Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: El Hag M. Acute antibody mediated rejection including hyperacute rejection. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverhumoralrejection.html. Accessed April 2nd, 2025.
Definition / general
- Antibody mediated immune injury to liver allografts with short and long term consequences
- 3 distinct subtypes:
- Hyperacute rejection (rare / mostly eliminated)
- Acute antibody mediated rejection (aAMR)
- Chronic active antibody mediated rejection (cAMR), see separate section
Essential features
- Hyperacute rejection is extremely rare nowadays and is predominantly limited to era of ABO incompatible transplants without desensitization
- Acute antibody mediated rejection is associated with circulating donor specific antibodies (human leukocyte antigen (HLA) and non-HLA), microvascular injury (capillaritis) and complement split products (C4d)
- Acute antibody mediated rejection may occur early posttransplantation in patients with preformed antibodies or late in patients with low immunosuppression compliance who may harbor preformed / memory antibodies or develop de novo antibodies
- Plasma cell rich rejection in patients with original disease other than autoimmune hepatitis (de novo autoimmune hepatitis / plasma cell hepatitis) is an atypical form of rejection, likely representing mixed T cell mediated rejection (TCMR) and aAMR etiology
Terminology
- Preferred terminology: antibody mediated rejection (AMR)
- Old terminology: humoral rejection (Am J Transplant 2016;16:2816)
- Preferred terminology: plasma cell rich rejection
- Old terminology: de novo autoimmune hepatitis / plasma cell hepatitis (Am J Transplant 2016;16:2816)
ICD coding
- ICD-10: T86.41 - liver transplant rejection
Epidemiology
- Hyperacute rejection:
- Now exceedingly rare; occurred during era of ABO incompatible transplantation without pretreatment (Surg Today 2011;41:317)
- Incidence: 60% without efforts to mitigate isoagglutinin titers, which must be kept below 1:16 (Semin Liver Dis 1992;12:51)
- Acute antibody mediated rejection:
- Estimated incidence is 5 - 20% in sensitized recipients with positive crossmatch (Am J Transplant 2012;12:171, Hepatology 1992;16:671)
- Plasma cell rich rejection variant is uncommon (3 - 5%) and is generally seen in patients with hepatitis C virus (HCV), primary sclerosing cholangitis (PSC) and primary biliary cholangitis (PBC), among other primary diseases (Am J Transplant 2016;16:2816)
- F > M
- Reduced size or living donor allografts > whole organs (Clin Transplant 2001;15:309)
Sites
- Liver allografts
- Also occurs in other solid organ allografts such as kidney and heart (Am J Transplant 2017;17:28, J Heart Lung Transplant 2005;24:1710)
Pathophysiology
- Can be caused by HLA and non-HLA donor specific antibodies (e.g. HLA, ABO isoagglutinins, AT1R, glutathione S-transferase, etc.) (Liver Transpl 2011;17:779, Liver Transpl 2004;10:1166, Transplantation 2020 Feb 25 [Epub ahead of print])
- Antibodies bind allograft endothelial cells and fix complement; this triggers the complement cascade with direct endothelial cell damage
- Donor specific antibody (DSA) binding also facilitates antibody dependent cellular cytotoxicity (ADCC), which is the basis for some of the histologic features of AMR, such as capillaritis and microvascular inflammation (Am J Transplant 2016;16:1653)
Etiology
- Transplantation in setting of ABO mismatch
- Presensitized patients with positive crossmatch
- Non compliance with immunosuppression regimen (particularly in late presentations of acute AMR)
Clinical features
- Hyperacute rejection:
- Begins immediately
- Allograft dysfunction evolves over a period of hours to days
- Coagulopathy, thrombocytopenia and increased need for blood products (Semin Liver Dis 1992;12:51)
- Acute antibody mediated rejection:
- Persistent elevation in transaminases alanine aminotransferase (ALT) / Aspartate transaminase (AST) and bilirubin
- Refractory thrombocytopenia
- Low serum complement levels
- Persistent circulating DSA
Diagnosis
- Criteria and categories for diagnosis of aAMR were defined by the Banff working group based on a combination of clinical, histopathological and serological findings (Am J Transplant 2016;16:2816):
