Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Timing of disease recurrence | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Marins LV, Gonzalez RS. Recurrent disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverrecurrentdisease.html. Accessed April 2nd, 2025.
Definition / general
- Chronic liver disease can lead to a patient needing liver transplantation (LT)
- Some of these chronic diseases can recur following LT
Essential features
- Recurrent liver disease (RLD) may impact the long term health of the transplanted liver
- Diagnosis of recurrence is multidisciplinary
- Liver biopsy (LB) has a major role in the post-liver transplantation (LT) setting
- Recurrence of autoimmune diseases (e.g., autoimmune hepatitis [AIH] and primary biliary cholangitis [PBC]) is prevented by immunosuppression
- Recurrence of viral infections (e.g., hepatitis B and C) may be severe and progress rapidly
Terminology
- Recurrent hepatitis B (R-HBV)
- Recurrent hepatitis C (R-HCV)
- Recurrent autoimmune hepatitis (R-AIH)
- Recurrent primary sclerosing cholangitis (R-PSC)
- Recurrent primary biliary cholangitis (R-PBC)
- Recurrent alcoholic liver disease (R-ALD)
- Recurrent metabolic dysfunction associated steatotic liver disease (R-MASLD)
- Recurrent hepatocellular carcinoma (R-HCC)
ICD coding
- ICD-10
- Z94.4 - liver transplant status
- B18.1 - chronic viral hepatitis B without delta agent
- B18.2 - chronic viral hepatitis C
- K75.4 - autoimmune hepatitis
- K83.01 - primary sclerosing cholangitis
- K74.3 - primary biliary cirrhosis
- K70 - alcoholic liver disease
- K76.0 - fatty (change of) liver, not elsewhere classified
- C22.9 - malignant neoplasm of liver, not specified as primary or secondary
Epidemiology
- Recurrent disease only occurs in patients who initially have the diagnosis pre-liver transplantation (LT)
- Alloimmune hepatitis is a form of acute cellular rejection and can occur in patients without pre-LT autoimmune hepatitis (AIH)
Sites
- Liver
Pathophysiology
- Most chronic liver disease cannot be cured by removal of the affected native liver; the goal is to cure end stage liver disease / cirrhosis or fulminant acute hepatitis
- Brief overview of pathophysiologic mechanisms involved in recurrence
- Recurrent hepatitis B and recurrent hepatitis C: virus persists in the patient's bloodstream if not cured pre-liver transplantation (LT) (Best Pract Res Clin Gastroenterol 2020;46:101689)
- Recurrent autoimmune hepatitis, recurrent primary sclerosing cholangitis and recurrent primary biliary cholangitis: autoimmunity / inappropriately overactive immune system persists (Am J Clin Pathol 2021;155:435, Best Pract Res Clin Gastroenterol 2020;46:101688, Liver Transpl 2006;12:S73, Gastroenterology 2019;156:96)
- Recurrent alcoholic liver disease: alcohol consumption may resume secondary to several factors (Liver Transpl 2020;26:25, World J Gastroenterol 2018;24:2785)
- Recurrent metabolic dysfunction associated steatotic liver disease: metabolic dysfunction (obesity, diabetes, etc.) may persist if not appropriately addressed clinically (Best Pract Res Clin Gastroenterol 2020;46:101688)
- Recurrent hepatocellular carcinoma: aggressive disease (e.g., with lymphovascular invasion) is more likely to recur (World J Gastroenterol 2023;29:1243)
- Diseases that do not recur include alpha-1 antitrypsin deficiency (as the defect lies within native hepatocytes) and Wilson disease (as the defect lies within native hepatocytes)
- Role of liver transplantation (LT) in curing hereditary hemochromatosis remains uncertain (Clin Liver Dis 2014;18:675)
- One study reported no significant iron overload in liver biopsies after LT (Transplant Direct 2020;6:e560)
Etiology
- Recurrent hepatitis B: hepatitis B virus infection
- Recurrent hepatitis C: hepatitis C virus infection
- Recurrent autoimmune hepatitis: autoimmune mediated inflammatory liver disease
- Recurrent primary sclerosing cholangitis: underlying causes not completely understood (immune dysregulation, vascular abnormalities, environmental factors)
- Recurrent primary biliary cholangitis: autoimmune mediated inflammatory liver disease
- Recurrent alcoholic liver disease: excessive alcohol intake
- Recurrent metabolic dysfunction associated steatotic liver disease: obesity, insulin resistance, hypertension or dyslipidemia
