Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Kikuchi A. Hepatitis C virus (HCV). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverhepC.html. Accessed April 1st, 2025.
Definition / general
- Infectious etiology of inflammatory liver injury from hepatitis C virus, a hepatotropic virus most commonly transmitted parenterally (IV drug use, needle stick)
- Untreated infections may progress to cirrhosis or develop into hepatocellular carcinomas requiring liver transplantation
Essential features
- Morphologic features include portal inflammation with interface activity, lobular necroinflammatory activity and portal based fibrosis
- Progressive fibrosis leads to cirrhosis (end stage liver disease) and possibly hepatocellular carcinoma
- Role of liver biopsy is grading and staging and to exclude other disease process
- Recurrent hepatitis C can occur in posttransplant livers and can mimic acute cellular rejection
Terminology
- Historical terms (not specific for HCV) (Am J Surg Pathol 1995;19:1409)
- Chronic persistent hepatitis (CPH)
- Chronic active hepatitis (CAH)
- Chronic lobular hepatitis (CLH)
ICD coding
- ICD-10
- ICD-11
Epidemiology
- Global prevalence of viremic HCV (HCV RNA positive) is estimated to be 1% (Lancet Gastroenterol Hepatol 2017;2:161)
- Increasing incidence of acute HCV infections attributed to injection drug use in young individuals in the U.S. (Clin Infect Dis 2014;59:1411)
- Genotypes 1 and 3 are the most common cause of infections (44% and 25%, respectively) (Lancet Gastroenterol Hepatol 2017;2:161)
- Historically recurrent in almost all liver allografts in patients who are HCV RNA positive at time of liver transplantation (Liver Transpl 2008;14:S36)
- Alcoholic liver disease increases risk of developing chronic HCV infection (unclear pathogenic mechanism)
- 10 - 20% of patients with chronic HCV develop cirrhosis after 20 - 30 years; 1 - 5% develop hepatocellular carcinoma (MMWR Recomm Rep 1998;47:1, Hepatology 2008;47:1128)
- Risk factors for disease progression: male sex, 40 years of age or older at time of infection, alcohol intake > 50 g daily, activity or steatosis on biopsy, coinfection with HBV or HIV, insulin resistance (Gastroenterology 2008;134:1699)
- Direct acting antivirals (DAAs) associated with improved clinical outcomes
- Increased sustained virologic response rates (SVR ≥ 95%, see Treatment) compared to interferon / ribavirin based regimens (Curr Epidemiol Rep 2017;4:174)
- Improved posttransplant survival, decreased waitlist mortality and liver transplant listing for HCV (Transpl Int 2019;32:854)
Sites
- Primary site: liver parenchyma
- Extrahepatic manifestations (J Clin Transl Hepatol 2019;7:172)
- Hematologic (mixed cryoglobulinemia, immune thrombocytopenia, autoimmune hemolytic anemia, increased risk of B cell non-Hodgkin lymphoma)
- Endocrine (diabetes mellitus, insulin resistance, thyroid dysfunction)
- Skin (porphyria cutanea tarda, lichen planus)
- Cardiovascular (polyarteritis nodosa, leukocytoclastic vasculitis, myocarditis, cardiomyopathies)
