Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Joneja U. Von Meyenburg complex. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livermeyenburgcomplex.html. Accessed April 2nd, 2025.
Definition / general
- Von Meyenburg complex (VMC) is a ductal plate malformation of the liver characterized by dilated interanastomosing bile duct structures in collagenized stroma that results from failure of involution of excess embryologic remnants
Essential features
- Common, incidental, small (usually < 0.5 cm), subcapsular or periportal, nodular or cystic lesions; multiple or single (AJR Am J Roentgenol 1995;165:309)
- Composed of dilated, irregularly anastomosing bile ducts with bland cuboidal epithelium embedded in collagenous stroma
- Considered benign and requires no treatment
- Usually asymptomatic; their clinical importance lies in simulation of malignancies, abscesses and granulomas on imaging
- Can also be associated with hepatic cysts and other ductal plate malformation diseases, such as polycystic kidney disease, Caroli disease, Caroli syndrome and congenital hepatic fibrosis
Terminology
- Biliary (bile duct) hamartoma
- Bile duct microhamartoma
- Not recommended: peribiliary gland hamartoma (this is an alternative name for bile duct adenoma)
ICD coding
- ICD-10: Q85.9 - phakomatosis, unspecified
Epidemiology
- Common incidental finding in liver surgical specimens and autopsies