- Recurrent hepatocellular carcinoma: remaining cancer cells or de novo carcinogenesis
- References: Am J Gastroenterol 2006;101:1370, Transpl Int 2008;21:459
Timing of disease recurrence
- Timing of recurrent liver disease (RLD) varies among different studies
- In addition to factors such as the original disease, immunosuppression scheme and epidemiologic factors, variables such as length of follow up and performance of protocol biopsies impact the determination of the timing of disease recurrence
- RLD can occur at any time in the allograft but each RLD has an average onset and a median time to graft loss (see table below)
- Recurrent hepatitis C
- ~50% of patients remain asymptomatic during the first 12 months post-LT
- Most patients will show histologic features of hepatitis
- Success of HCV treatment has changed the epidemiology of liver transplantation (decline of HCV liver transplants) and correlates with improved graft survival (Transplant Direct 2019;5:e427)
- Recurrent autoimmune hepatitis
- More common in children (Clin Liver Dis 2017;21:381)
- Recurrent alcoholic liver disease
- Although there is no consensus about definition of harmful drinking post-LT, abusive drinking is less common after LT (about 10% of patients)
Average onset of recurrent diseases and median time to graft loss (Transpl Int 2008;21:459)
| Recurrent disease | Average onset | Median time to graft loss in days (years) |
| Recurrent hepatitis B | 1 - 1.5 years | 717 days (~2 years) |
| Recurrent hepatitis C | First hours and days | 1429 days (~4 years) |
| Recurrent autoimmune hepatitis | > 1 year | 525 days (~1.5 years) |
| Recurrent primary sclerosing cholangitis | 2 - 3 years | 1342 days (~4 years) |
| Recurrent primary biliary cholangitis | 2 - 5 years | 2833 days (~8 years) |
| Recurrent alcoholic liver disease | 1 - 2 years | 2543 days (~7 years) |
| Recurrent metabolic dysfunction associated steatotic liver disease | 3 - 10 years | 1123 days (~3 years) |
| Recurrent hepatocellular carcinoma | 1 - 2 years | 581 days (~1.5 years) |
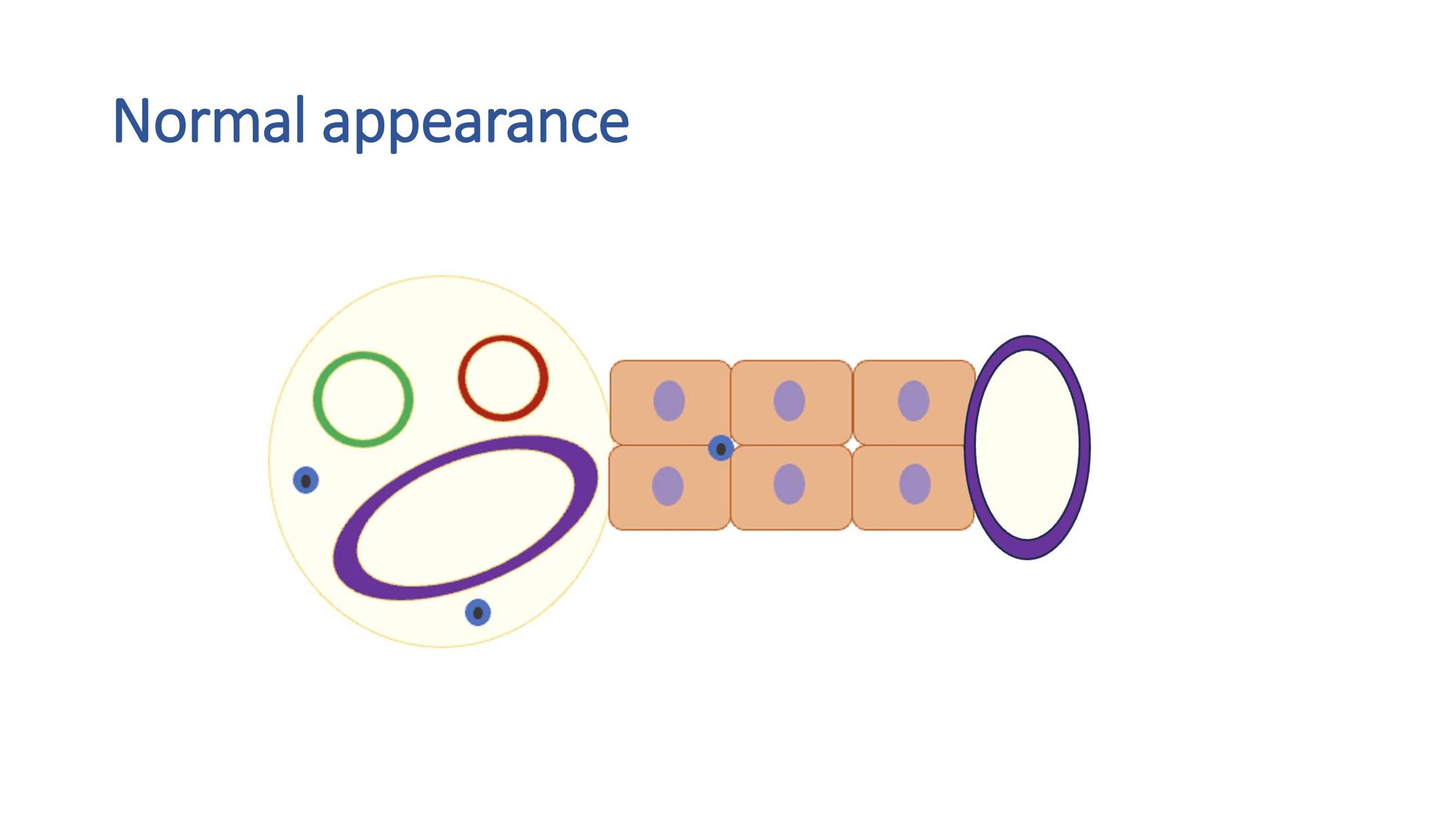
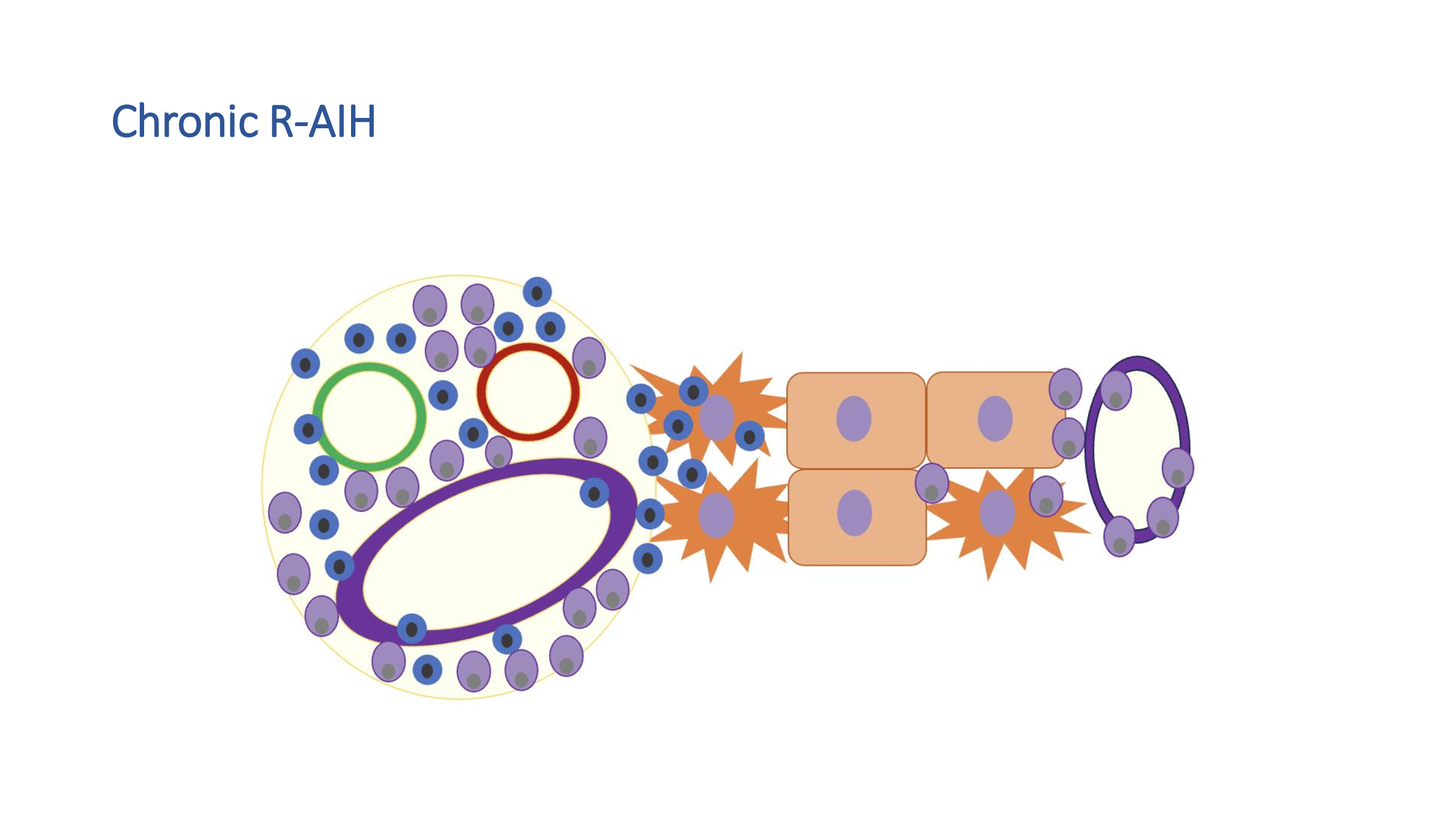
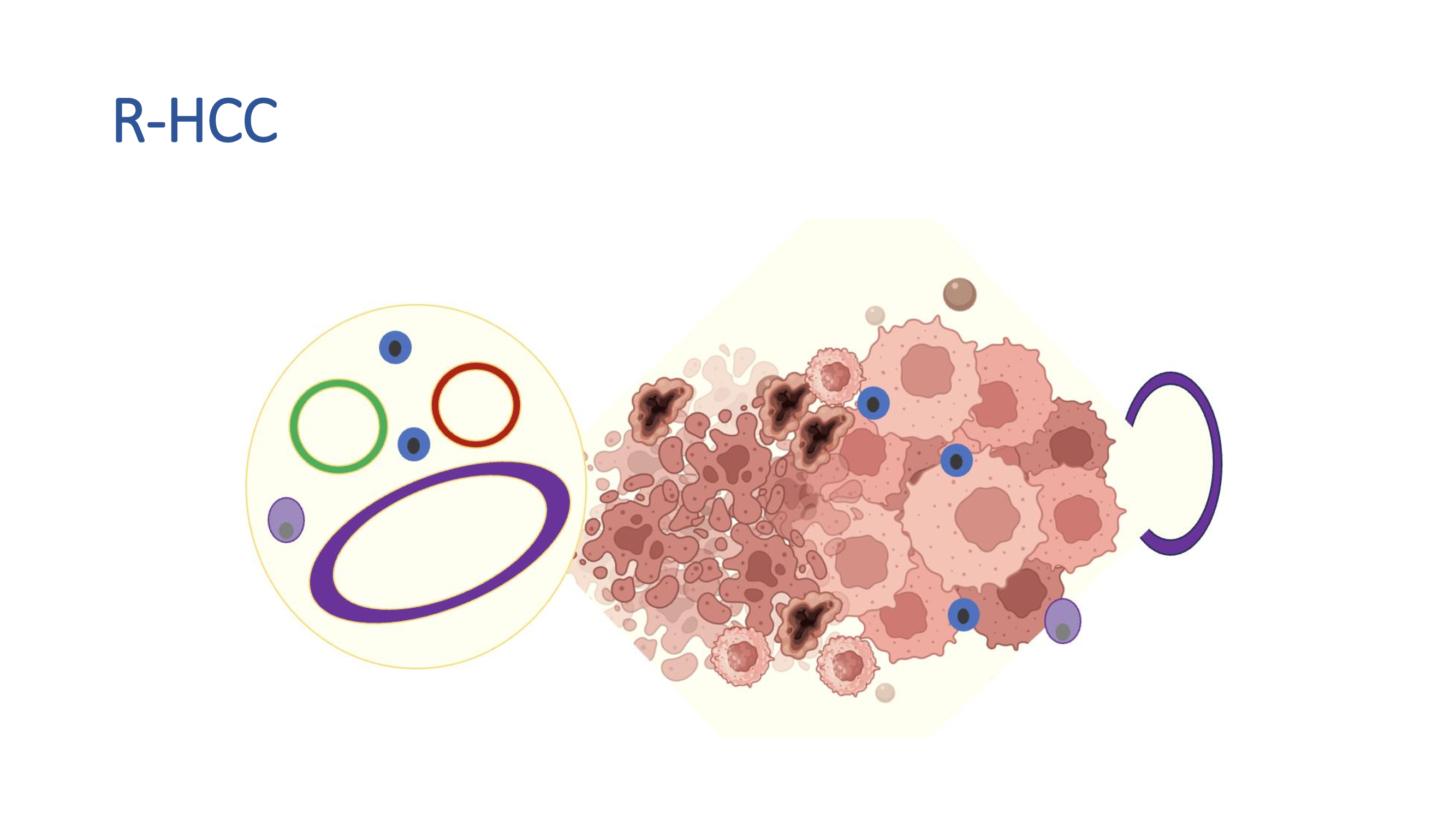
Diagrams / tables
Clinical features
- Patients may be asymptomatic
- Signs and symptoms: fatigue, jaundice, pruritus, abdominal pain, hepatomegaly
- Patients with primary sclerosing cholangitis (PSC) may present with concomitant inflammatory bowel disease (IBD), especially ulcerative colitis (UC)
- Important to investigate alcohol consumption and all medications, herbs and supplements the patient is taking
- Specific recurrent liver disease (RLD) diagnosis, genetic profile and immunosuppression status are some of the factors that determine recurrence
- In some studies, RLD accounts for 19% of deaths following LT (Ann Hepatol 2012;11:415)
Diagnosis
- Diagnosis is multidisciplinary, involving (Am J Gastroenterol 2006;101:1370, Best Pract Res Clin Gastroenterol 2020;46:101688, World J Gastroenterol 2014;20:10668)
- Clinical features (as above)
- Laboratory results for liver function (see the Laboratory section below)
- Most common biochemical profiles: cholestatic, hepatocellular and mixed cholestatic / hepatocellular
- Each disease has a more specific profile
- Imaging techniques
- Radiologic features may be nonspecific
- Imaging may show hepatomegaly, steatosis, strictures or dilation of bile ducts, fibrosis
- Liver biopsy
- Helps integrate all information and deliver a definitive diagnosis
- May identify more than one cause of graft damage
- Histologic features of recurrent autoimmune hepatitis may precede clinical and biochemical alterations
Laboratory
- Liver function assessment includes
- Liver enzyme tests: alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP) and gamma glutamyl transferase (GGT)
- Total bilirubin, direct bilirubin, indirect bilirubin and albumin
- Prothrombin time and complete blood count
- Depending on the pretransplant disease and clinical suspicion of recurrence, additional laboratory tests may be performed
- Recurrent hepatitis B (World J Hepatol 2018;10:352, JHEP Rep 2023;5:100728)
- HBV DNA quantification in serum
- Serum hepatitis antigens (HBsAg, HBeAg, HBcAg, others)
- Recurrent hepatitis C (Ann Gastroenterol 2013;26:304, Nat Rev Gastroenterol Hepatol 2014;11:710)
- HCV RNA quantification in serum