- Kidney (membranoproliferative glomerulonephritis, membranous glomerulonephritis)
Pathophysiology
- HCV life cycle tightly linked to hepatocyte lipid metabolism (J Hepatol 2014;61:S3)
- HCV assembly / release connected to fatty acid pathways and biogenesis of very low density lipoprotein (VLDL)
- Spontaneous resolution of acute infection in 15 - 45% of individuals (Gastroenterol Clin North Am 2015;44:717, Clin Liver Dis 2005;9:383)
- Chronic infection in remaining individuals if not treated / clinically undetected
- Predominantly immune response mediated injury
- Direct viral cytotoxic effect uncertain
- Innate immune system response to HCV infection
- Type I or type III interferon driven response, interferon stimulated genes and NK cells (Cells 2019;8:376)
- Partially controls viral replication but does not eliminate infection
- Adaptive immune response
- Neutralizing antibodies target hypervariable envelope glycoproteins E1 and E2 but are short lived and nonpersistent in chronic infection (Cells 2019;8:376)
- HCV specific CD8+ T lymphocytes mediate viral clearance through cytolytic and noncytolytic functions (J Gastroenterol Hepatol 2008;23:1473)
- Primed by HCV specific CD4+ T lymphocytes (Gastroenterology 2007;132:654)
- Vigorous, sustained cytotoxic T lymphocyte response needed for resolution of acute infection and permanent clearance
- Genotype 3 HCV infection independently associated with steatosis, directly steatogenic through alterations in hepatic lipid metabolism (Liver Int 2011;31:23, World J Gastroenterol 2014;20:15233)
- Resolution of steatosis with antiviral therapy (J Hepatol 2004;40:484, Gut 2004;53:420)
Etiology
- Spherical, enveloped, single stranded RNA virus
- Genus Hepacivirus
- Flaviviridae family
- Sequence heterogeneity with 6 major genotypes (types 1 - 6)
- Most common subtypes in the U.S. are 1a, 1b, 2, 3 (J Clin Gastroenterol 2019;53:40, Gastroenterology 2006;131:478)
- Transmission
- IV drug use
- Vertical (perinatal)
- Sexual (low compared to HBV, HIV)
- Transfusion (low risk with donor screening)
Diagrams / tables
Batts-Ludwig grading and staging of chronic hepatitis
| Grading | Staging | |||||
| Semiquantitative | Descriptive | Interface activity | Lobular activity | Semiquantitative | Descriptive | Criteria |
| 0 | Portal inflammation only (no activity) | None | None | 0 | No fibrosis | Normal connective tissue |
| 1 | Minimal | Minimal; patchy | Minimal; occasional hepatocyte apoptosis | 1 | Portal fibrosis | Fibrous portal expansion |
| 2 | Mild | Mild; involving some or all portal tracts | Mild; little hepatocellular damage | 2 | Periportal fibrosis | Periportal or rare portal - portal septae |
| 3 | Moderate | Moderate; involving all portal tracts | Moderate; with noticeable hepatocellular damage | 3 | Septal fibrosis | Fibrous septa with architectural distortion; no obvious cirrhosis |
| 4 | Severe | Severe; may have bridging necrosis | Severe; with prominent diffuse hepatocellular damage | 4 | Cirrhosis | Cirrhosis |