- Incidence: 5.6% of adults and 0.9% of children (Mod Pathol 1996;9:233)
- Age and gender predilections not well studied
- Macroscopic hepatic cysts identified in 16.9% of livers with VMC (Mod Pathol 1996;9:233)
- Can be found in association with other diseases of ductal plate malformation, such as polycystic kidney disease, Caroli disease, Caroli syndrome and congenital hepatic fibrosis (Mayo Clin Proc 1998;73:80)
Sites
- Liver is the only affected organ
Pathophysiology
- During embryologic development at 9 - 10 weeks gestation, primitive hepatocyte precursor cells destined to form smaller intrahepatic bile ducts condense around the portal tracts forming a sleeve referred to as the ductal plate (J Med Genet 2003;40:311)
- During weeks 18 - 40, certain ductal plates are selected by the way of remodeling to form intrahepatic bile ducts while redundant ones are deleted (Mayo Clin Proc 1998;73:80)
- This process is regulated by epithelial mesenchymal interactions
- Defects at this stage, which have molecular basis in ciliogenesis and cellular polarization orchestrated by transcription factors HNF6 and HNF1ß, lead to persistence of excess embryonic bile ducts in a ductal plate configuration that is referred to as ductal plate malformation (DPM) (Hepatology 2011;53:1959)