Definitive for acute / active AMR (all 4 criteria required) A Histopathological pattern of injury consistent with acute AMR: e.g portal
microvascular endothelial cell hypertrophy, portal capillary and inlet venule
dilatation and portal microvasculitis (see microscopic description below for
h scoring and other associated pathological features)B Positive serum DSA (mean fluorescence intensity [MFI] usually > 5,000) C Diffuse microvascular endothelial C4d deposition (C4d score = 3) on formalin
fixed or frozen tissue in ABO compatible or portal stromal C4d in ABO
incompatible allografts (see positive stains below for C4d scoring)D Reasonable exclusion of other insults that might cause a similar pattern of injury
Suspicious for AMR (both criteria required)A DSA is positive B Nonzero h score with (C4d score + h score = 3 or 4) (see microscopic
description below for scoring parameters)
Indeterminate for AMR (requires a + b and c or d)A C4d score + h score ≥ 2 B DSA not available, equivocal or negative C C4d staining not available, equivocal or negative D Coexisting insult might be contributing to the injury
Laboratory
- ABO incompatible: isoagglutinins titer > 1:64
- HLA-DSA particularly against class II, frequently against multiple specificities, MFI usually > 5,000
- C1q binding capabilities
- Elevated AST, ALT, alkaline phosphatase, gamma glutamyl transpeptidase, bilirubin
Radiology description
- Helpful for ruling out other causes of dysfunction, such as biliary and vascular etiologies
Prognostic factors
- DSA are associated with:
- Decreased 5 year graft and patient survival
- Increased incidence of TCMR and plasma cell rich rejection
- Increased incidence of allograft fibrosis and chronic rejection (Am J Transplant 2014;14:779, J Immunol Res 2017;2017:3234906)
Case reports
- 23 year old woman with severe aAMR treated with plasmapheresis and mycophenolate mofetil (Transpl Int 2005;18:1298)
- 27 year old man with portal vein thrombosis and antibody mediated rejection (Transplant Proc 2008;40:870)
- 50 year old woman with isolated aAMR post-ABO compatible liver transplantation (Am J Transplant 2006;6:3022)