- Batts-Ludwig grading and staging system is simpler and more routinely used in clinical practice compared to the Ishak modified hepatic activity index (HAI) (Am J Surg Pathol 1995;19:1409, Clin Exp Med 2023;23:273)
Ishak modified hepatitis activity index (HAI) grading and staging of chronic hepatitis
| Necroinflammatory score | Portal inflammation | Interface hepatitis | Confluent necrosis | Focal (spotty) lytic necrosis and focal inflammation | Modified staging | Descriptive |
| 0 | None | Absent | Absent | Absent | 0 | No fibrosis |
| 1 | Mild (some or all portal areas) | Mild (focal, few portal areas) | Focal | 1 focus or less per 10x objective | 1 | Fibrous expansion of some portal areas, with or without short fibrous septa |
| 2 | Moderate (some or all portal areas) | Mild to moderate (focal, most portal areas) | Zone 3 necrosis in some areas | 2 - 4 foci per 10x objective | 2 | Fibrous expansion of most portal areas, with or without short fibrous septa |
| 3 | Moderate to marked (all portal areas) | Moderate (continuous around < 50% of tracts or septa) | Zone 3 necrosis in most areas | 5 - 10 foci per 10x objective | 3 | Fibrous expansion of most portal areas with occasional portal - portal bridging |
| 4 | Marked (all portal areas) | Severe (continuous around > 50% of tracts or septa) | Zone 3 necrosis + occasional portal - central bridging | > 10 foci per 10x objective | 4 | Fibrous expansion of portal areas with marked bridging (portal - portal, portal - central) |
| 5 | Zone 3 necrosis + multiple portal - central bridging | 5 | Marked bridging (portal - portal or portal - central) with occasional nodules (incomplete cirrhosis) | |||
| 6 | Panacinar or multiacinar necrosis | 6 | Cirrhosis, probable or definite |
- Ishak modified hepatitis activity index (HAI) was published in 1995 as a modification of the original Knodell system (1981)
- It is still commonly used in therapeutic trials as it includes semiquantitative evaluation of necroinflammatory activity and provides a numerical value
- Original system included adding both the necroinflammatory and fibrosis parameters to produce a numerical score; however, in practice, a modified HAI (mHAI) is produced by separately reporting the sum of necroinflammatory scores (0 - 18) and the fibrosis stage (J Hepatol 1995;22:696, Clin Exp Med 2023;23:273)
Images hosted on other servers:
Clinical features
- Often asymptomatic
- Nonspecific symptoms: fatigue, fever, headache, malaise, anorexia, nausea / vomiting, abdominal pain, diarrhea
- Spontaneous resolution of HCV infection in 15 - 45% of individuals (Gastroenterol Clin North Am 2015;44:717, Clin Liver Dis 2005;9:383)
- Patients with chronic infection may develop cirrhosis and clinical sequelae (hepatomegaly, ascites, clotting deficiency, esophageal / cutaneous varices)
- Extrahepatic manifestations
- Mixed cryoglobulinemia, glomerulonephritis, porphyria cutanea tarda, polyarteritis nodosa, Sjögren syndrome, lichen planus (Case Reports Hepatol 2021;2021:8244432, J Community Hosp Intern Med Perspect 2022;12:53, Am J Transplant 2021;21:2895, Mol Genet Metab 2019;128:282, Cureus 2023;15:e44129, Cureus 2021;13:e20091, Ann Saudi Med 2005;25:243)