- DPMs represent a category of diseases involving abnormal formation of intrahepatic ducts, such as von Meyenburg complex, congenital hepatic fibrosis, Caroli disease, Caroli syndrome and polycystic kidney disease (Hepatology 1992;16:1069, Mayo Clin Proc 1998;73:80)
Etiology
- Complete or partial arrest of involution of redundant bile duct structures in the smaller interlobular bile ducts
Clinical features
- Usually asymptomatic; rare cases have been reported with
- Abdominal pain, hemorrhage, cholangitis (J Surg Case Rep 2017;2016:rjw195)
- Jaundice (Clin Imaging 2007;31:50)
- Portal hypertension (Liver Int 2009;29:614)
- Usually small (0.1 - 1.5 cm); however, giant VMCs have been reported in 0.4% of cases (J Magn Reson Imaging 2010;31:903)
- Largest reported size is 21.6 cm (Mod Pathol 1996;9:233)
- Fewer than 40 reports postulating development of cholangiocarcinomas / even rarer hepatocellular carcinomas in association with VMC (Am J Gastroenterol 1977;67:40, Eur J Gastroenterol Hepatol 2009;21:580, Ann Diagn Pathol 2008;12:208)
- Presence of numerous VMCs raises consideration for other ductal plate malformation associated diseases
Diagnosis
- Magnetic resonance imaging (MRI) with gadolinium is the best diagnostic imaging modality
- Biopsy or surgical resection
Radiology description
- MRI: hypointense on T1 weighted imaging and hyperintense on T2 weighted sequences; similar signal intensity to the spleen but less than liver cysts (World J Gastroenterol 2005;11:6354)