- Recurrent autoimmune hepatitis (Clin Liver Dis 2017;21:381, World J Transplant 2022;12:59)
- There is no specific marker for diagnosis
- The International Autoimmune Hepatitis Group criteria, developed in the nontransplant setting, is also applied post-liver transplantation (LT) (Liver Transpl 2001;7:285, J Hepatol 2022;77:84)
- Increased aspartate aminotransferase (AST) and alanine aminotransferase (ALT)
- Hypergammaglobulinemia, particularly elevated IgG
- Diagnostic utility of autoantibody testing (e.g., anti-smooth muscle antibodies [ASMA]) is considered uncertain
- Patients transplanted for AIH may have positive autoantibodies with no other abnormalities
- Patients transplanted for non-AIH etiologies can develop autoantibodies after LT
- Recurrent primary sclerosing cholangitis (Transplant Direct 2017;3:e334)
- Autoantibodies such as antinuclear antibodies (ANA) and ASMA may help, although they are not specific to PSC
- Assessment of IBD / UC related markers: antineutrophil cytoplasmic antibodies (ANCA) positivity, elevated levels of C reactive protein (CPR), elevated levels of fecal calprotectin, abnormal colonoscopy
- Recurrent primary biliary cholangitis (Gastroenterology 2019;156:96, Best Pract Res Clin Gastroenterol 2020;46:101688)
- Autoantibodies such as antimitochondrial antibodies (AMA), particularly the AMA M2 subtype
- Hypergammaglobulinemia, particularly elevated IgM
- Recurrent alcoholic liver disease (World J Gastroenterol 2018;24:2785, Liver Transpl 2020;26:25)
- Increased AST, ALT, GGT, ethyl glucuronide, serum carbohydrate deficient transferrin and bilirubin, thrombocytopenia and decreased serum albumin
- Recurrent metabolic dysfunction associated steatotic liver disease (Best Pract Res Clin Gastroenterol 2020;46:101688)
- Total cholesterol, low density lipoprotein cholesterol (LDL C), high density lipoprotein cholesterol (HDL C), triglycerides, fasting blood glucose and insulin
- Recurrent hepatocellular carcinoma (World J Gastroenterol 2023;29:1243)
- Elevated alpha fetoprotein (AFP), although not specific, may indicate HCC recurrence
- Elevated des-gamma-carboxy prothrombin can be used in conjunction with AFP for monitoring
Radiology description
- Recurrent hepatitis C, recurrent hepatitis B, recurrent autoimmune hepatitis (World J Gastroenterol 2014;20:6180)
- Radiologic features may be nonspecific
- Imaging may show hepatomegaly, steatosis and fibrosis
- Recurrent primary sclerosing cholangitis, recurrent primary biliary cholangitis (Transpl Int 2021;34:1455)
- Magnetic resonance cholangiopancreatography or endoscopic retrograde cholangiopancreatography can evaluate the bile ducts
- Imaging may show multifocal nonanastomotic biliary strictures and dilation of intrahepatic and extrahepatic bile ducts
- Recurrent alcoholic liver disease, recurrent metabolic dysfunction associated steatotic liver disease (World J Gastroenterol 2014;20:6180)
- Imaging may show features of steatosis, hepatomegaly and fibrosis
- Recurrent hepatocellular carcinoma (World J Gastroenterol 2014;20:6180)
- Tumors can be identified through characteristic enhancement patterns on CT
- MRI with hepatospecific contrast: detection and characterization of focal lesions; useful in determining whether a lesion is of hepatocellular origin or not
- Contrast enhanced ultrasound (CEUS): real time assessment of tumor vascularity and differentiation between benign and malignant liver lesions
- PET: metabolic activity within liver lesions
Prognostic factors
- Ranges in the recurrence frequency (R%) between different studies may be influenced by variables such as length of follow up and performance of protocol biopsies (routine procedure instead of event driven biopsy)
- Recurrent hepatitis C (Transplant Direct 2019;5:e427)
- R%: > 90% over 5 years (Am J Gastroenterol 2006;101:1370)
- HCV recurrence is considered universal in patients with pretransplant viremia
- Time of histologic recurrence in the liver allograft is variable (Transplantation 2004;77:210)
- Risk factors: female sex, African American recipient, HIV coinfection, ILB28 genotype, HCV genotype 1b, high viral load, older donor age, prolonged cold ischemia, acute rejection treatment, cytomegalovirus (CMV) hepatitis (Transplant Proc 2014;46:3100)
- Recurrent hepatitis B
