Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Khurram NA. Late T cell mediated (cellular) rejection. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverlateTcellrejection.html. Accessed April 2nd, 2025.
Definition / general
- Alloimmune injury to the allograft driven primarily by effector T cells (with varying accompaniment by monocytes and macrophages), usually occurring > 3 - 6 months posttransplantation with the potential to produce clinically significant, progressive and chronic structural changes that include vascular, biliary, fibrotic and parenchymal remodeling transformation of the liver architecture (Banff Foundation: Banff Liver Group 2022 [Accessed 3 January 2024])
- Leads to worse patient and graft survival after liver transplantation (Arq Bras Cir Dig 2015;28:212)
Essential features
- Late onset T cell mediated rejection is a form of T cell mediated rejection (TCMR) usually occurring > 1, 3 or 6 months after transplantation (no uniform definition of the time point for late rejections); however, it is mostly believed to present after 6 weeks of transplantation (Liver Transpl 2019;25:425, Arq Bras Cir Dig 2015;28:212)
- Interface activity and centrilobular necroinflammatory lesions falling within the spectrum of central perivenulitis (with or without portal inflammation) are common features
- Perivenular fibrosis in severe cases
- Frequently in patients noncompliant with immunosuppression (Transplant Direct 2022;8:e1076)
Terminology
- Late onset T cell mediated rejection (Liver Transpl 2019;25:425)
- Idiopathic posttransplantation hepatitis (J Hepatol 2011;55:702)
- Hepatitic variant of acute cellular rejection (ACR), plasma cell rich ACR, late occurring rejection, atypical rejection with zone 3 perivenulitis
ICD coding
- ICD-10: T86.41 - liver transplant rejection
Epidemiology
- Incidence rate ranges from 7% to 23% (World J Gastroenterol 2006;12:6674, Transplantation 2013;95:955)
- Young adults (10 - 24 years old) have a significantly higher incidence of late TCMR than controls (Transplant Direct 2022;8:e1076)