- MR cholangiography: identifies even smaller lesions that may not be evident on MR
- MRI with contrast with biliary excretion (gadolinium): helps differentiate saccular dilatation of biliary tree (Caroli disease) from VMC (no communication / no change in enhancement)
- CT: small, round or irregular, low attenuation areas that do not enhance on contrast injection but are more easily identifiable
- Ultrasound: hypoechoic or hyperechoic lesions depending on the density of glandular (hypoechoic) versus stromal (hyperechoic) elements with comet tail artifact
Case reports
- 6 year old girl with congenital hepatic fibrosis who received a liver transplant from mother with VMC (World J Gastroenterol 2016;22:9865)
- 40 year old man with hematochezia and numerous diffusely distributed liver lesions (World J Clin Cases 2020;8:1745)
- 45 year old woman with chickenpox infection and incidental MRI finding of extensive hepatic micronodularity (BMJ Case Rep 2015;2015:bcr2015211141)
- 50 year old man with abnormal liver function tests and multiple liver lesions (Ann Hepatol 2017;16:812)
- 53 year old man with jaundice and right upper quadrant pain (BBMJ Case Rep 2016;2016:bcr2016215220)
- 55 year old woman with epigastric pain, vomiting and early satiety for 1 year (J Surg Case Rep 2017;2016:rjw195)
Treatment