- R%: < 5% with prophylaxis over 5 years (Am J Gastroenterol 2006;101:1370)
- Effective prophylactic protocols and potent antiviral drugs improve the control of infection (World J Gastroenterol 2020;26:2166)
- Risk factors: pretransplant HCC, HCC recurrence, serum HBV DNA ≥ 105 copies/mL, hepatitis B e antigen (HBeAg) positivity, hepatitis B immune globulin (HBIG) monoprophylaxis (Chin Med J (Engl) 2021;134:2388)
- Recurrent autoimmune hepatitis
- R%: 16.6 - 41% over 5 years (Liver Int 2011;31:291)
- Risk factors: high grade inflammation in native liver, female recipient, younger age at liver transplantation (LT), recipient HLA-DR3 serotype, suboptimal immunosuppression, use of mycophenolate mofetil post-LT, higher IgG level pre-LT (J Hepatol 2022;77:84, Aliment Pharmacol Ther 2017;45:485)
- Recurrent primary sclerosing cholangitis
- R%: 10 - 38.7% over 5 years (Liver Int 2011;31:291)
- Risk factors: CMV infection, colectomy before LT, cholangiocarcinoma before LT, multiple episodes of acute cellular rejection, bacteria in bile culture, active UC post-LT (Aliment Pharmacol Ther 2019;49:636, Transplant Direct 2017;3:e334)
- Recurrent primary biliary cholangitis
- R%: 10.9 - 35% over 5 years (Liver Int 2011;31:291)
- Risk factors: suboptimal immunosuppression, male recipient, younger or older age at LT, high IgM level before LT, use of tacrolimus post-LT (Best Pract Res Clin Gastroenterol 2017;31:187)
- Recurrent alcoholic liver disease
- R%: 3 - 43.70% over 5 years (World J Gastroenterol 2018;24:2785)
- Risk factors: anxiety, depression, illicit drug use, lack of social support, short pre-LT duration of sobriety (World J Gastroenterol 2018;24:2785)
- Recurrent metabolic dysfunction associated steatotic liver disease
- R%: 11 - 38% over 5 years (Am J Gastroenterol 2006;101:1370)
- Risk factors: hypertension, diabetes, obesity, prolonged corticotherapy for other concomitant disease (Clin Mol Hepatol 2023;29:S286)
- Recurrent hepatocellular carcinoma
- R%: 8 - 15% over 5 years (Ann Transplant 2022;27:e934924)
- Risk factors: poorly differentiated tumors, vascular invasion, high concentration of calcineurin inhibitors, prolonged corticotherapy, donor age > 60 years, prolonged cold (≥ 10 hours) or warm (≥ 50 minutes) ischemia times (Ann Transplant 2022;27:e934924)
Case reports
- 12 year old girl with posttransplant recurrence of primary sclerosing cholangitis (PSC) treated with vancomycin (Case Rep Transplant 2013;2013:314292)
- 41 year old man with posttransplant recurrence of \hepatitis B (HBV) and HDV (Transplant Proc 2017;49:175)
- 45 and 56 year old men with refractory recurrent autoimmune hepatitis (AIH) after liver transplantation (Transplant Proc 2014;46:298)
- 77 year old man with recurrent hepatocellular carcinoma 15 years after transplantation (Exp Clin Transplant 2007;5:713)
Treatment
- For all recurrent liver diseases (RLD) (especially autoimmune diseases): adjustments in immunosuppressive therapy and avoidance or dose adjustment of hepatotoxic medications
- Recurrent hepatitis B and recurrent hepatitis C (Transplant Direct 2019;5:e427)
- Treatment is complex and must follow guidelines (Clin Infect Dis 2018;67:1477, Clin Infect Dis 2023 May 25 [Epub ahead of print])
- It is important to differentiate recurrence from new viral infection
- Viral genotypes and therapeutic failures in the pretransplant phase are helpful information
- Avoiding excessive immunosuppression is necessary
- Antiviral therapy involves different classes of medications
- Recurrent hepatitis C
- Pegylated interferon and ribavirin (Transplant Proc 2014;46:3100)
- Triple therapy with protease inhibitors after liver transplantation (LT) has efficacy to 60 - 70% of sustained viral response (Transplant Proc 2014;46:3100)
- Direct acting antiviral therapy has been well tolerated but there is risk of immune mediated graft dysfunction, hepatitis B (HBV) reactivation and interactions with immunosuppressant drugs
- Recurrent hepatitis B: HBIG and nucleos(t)ide analogues (entecavir, tenofovir disoproxil fumarate and tenofovir alafenamide)
- Recurrent hepatitis C
- Recurrent autoimmune hepatitis
- Increasing immunosuppressive doses is sufficient in mild cases
- Corticosteroids and azathioprine may be required in moderate / severe cases (World J Transplant 2022;12:59)