- Other risk factors
- Patients with preserved renal function at the time of transplantation (Transplant Direct 2022;8:e1076)
- Documented medication noncompliance
- Young age
- Early moderate to severe or steroid resistant TCMR remains a significant variable for late onset TCMR (Liver Transpl 2019;25:425)
- de novo donor specific antibody (DSA) development (Am J Transplant 2016;16:2816)
Sites
- Liver allografts
- Also occurs in other solid organ allografts, such as the kidney
Pathophysiology
- Indirect antigen recognition (Am J Transplant 2016;16:2816)
- Linked to de novo donor specific antibodies (DSA) development (Transplant Direct 2022;8:e1076)
- Diagnostic designation as TCMR does not exclude a contribution from DSA or innate effector mechanisms but is a practical synoptic recognition of the dominant tissue appearance and associated RNA signature (Banff Foundation: Banff Liver Group 2022 [Accessed 3 January 2024])
Diagrams / tables
Grading descriptors of late onset T cell mediated rejection presenting as isolated central perivenulitis (Hepatology 2006;44:489)
| Description | Biopsy findings |
| Minimal or indeterminate | Perivenular inflammation involving a minority of terminal hepatic veins, with patchy perivenular hepatocyte loss but without confluent perivenular necrosis |
| Mild | As above but involving most terminal hepatic veins |
| Moderate | As above, with focal confluent perivenular hepatocyte dropout and mild or moderate inflammation but without bridging necrosis |
| Severe | As above, with confluent perivenular hepatocyte dropout and inflammation involving most hepatic venules and with central to central bridging necrosis |
Banff working group proposed scoring of late TCMR for further development (Banff Foundation: Banff Liver Group 2022 [Accessed 3 January 2024])
| Subscore | Component | Contribution | Criteria |
| Alloimmune activity grade | Portal inflammation | 0 - 3 | Existing Banff criteria |