- Benign lesions that require no treatment
Gross description
- Small (0.1 - 1.5 cm), single or multiple, gray-white or green (bile stained), cystic or solid lesions; well delineated, unencapsulated, subcapsular or portal based (Am J Roentgenol 1995;165:309)
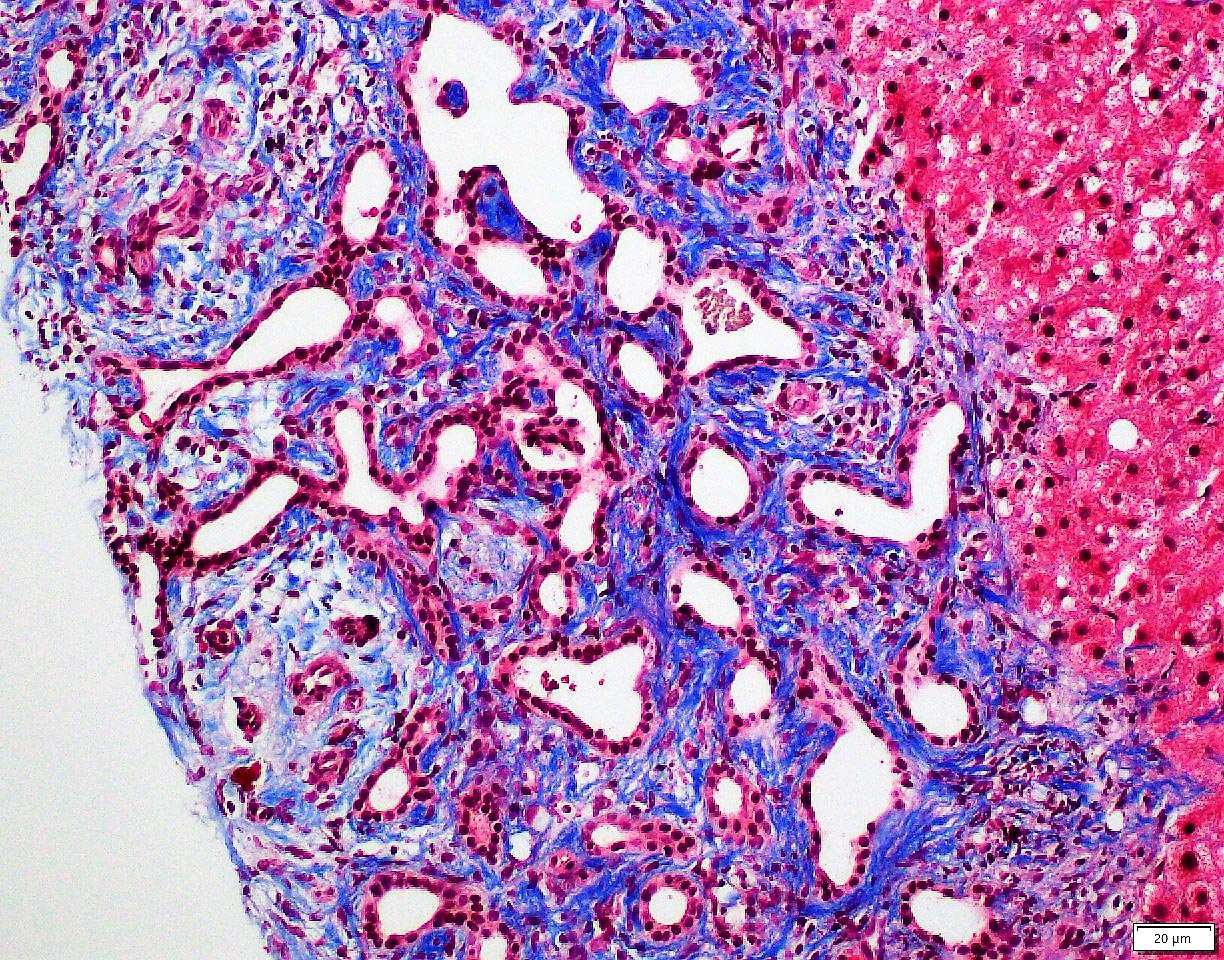
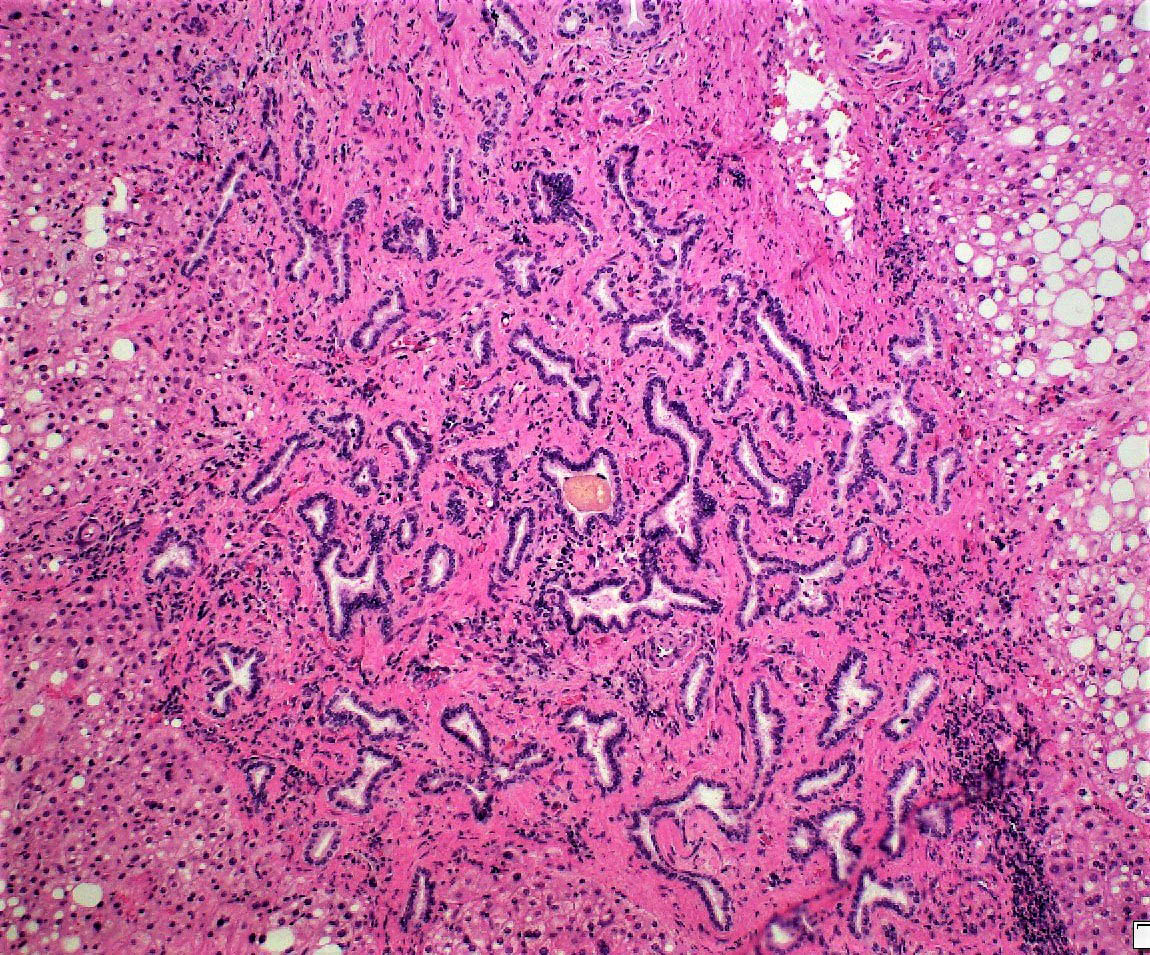
Microscopic (histologic) description
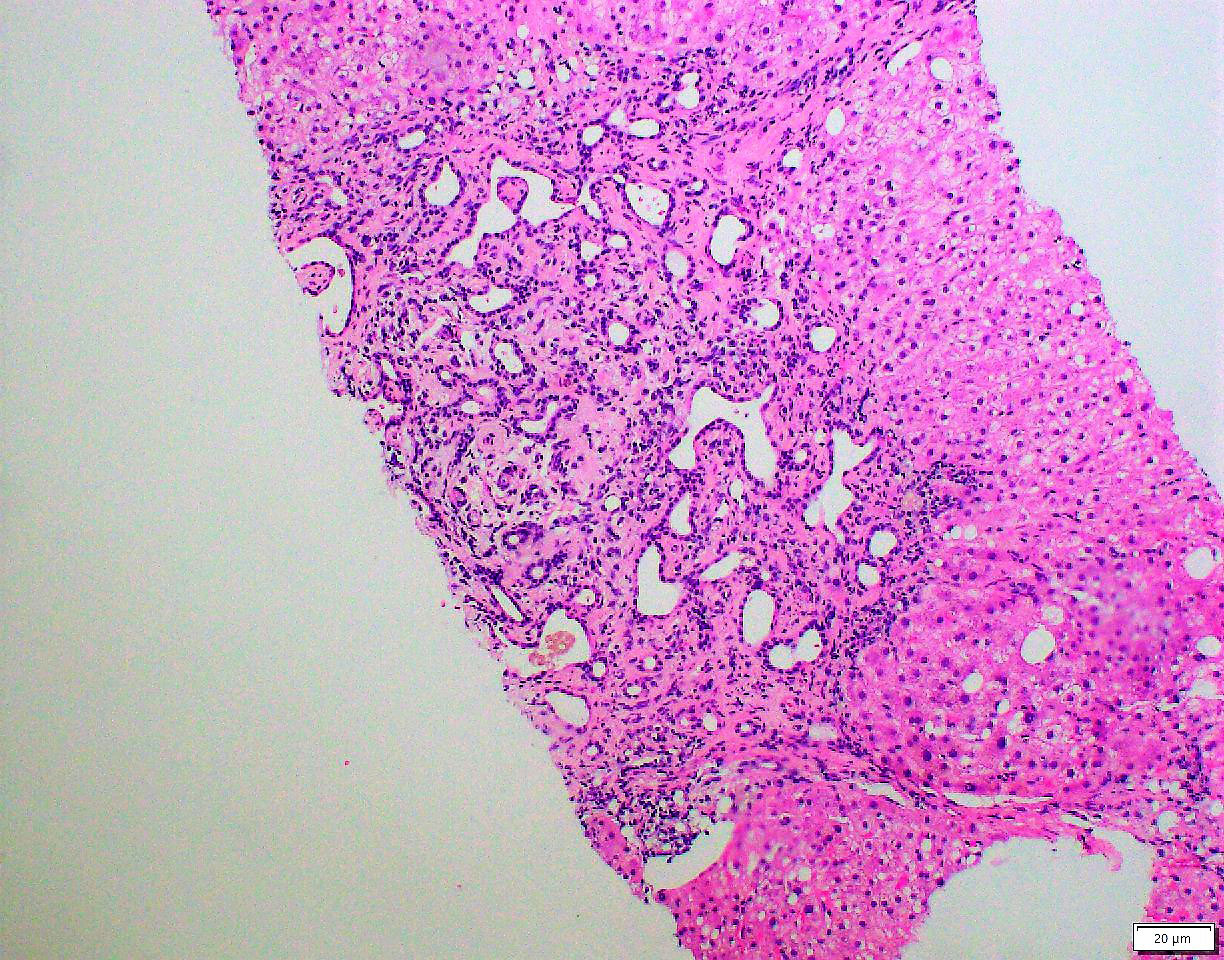
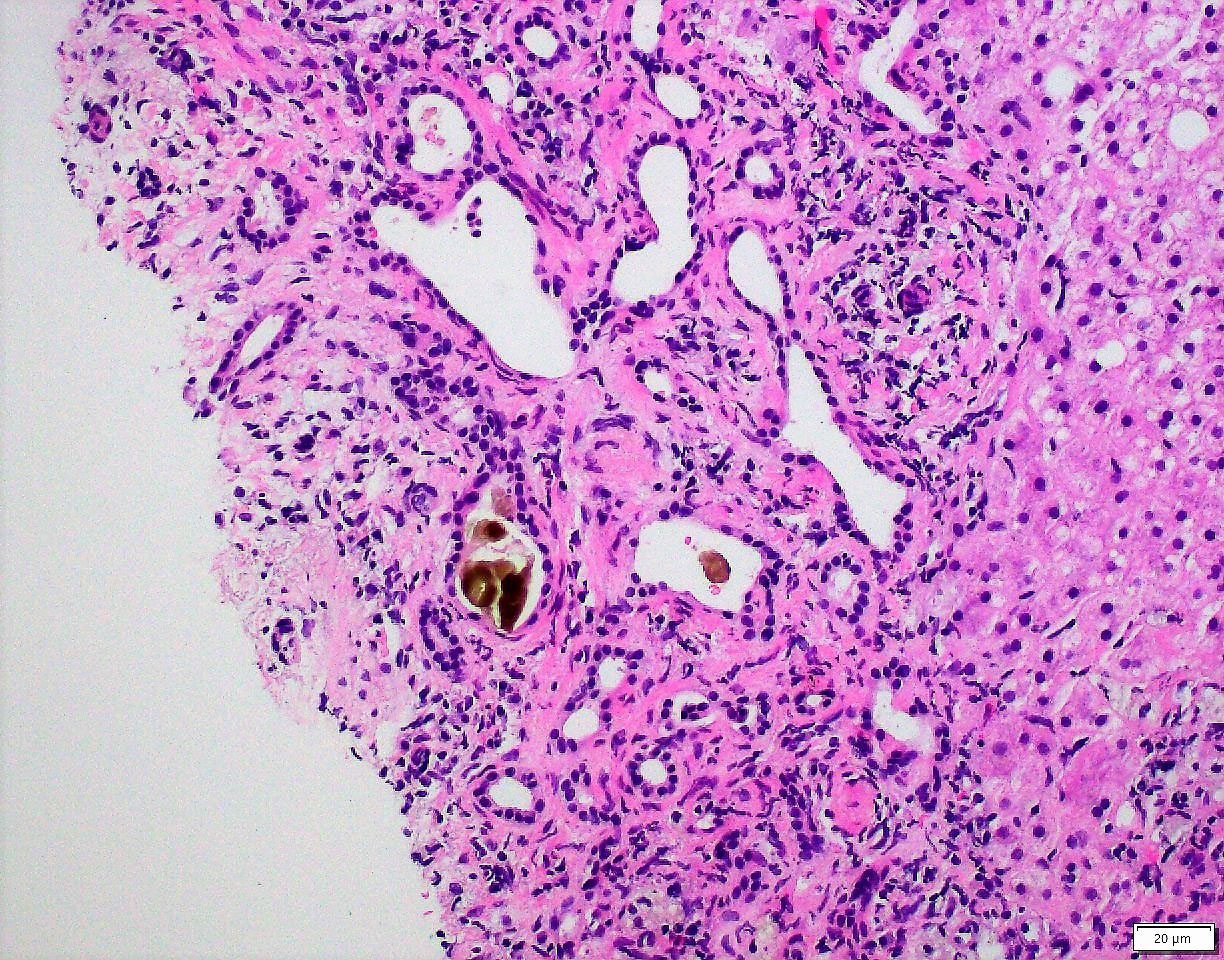
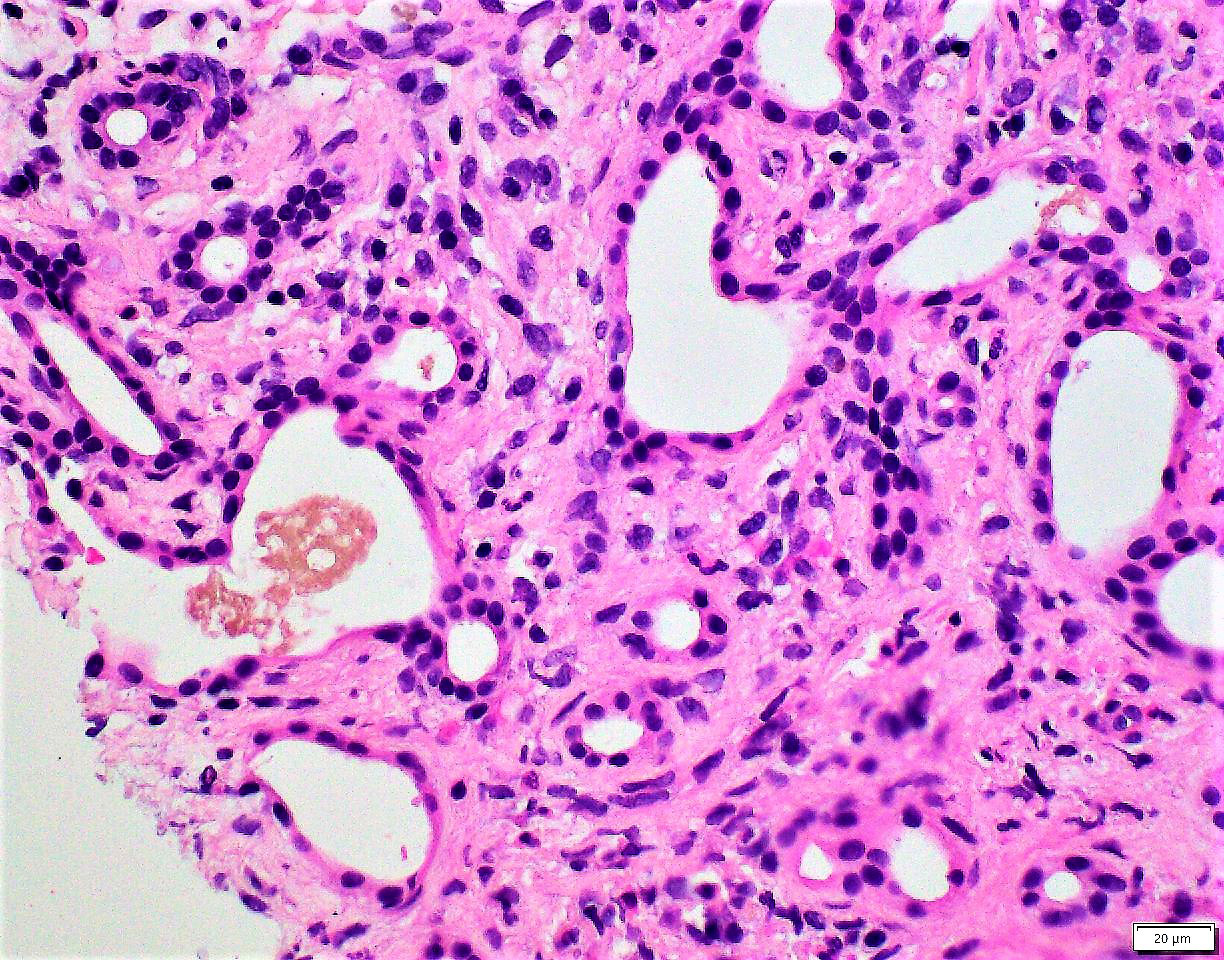
- Small to medium sized, irregularly shaped bile ducts lined by bland cuboidal or flattened epithelium; glands typically more dilated / cystic than normal bile ducts with prominent intervening collagenous stroma (Torbenson: Surgical Pathology of the Liver, 1st Edition, 2017)
- Bile ducts may contain inspissated bile or eosinophilic debris
- Commonly subcapsular or located at or in the periphery of portal tracts
- Surrounding inflammatory cells may be present
Microscopic (histologic) images
Cytology description
- Benign appearing bile duct epithelial cells often in the form of monolayer sheets of glandular cells with small uniformly spaced round nuclei (Torbenson: Surgical Pathology of the Liver, 1st Edition, 2017)
- Scant mucin may be present in the apical aspect
- Absence of background benign hepatocytes raises consideration for this lesion