Treatment
- Usually consists of steroids and tacrolimus
- Thymoglobulin helps by disrupting T and B cell interaction
- Plasmapheresis and IVIG are used to deplete circulating antibodies in patients with severe aAMR (Curr Opin Organ Transplant 2016;21:209)
- Bortezomib, proteasome inhibitors and rituximab have also been used (Am J Transplant 2012;12:2526, World J Gastroenterol 2009;15:3426)
Gross description
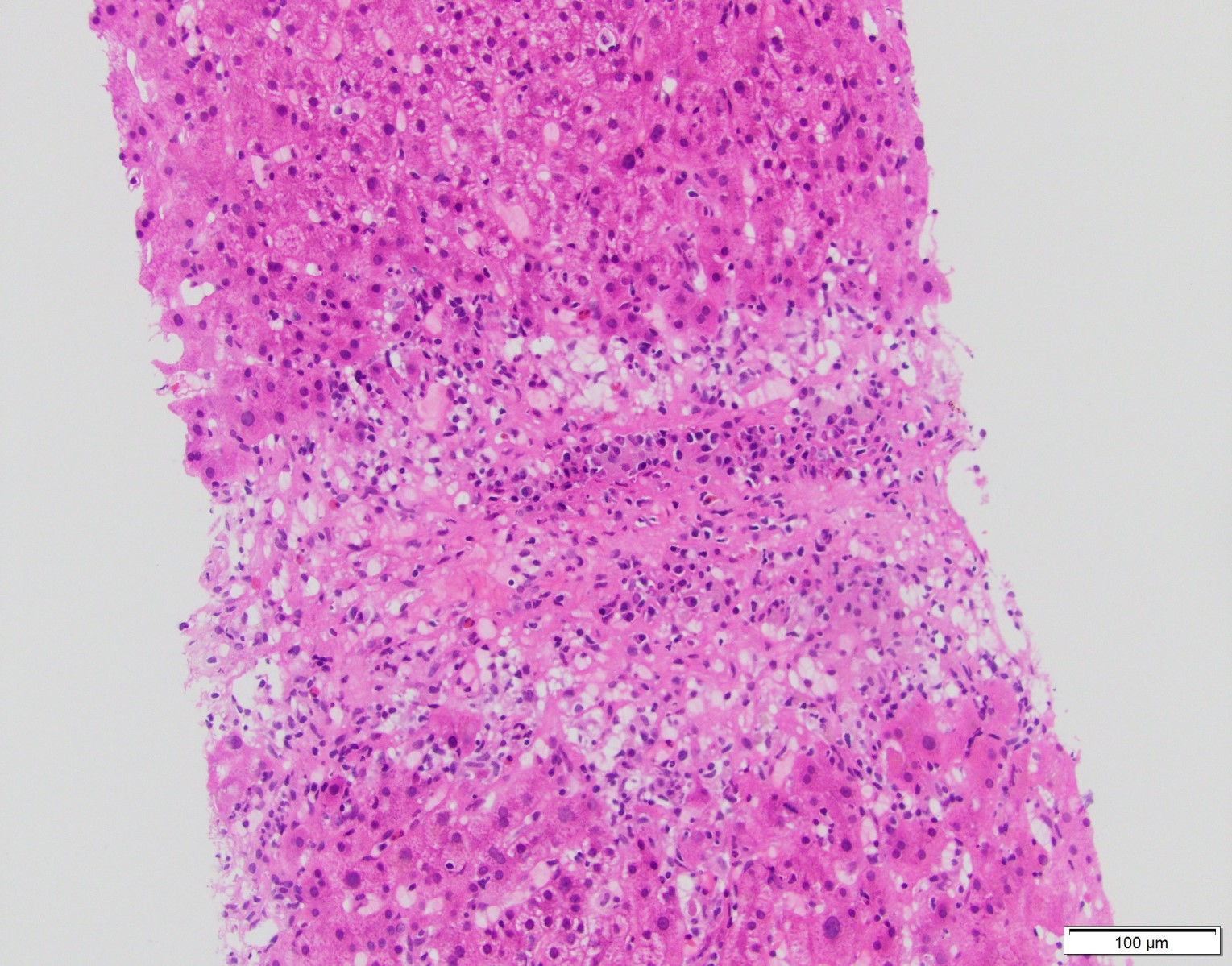
- In hyperacute rejection:
- Explanted organs are grossly enlarged and mottled areas of geographic necrosis
- Hepatic artery and portal vein thrombosis
- Capsular rupture
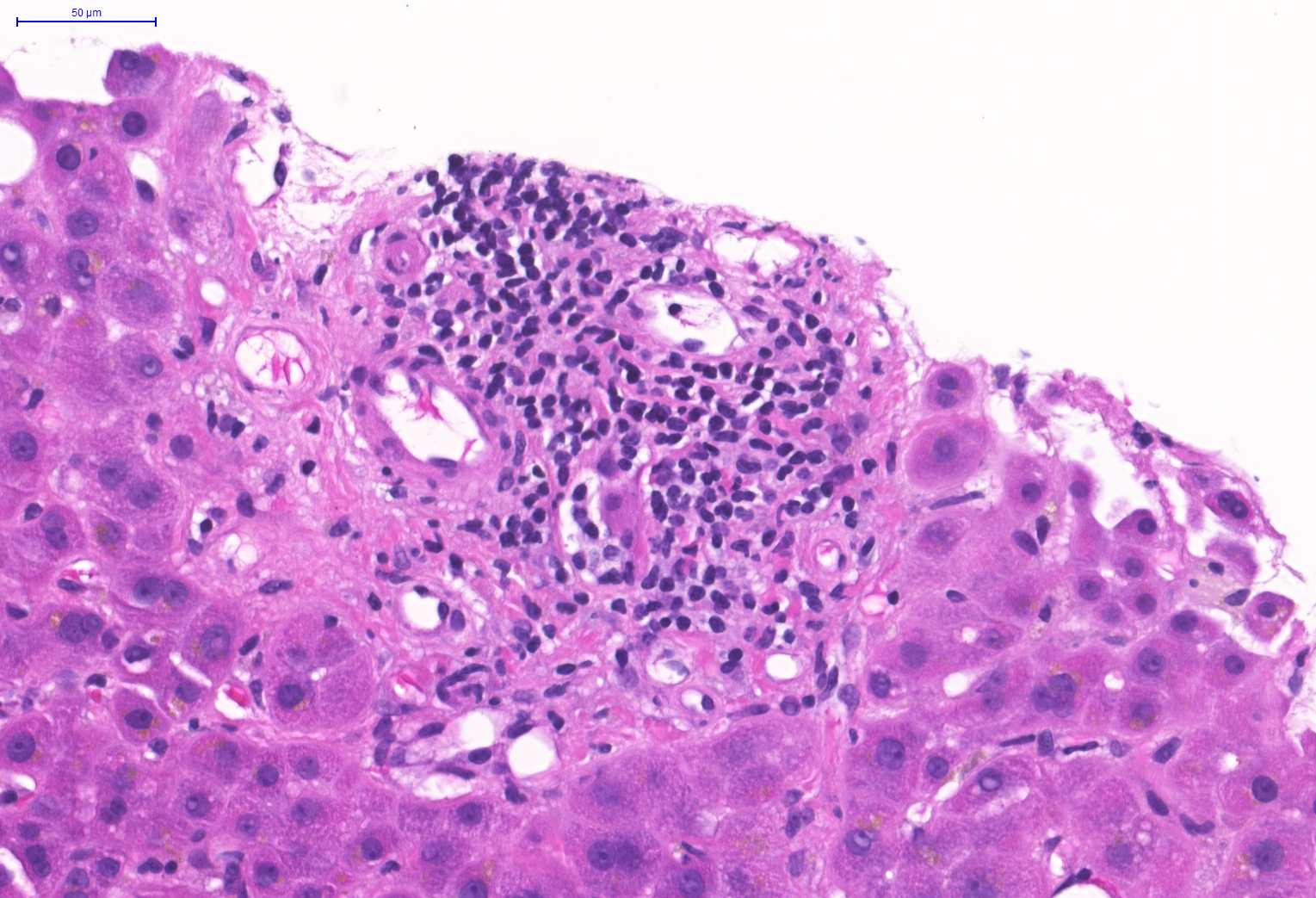
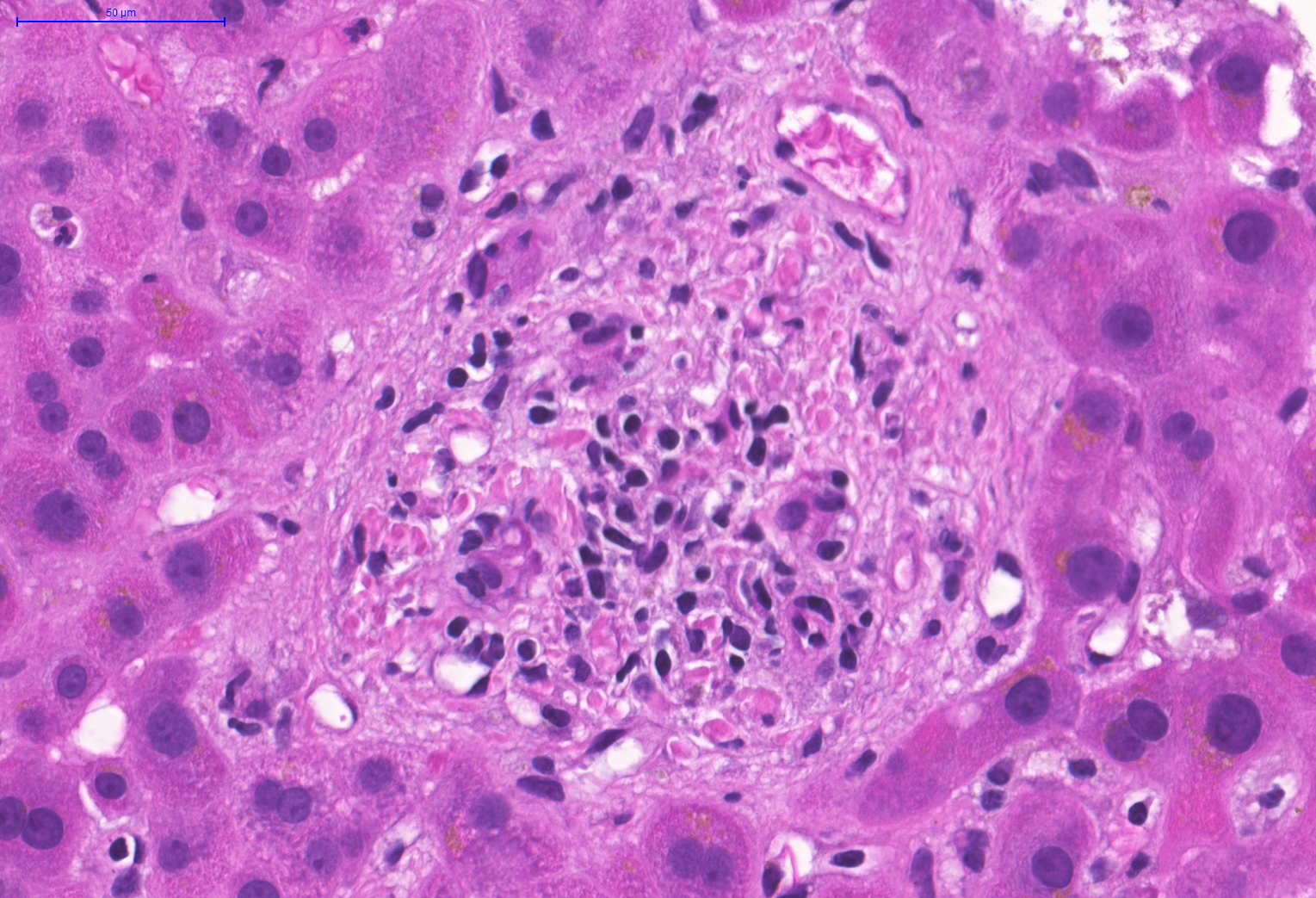
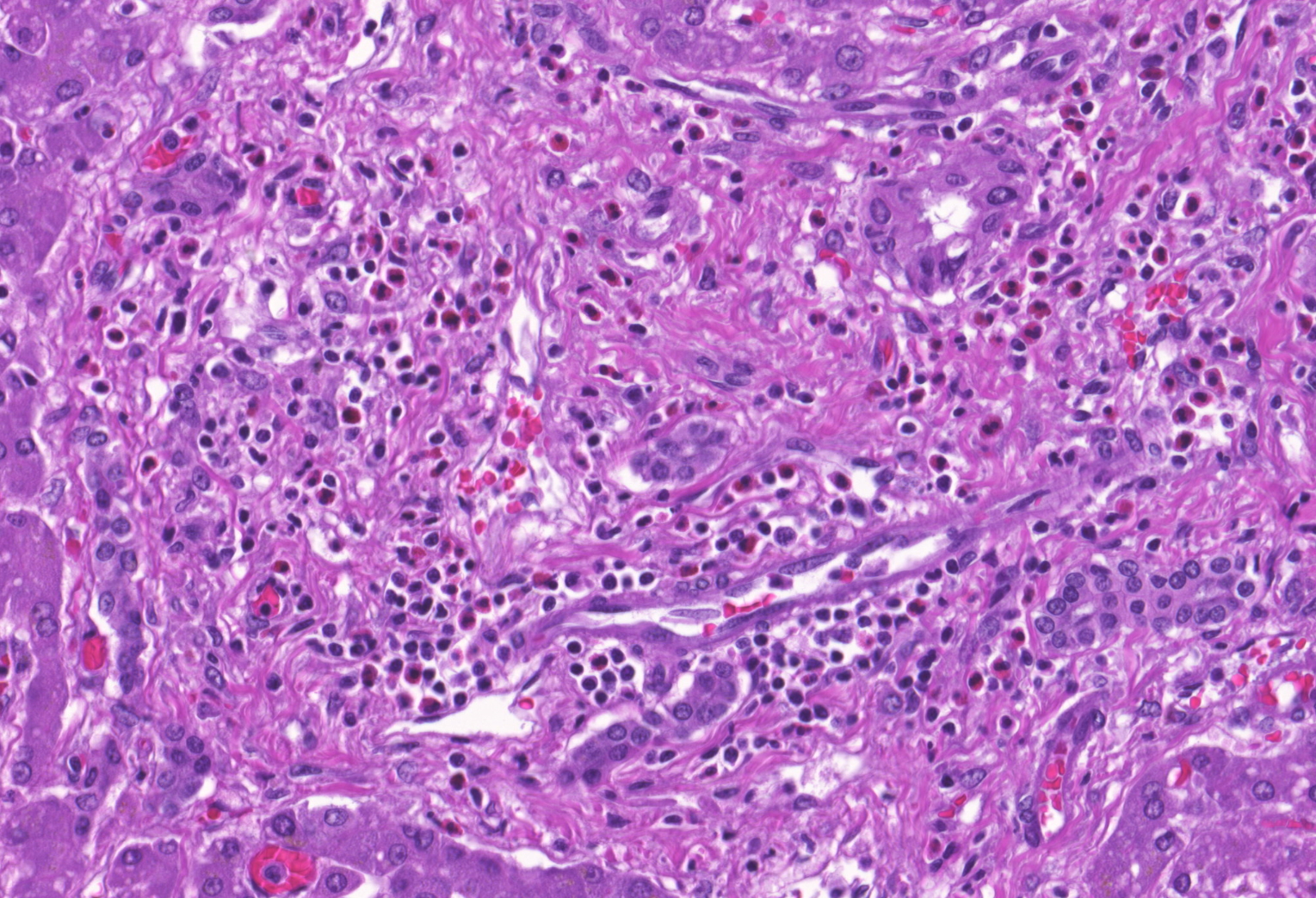
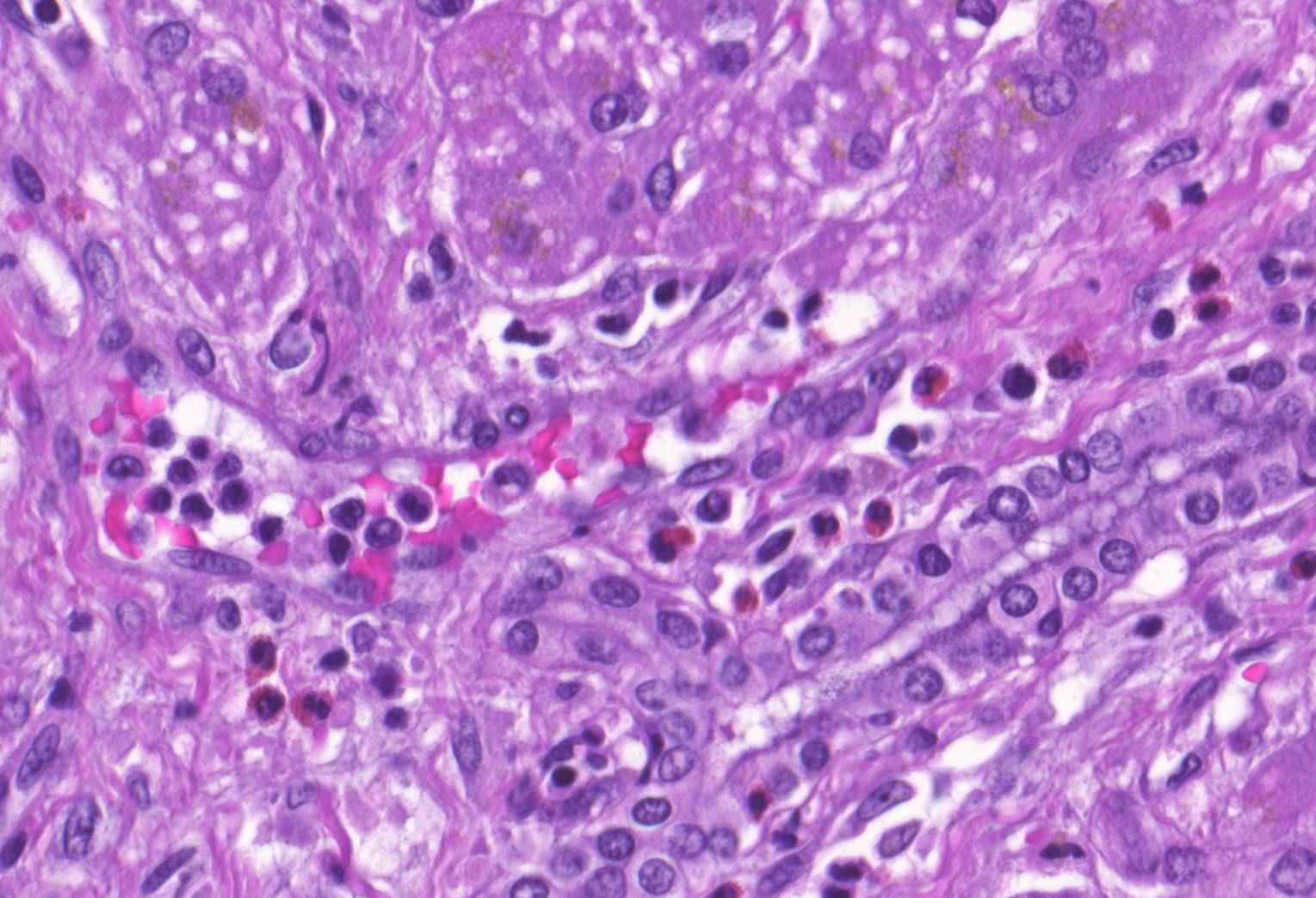
Microscopic (histologic) description
- Hyperacute rejection:
- Portal edema, necrosis, neutrophilic infiltration and ductular reaction
- Platelet fibrin thrombi in sinusoidal spaces, portal veins and central veins
- Hepatocyte necrosis, hemorrhage and (if untreated) confluent necrosis
- Necrotizing arteritis
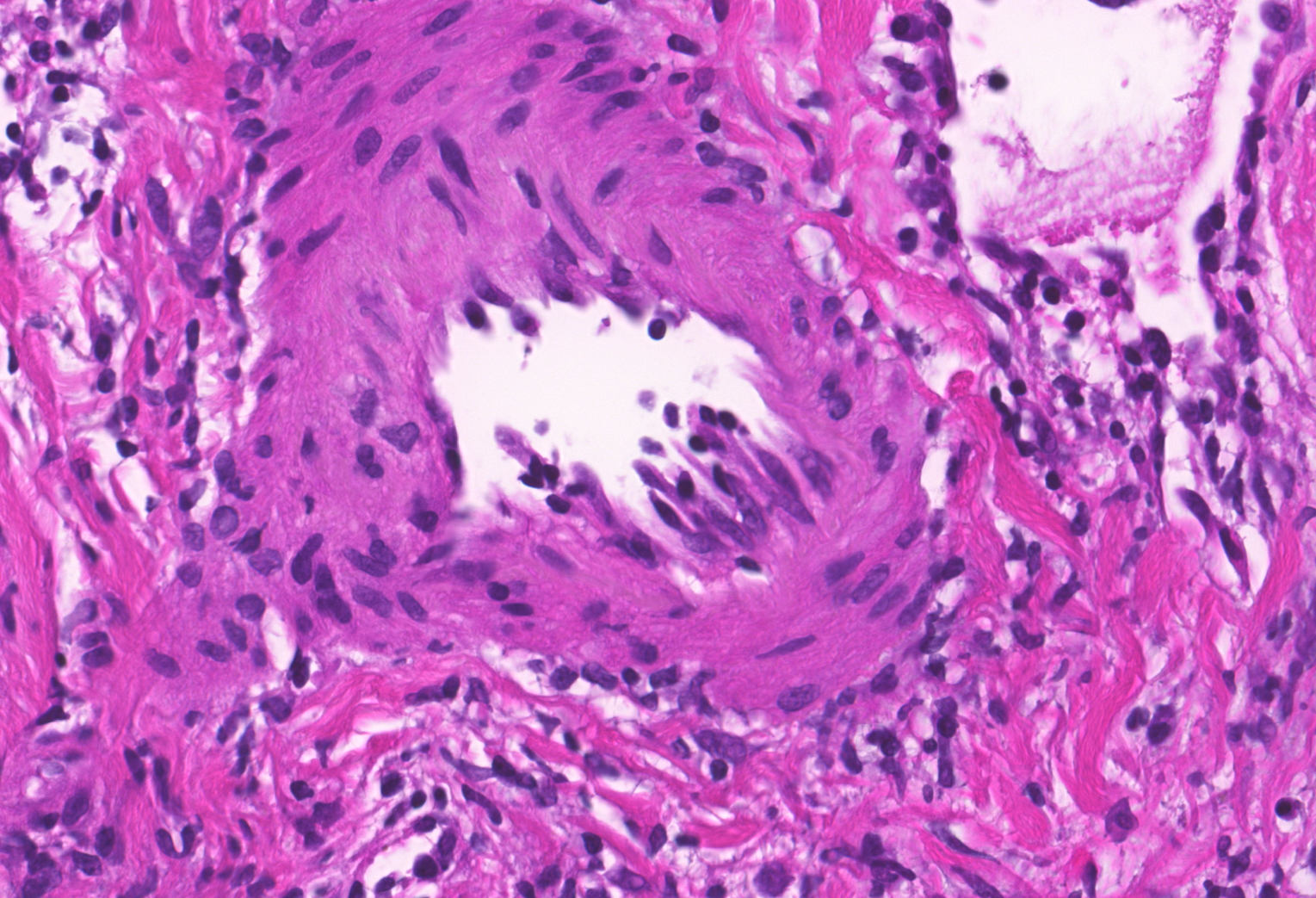
- Acute antibody mediated rejection:
- Microvascular injury with endothelial swelling, dilated capillaries and inlet venules and marginating leukocytes (eosinophils, neutrophils, monocytes, lymphocytes, macrophages)
- Ductular reaction and cholestasis
- Arteritis
- May coexist with TCMR
- Histopathologic lesions are scored based on criteria described by the Banff working group (Am J Transplant 2016;16:2816):
| h score | Histologic criteria |
| h score 1 | Portal microvascular endothelial cell enlargement (portal veins, capillaries and inlet venules) involving a majority of portal tracts with sparse microvasculitis defined as 3 - 4 marginated or intraluminal monocytes, neutrophils or eosinophils in the maximally involved capillary with generally mild dilation |
| h score 2 | Monocytic, eosinophilic or neutrophilic microvasculitis / capillaritis, defined as at least 5 - 10 leukocytes marginated or intraluminal in the maximally involved capillary, prominent portal or sinusoidal microvascular endothelial cell enlargement involving a majority of portal tracts or sinusoids, with variable but noticeable portal capillary and inlet venule dilatation and variable portal edema |