| Bile duct damage | 0 - 3 | Existing Banff criteria | |
| More severe lesion: subendothelial inflammation or central perivenulitis | 0 - 4 | Banff rejection activity index (RAI) "v" score or Banff 2006 isolated CP score | |
| Interface hepatitis | 0 - 4 | Proposed criteria (see below) | |
| Fibrosis stage | Periportal | 0 - 3 | Venturi: LAFS |
| Subsinusoidal | 0 - 3 | ||
| Perivenular | 0 - 3 |
Images hosted on other servers:
Clinical features
- May be asymptomatic and detected on surveillance / protocol biopsies
- Some patients present with fever, malaise, abdominal pain, hepatosplenomegaly and rarely, increasing ascites; because most patients are asymptomatic, TCMR is suspected primarily by an increase in values on liver biochemical tests
- Biochemical tests measuring liver function may show a rise in transaminase levels in cases with more prominent lobular changes, contrasting with the cholestatic profile that is more typically seen in early portal based acute TCMR
- Presence of cholestasis may signify a more severe form of late onset TCMR, which is less likely to be steroid responsive
- Associated increased risk of developing a number of adverse outcomes including further episodes of TCMR and progression to chronic rejection or allograft failure
- References: Clin Transplant 2008;22:316, Transplant Proc 2001;33:1525
Diagnosis
- Criteria and categories for the diagnosis of TCMR were defined by the Banff working group (see Diagrams / tables) (Am J Transplant 2016;16:2816)
- Portal based inflammation may contain plasma cells and eosinophils with interface activity, portal subendothelitis and to a lesser extent bile duct involvement (less prominent compared with early TCMR)
- Lobular and central vein lesions are common, characterized by central perivenulitis, hemorrhage and hepatocellular dropout
- Isolated arterial "v" lesions have been described, with or without associated inflammatory component (Am J Transplant 2018;18:1534)
