Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Aghighi M, Gonzalez RS. Glycogenic hepatopathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverglycogenichepatopathy.html. Accessed March 30th, 2025.
Definition / general
- Hepatomegaly, raised liver enzymes and abundant glycogen in hepatocytes related to uncontrolled diabetes mellitus
Essential features
- Mauriac syndrome: rare phenomenon in type 1 diabetics characterized by excessive hepatic glycogen deposition, elevated liver enzymes, hepatomegaly, obesity, cushingoid features and late puberty
- Presents with abdominal pain, hepatomegaly, nausea, vomiting and ketoacidosis
- Histologic correlate is glycogenic hepatopathy: diffuse pale appearance of hepatocyte cytoplasm and glycogenated hepatocyte nuclei
Terminology
- Hepatic / liver glycogenosis
- Diabetes mellitus associated glycogen storage hepatomegaly
- Mauriac syndrome: rare phenomenon in type 1 diabetics characterized by excessive hepatic glycogen deposition, elevated liver enzymes, hepatomegaly, obesity, cushingoid features and late puberty (Arch Dis Child 2014;99:354)
ICD coding
- ICD-10: E74.00 - glycogen storage disease, unspecified
Epidemiology
- Higher prevalence in diabetic patients, particularly type 1 diabetics (BMC Pediatr 2012;12:160)
- Mostly in children and young adults
- Slightly higher incidence in women (World J Hepatol 2018;10:172)
Sites
- Liver
Etiology
- Prolonged hyperglycemia due to uncontrolled diabetes mellitus leads to accumulation of glycogen in hepatocytes, resulting in hepatomegaly and elevation of liver enzymes (World J Hepatol 2018;10:172)