- Selective clonal B cell activation may be related to development of B cell lymphomas (World J Gastroenterol 2016;22:6214, Blood Rev 2002;16:119)
Diagnosis
- Acute phase rarely diagnosed (asymptomatic)
- Chronic infection (> 6 months) often diagnosed during serologic workup of elevated transaminases
- Initial screening for anti-HCV antibodies (standard or rapid immunoassay)
- Positivity does not distinguish between current and previous infections
- HCV RNA assays
- Real time PCR or transcription mediated amplification (TMA)
- Detection confirms present infection
- Quantitative and qualitative tests; quantitative tests can measure baseline viral load
- HCV core antigen test
- Resource limited settings where nucleic acid tests not available
- Liver biopsy performed infrequently for primary diagnosis but can serve the following purposes (N Engl J Med 2017;377:756)
- Grading (activity) and staging (fibrosis) of liver (Mod Pathol 2007;20:S3)
- Diagnosis / exclusion of other injury etiologies (e.g., autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis, metabolic dysfunction associated steatotic liver disease)
- Evaluation of suspicious lesions / masses
Laboratory
- Aminotransferase levels (ALT, AST) typically elevated
- Anti-HCV antibody immunoassay and HCV RNA detection by real time PCR or TMA (see Diagnosis)
- Autoantibodies may be detected: antinuclear antibodies (ANA), anti-liver kidney microsomal antibody (anti-LKM), anti-smooth muscle, antithyroid antibodies (BMJ Open Gastroenterol 2018;5:e000203, Biomed Pharmacother 1999;53:234)
Radiology description
- MRI and CT findings in cirrhosis (Radiopaedia: Cirrhosis [Accessed 17 May 2024])
- Surface / parenchymal nodularity
- Hypertrophy of caudate lobe and lateral segments of left lobe
- Atrophy of posterior segments of the right lobe
- Ultrasound findings in cirrhosis
- Surface nodularity
- Coarse and heterogeneous texture
- Segmental hypertrophy / atrophy (described above)
- Doppler flow changes (portal hypertension)
- Enlargement of portal vein, superior mesenteric vein or splenic vein
- Slowing or reversal of portal venous flow
- Portal venous thrombosis with or without cavernous transformation
- Portosystemic collaterals
Radiology images
Prognostic factors
- Fibrosis is a major predictor of clinical outcomes, including liver related deaths and need for liver transplantation (Hepatology 2010;51:585, Intern Med J 2015;45:48)
- Degree of inflammation (inflammatory score) corresponds to development of fibrosis (Pathol Int 2002;52:683)
- Human immunodeficiency virus (HIV) coinfection, hepatitis B virus (HBV) coinfection, alcohol use, hemochromatosis and minority status are associated with hepatitis C related deaths (Public Health Rep 2010;125:414, Ann Intern Med 2012;156:271)
- Steatosis and insulin resistance associated with more severe fibrosis, treatment failure (with pegylated interferon and ribavirin) and hepatocellular carcinoma (Liver Int 2011;31:23, Liver Int 2011;31:507)
Case reports
