Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Etiology | Clinical features | Diagnosis | Radiology description | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Board review style question #1 | Board review style answer #1Cite this page: Gonzalez R. Hepatoportal sclerosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverhepatoportalsclerosis.html. Accessed January 13th, 2025.
Definition / general
- Portal vein abnormalities and bridging fibrosis, causing portal hypertension
Essential features
- Portal hypertension without overt liver failure
- Variety of portal vein changes may be seen histologically
Terminology
- Also called obliterative portal venopathy, noncirrhotic portal fibrosis (Semin Liver Dis 2002;22:59)
- It has recently been suggested that the term hepatoportal sclerosis be retired and replaced with portal vein stenosis and herniated portal vein depending on the particular histologic findings (Histopathology 2019;74:219)
- Sometimes considered synonymous with incomplete septal cirrhosis, although overall this finding is more favored to indicate regressed cirrhosis
Epidemiology
- Relatively uncommon in U.S. but more common in India (Hepatology 2011;54:1071)
Etiology
- Can be idiopathic
- Many cases likely due to extrahepatic or intrahepatic portal venous obstruction, mainly portal vein thrombosis
- Also linked to exposure to arsenic or vinyl chloride, didanosine in AIDS patients (Curr Opin Infect Dis 2011;24:12) and other medications
Clinical features
- Main finding is portal hypertension, without cirrhosis or liver dysfunction
- May occur in children (J Korean Med Sci 2013;28:1507)
Diagnosis
- Tissue generally required for diagnosis; on biopsy, findings are usually only suggestive of or consistent with the diagnosis, due to patchy nature of disease
Radiology description
