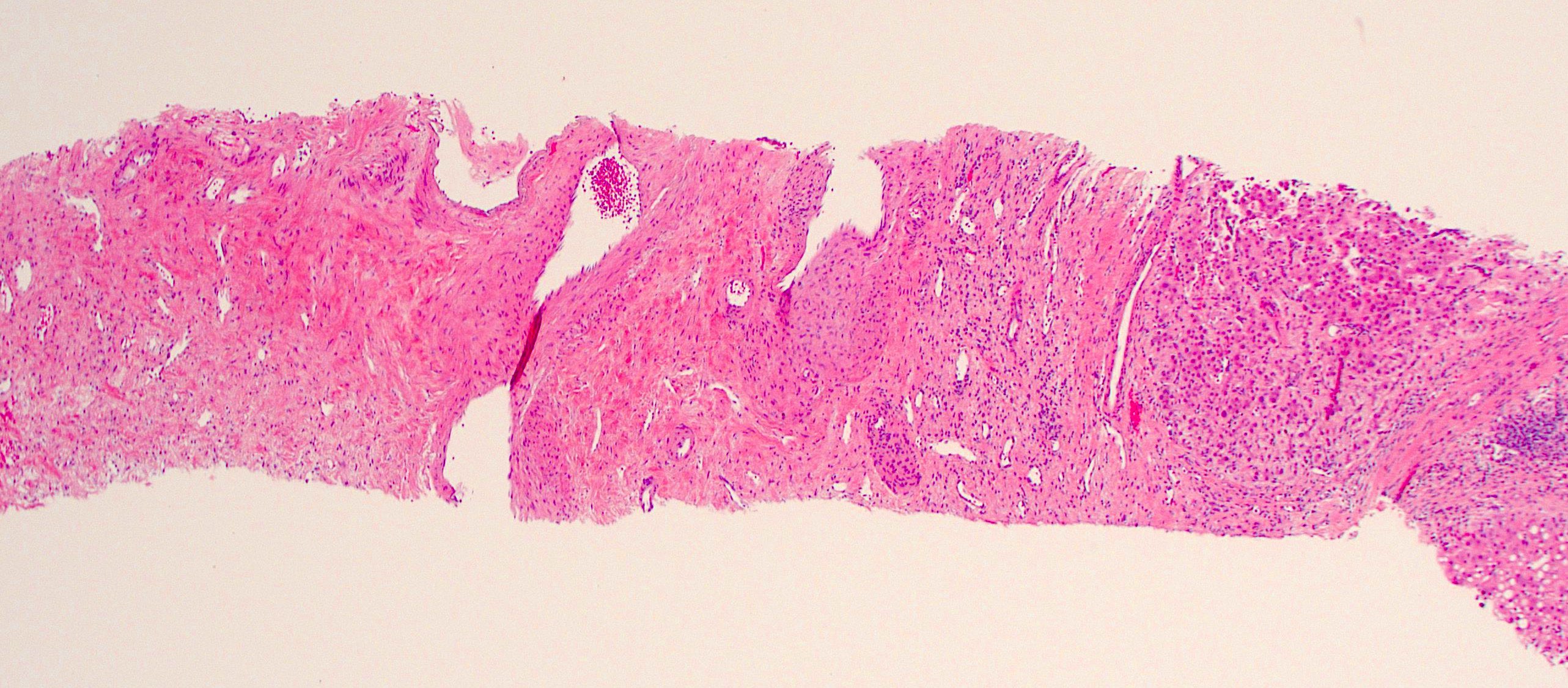
Frozen section description
- Occasionally seen during frozen sections for transplant evaluation, often as a small subcapsular nodule
- It is important to distinguish the presence of FNH from cirrhosis in these cases since the fibrous bands surrounding benign hepatocytes will be focal and not diffuse
- Reference: UPMC: Donor Allograft Frozen Sections [Accessed 24 January 2024]
Frozen section images
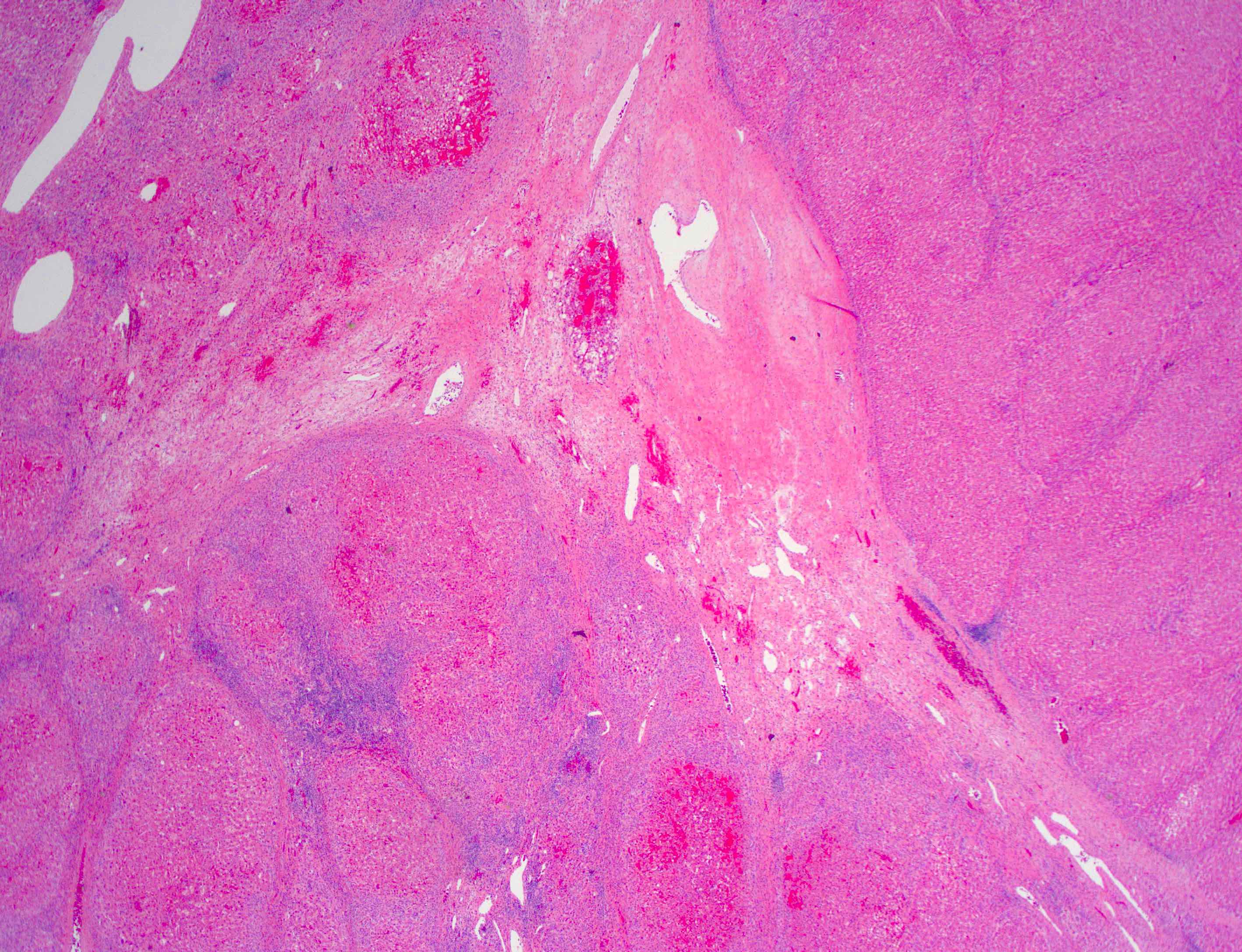
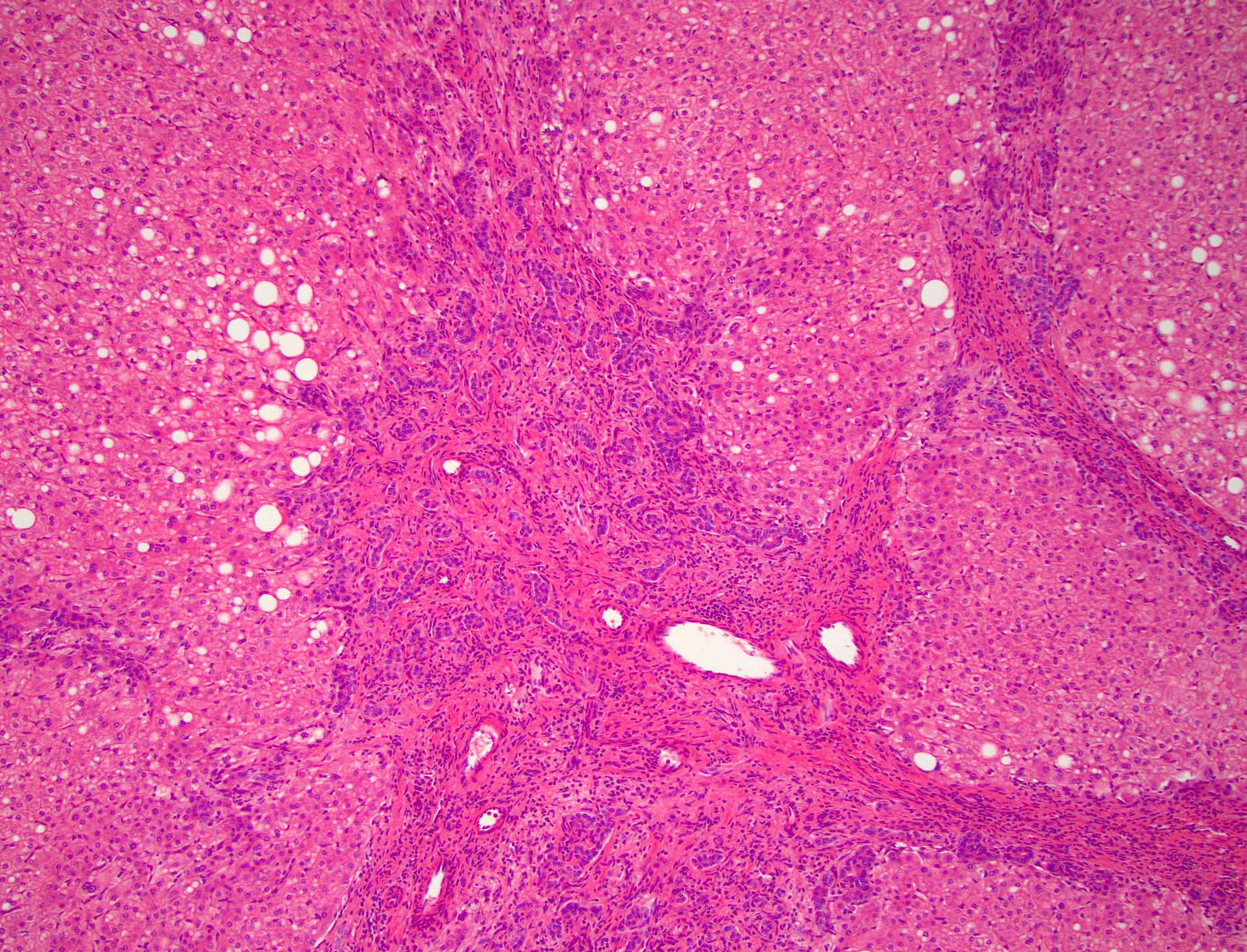
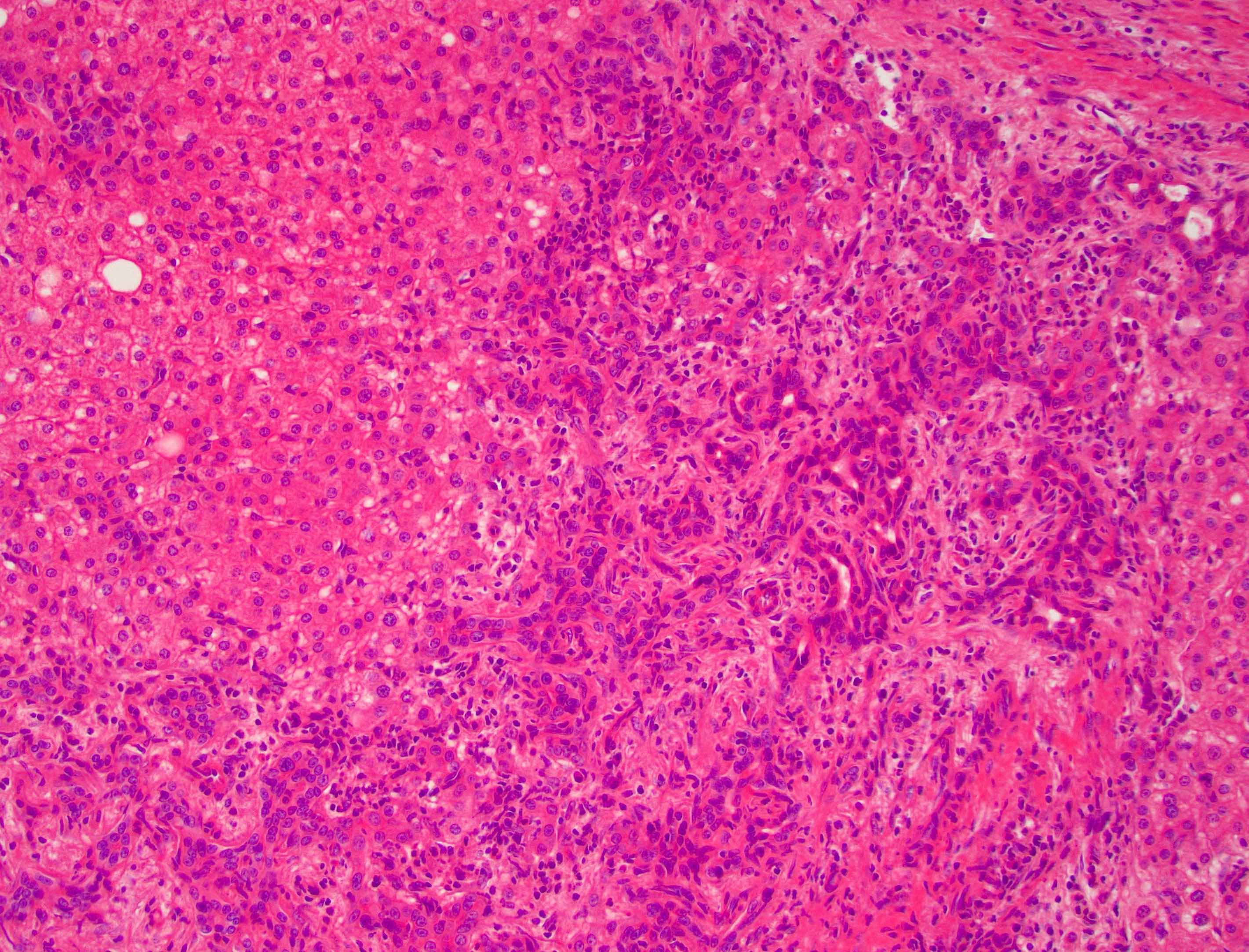