- 48 year old woman with hepatitis C infection and Sjögren syndrome (Cureus 2021;13:e20091)
- 48 year old woman with fibrosing cholestatic hepatitis versus acute cellular rejection following liver transplantation (ACG Case Rep J 2023;10:e01058)
- 55 year old man with hepatitis C induced mixed cryoglobulinemia (Case Reports Hepatol 2021;2021:8244432)
- 57 year old man with hepatitis C induced mixed cryoglobulinemia (J Community Hosp Intern Med Perspect 2022;12:53)
- 60 year old woman with hepatitis C associated proliferative glomerulonephritis following liver transplantation from a hepatitis C positive antibody donor (Am J Transplant 2021;21:2895)
- 66 year old man with hepatitis C infection and polyarteritis nodosa (Cureus 2023;15:e44129)
Treatment
- Goal is eradication of HCV RNA and achieve sustained virologic response (SVR)
- SVR = undetectable viral level at 12 weeks following cessation of therapy
- Direct acting antiviral agents (DAAs)
- Acute and chronic infection
- Pangenotypic DAA regimens have high efficacy (SVR ≥ 95%)
- Prevent recurrent (posttransplant) hepatitis C in HCV viremic donors
- Examples of DAA regimens include sofosbuvir - velpatasvir and glecaprevir - pibrentasvir
- Historically, treatment included pegylated interferon alpha in combination with ribavirin
- High rate of side effects
- SVR rate ~30% (J Clin Transl Hepatol 2015;3:140)
Gross description
- Cirrhotic liver is firm and nodular
- Micronodular (uniform nodules, < 3 mm each), macronodular (irregular nodules, some > 3 mm) or mixed pattern (StatPearls: Hepatic Cirrhosis [Accessed 22 May 2024])
- Parenchyma can be dark red (normal), dark green (cholestasis) or pale yellow (steatosis or necrotic areas)
Gross images
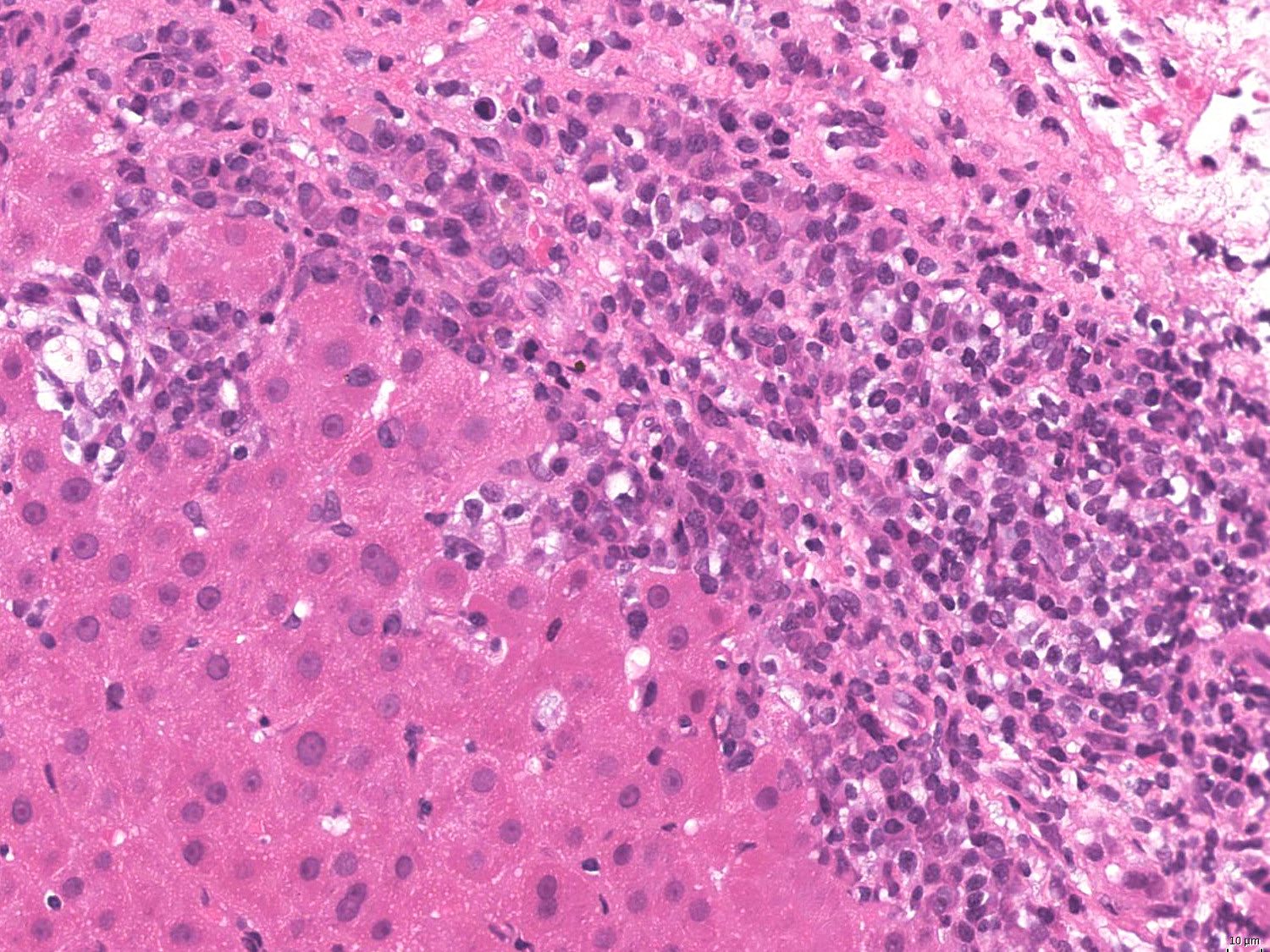
Microscopic (histologic) description
- See Diagrams for grading and staging criteria
- Chronic infection
- Portal based inflammation
- Predominantly lymphocytic
- Portal lymphoid aggregates
- With or without germinal centers
- Interface activity with necroinflammatory activity
- Swelling, eosinophilia and necrosis of periportal hepatocytes
- Bile duct changes
- Focal, mild lymphocytosis and reactive epithelial changes
- Mild damage, duct loss is rare
- Steatosis
- Mixed macro and microvesicular steatosis
- Lacks zonal distribution
- Usually mild (if severe or zone 3 restricted steatosis, consider metabolic dysfunction associated steatotic liver disease [MASLD])
- Lobular lymphocytic inflammation
- With or without spotty necrosis (acidophil bodies)
- Portal based fibrosis
- Progressive portal fibrosis expands portal tracts and forms stellated fibrous extensions / septa (stages 1 - 2, Batts-Ludwig methodology)
- Portal - portal, portal - central fibrous bridging (stage 3, Batts-Ludwig methodology)
- Cirrhosis (stage 4, Batts-Ludwig methodology)
- Frequently increased iron deposition
- Reticuloendothelial iron deposition, likely due to necroinflammatory activity
- Portal based inflammation
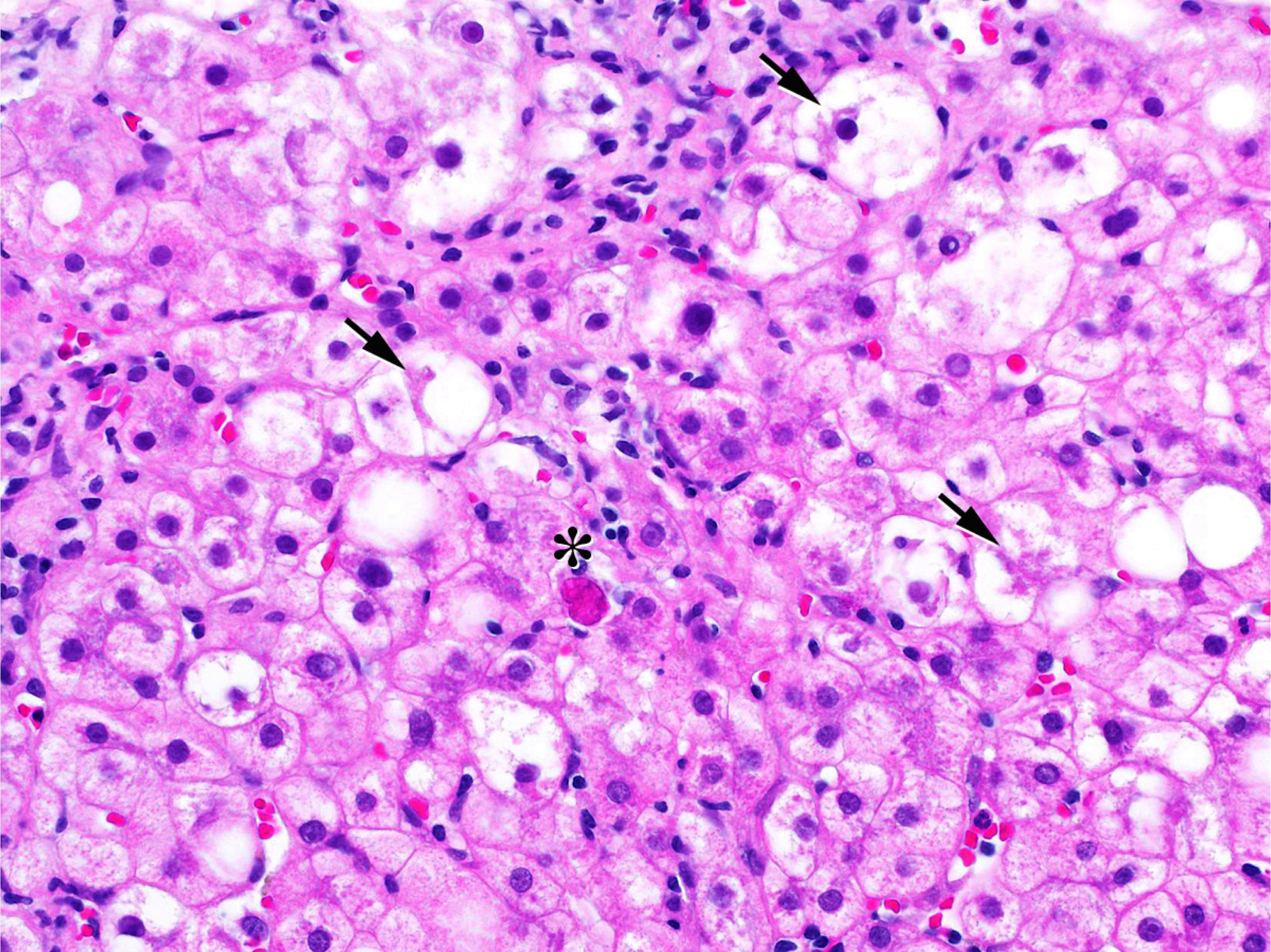
- Acute infection
- Predominantly lobular inflammation