| h score 3 | As above, with marked capillary dilatation, marked microvascular inflammation (10 or more marginated or intraluminal leukocytes in the most severely affected vessels), at least focal microvascular disruption with fibrin deposition and extravasation of red blood cells into the portal stroma or space of Disse (subsinusoidal space) |
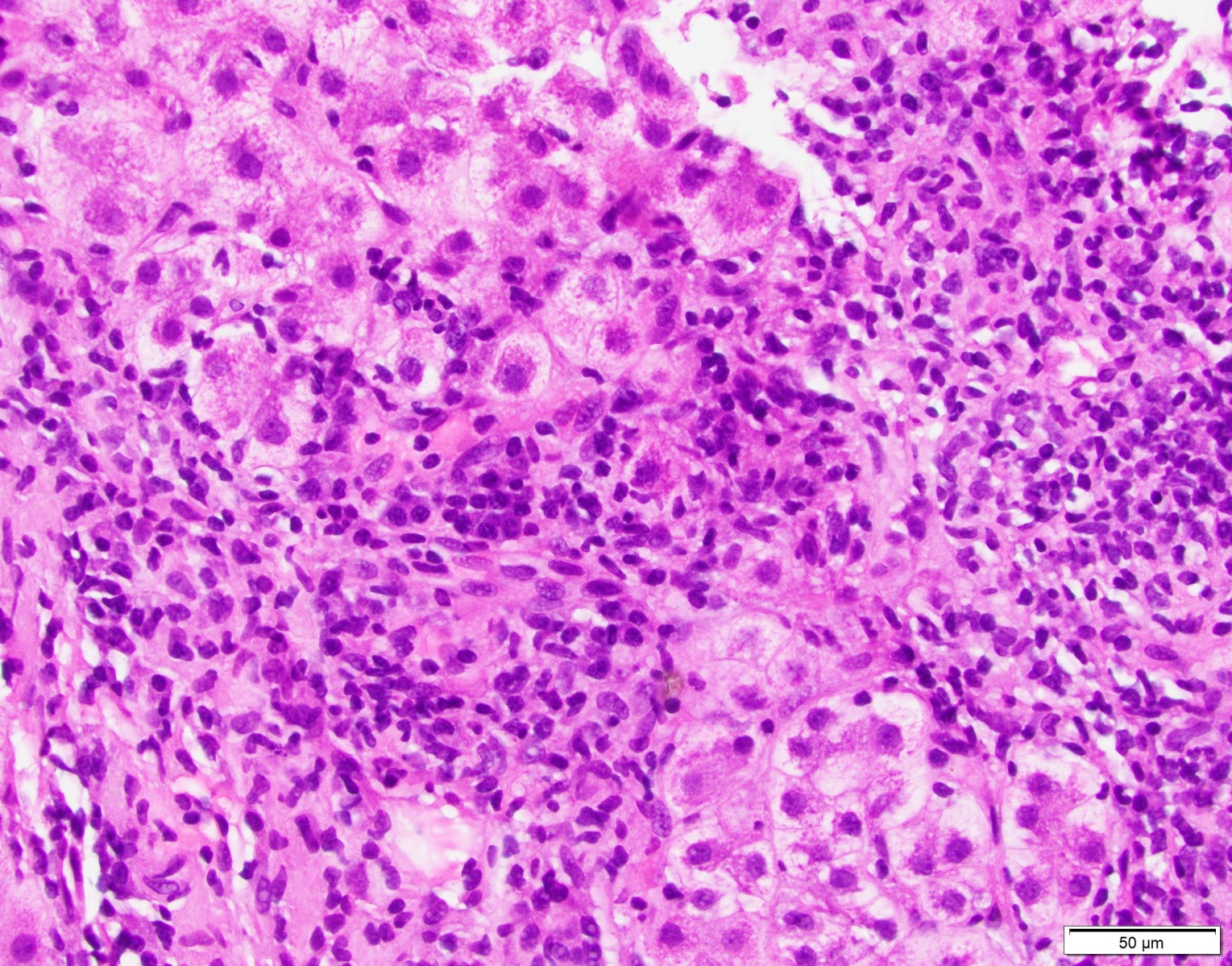
- Plasma cell rich rejection (de novo autoimmune hepatitis / plasma cell hepatitis) must meet criteria 1 and 3, criterion 2 is desirable (Am J Transplant 2016;16:2816):
| Criteria for plasma cell rich rejection | |
| 1 | Plasma cell rich (> 30%) portal or perivenular infiltrates with easily identifiable interface and perivenular necroinflammatory activity; in most cases rejection activity index (RAI) score ≥ 5/9 |
| 2 | Lymphocytic cholangitis is usually present but not required for diagnosis |
| 3 | Original disease other than autoimmune hepatitis |
Microscopic (histologic) images
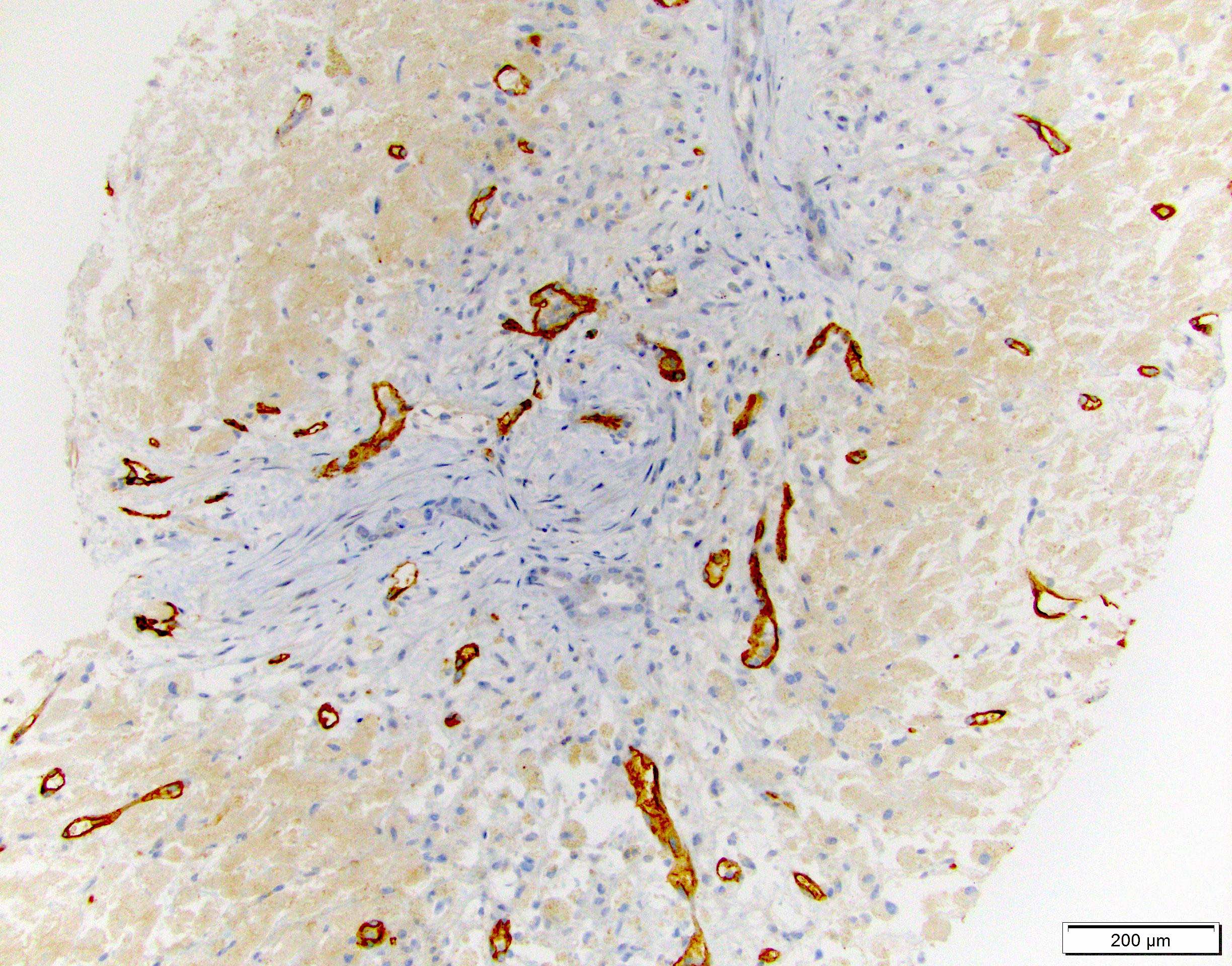
Immunofluorescence description
- C4d on frozen tissue has been used in liver but not very commonly; described as sinusoidal deposits (Liver Transpl 2012;18:641)
- C4d on paraffin tissue is more practical and accessible (see below)
Positive stains
- C4d on paraffin tissue is a successful method for screening and diagnosing AMR in liver allografts (Hum Pathol 2018;73:144)
- To consider a portal tract positive, C4d has to be deposited in > 50% of the circumference of portal microvascular endothelium (portal vein and capillaries)
- C4d immunohistochemistry (performed on paraffin tissue) is scored based on criteria described by the Banff working group (Am J Transplant 2016;16:2816):
C4d score Criteria 0 No C4d deposition in portal microvasculature 1 Minimal: < 10% of portal tracts 2 Focal: 10 - 50% portal tracts 3 Diffuse: > 50% of portal tracts; often with extension; often with extension