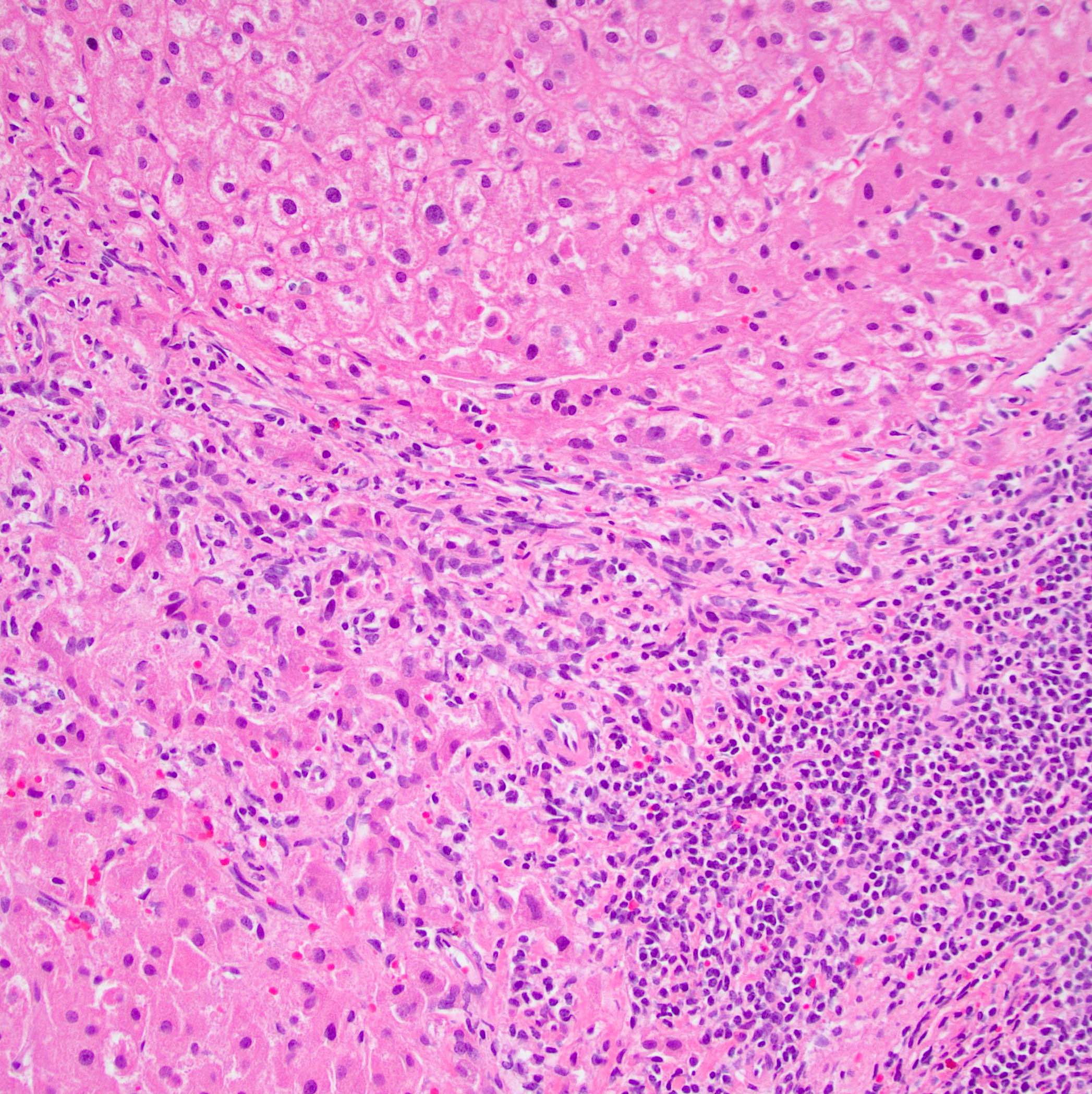
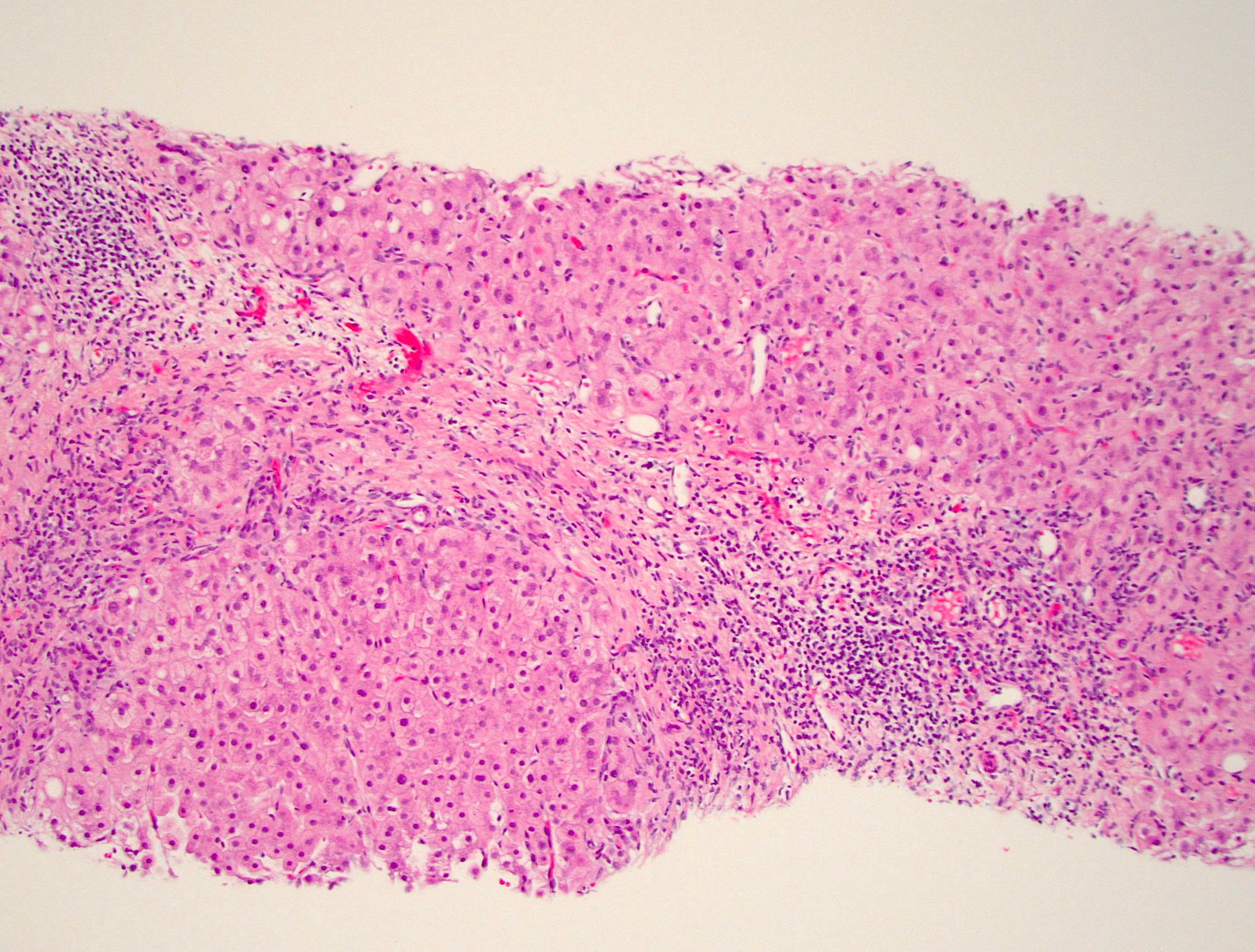
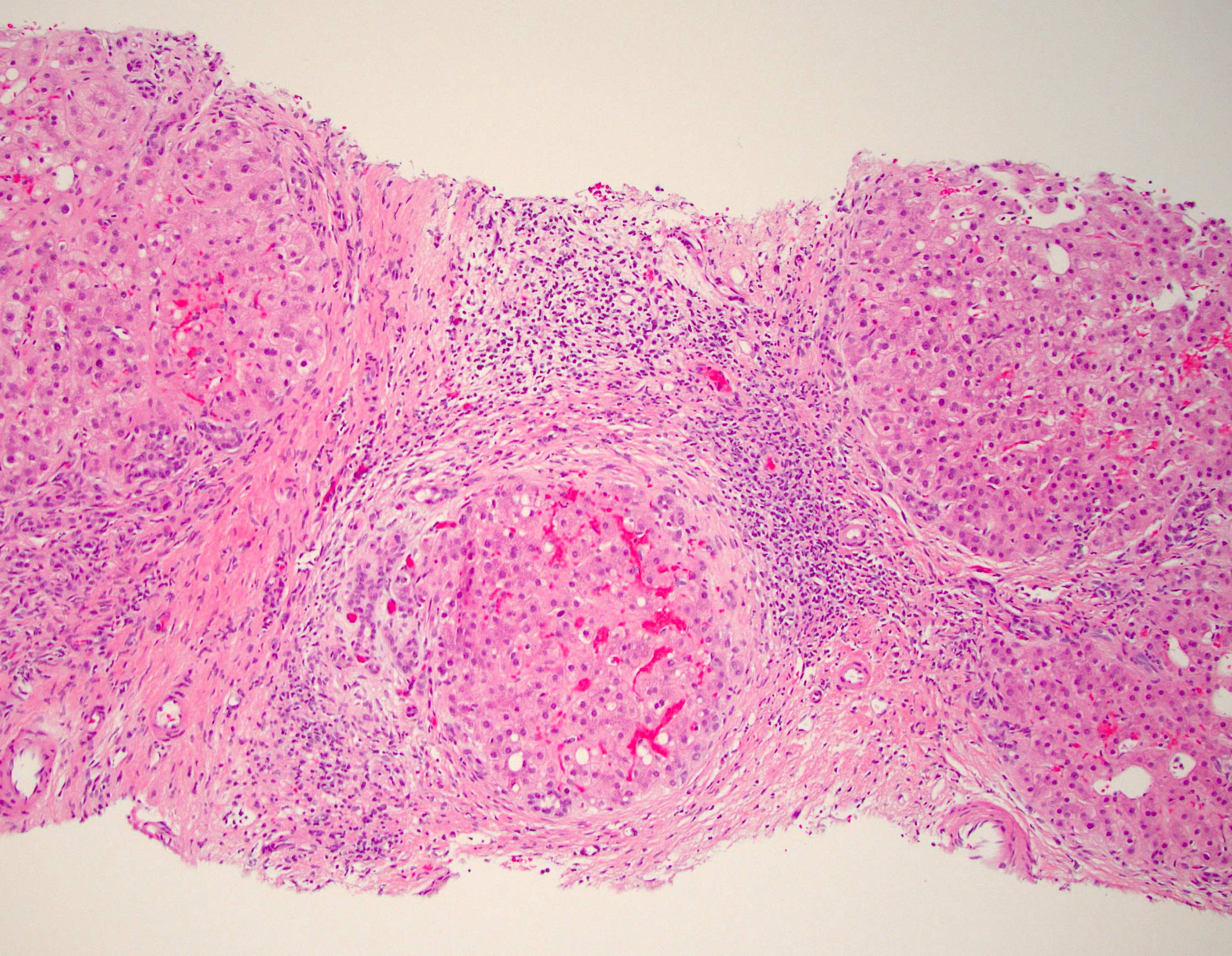
Microscopic (histologic) description
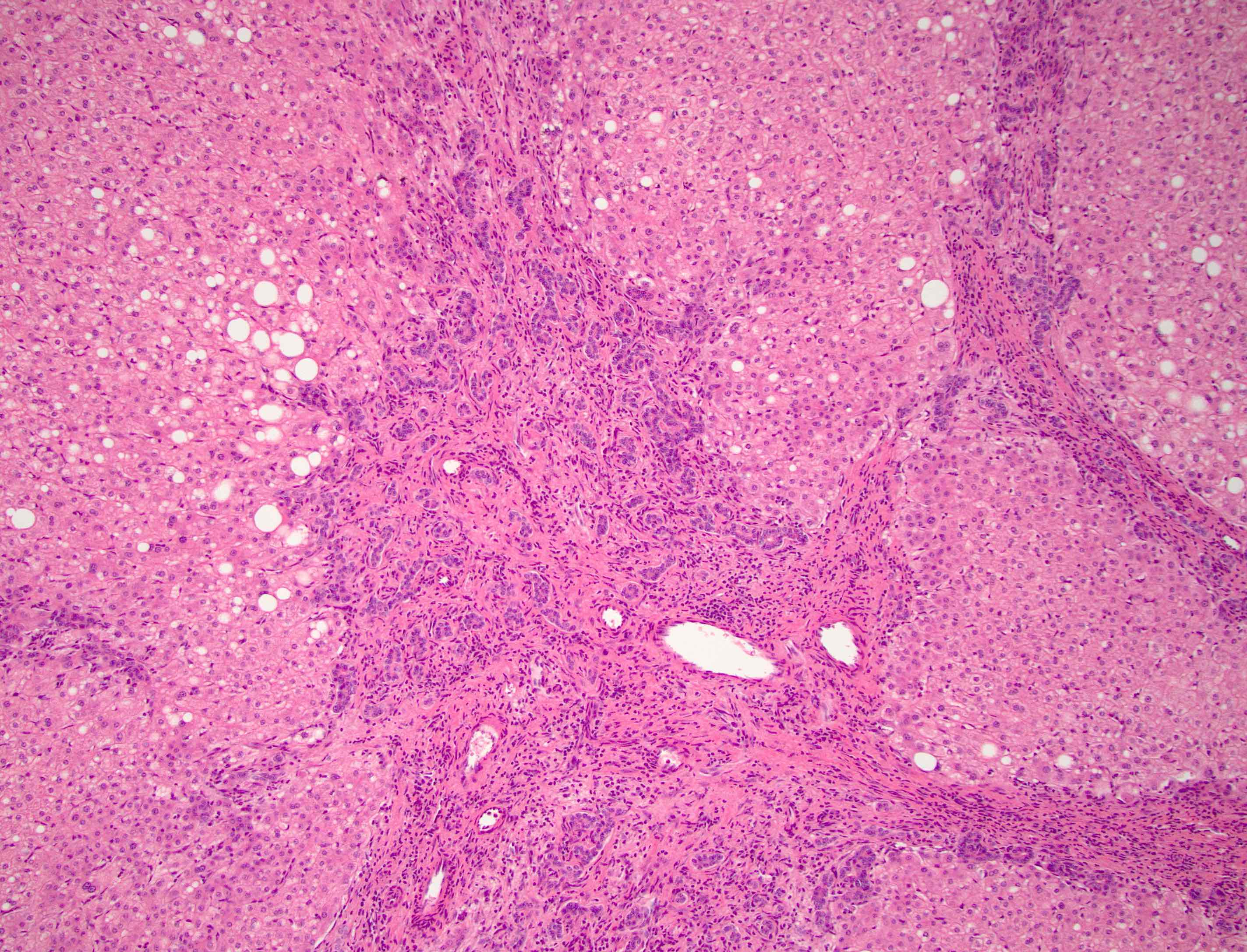
- Classically described as focal cirrhosis since FNH has fibrous bands separating the liver into nodules but is only focal, limited to the mass lesion and not diffuse (Visc Med 2020;36:292)
- Nodules of hepatocytes are formed by fibrous septa, which may coalesce into a central scar that characteristically contains abnormally thick walled vessels, which may demonstrate