- Lobular regeneration and disarray
- Hepatocellular apoptosis (swollen hepatocytes, acidophil bodies)
- Kupffer cell aggregates
- Multinucleated hepatocytes (giant cell change)
- Bridging / confluent necrosis
- Central - central or portal - central
- Hepatocyte death / dropout leaving loose stroma leading to architectural distortion, which can mimic cirrhosis
- Panlobular (massive) necrosis in severe cases
- Cholestasis
- Canalicular, bile plug formation, intracellular
- Recurrent hepatitis C (posttransplant)
- Similar to hepatitis C in native liver but histologic overlap with acute cellular rejection is a consideration
- Fibrosing cholestatic HCV: rare form of rapidly progressive cholestatic injury from recurrent hepatitis C
- Marked hepatocellular ballooning / swelling, hepatocanalicular cholestasis, ductular reaction and periportal or perisinusoidal fibrosis (Int J Clin Exp Pathol 2008;1:396, Ann Gastroenterol 2016;29:454, Am J Gastroenterol 2000;95:753)
- Cases also reported in association with HIV infection (Am J Gastroenterol 2002;97:478)
Microscopic (histologic) images
Contributed by Alexander Kikuchi, M.D., Ph.D.
Positive stains
- Trichrome: staging of portal fibrosis; also helpful to distinguish hepatic necrosis from established fibrosis
- Elastin and reticulin: useful in distinguishing hepatic necrosis from established fibrosis (Liver Int 2007;27:681)
- Elastin fibers are present in established fibrous septa but not in areas of recent parenchymal loss / necrosis
- Reticulin may highlight residual structure of cell plates in areas of necrosis that are not seen in established fibrosis
Negative stains
- PASD: negative for intracytoplasmic globules of alpha-1 antitrypsin deficiency
Molecular / cytogenetics description
- See information covered under Etiology, Diagnosis and Laboratory subsections
Videos
Overview of biology, pathophysiology and histopathology of viral hepatitis
Sample pathology report
- Liver, core biopsy:
- Active hepatitis with mild activity and periportal fibrosis (grade 2 of 4, stage 2 of 4, Batts-Ludwig methodology), consistent with hepatitis C (see comment)
- Comment: Sections of the biopsy contain approximately 12 portal tracts for evaluation. The portal areas show mild, predominantly lymphocytic inflammation with patchy interface activity and associated periportal hepatocellular swelling. One portal area contains a lymphoid aggregate. No significant ductular reaction is seen and interlobular bile ducts are intact. The lobular parenchyma shows mild inflammation with frequent spotty necrosis (acidophil bodies). No significant steatosis, cholestasis or viropathic changes are identified. A trichrome stain is performed and shows mild periportal fibrosis (stage 2, scale 0 - 4, Batts-Ludwig methodology). The overall findings are consistent with the provided clinical history of hepatitis C; however, other causes of hepatitis, including drug induced injury, other infectious etiologies (hepatotropic and nonhepatotropic viruses), Wilson disease and autoimmune hepatitis, should be excluded.