- Recurrent primary sclerosing cholangitis, recurrent primary biliary cholangitis: endoscopic therapy (balloon dilation or stent placement to manage strictures and bile duct complications), ursodeoxycholic acid, alternative immunosuppressive regimens, antibiotic prophylaxis to prevent bacterial cholangitis (Best Pract Res Clin Gastroenterol 2020;46:101688, Liver Transpl 2006;12:S73, Gastroenterology 2019;156:96)
- Recurrent alcoholic liver disease: abstinence from alcohol, management of associated complications, supportive care (World J Hepatol 2017;9:771, World J Gastroenterol 2018;24:2785, Liver Transpl 2020;26:25)
- Recurrent metabolic dysfunction associated steatotic liver disease: lifestyle modifications (healthy diet, regular exercise, avoidance of alcohol), prescription of medications to manage metabolic risk factors (dyslipidemia, hypertension, diabetes) (Best Pract Res Clin Gastroenterol 2020;46:101688)
- Role of bariatric surgery is debatable (Clin Mol Hepatol 2023;29:S286)
- Recurrent hepatocellular carcinoma: surgical resection, locoregional therapies (radiofrequency ablation, transarterial chemoembolization, radioembolization), systemic therapies (sorafenib, lenvatinib, immune checkpoint inhibitors), participation in clinical trials, supportive care (World J Gastroenterol 2023;29:1243)
- If all other measures fail, the patient may be considered for liver retransplantation
Microscopic (histologic) description
- Recurrent hepatitis C (World J Gastroenterol 2014;20:2810, Liver Transpl 2009;15:S35)
- Acute hepatitis (< 6 months post-liver transplantation [LT]): lobular disarray, focal necrosis, acidophil bodies, sinusoidal lymphocytosis, hepatocellular ballooning, steatosis (mild to severe, usually macrovesicular)
- Acute HCV is rarely biopsied outside the post-LT setting
- Chronic hepatitis (> 6 months post-LT): lymphocytic inflammation in portal tracts (small and nonactivated lymphocytes, lymphoid aggregates, lymphocytic infiltration of bile ducts), variable interface activity (usually mild to moderate), variable lobular activity (irregular trabecular pattern, focal necrosis, acidophil bodies), steatosis (mild to severe, usually macrovesicular)
- Steatosis is a common histologic feature of chronic hepatitis C (Gut 2006;55:123)
- Grading and staging system: Ishak or METAVIR (not developed for recurrent disease but may be used as reference)
- Atypical histologic manifestations
- Fibrosing cholestatic hepatitis (FCH): severe bile duct injury, bile duct loss, ductular reaction, bile plugs within bile duct lumens, cholestasis, lymphocytic inflammation in portal tracts, interface hepatitis, lobular activity, hepatocellular ballooning, variable steatosis and periportal and perisinusoidal fibrosis, often with bridging fibrosis
- Hepatitis C with autoimmune features: portal and lobular inflammatory infiltrates rich in plasma cells, central perivenulitis
- Hepatitis C with granulomas: compact, usually small and nonnecrotizing granulomas in portal tracts
- Acute hepatitis (< 6 months post-liver transplantation [LT]): lobular disarray, focal necrosis, acidophil bodies, sinusoidal lymphocytosis, hepatocellular ballooning, steatosis (mild to severe, usually macrovesicular)
- Recurrent hepatitis B (Liver Transpl 2006;12:S50)
- Acute hepatitis (< 6 months post-LT): mild to moderate lobular disarray, focal necrosis, acidophil bodies, ground glass hepatocytes
- Chronic hepatitis (> 6 months post-LT): lymphocytic inflammation in portal tracts with variable interface activity, variable lobular disarray, focal necrosis, acidophil bodies, ground glass hepatocytes
- Grading and staging systems: Ishak or METAVIR (not developed for recurrent disease but may be used as reference)
- Atypical histologic manifestations
- FCH: hepatocellular ballooning, steatosis, cholestasis, ground glass hepatocytes, bile duct injury, ductular reaction and periportal and perisinusoidal fibrosis, often with bridging fibrosis
- Recurrent autoimmune hepatitis (Am J Clin Pathol 2021;155:435)
- Acute recurrent autoimmune hepatitis: moderate to severe lobular disarray, necrosis, regeneration, acidophil bodies
- Chronic recurrent autoimmune hepatitis: lymphocytic inflammation in portal tracts including plasma cells, interface activity (moderate to severe), lobular activity with necrosis or central perivenulitis (in severe cases, there is confluent / bridging necrosis)