- Caudate lobe hypertrophy and right hepatic lobe atrophy; advanced cases may show nodularity resembling cirrhosis (AJR Am J Roentgenol 2012;198:370)
Case reports
- 23 year old man with Crohn’s disease and mercaptopurine induced hepatoportal sclerosis (J Crohns Colitis 2013;7:590)
Treatment
- Patients may require anticoagulation if disease is secondary to portal vein thrombosis
Microscopic (histologic) description
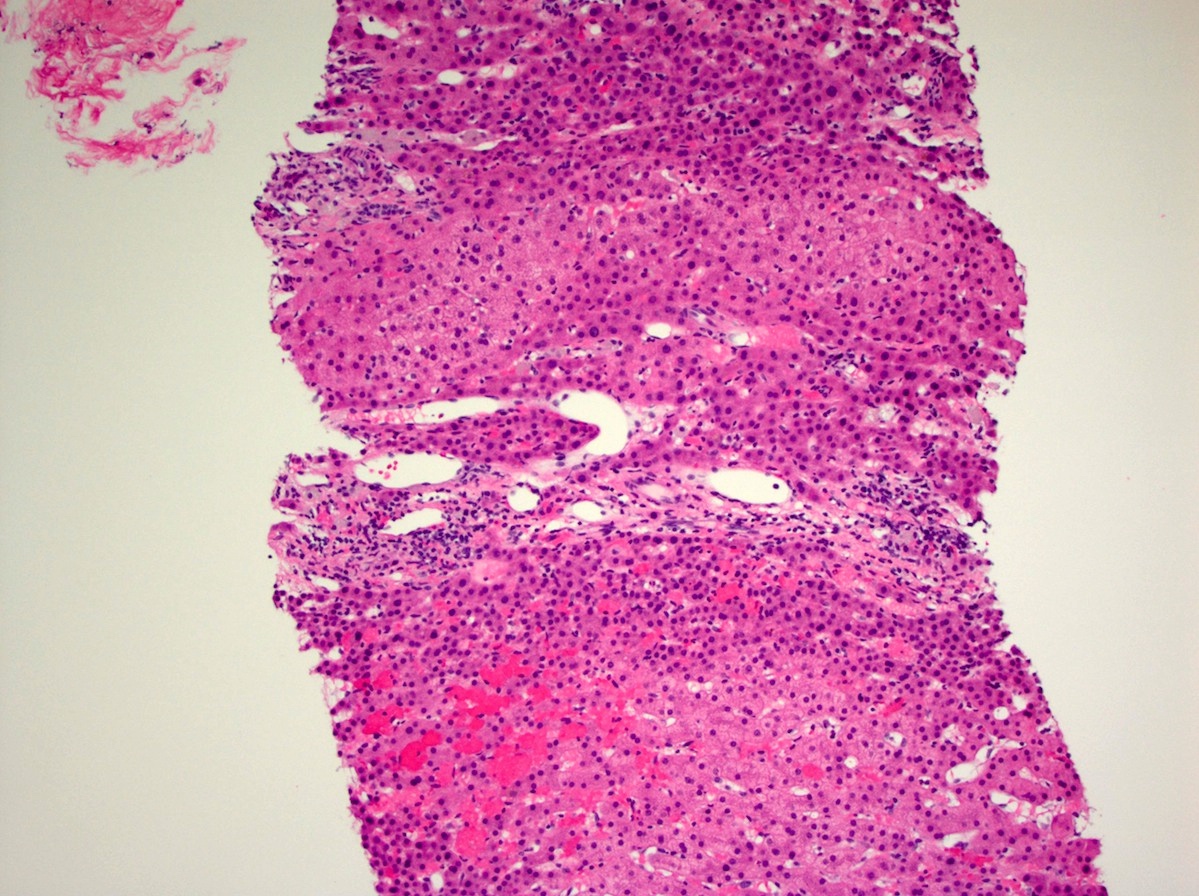
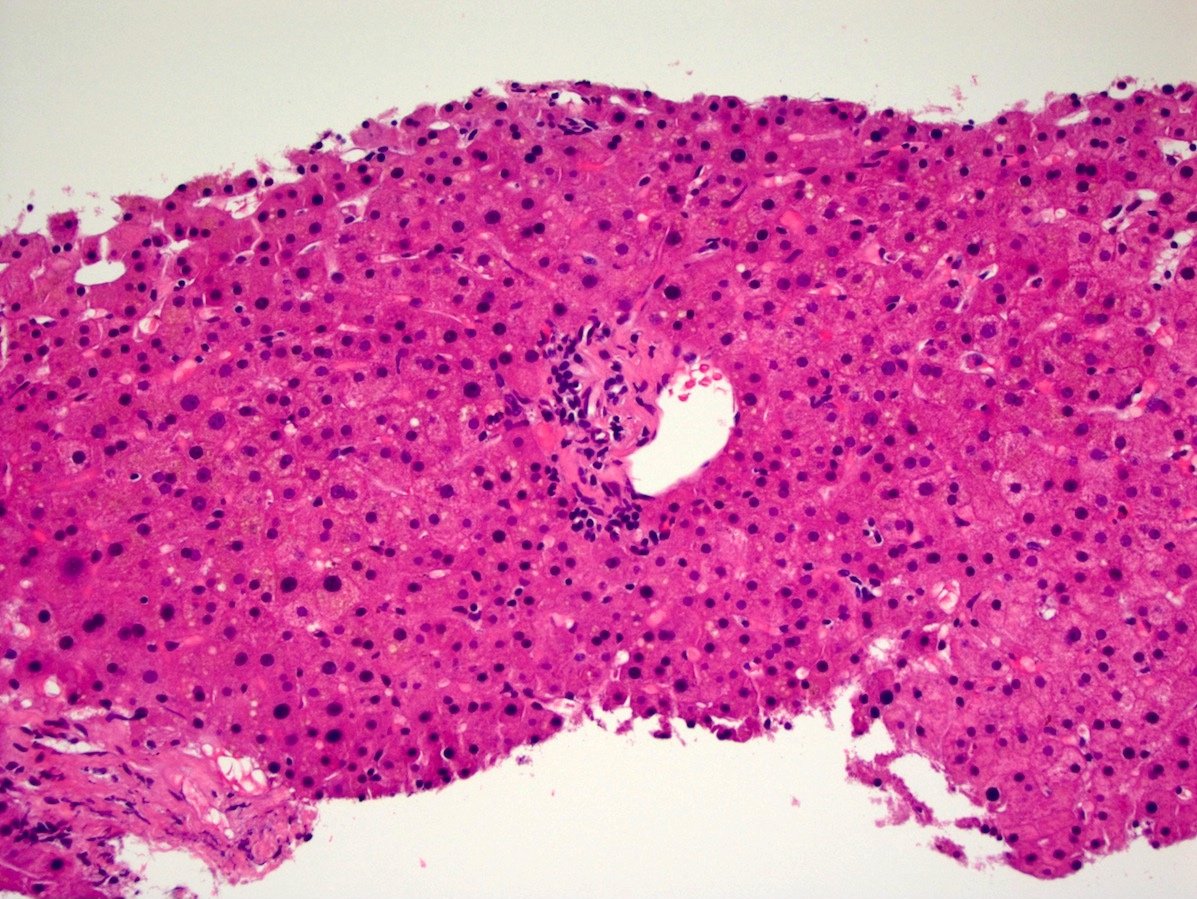
- Portal vein abnormalities, including fibrous intimal thickening, vein loss, herniation beyond portal tract borders into hepatic parenchyma and replacement by numerous small vein radicles
- Collagen deposition into space of Disse and periportal areas
- Bridging fibrosis between portal areas without background cirrhosis, although hepatocyte regeneration (nodular regenerative hyperplasia) may be present, as may parenchymal atrophy secondary to portal malperfusion
- Obliteration of portal veins has been specifically linked to didanosine (AIDS 2010;24:1171)
Microscopic (histologic) images
Sample pathology report
- Liver, biopsy:
- Liver parenchyma with herniated portal veins (see comment)
- Comment: The findings are indicative of so called hepatoportal sclerosis, which can cause noncirrhotic portal hypertension. Trichrome and iron stains are unremarkable.
Board review style question #1
- A 60 year old man in the United States with no known history of liver disease develops ascites and is discovered to have portal hypertension. He undergoes biopsy, which shows portal tract abnormalities but no cirrhosis. Additional workup determines he has Factor V Leiden. What is the most likely cause of the patient’s portal hypertension?
- Cirrhosis missed on biopsy
- Granulomatous hepatitis
- Hepatoportal sclerosis
- Schistosomiasis
- Sinusoidal obstruction syndrome
Board review style answer #1