- Liver, core biopsy:
- Active hepatitis with mild periportal fibrosis; mild steatosis and centrizonal pericellular fibrosis (see comment)
- Comment: Sections of the biopsy contain approximately 18 portal tracts for evaluation. Prominent, dense lymphoid aggregates are noted within the portal tracts along with occasional plasma cells, eosinophils and histiocytes. Mild interface activity is seen as well as focal ductular reaction. The interlobular bile ducts are intact. The lobular parenchyma shows patchy inflammation with scattered spotty necrosis (acidophil bodies). Mild steatosis is present, involving approximately 30% of the sampled hepatic parenchyma. Occasional swollen hepatocytes are present but no definite ballooned hepatocytes are identified. No cholestasis or viropathic changes are identified. A trichrome stain highlights centrizonal, pericellular fibrosis as well as periportal fibrosis with septa formation. The overall findings are those of active hepatitis. Some of the histologic features, such as dense periportal lymphocytic inflammation with lymphoid aggregates and interface activity, are in keeping with the clinical history of hepatitis C. Other features, including the presence of steatosis and centrizonal pericellular fibrosis, may also raise consideration of prior steatohepatitic injury. By the Batts-Ludwig system of chronic hepatitis grading, the mild lobular and periportal inflammatory activity would be grade 2 (scale 0 - 4). The findings of centrizonal and periportal fibrosis with septal formation indicate stage 2 by either the Batts-Ludwig or modified Kleiner-Brunt methodology (scale 0 - 4).
Differential diagnosis
- HBV hepatitis:
- Serologic testing for hepatitis B markers
- May have ground glass hepatocytes (chronic infection; not specific for hepatitis B)
- Autoimmune hepatitis:
- Generally more severe hepatitis (interface activity, hepatocyte injury)
- Prominent plasma cells
- Serologic testing for autoantibodies
- Caveat: autoantibodies can be expressed in HCV; false positive anti-HCV has been reported in autoimmune hepatitis (Ann Intern Med 1992;116:21)
- Drug induced hepatitis:
- History of causative agent (drug / herbal supplement)
- Metabolic dysfunction associated steatotic liver disease (formerly nonalcoholic fatty liver disease):
- Ballooned hepatocytes
- Pericentral pericellular fibrosis
- Predominantly lobular inflammation
- Portal inflammation less pronounced (ranging from mild to focally moderate)
- Zone 3 predominant steatosis (rather than nonzonal distribution)
- Acute cellular rejection (transplant setting):
- Predominantly mixed portal inflammatory infiltrate (typically containing eosinophils)
- More prevalent duct injury or presence of true endothelial injury (not just passenger lymphocytes in subendothelial space)
- More rapid rise in liver function enzymes, negative viral load
- Both recurrent hepatitis C and acute cellular rejection can be present in same biopsy
- Primary biliary cholangitis:
- May demonstrate similar portal based inflammation with interface and lobular activity
- More prominent duct injury, eventual duct loss
- Florid duct lesions
- Elevated alkaline phosphatase (ALP), gamma glutamyl transferase (GGT), serum IgM and antimitochondrial autoantibodies
Additional references
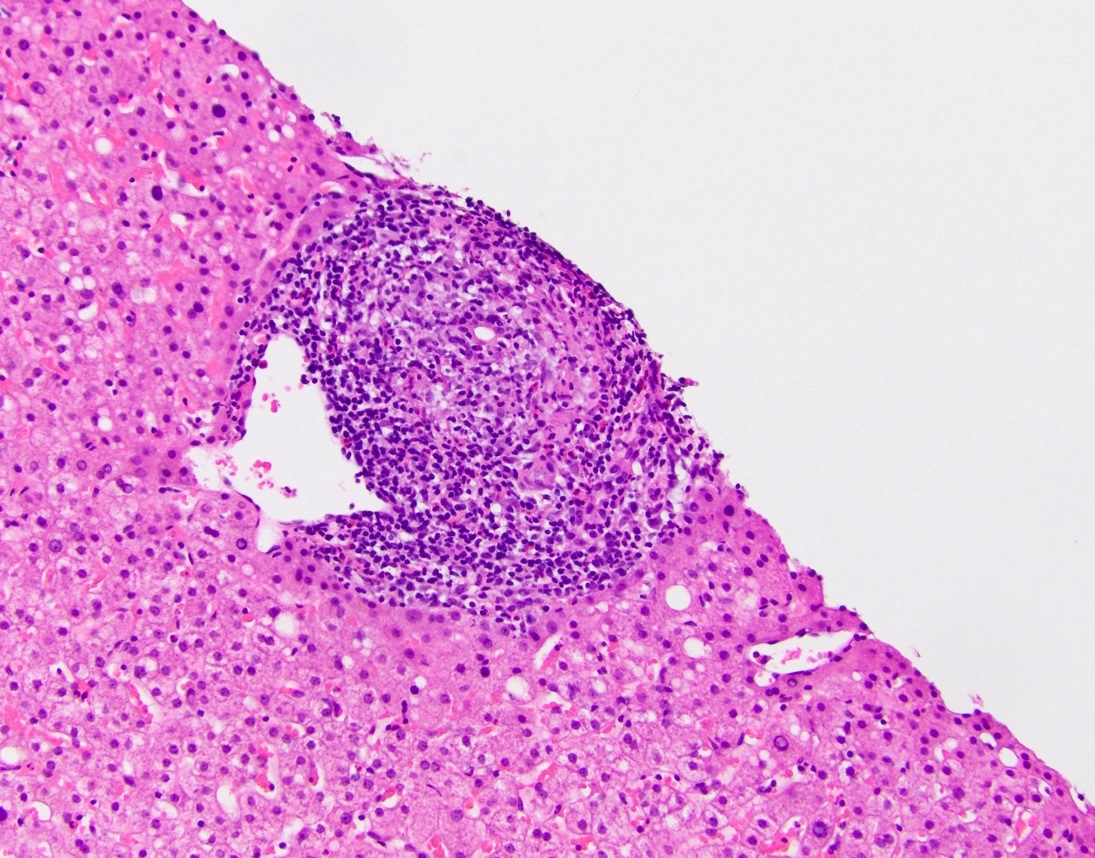
Board review style question #1
Board review style answer #1
D. Hepatitis C. The image shows a portal tract containing a lymphoid aggregate composed of a dense, relatively well circumscribed collection of lymphocytes. Occasionally these lymphoid aggregates may also contain a germinal center (not seen in this example). This finding is characteristic (though not pathognomonic) for chronic hepatitis C infection.