- "v" lesions are defined as intimal inflammation, age inappropriate fibrointimal hyperplasia or both, without the presence of associated interstitial T cell mediated rejection (TCMR)
- Arteritis and foamy arteriopathy may be seen when larger arteries are sampled
- Plasma cell rich variant: an atypical variant of rejection with mixed cellular and antibody components (see chronic antibody mediated rejection)
- Plasma cell component exceeding 30% of inflammatory cells
- Primary disease not antibody mediated rejection (AMR)
- Cholangitis can be seen but not a required feature
- Atypical features associated with late TCMR include features seen in chronic viral hepatitis or autoimmune hepatitis (AIH)
Laboratory
- Deranged liver function tests; higher levels of aspartate aminotransferase and alanine aminotransferase, and in severe forms, alkaline phosphatase and gamma glutamyl transferase
- Negative testing for hepatitis B, C and E (Liver Transpl 2016;22:1593)
- Presence of donor specific anti-HLA antibodies (DSA)
- No serum markers of inflammation are currently recommended
Radiology description
- Imaging studies are generally performed to exclude other causes of elevated liver biochemical tests and allograft dysfunction
- Imaging findings in patients with acute TCMR (e.g., liver allograft enlargement) are not specific
Case reports
- 20 year old woman who underwent liver replacement because of biliary type fibrosis / cirrhosis secondary to Alagille syndrome (Transplant Direct 2022;8:e1076)
Treatment
- For all patients with histologic evidence of acute TCMR of the liver allograft, the baseline maintenance immunosuppressive regimen is assessed and optimized, while the specific approach depends on the patient's drug regimen and baseline liver function
- For patients with rejection activity index (RAI) < 5, treatment usually depends on optimizing immunosuppression; options for immunosuppression include tacrolimus and mycophenolate