into inlet venules and periportal sinusoids
- IgG4 positive plasma cells are increased in plasma cell rich variant
Negative stains
- CK7 and copper stains are generally used to screen and rule out biliary pathology
Sample pathology report
- Liver allograft, needle biopsy:
- Acute antibody mediated rejection with active intimal arteritis
- Portal capillary dilatation, endothelial cell hypertrophy and capillaritis (Banff h score 2/3)
- C4d on paraffin tissue: diffuse uptake by portal microvasculature (Banff C4d score 3/3)
- Liver allograft fibrosis score (Am J Transplant 2012;12:2986):
- Mild portal fibrosis (1/3)
- Moderate subsinusoidal fibrosis (2/3)
- Mild perivenular fibrosis (1/3)
- Acute antibody mediated rejection with active intimal arteritis
Differential diagnosis
- Preservation / reperfusion injury:
- It can be difficult to distinguish early aAMR from reperfusion injury
- aAMR is favored if there is diffuse endothelial cell enlargement, diffuse C4d uptake and portal or perivenular inflammation
- Suboptimal biliary drainage:
- It is occasionally difficult to distinguish aAMR from biliary obstructive changes; both entities can show portal based neutrophilic inflammation, ductular reaction and cholestasis
- aAMR shows endothelial cell hypertrophy and intraluminal leukocyte margination
- Positive C4d, negative CK7 and negative copper stain help rule out imparied biliary drainage
- Recurrent hepatitis C virus infection:
- Small for size syndrome (SFSS):
- Seen in reduced size partial liver allografts (e.g. living donor transplantation / split liver allograft), due to persistent portal vein hypertension and hyperperfusion
- Usually occurs in setting of less than 0.8% graft to recipient body weight ratio
- Occurs early and similarly to early aAMR presents with hyperbilirubinemia and coagulopathy
- Histologically, aAMR shows distinctive capillaritis and C4d uptake distinguishing those two entities
- In aAMR patients are usually sensitized
Additional references