- Grading and staging system: Ishak (not developed for recurrent disease but may be used as reference)
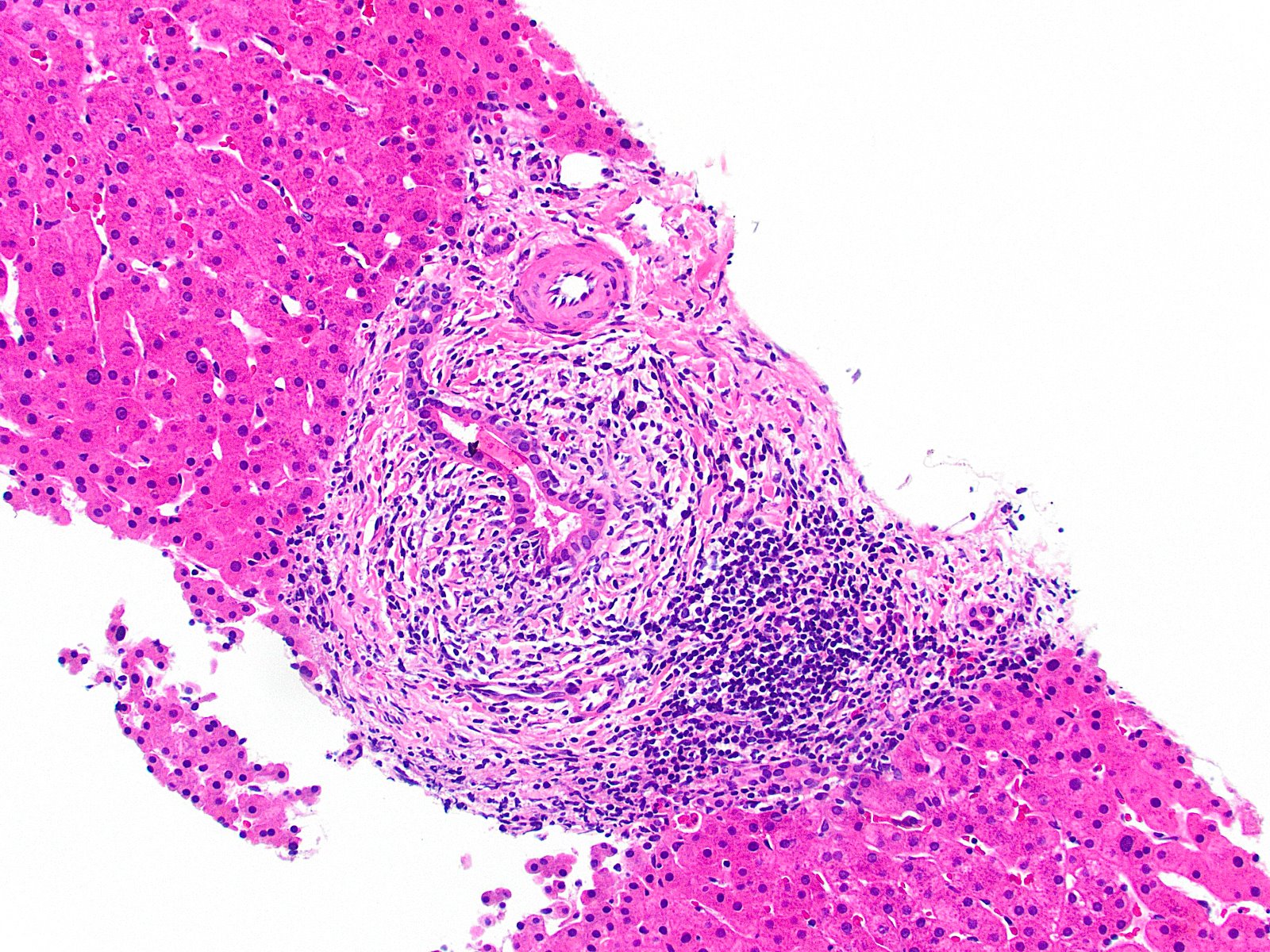
- Recurrent primary sclerosing cholangitis (Liver Transpl 2006;12:S73, Best Pract Res Clin Gastroenterol 2020;46:101688)
- Biliary epithelial injury, periductal onion skin fibrosis, edema and inflammation in portal tracts, cholestasis, ductular reaction, ductopenia
- Grading and staging system: Scheuer or Nakanuma (not developed for recurrent disease but may be used as reference)
- Recurrent primary biliary cholangitis (Gastroenterology 2019;156:96, Best Pract Res Clin Gastroenterol 2020;46:101688)
- Lymphoplasmacytic infiltrate in portal tracts, interface activity (mild to moderate), florid duct lesions (lymphocytic cholangitis or granulomas in portal tracts), ductular reaction, ductopenia
- Grading and staging system: Scheuer or Nakanuma (not developed for recurrent disease but may be used as reference)
- Recurrent alcoholic liver disease (World J Gastroenterol 2018;24:2785, Liver Transpl 2020;26:25)
- Macrovesicular steatosis (mild, moderate or severe), hepatocellular ballooning, lobular inflammation (may contain prominent neutrophilic component), Mallory-Denk bodies, bile ductular reaction, cholestasis, perivenular / pericellular fibrosis
- Grading and staging system: Kleiner scoring, SALVE staging (not developed for recurrent disease but may be used as reference) (J Hepatol 2021;75:810)
- Recurrent metabolic dysfunction associated steatotic liver disease (Liver Transpl 2014;20:1064, Best Pract Res Clin Gastroenterol 2020;46:101688)
- Macrovesicular steatosis (mild, moderate or severe), hepatocellular ballooning, lobular inflammation, Mallory-Denk bodies, bile ductular reaction, perivenular / pericellular fibrosis
- Grading and staging system: NAFLD Activity Score (not developed for recurrent disease but may be used as reference) (Hepatology 2005;41:1313)
- Recurrent hepatocellular carcinoma (World J Gastroenterol 2023;29:1243)
- Malignant hepatocytes with cellular atypia, architectural irregularity and possibly vascular invasion
- Tumor grading: WHO and Edmondson-Steiner system
Microscopic (histologic) images
Positive stains
- Immunohistochemical studies do not generally help establish a diagnosis of recurrent liver disease (RLD)
- However, in the post-liver transplantation (LT) setting, they can be used for several purposes
- CMV, HSV, HBV stains evaluate infectious agents
- CK7 and CK19 highlight native bile ducts, aiding in the assessment of ductopenia and ductular reaction
- CK7 immunostaining in hepatocytes highlights ongoing hepatocyte injury and regeneration, particularly notable in chronic cholestatic diseases
- CK7 immunostaining may help diagnose recurrent primary biliary cholangitis (Hepatol Res 2020;50:478)
- HCC markers (e.g., HepPar1, arginase1) to confirm recurrence
Videos
Recurrent disease post-liver transplantation
Sample pathology report
- Liver, allograft, needle biopsy:
- Bile duct injury with periductal onion skin fibrosis and ductular reaction (see comment)
- Negative for acute cellular rejection
- Comment: The history of liver transplantation for primary sclerosing cholangitis (PSC) 3 years ago is noted. The histologic findings characterized by portal tract mixed inflammation, ductular reaction and bile duct injury exhibiting onion skin fibrosis favor a diagnosis of recurrent PSC. Imaging studies do not show stricture at the anastomosis site and Doppler evaluation demonstrates normal vascular flow.
- Liver, allograft, needle biopsy:
- Chronic hepatitis with mild interface activity, suggestive of recurrent disease (see comment)
- Indeterminate for acute T cell mediated rejection
- Comment: The history of liver transplantation for end stage liver disease secondary to hepatitis C virus and hepatocellular carcinoma 11 months ago is noted. Histologic sections show expansion of most of the portal tracts by an inflammatory infiltrate rich in mature lymphocytes with mild interface activity. The lobules show sparse necroinflammatory foci with rare acidophil bodies. Eosinophils, ductitis and endotheliitis are not seen. These findings are suggestive of recurrent chronic HCV related hepatitis with mild activity. The findings are not definitive for acute T cell mediated rejection.