- Cytology findings of VMCs and bile duct adenomas are similar
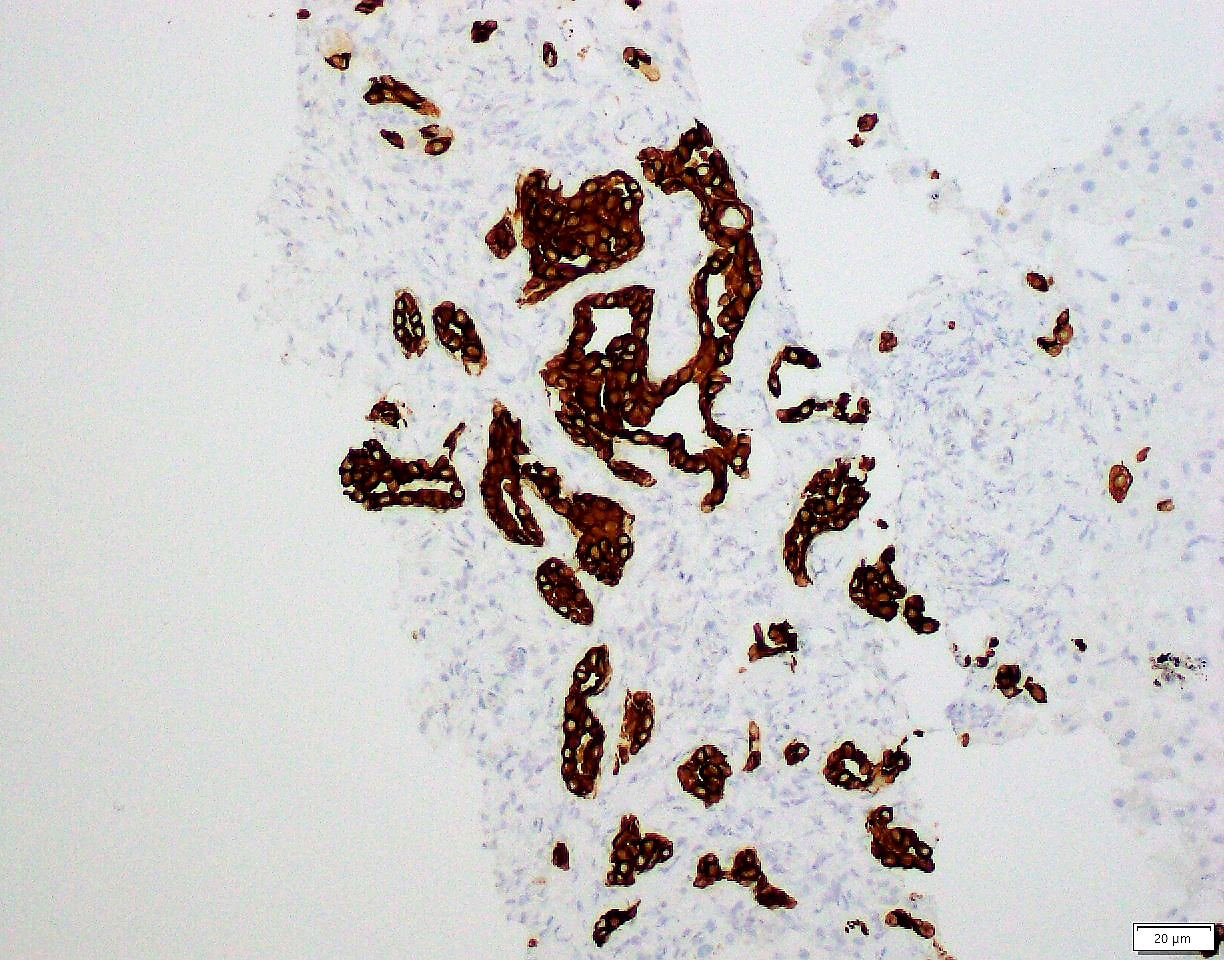
Positive stains
Sample pathology report
- Liver, needle core biopsy:
- Incidental biliary hamartoma / von Meyenburg complex, 0.3 cm
- Liver, needle core biopsy:
- Ductal plate malformation / multiple von Meyenburg complexes with portal to portal bridging fibrosis (see comment)
- Comment: Given the presence of multiple VMCs and increased portal based fibrosis, consideration for ductal plate malformation associated diseases, such as polycystic kidney disease, Caroli disease, Caroli syndrome and congenital hepatic fibrosis should be given. Radiologic correlation is recommended.
Differential diagnosis
- Pancreatic adenocarcinoma / cholangiocarcinoma:
- Irregularly shaped glands including single tumor cells with uneven gland distribution and infiltrative borders at hepatic interface
- Cellular atypia including variability in nuclear size, irregular nuclear contours, hyperchromasia, prominent mucin, mitoses and absence of bile within glandular lumens
- Immunohistochemical stain for SMAD4 / DPC4, which shows loss of expression in some pancreatic adenocarcinomas, can be helpful in challenging cases
- Bile duct adenoma (peribiliary duct hamartoma):
- Uncommon, benign neoplastic proliferation
- Wedge or round lesions, circumscribed and unencapsulated