fibromuscular hyperplasia, myxomatous change or myointimal hyperplasia (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
- Fibrous septa also contain a bile ductular reaction and an inflammatory cell infiltrate (Visc Med 2020;36:292, Autops Case Rep 2014;4:5)
- Features of cholestasis, including feathery degeneration of hepatocytes and Mallory-Denk bodies, may be present
- Hepatocytes are cytologically bland and are arranged in plates 1 - 2 cells thick (Autops Case Rep 2014;4:5)
- Clues to the diagnosis on biopsy material include proliferating ductules at the junction of the fibrous bands and hepatocellular nodules, fibrous septa (thick or thin bands), large abnormal arteries and cholate stasis (Hum Pathol 2005;36:1210)
Microscopic (histologic) images
Cytology description
- Bland appearing hepatocytes, arranged as single cells to trabeculae of 2 - 3 cells thick
- Bile duct epithelium of cuboidal to columnar cells with nuclear palisading can be present
- Stromal elements may also be present
- It is important that only the lesion (and not the surrounding parenchyma) is sampled in order to make an accurate diagnosis
- Reference: World J Surg Oncol 2004;2:5
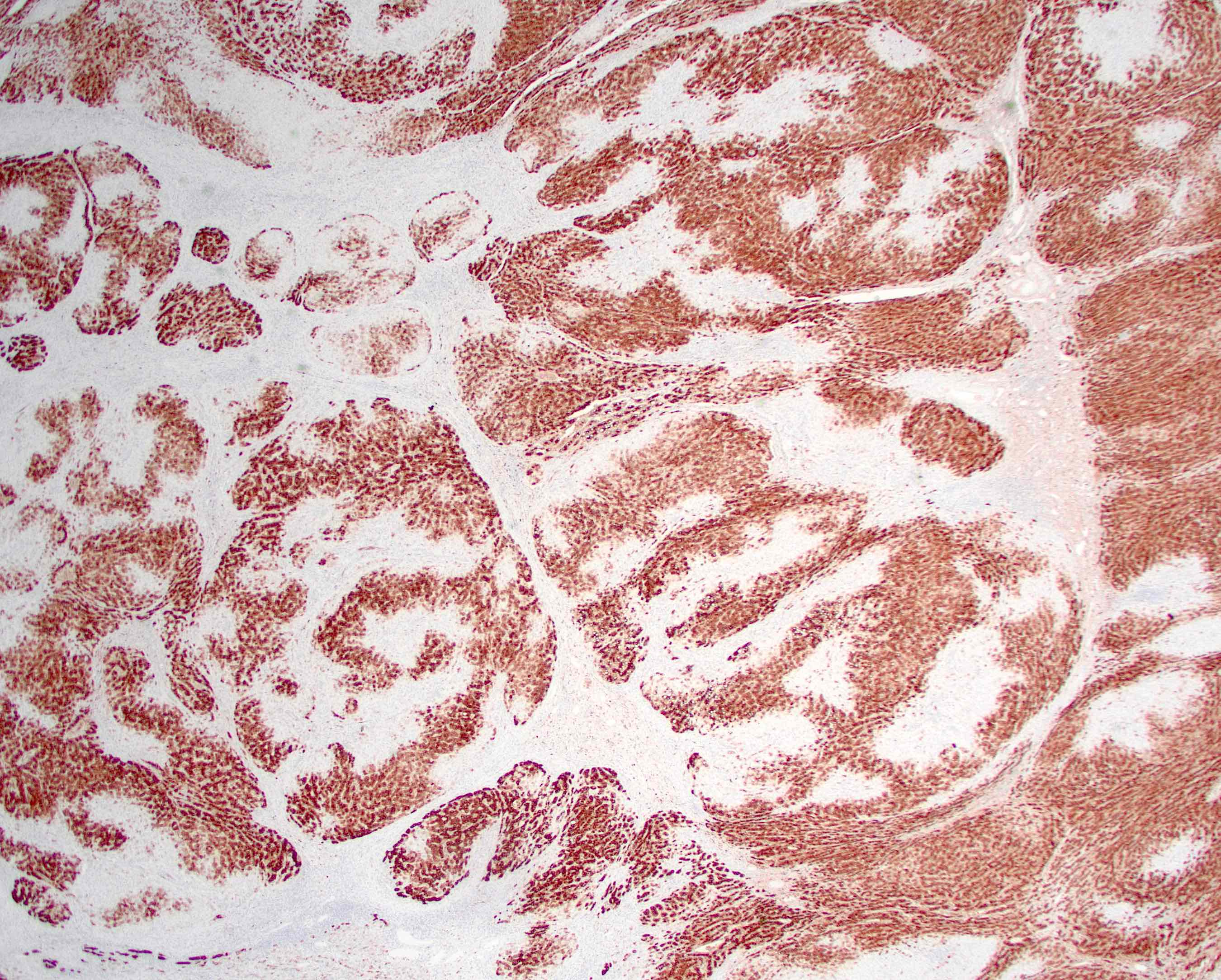
Positive stains
- Glutamine synthetase: strong, patchy, map-like pattern is highly specific (J Clin Med 2023;12:6034, Histopathology 2021;79:791, Liver Int 2009;29:459)
- Trichrome: fibrous bands surrounding nodules of hepatocytes (World J Hepatol 2014;6:580, Hum Pathol 2005;36:1210)
- CK7 and CK19: positive in the ductular reaction
- CK7 will also highlight periportal cholestatic hepatocytes (Hum Pathol 2005;36:1210)
- HepPar1 and arginase1: benign hepatocyte nodules (Lab Invest 2008;88:78, Am J Surg Pathol 2010;34:1147)
- Reticulin: retained framework without loss or thickened cell plates (Visc Med 2020;36:292)
- CD34: vascular structures and spaces, expression decreases further away from the septa (Hum Pathol 2005;36:1210)
Molecular / cytogenetics description
- Increased expression levels of ANGPT1 and ANGPT2 mRNA, which are associated with angiogenesis (Clin Mol Hepatol 2016;22:199)
- Beta catenin pathway is activated, including the downstream target, glutamine synthetase; however, no mutations in beta catenin have been described (Insights Imaging 2015;6:347)
Sample pathology report
- Liver, lesion, wedge resection:
- Focal nodular hyperplasia (see comment)
- Comment: This liver specimen shows a benign hepatocellular lesion with fibrous septa containing thick walled vessels, bile ductular reaction and mild chronic inflammation. CK7 highlights a ductular reaction in the fibrous bands. Glutamine synthetase demonstrates map-like staining. Beta catenin shows membranous staining without abnormal nuclear expression. The morphology and immunoprofile are compatible with a diagnosis of focal nodular hyperplasia.