- For patients with severe TCMR (i.e., RAI ≥ 5), initial therapy consists of high dose glucocorticoids (e.g., methylprednisolone) followed by a glucocorticoid taper, in addition to optimizing the maintenance immunosuppression regimen (Transplantation 2018;102:727)
- For nonresponders, therapeutic options such as antithymocyte globulin have been used to treat patients with glucocorticoid refractory rejection
- Retransplantation for failed allografts (very rare)
- In contrast to early TCMR, late TCMR is difficult to treat
- Current treatment recommendations for late onset / persistent TCMR generally include an algorithmic stepwise approach
- Corticosteroids
- Increased calcineurin inhibitors
- Calcineurin inhibitor conversion (e.g., from cyclosporine to tacrolimus)
- Addition of an antimetabolite (azathioprine or mycophenolate)
- Antilymphocyte antibody therapy; one group even resorted to local allograft irradiation (Transplant Direct 2022;8:e1076, Liver Transpl 2015;21:47)
- Current treatment recommendations for late onset / persistent TCMR generally include an algorithmic stepwise approach
Gross description
- Rare specimens
- Explanted livers may show necrosis, discoloration or rupture if rejection is severe
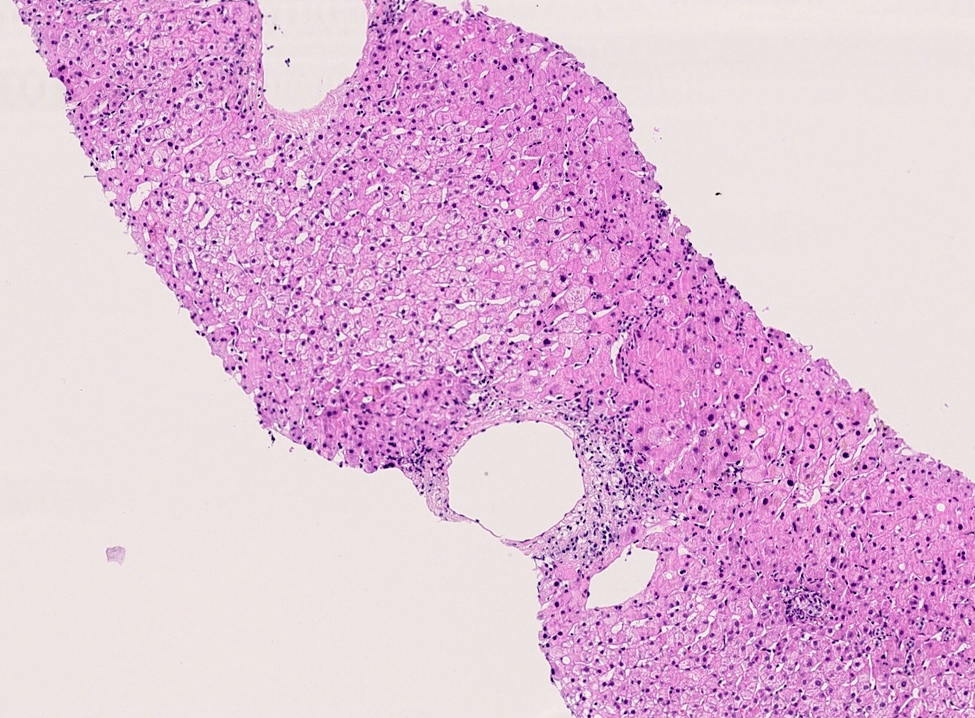
Microscopic (histologic) description
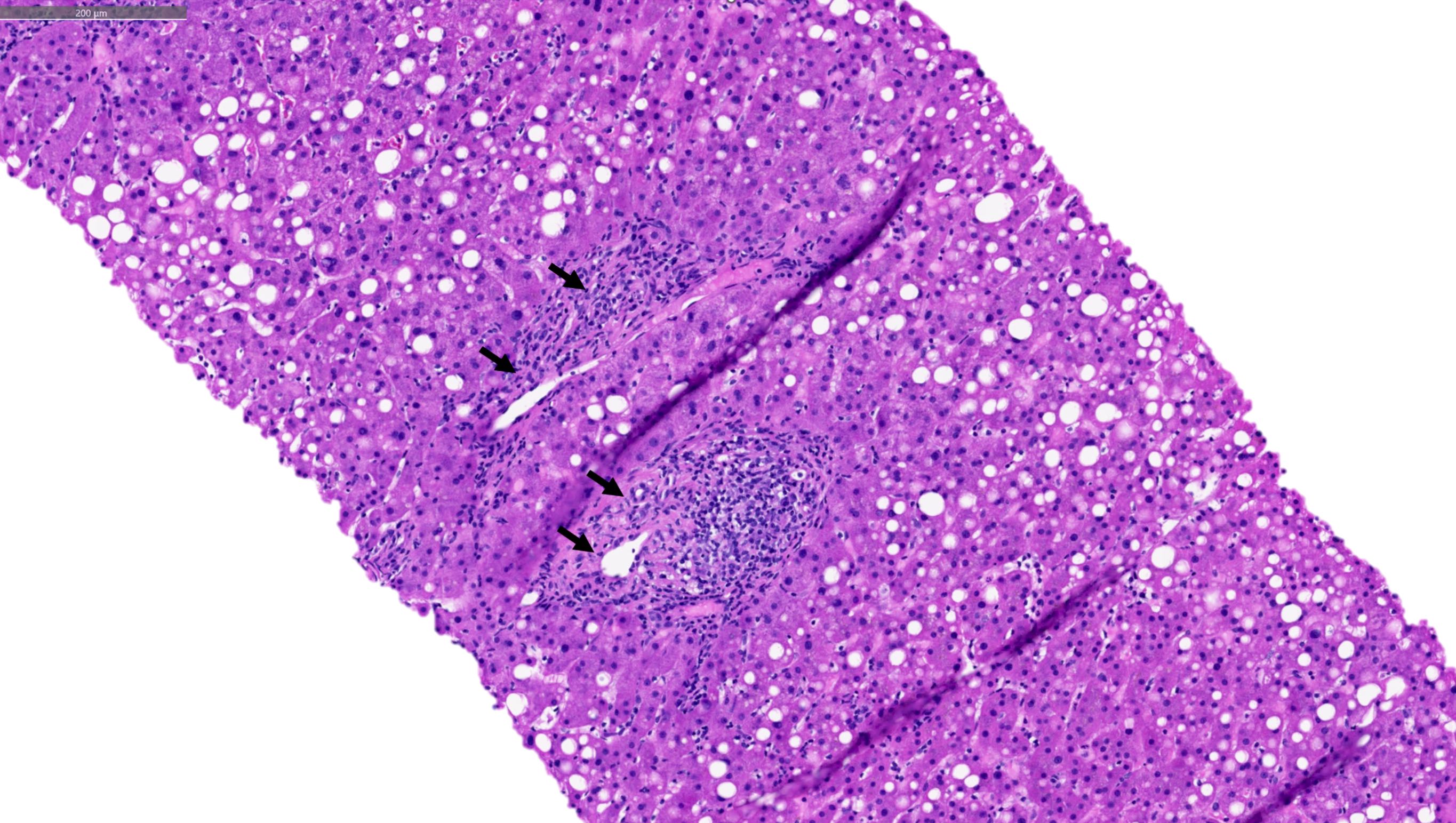
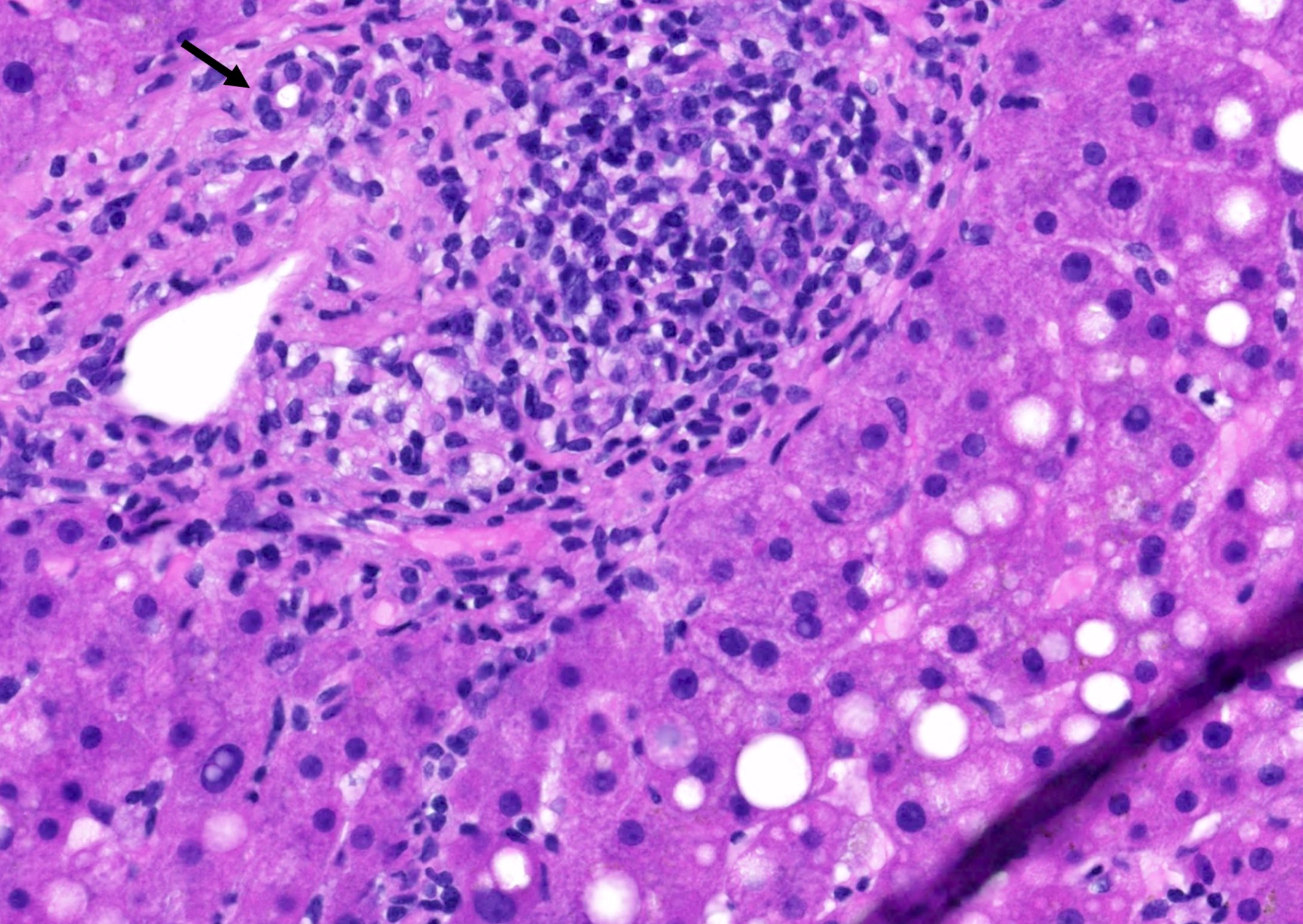
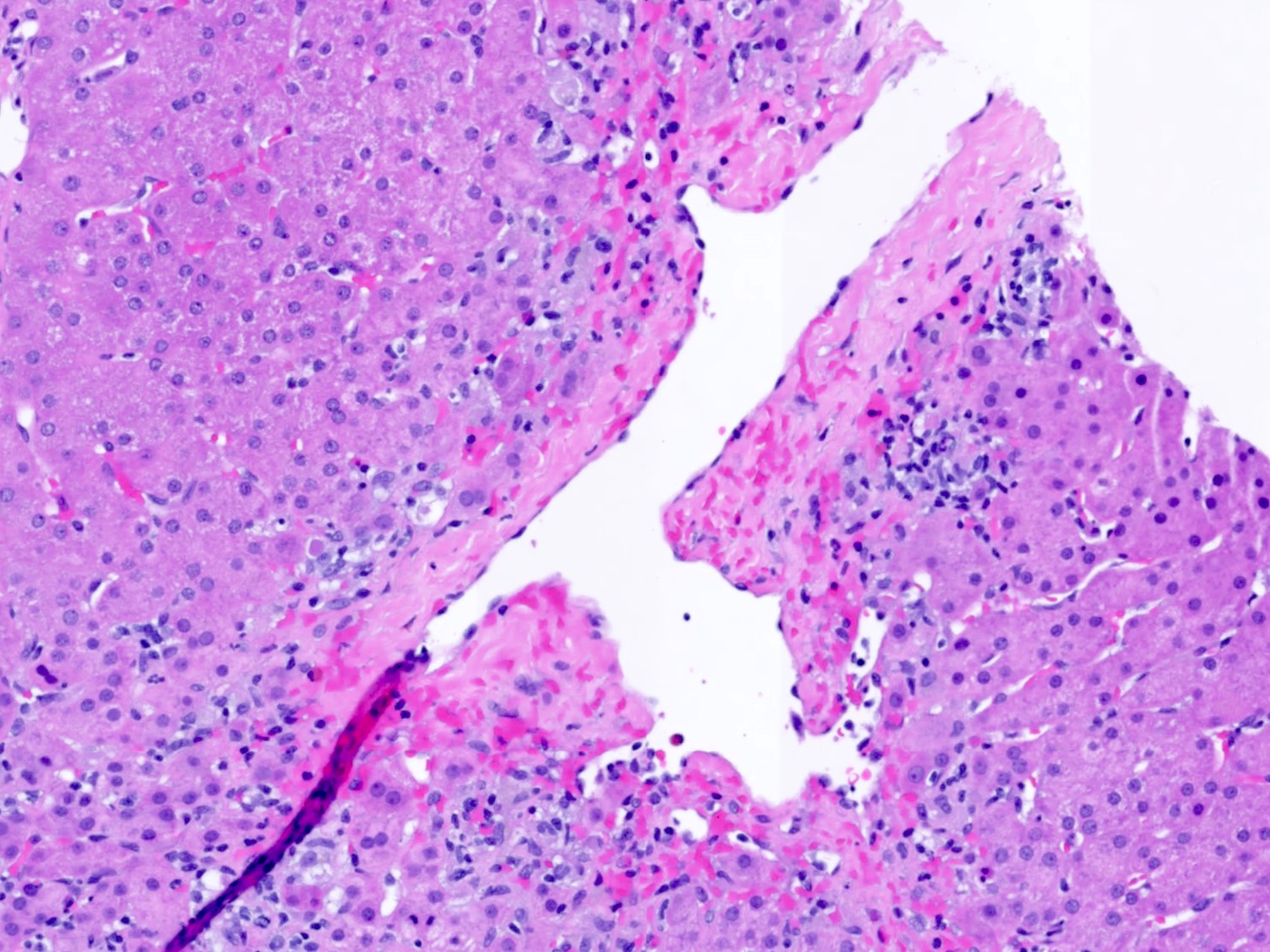
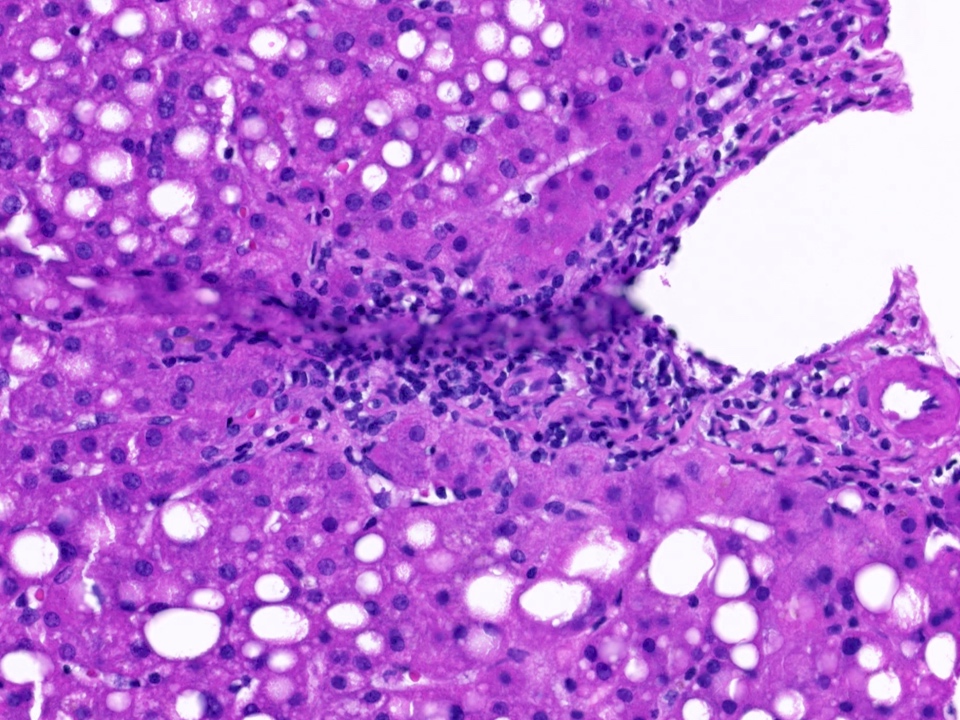
- Portal tract changes
- Portal inflammation: mononuclear portal inflammatory infiltrate (contrasting with the mixed population of cells [lymphocytes, plasma cells, eosinophils, macrophages] seen in biopsies taken during early TCMR < 6 weeks) (Hepatology 2006;44:489)
- Bile duct inflammation damage
- Venous endothelial inflammation
- Interface hepatitis: extension of portal inflammation beyond the limiting plate into the adjacent lobule with damage and progressive loss of hepatocytes at the portal lobular interface
- Lobular parenchyma
- Prominent central perivenular inflammation and hepatocyte dropout with minimal or no portal tract changes (i.e., isolated central perivenulitis) (Histopathology 2020;76:822, Hepatology 2006;44:489)