- Composed of uniform rounded bile ducts with single layer of plump cuboidal epithelium in hyalinized or cellular desmoplastic appearing stroma
- Usually, no bile is identified in the glandular lumens
- 53% of bile duct adenomas have BRAF V600E mutations (Histopathology 2015;67:562)
- Ductal plate malformations
- Caroli disease:
- Dilatations of larger intrahepatic bile ducts, saccular or fusiform, that communicate with the biliary system (Mayo Clin Proc 1998;73:80)
- Multiple VMCs
- Morbidity and mortality due to biliary stasis, stones and recurrent cholangitis
- Congenital hepatic fibrosis:
- Prominent portal fibrosis with thick portal to portal bridges in a cirrhosis-like pattern
- Numerous von Meyenburg complexes in periportal / periseptal areas
- Caroli syndrome:
- Features of congenital hepatic fibrosis and Caroli disease (liver fibrosis, VMCs and saccular dilatations of the biliary tree)
- Currently assumed to be part of the spectrum of autosomal recessive polycystic kidney disease (Mayo Clin Proc 1998;73:80)
- Polycystic liver disease and polycystic kidney disease (Orphanet J Rare Dis 2014;9:69):
- VMC with or without Caroli syndrome and renal cysts
- Variable phenotypes, including exclusively renal or exclusively liver disease (Am J Med Genet A 2015;167A:3046)
- Caroli disease:
Board review style question #1
Which of the following is true regarding the lesion shown above?