- Am J Transplant 2018;18:1604, Am J Transplant 2015;15:1003, Liver Transpl 2014;20:218, Liver Transpl 2014;20:200, Liver Transpl 2013;19:1001, Liver Transpl 2012;18:984, Curr Opin Organ Transplant 2015;20:314, Curr Opin Organ Transplant 2012;17:280, Transplantation 2017;101:2399, Pediatr Transplant 2017 Feb [Epub ahead of print]
Board review style question #1
- A 60 year old woman, 2 months post living donor liver transplantation from her son presented with jaundice, elevated transaminases and elevated bilirubin. A biopsy showed moderate T cell mediated rejection (TCMR) and the patient received steroids with no significant improvement. Assessment of pretransplant workup showed that the patient is sensitized and had a positive crossmatch. Posttransplant workup showed persistent Donor specific antibodies (multiple specificities, sum MFI 36,928). Imaging studies showed intact biliary tree and normal vascular flow. A repeat biopsy showed capillaritis, portal edema and focal luminal arteritis. According to Banff criteria, what else is needed to establish a definite diagnosis of acute antibody mediated rejection (aAMR)?
- Banff criteria is met, the patient can be diagnosed with acute antibody mediated rejection (aAMR) and no additional requirements are needed
- Diffuse C4d uptake by portal microvasculature (C4d score 3)
- IgG4 staining and quantification of positive plasma cells
- Presence of central perivenulitis and cholestasis
Board review style answer #1
B. Diffuse C4d uptake by portal microvasculature. The patient otherwise met all criteria for a diagnosis of acute antibody mediated rejection (aAMR): 1) Evidence of histopathologic damage (capillaritis), 2) positive donor specific antibody (DSA), 3) reasonable exclusion of other causes by available diagnostic modalities (e.g. imaging) and finally 4) diffuse C4d uptake is needed to complete the criteria and establish the diagnosis. Increased IgG4 positive cells are seen in plasma cell rich rejection and are not part of the criteria in diagnosis of acute antibody mediated rejection (aAMR) or plasma cell rich rejection (Am J Transplant 2013;13:2966). Central perivenulitis and cholestasis can be seen with TCMR, aAMR and cAMR and are not part of the criteria. Central perivenulitis occurs most commonly with portal inflammatory changes but can also occur as an isolated lesion (Histopathology 2020;76:822).