- Subendothelial inflammation of the portal or central veins is not a required finding
- More prominent interface hepatitis
- Overall appearances may thus come to resemble those seen in chronic viral hepatitis or AIH
- Centrilobular necroinflammatory lesions falling within the spectrum of central perivenulitis (CP), either with or without portal inflammation, are a common feature of late TCMR
- Fibrosis
- Extensive and severe perivenular fibrosis resembling Budd-Chiari syndrome or a sinusoidal obstruction type syndrome can develop as a consequence of severe or persistent central perivenulitis
Microscopic (histologic) images
Sample pathology report
- Liver allograft, needle biopsy:
- Mild perivenular lymphoplasmacytic inflammation with perivenular hepatocyte dropout and fibrosis favors T cell mediated rejection manifesting primarily as central perivenulitis (rejection activity index: 3/8) (see comment)
- Mild lymphoplasmacytic portal inflammation with ongoing interface activity and capillaritis and focally prominent shunt type vessels
- C4d negative for convincing portal microvascular endothelial cell positivity
- Mild to moderate portal / periportal and severe perivenular fibrosis with focal bridging
- No previous biopsy available for comparison
- Comment: The main histopathological findings include mild lymphoplasmacytic and histiocytic perivenular inflammation, hepatocyte dropout and fibrosis, accompanied by mild patchy lymphoplasmacytic portal inflammation with mild ongoing interface activity but without significant lymphocytic cholangitis or ductopenia. This pattern of injury is most often seen with late onset T cell mediated rejection; however, the differential diagnosis would also include so called de novo autoimmune hepatitis, which some refer to as late onset plasma cell rich T cell mediated rejection, suboptimal hepatic arterial flow or suboptimal venous drainage and drug induced liver injury (DILI).