Differential diagnosis
- Newly acquired viral infections (hepatitis A, hepatitis B, hepatitis C, hepatitis E, CMV, Epstein-Barr virus (EBV), herpes simplex virus (HSV) types 1 and 2, arboviruses and others) (Best Pract Res Clin Gastroenterol 2020;46:101689):
- Liver transplantation (LT) patients are immunocompromised, raising the likelihood of subsequent infection
- These mainly enter the differential diagnosis for acute recurrent hepatitis C, acute recurrent hepatitis B and acute recurrent autoimmune hepatitis
- Histologic findings may be similar
- Travel history, socioepidemiological factors and serological tests can provide valuable insights
- Favoring HAV (hepatitis A virus), HEV (hepatitis E virus) and arboviruses: histology may show discrete / moderate findings (spotty necrosis and few / many apoptotic bodies) or severe alterations (massive hepatocellular necrosis) (Eur J Gastroenterol Hepatol 2020;32:916, Case Rep Transplant 2021;2021:5159934)
- Favoring HCV: steatosis and hepatocellular ballooning (World J Gastroenterol 2014;20:2810)
- Favoring HBV: ground glass hepatocytes (Liver Transpl 2006;12:S50)
- Favoring CMV: reactive bile duct changes, lobular microabscesses, sinusoidal inflammatory infiltrate, CMV inclusions (Transpl Infect Dis 2006;8:21)
- Favoring EBV: sinusoidal lymphocytosis (mostly B cells), portal infiltrate with immunoblasts and eosinophils (Hum Pathol 1993;24:1306)
- Favoring HSV: geographic necrosis and nuclear inclusions
- Drug induced liver injury (DILI) (Liver Transpl 2020;26:1167):
- Considered a differential diagnosis for all recurrent liver diseases (RLD)
- Can mimic all major histologic patterns of liver injury
- Excluded by a detailed investigation of medications taken by the patient
- Association between DILI and RLD can occur
- More easily diagnosed when the drug injury and the RLD have different histologic patterns of injury
- Some RLD have specific further differential diagnoses
- Recurrent hepatitis B and recurrent hepatitis C (World J Gastroenterol 2014;20:2810):
- Acute recurrent hepatitis B / recurrent hepatitis C versus acute T cell mediated rejection (TCMR):
- Clinical features, laboratory tests and timing of biopsy do not help to differentiate TCMR from acute recurrent hepatitis C but accurate diagnosis is crucial
- Mild acute TCMR is not a major concern because it is not treated in most transplant centers
- Detection of moderate / severe acute TCMR is important because it requires modification in the immunosuppressive regimen and may exacerbate recurrent hepatitis B / recurrent hepatitis C
- Histologic findings are similar in both conditions: lymphocytes and eosinophils in the portal tracts, bile duct injury, endotheliitis
- Favoring acute TCMR
- Portal based injury
- Activated and blastic lymphocytes, more prominent bile duct injury / ductitis, more prominent endotheliitis and many eosinophils in the inflammatory infiltrate
- Important to meet the criteria for at least moderate acute rejection
- Favoring acute recurrent hepatitis B / recurrent hepatitis C
- Lobular based injury
- Lobular inflammation, hepatocyte ballooning, steatosis, apoptotic bodies
- Favoring acute TCMR
- Clinical features, laboratory tests and timing of biopsy do not help to differentiate TCMR from acute recurrent hepatitis C but accurate diagnosis is crucial
- Chronic recurrent hepatitis B / recurrent hepatitis C versus fibrosing cholestatic hepatitis (FCH) versus mechanical biliary stricture:
- Histologic findings may be similar
- Favoring chronic recurrent hepatitis B / recurrent hepatitis C
- Portal based mononuclear inflammatory infiltrate, mild to moderate interface hepatitis, lobular inflammation, discrete ductular reaction, mild steatosis
- Favoring mechanical biliary stricture
- Prominent ductular reaction, mixed portal inflammatory infiltrate and bile plugs in bile duct lumina
- Imaging studies may provide additional assistance
- Favoring FCH
- Prominent ductular reaction, mixed portal inflammatory infiltrate in the portal tracts, intense lobular disarray, hepatocyte ballooning, steatosis, pericellular fibrosis
- High viral RNA levels
- Chronic recurrent hepatitis B / recurrent hepatitis C with plasma cell rich infiltrate:
- Resembles autoimmune hepatitis (AIH)
- May represent an alloimmune response (especially if the patient has a previous history of interferon treatment)
- Acute recurrent hepatitis B / recurrent hepatitis C versus acute T cell mediated rejection (TCMR):
- Recurrent autoimmune hepatitis (Am J Clin Pathol 2021;155:435):
- Acute TCMR:
- This dilemma is less critical, since increased immunosuppression is required in both conditions
- Favoring recurrent autoimmune hepatitis
- Prominent lobular inflammation and extensive lobular necrosis
- Acute TCMR:
- Recurrent primary sclerosing cholangitis (Liver Transpl 2006;12:S68):
- Chronic ductopenic rejection (CR):
- Favoring recurrent primary sclerosing cholangitis
- Concentric onion skin periductal fibrosis, fibrotic scars in the portal tracts
- Favoring CR
- Lack of ductular reaction, senescent changes in bile ducts, foam cell arteriopathy
- Favoring recurrent primary sclerosing cholangitis
- Complications related to biliary anastomosis and ischemic cholangitis:
- Histologic findings are similar
- Imaging studies may provide additional assistance
- Favoring recurrent primary sclerosing cholangitis
- Nonanastomotic structures, > 90 days post-LT
- Chronic ductopenic rejection (CR):
- Recurrent primary biliary cholangitis (Best Pract Res Clin Gastroenterol 2020;46:101688):
- CR:
- Recurrent primary biliary cholangitis and CR may both demonstrate ductopenia and chronic cholestasis
- Favoring recurrent primary biliary cholangitis
- Lymphocytic or granulomatous cholangitis
- Lobular chronic inflammation
- Favoring CR
- Lack of ductular reaction, senescent changes in bile ducts, foam cell arteriopathy
- Infectious granulomatous diseases:
- Favoring infection
- Large granulomas with necrosis
- Favoring infection
- CR:
- Recurrent alcoholic liver disease and recurrent metabolic dysfunction associated steatotic liver disease (Liver Transpl 2020;26:25, World J Gastroenterol 2018;24:2785, Best Pract Res Clin Gastroenterol 2020;46:101688):
- These 2 diseases share toxic metabolic pathways causing liver dysfunction and one can simulate the other
- Favoring recurrent alcoholic liver disease
- Ductular reaction, cholestasis, abundant Mallory-Denk bodies
- Recurrent hepatocellular carcinoma (World J Gastroenterol 2023;29:1243):
- De novo development of new hepatocellular carcinoma
- Important to verify the histologic subtype of hepatocellular carcinoma and tumor grade in the native liver
- Different histologic subtype suggests de novo hepatocellular carcinoma
- Important to verify the histologic subtype of hepatocellular carcinoma and tumor grade in the native liver
- De novo development of new hepatocellular carcinoma
Additional references
Board review style question #1
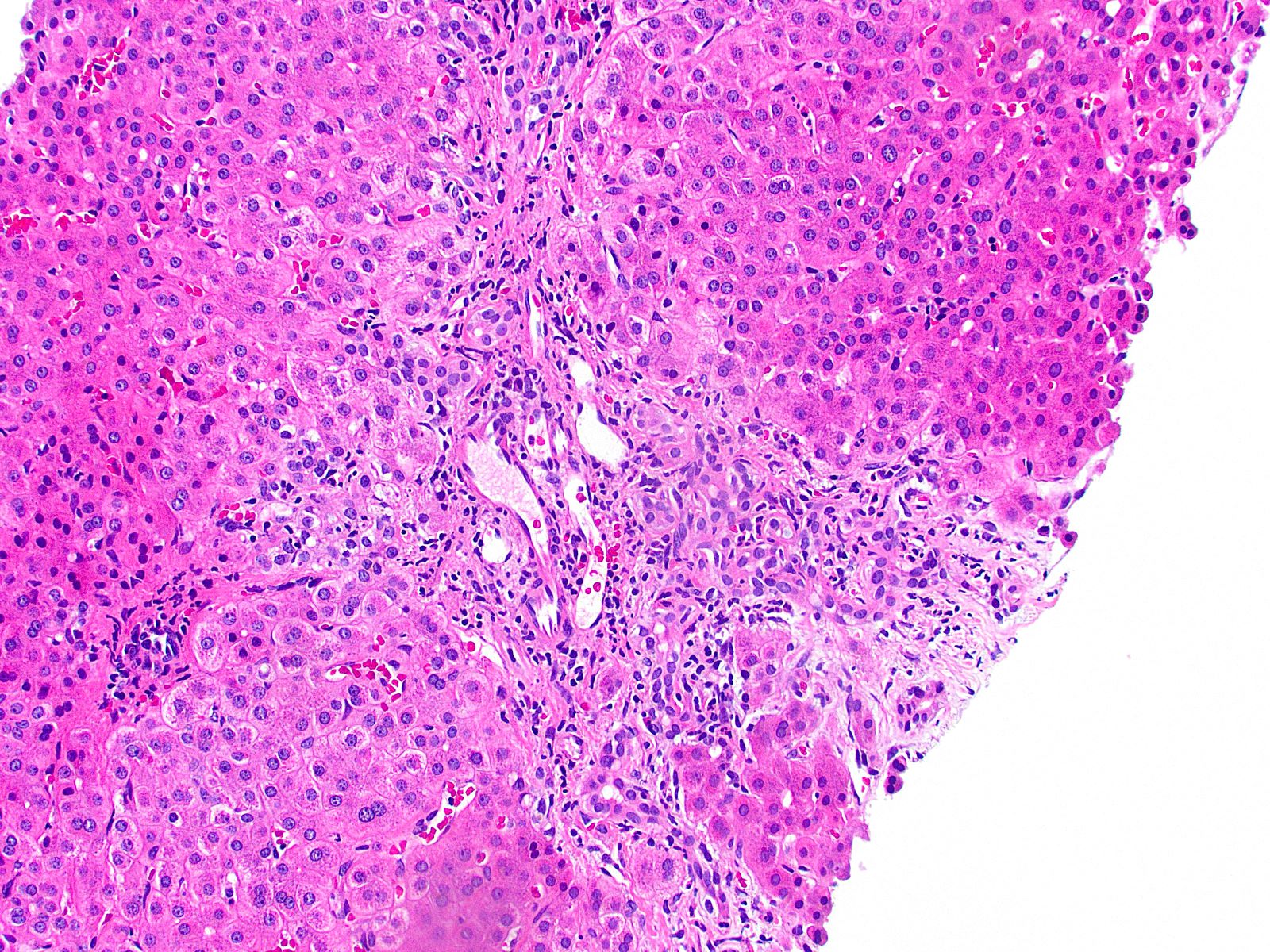
A 55 year old man with a history of chronic alcohol abuse underwent liver transplantation 2 years ago. He now presents with elevated aspartate aminotransferase (AST) and alanine aminotransferase (ALT). A history of depression and alcohol intake is noted by the clinician and he orders a liver biopsy, with findings as shown above. Which finding(s) help the clinician to consider recurrent alcoholic liver disease as the diagnosis in this setting?
- Chronic inflammation in the portal tracts with granulomas in the histology
- History of alcohol intake and chronic hepatitis with severe activity
- History of alcohol intake and liver biopsy showing steatosis
- Steatosis alone allows the diagnosis of recurrent alcoholic liver disease
Board review style answer #1
C. History of alcohol intake and liver biopsy showing steatosis. The diagnosis of recurrent disease relies on the evidence that the same disease is happening again in the liver allograft. The diagnosis is multidisciplinary. The history of the patient's alcohol intake leads to clinical suspicion of recurrent alcoholic liver disease. If the liver biopsy shows steatosis, this is consistent with recurrent alcoholic liver disease, especially if other metabolic dysfunctions are excluded by the clinician (World J Gastroenterol 2018;24:2785, Best Pract Res Clin Gastroenterol 2020;46:101688). Answer A is incorrect because chronic inflammation in the portal tracts with granulomas in the histology is more common in primary biliary cholangitis and is not described in recurrent alcoholic liver disease. Answer D is incorrect because the histologic evidence of steatosis alone is not sufficient. A history of alcohol intake must be noted clinically. The diagnosis of recurrent alcoholic liver disease is multidisciplinary. Answer B is incorrect because recurrent alcoholic liver disease is linked to steatosis or steatohepatitis patterns of injury. If chronic hepatitis with severe activity is noted, the pathologist must consider the possibility of de novo autoimmune hepatitis.
Comment Here
Reference: Recurrent disease
Comment Here
Reference: Recurrent disease
Board review style question #2
A 45 year old woman with autoimmune hepatitis underwent liver transplantation. After 14 months, she presents with elevated aspartate aminotransferase (AST) and alanine aminotransferase (ALT). She has not taken her immunosuppressive medicines for the last 2 months. Serologic testing reveals antinuclear antibodies (ANA) and anti-smooth muscle antibodies (ASMA). Which histologic feature is characteristic of recurrent autoimmune hepatitis (AIH) in the liver allograft?
- Chronic hepatitis with moderate to severe interface activity
- Chronic inflammation in the portal tracts with granulomas in the histology
- Ductular reaction and periductal onion skin fibrosis
- Severe steatosis
Board review style answer #2
A. Chronic hepatitis with moderate to severe interface activity. Interface hepatitis, characterized by inflammation at the interface between hepatocytes and the portal tract, is a hallmark histologic feature of recurrent autoimmune hepatitis in the liver allograft, especially when it is moderate to severe. Other findings that may be seen in recurrent autoimmune hepatitis include prominent plasma cells, lobular activity with necrosis and perivenulitis (Ann Gastroenterol 2013;26:304, Liver Transpl 2009;15:S35). Answer B is incorrect because chronic inflammation in the portal tracts with granulomas in the histology is more common in primary biliary cholangitis and it is not part of the classic histologic pattern of recurrent autoimmune hepatitis. Answer C is incorrect because ductular reaction and periductal onion skin fibrosis are more common in primary sclerosing cholangitis and they are not part of the classic histologic pattern of recurrent autoimmune hepatitis. Answer D is incorrect because severe steatosis is not pathognomonic of recurrent autoimmune hepatitis, although steatosis can be noted because of toxic injury when the patient is being treated with steroids.
Comment Here
Reference: Recurrent disease
Comment Here
Reference: Recurrent disease