Answer A is incorrect because autoimmune hepatitis is typically characterized by prominent portal plasma cells and the presence of a relatively discrete portal lymphoid aggregate is more suggestive of hepatitis C virus. Answer B is incorrect because features suggestive of chronic biliary obstruction including ductular reaction, cholestasis, duct injury or cholangitis are not identified. Answer C is incorrect because the histologic finding of a portal lymphoid aggregate is more characteristically seen in hepatitis C, although hepatitis B is an important differential diagnosis that should be clinically excluded. Hepatocytes with glassy eosinophilic cytoplasm (so called ground glass hepatocytes, not seen in this example) can also be seen in hepatitis B. Answer E is incorrect because although chronic hepatitis C is associated with non-Hodgkin B cell lymphomas, the findings in the current biopsy tract show a polymorphic appearing lymphoid aggregate without significant cytologic atypia or monomorphic appearance.
Comment Here
Reference: Hepatitis C virus (HCV)
Answer A is incorrect because autoimmune hepatitis is typically characterized by prominent portal plasma cells and the presence of a relatively discrete portal lymphoid aggregate is more suggestive of hepatitis C virus. Answer B is incorrect because features suggestive of chronic biliary obstruction including ductular reaction, cholestasis, duct injury or cholangitis are not identified. Answer C is incorrect because the histologic finding of a portal lymphoid aggregate is more characteristically seen in hepatitis C, although hepatitis B is an important differential diagnosis that should be clinically excluded. Hepatocytes with glassy eosinophilic cytoplasm (so called ground glass hepatocytes, not seen in this example) can also be seen in hepatitis B. Answer E is incorrect because although chronic hepatitis C is associated with non-Hodgkin B cell lymphomas, the findings in the current biopsy tract show a polymorphic appearing lymphoid aggregate without significant cytologic atypia or monomorphic appearance.
Comment Here
Reference: Hepatitis C virus (HCV)
Board review style question #2
The liver from a 55 year old man with a known history of hepatitis C infection is shown above. If the findings in this image are representative of the remaining liver, what would be an appropriate grade and stage using Batts-Ludwig methodology for chronic hepatitis?
- Grade 1, stage 1
- Grade 1, stage 2
- Grade 2, stage 3
- Grade 2, stage 4
- Grade 4, stage 4
Board review style answer #2
D. Grade 2, stage 4. The image shows cirrhotic liver recognizable by the presence of thick, bridging fibrotic bands separating nodules of hepatocytes. Cirrhosis is stage 4 (highest available stage) using Batts-Ludwig methodology. Patchy, mild interface activity is seen without prominent, diffuse hepatocellular injury, making grade 2 (not grade 4 as listed in answer choice E) the more appropriate interpretation. Answer A is incorrect because the image shows cirrhotic liver (stage 4) and the inflammation is more appropriately categorized as mild (grade 2), not minimal (grade 1). Answers B and C are incorrect because the image shows cirrhotic liver (stage 4).
Answer E is incorrect because the image shows patchy, mild interface activity without prominent diffuse hepatocellular injury, making grade 2 (not grade 4) the more appropriate interpretation.
Comment Here
Reference: Hepatitis C virus (HCV)
Comment Here
Reference: Hepatitis C virus (HCV)