Comment Here
Reference: Acute antibody mediated rejection including hyperacute rejection
Comment Here
Reference: Acute antibody mediated rejection including hyperacute rejection
Board review style question #2
- A 65 year old man underwent liver transplant for Hepatitis C virus (HCV) induced cirrhosis with prior history of interferon treatment. The patient's posttransplant history was complicated by two episodes of early T cell mediated rejection (TCMR). The patient is now 2 years posttransplantation and presents with allograft dysfunction. A biopsy showed portal inflammation with mild cholangitis, interface activity and central perivenulitis. Plasma cells were visibly abundant and constituted about 45% of the inflammation. Hepatitis C virus (HCV) RNA was undetectable. What is the correct diagnosis?
- Idiopathic posttransplantation hepatitis
- Plasma cell rich rejection
- Recurrent autoimmune hepatitis
- Recurrent Hepatitis C virus (HCV)
Board review style answer #2
B. Plasma cell rich rejection. The patient was transplanted for Hepatitis C virus (HCV) and treated with interferon (primary disease other than autoimmune hepatitis). While recurrent Hepatitis C virus (HCV) is a major differential, the central perivenulitis and negative RNA test essentially rule it out. Idiopathic posttransplantation hepatitis is a broad term used to describe chronic hepatitis changes in patients without clinical or serologic evidence of viral hepatitis, autoimmunity or drug induced liver injury (Liver Transpl 2001;7:285). More recently, however, late onset T cell mediated rejection (TCMR) and chronic active acute antibody mediated rejection (aAMR) have been identified as causes of chronic allograft inflammation and fibrosis (Gastroenterology 2018;155:1838, Liver Transpl 2016;22:1593, Liver Transpl 2009;15:S19, Liver Transpl 2018;24:897).
Comment Here
Reference: Acute antibody mediated rejection including hyperacute rejection
Comment Here
Reference: Acute antibody mediated rejection including hyperacute rejection