- Approximately 50% have BRAF V600E gene mutation
- Distinguishing bile duct adenomas and these lesions is clinically relevant
- Immunohistochemical chemical stain for CK7 can be helpful in distinguishing this lesion from metastatic pancreatic adenocarcinoma
- Isolated lesions are insignificant but their clinical importance lies in their mimicry of malignant tumors
Board review style answer #1
D. Isolated lesions are insignificant but their clinical importance lies in their mimicry of malignant tumors. The picture shows a small liver lesion comprising irregular anastomosing bile duct structures lined by a bland single layer of cuboidal / flattened epithelium with intervening dense collagenous stroma and intraluminal bile. The histologic findings are consistent with von Meyenburg complex.
Usually, incidental VMCs are asymptomatic and of no clinical significance. Their clinical relevance lies in their mimicry of metastatic tumors or infections on radiology and intraoperatively.
Answer A is incorrect because the lesions are ductal plate malformations (not neoplasms) and are not associated with mutations in the BRAF gene. BRAF mutations have been identified in a subset of bile duct adenomas. Answer B is incorrect because bile duct adenomas and VMCs are both benign entities; therefore, differentiating them is of academic interest but does not hold clinical relevance. Answer C is incorrect because both VMCs and metastatic pancreatic adenocarcinomas can be CK7 positive and therefore, CK7 does not help in this differential diagnosis. SMAD4 loss when present is specific for metastatic pancreatic carcinoma over benign biliary lesions, such as VMC or bile duct adenoma.
Comment Here
Reference: Von Meyenburg complex
Answer A is incorrect because the lesions are ductal plate malformations (not neoplasms) and are not associated with mutations in the BRAF gene. BRAF mutations have been identified in a subset of bile duct adenomas. Answer B is incorrect because bile duct adenomas and VMCs are both benign entities; therefore, differentiating them is of academic interest but does not hold clinical relevance. Answer C is incorrect because both VMCs and metastatic pancreatic adenocarcinomas can be CK7 positive and therefore, CK7 does not help in this differential diagnosis. SMAD4 loss when present is specific for metastatic pancreatic carcinoma over benign biliary lesions, such as VMC or bile duct adenoma.
Comment Here
Reference: Von Meyenburg complex
Board review style question #2
Which of the following is true about von Myenberg complexes?
- Alternatively called peribiliary duct hamartomas
- Can be associated with other ductal plate malformation diseases
- CK20 is positive in the glandular elements of VMC
- They are considered to be neoplastic proliferations in the liver
- They communicate with the intrahepatic biliary tree
Board review style answer #2
B. Can be associated with other ductal plate malformation diseases. They can be found in association with other ductal plate malformation diseases, such as Caroli disease, Caroli syndrome and polycystic kidney disease. VMC is a ductal plate malformation usually found incidentally, though it can be seen in association with ductal plate malformation diseases, such as Caroli disease, congenital hepatic fibrosis, Caroli syndrome and polycystic kidney disease.
Answer A is incorrect because VMCs are alternatively called bile duct hamartomas or biliary microhamartomas. Bile duct adenomas are also called peribiliary duct hamartomas, which can lead to confusion. Answer D is incorrect because VMCs are usually incidental findings that result from the presence of redundant bile duct structures due to aberrations in embryogenesis. Answer E is incorrect because they do not characteristically show communication with the intrahepatic biliary system. Answer C is incorrect because the biliary structures in VMC are positive for CK7, CK18 and CK19, while negative for CK20 and CDX2.
Comment Here
Reference: Von Meyenburg complex
Answer A is incorrect because VMCs are alternatively called bile duct hamartomas or biliary microhamartomas. Bile duct adenomas are also called peribiliary duct hamartomas, which can lead to confusion. Answer D is incorrect because VMCs are usually incidental findings that result from the presence of redundant bile duct structures due to aberrations in embryogenesis. Answer E is incorrect because they do not characteristically show communication with the intrahepatic biliary system. Answer C is incorrect because the biliary structures in VMC are positive for CK7, CK18 and CK19, while negative for CK20 and CDX2.
Comment Here
Reference: Von Meyenburg complex