Differential diagnosis
- Hepatocellular adenoma (Hepatology 2006;43:515, Ann Diagn Pathol 2019;38:126, Clin Liver Dis (Hoboken) 2021;17:244):
- Benign hepatocellular neoplasm
- Occurs in women of childbearing age
- Associated with oral contraceptive use
- By definition, occurs in noncirrhotic liver
- May progress to malignancy, unlike FNH, depending on subtype
- Histologically does not contain portal structures, is composed of benign hepatocytes with cell plates of normal thickness and has so called naked arteries scattered throughout the tumor
- Glutamine synthetase will not show the characteristic map-like positivity
- Fibrolamellar hepatocellular carcinoma (Surg Pathol Clin 2018;11:377):
- Malignant hepatocellular neoplasm with distinct clinicopathologic features
- Occurs in young people with no background liver disease
- Similar to FNH, fibrolamellar hepatocellular carcinoma may have a central scar on imaging and gross examination
- Histologically, fibrolamellar hepatocellular carcinoma is composed of nests or trabeculae of large oncocytic cells with abundant cytoplasm and nuclei with open chromatin and prominent nucleoli set within a collagenous background arranged in parallel bands
- CK7 and CD68 positive
- Glutamine synthetase will not show the characteristic map-like positivity
- Lastly, fibrolamellar hepatocellular carcinoma demonstrates a consistent DNAJB1::PRKACA fusion in 95% of cases, which is not seen in FNH
- Focal nodular hyperplasia-like (FNH-like) nodules (Comp Hepatol 2003;2:7, Radiol Clin North Am 2022;60:795, J Hepatol 2008;49:61, Hum Pathol 2023;142:20):
- FNH-like lesions or nodules have the histologic features of FNH but occur in the cirrhotic liver or in association with other diseases particularly Budd-Chiari syndrome
- FNH does not occur in the cirrhotic liver
- FNH-like changes next to another mass lesion (HPB (Oxford) 2002;4:135, Lamps: Diagnostic Pathology - Hepatobiliary and Pancreas, 2nd Edition, 2017):
- Can see fibrosis, ductular reaction, inflammation or cholestasis next to any mass lesion including malignancy
- Typically changes are focal, involving portion(s) of biopsy core(s)
- Glutamine synthetase staining is not map-like
- Hepatic hemangioma (Visc Med 2020;36:292):
- Most common benign liver tumor with an incidence up to 20%
- Occurs more commonly in women
- Typically, an incidental finding on imaging studies
- Most commonly solitary
- Composed entirely of vascular channels and may be of cavernous (most common), capillary or anastomosing types
- Lacks the bile ductular reaction, inflammation and hepatocyte nodules seen in FNH
- Will be most problematic on small biopsies that only sample the central scar of FNH; look carefully for the bile ductular reaction, inflammatory infiltrate and hepatocyte nodules
- Cirrhosis (Med Clin North Am 2022;106:437):
- Diffuse process that causes hepatic fibrosis leading to the formation of fibrous bands that separate the liver into nodules
- Histologic evidence or clinical history of liver disease
- No abnormal thick walled vessels and is not a focal lesion
- Glutamine synthetase will not show characteristic map-like positivity; however, be aware that inflammatory type hepatocellular adenomas can show a pseudo map-like pattern (about 10 - 15% of cases), which is challenging to interpret and a potential diagnostic pitfall
- Attention to morphology and serum amyloid A immunohistochemistry (which should be positive in adenoma and not in FNH) can help favor one over the other in such cases
- Some lesions may be indeterminate and a multidisciplinary approach may be needed to determine treatment strategy (Mod Pathol 2014;27:62)
Additional references
Board review style question #1
Board review style answer #1
D. Vascular malformations. The liver tumor shown in the picture depicts focal nodular hyperplasia (FNH). While the pathogenesis is unknown, it is generally accepted to be a hyperplastic reaction due to a vascular malformation, which makes answer D correct. Answers A and B are incorrect because there is no link between alcohol or hepatitis C and FNH, even though they can be tied to multiple other liver lesions. Answer C is incorrect because estrogen (typically through oral contraceptives or pregnancy) is not necessary for the development of FNH but has been found to influence the growth of the lesion.
Comment Here
Reference: Focal nodular hyperplasia
Comment Here
Reference: Focal nodular hyperplasia
Board review style question #2
Which of the following findings would be most diagnostic of focal nodular hyperplasia (FNH)?
- Arginase positivity
- CK7 positivity
- Glutamate synthetase strong map-like positivity
- Mutated beta catenin
Board review style answer #2
C. Glutamate synthetase strong map-like positivity. Strong map-like positivity of glutamate synthetase is highly specific for FNH. Answer A is incorrect because arginase positivity in FNH is not specific due to generally staining hepatocytes. Answer B is incorrect because the ductular reaction would be highlighted by CK7 but this is also not specific to FNH. Answer D is incorrect because beta catenin is only activated in FNH, not mutated.
Comment Here
Reference: Focal nodular hyperplasia
Comment Here
Reference: Focal nodular hyperplasia