- T cell mediated rejection is favored because of the combination of portal inflammation with interface activity combined with prevalent and prominent central perivenulitis and the patient's age. Vascular abnormalities are felt to be less likely because of the noticeable lymphoplasmacytic portal and perivenular inflammation but should be reasonably excluded; however, the other possibilities mentioned above cannot be absolutely excluded. Additional serologic studies, such as quantitative serum immunoglobulins and liver directed autoantibodies (ANA, ASMA, LKM, etc.) might provide additional useful information. Correlation with baseline immunosuppression is also suggested as nontacrolimus regimens are more frequently associated with late onset rejection and serum DSA development.
Differential diagnosis
- Late onset TCMR must be differentiated from recurrent hepatitis B or C and autoimmune hepatitis (AIH)
- Hepatitis B / hepatitis C:
- Features that suggest rejection rather than viral etiology include
- More prominent lymphocytic cholangitis
- Interface hepatitis
- Perivenular inflammation involving a majority of bile ducts and central veins
- Low grade or absent lobular and interface necroinflammatory activity
- Correlation with serum viral nucleic acid and autoantibody studies is essential
- Features that suggest rejection rather than viral etiology include
- Autoimmune hepatitis:
- Shows aggressive plasma cell rich interface activity
- Autoantibodies positivity (ASMA, anti-LKM, ANA, etc.)
- More prominent lobular necroinflammatory activity
Additional references
Board review style question #1
What is late onset T cell mediated rejection usually associated with?
- Excessive immunosuppression
- Focal to diffuse C4d uptake
- Immunosuppression noncompliance
- No fibrosis of the allograft
- Old age
Board review style answer #1
C. Immunosuppression noncompliance. Late onset TCMR often presents in patients > 1, 3 or 6 months after transplantation; however, it is mostly believed to present after 6 months of transplantation often as a result of noncompliance with immunosuppressive medications. Answer E is incorrect because late onset TCMR has no negative association with age of the recipient. Answer A is incorrect because excessive immunosuppression would lower immune cell counts, decreasing the risk for T cell mediated rejection but would cause other side effects. Answer B is incorrect because C4d deposition is more commonly seen in vascular walls of portal areas and hepatic sinusoidal walls in cases with antibody mediated rejection. Answer D is incorrect because late onset TCMR is associated with atrophy and fibrosis.
Comment Here
Reference: Late T cell mediated (cellular) rejection
Comment Here
Reference: Late T cell mediated (cellular) rejection
Board review style question #2
Per Banff rules, what would perivenular inflammation involving a minority of terminal hepatic veins, with patchy perivenular hepatocyte loss but without confluent perivenular necrosis be regarded as?
- Mild late T cell mediated rejection
- Minimal late T cell mediated rejection
- No rejection
- Severe late T cell mediated rejection
Board review style answer #2
B. Minimal late T cell mediated rejection. Answer C is incorrect because late onset TCMR can involve minority of terminal hepatic veins and that is considered rejection. Answer A is incorrect because mild late T cell mediated rejection involves most terminal hepatic veins. Answer D is incorrect because severe late T cell rejection shows confluent perivenular hepatocyte dropout with inflammation involving most hepatic venules along with central to central bridging necrosis.
Comment Here
Reference: Late T cell mediated (cellular) rejection
Comment Here
Reference: Late T cell mediated (cellular) rejection