Clinical features
- Abdominal pain, hepatomegaly, nausea and vomiting, history of ketoacidosis
Diagnosis
- Clinical and pathological association is required for diagnosis
Laboratory
- Hyperglycemia
- Elevated transaminases or alkaline phosphatase
- Elevated hemoglobin A1C, which shows poor glycemic control (Clin Gastroenterol Hepatol 2017;15:927)
Radiology description
- Hyperdense liver on CT without contrast
Prognostic factors
- Good prognosis with medical treatment (World J Hepatol 2018;10:172)
- Blood sugar control helps to adjust liver enzymes and microscopic features (Saudi Med J 2017;38:89)
Case reports
- 15 year old boy with glycogenic hepatopathy (Case Reports Hepatol 2018;2018:6037530)
- 18 year old woman with diabetes and Mauriac syndrome (Case Rep Crit Care 2016;2016:6072909)
- 19 year old woman with diabetes and glycogenic hepatopathy (BMJ Case Rep 2019;12:e228524)
- 25 year old man with diabetes and suicide by high dose insulin presented with glycogenic hepatopathy (J Am Coll Emerg Physicians Open 2020;1:1097)
- 44 year old woman with diabetes and glycogenic hepatopathy (ACG Case Rep J 2018;5:e31)
Treatment
- Blood sugar control by adjusting insulin and diet (Saudi Med J 2017;38:89)
- Improvement of glycogenic hepatopathy observed after pancreatic transplantation in diabetic patients (Ann Hepatol 2012;11:554)
Gross description
- Not applicable, as liver transplantation is not indicated for this diagnosis
Microscopic (histologic) description
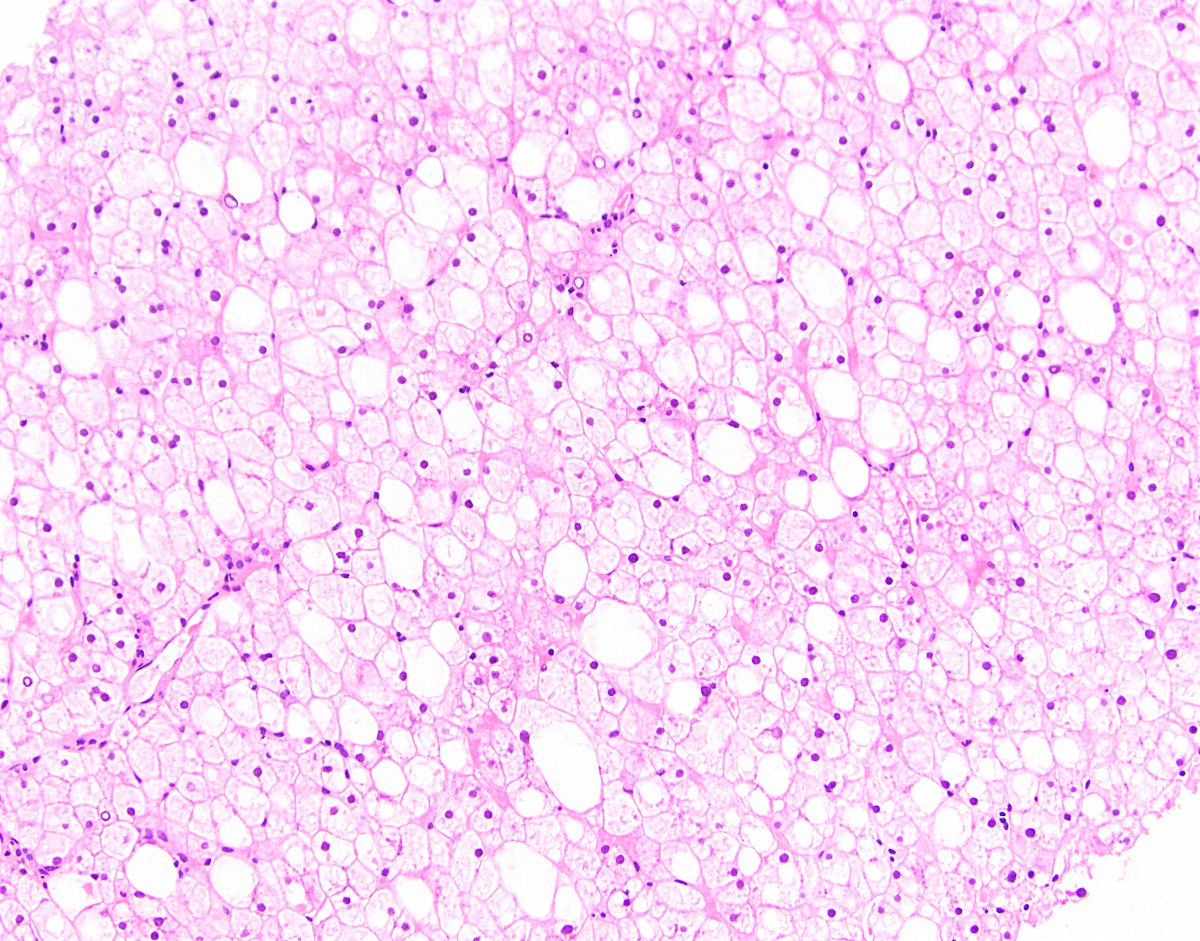
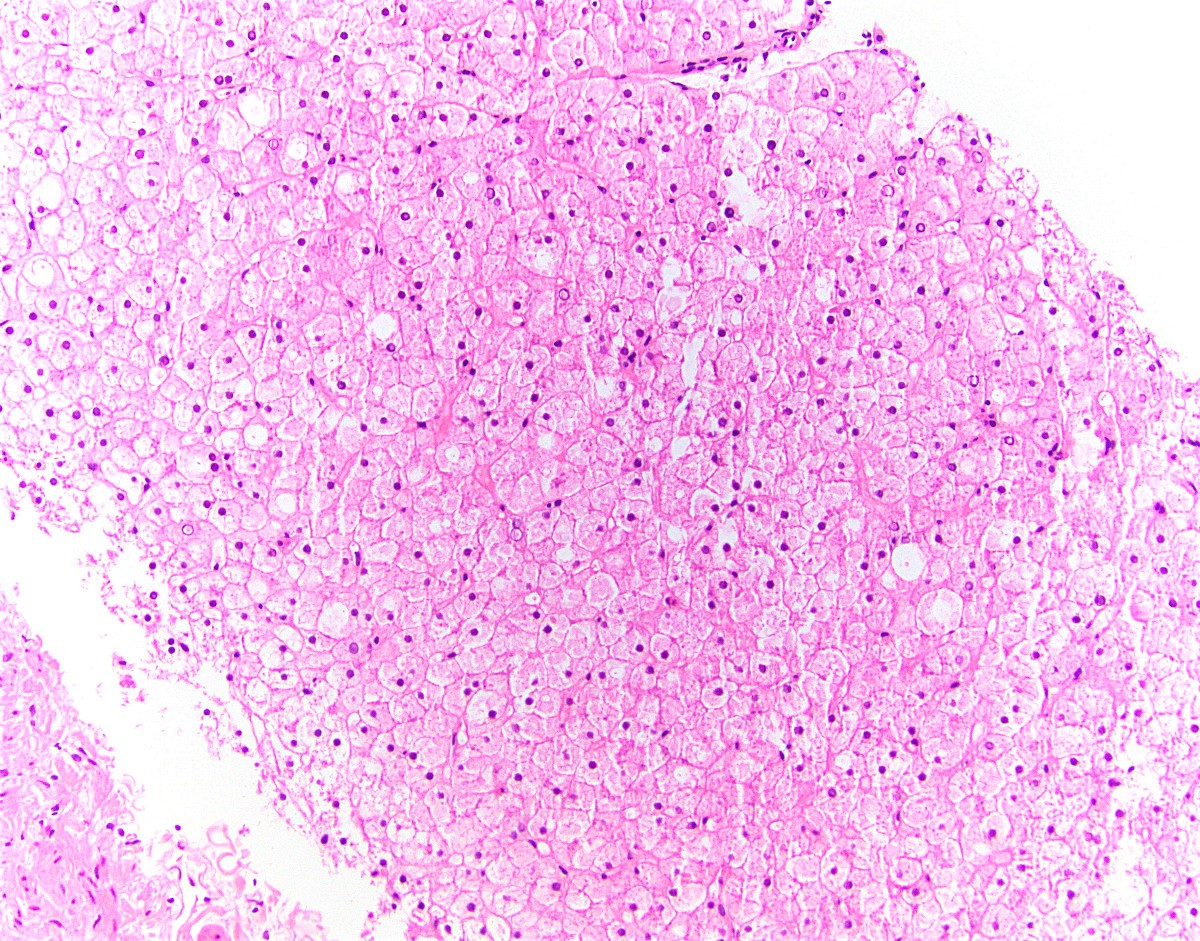
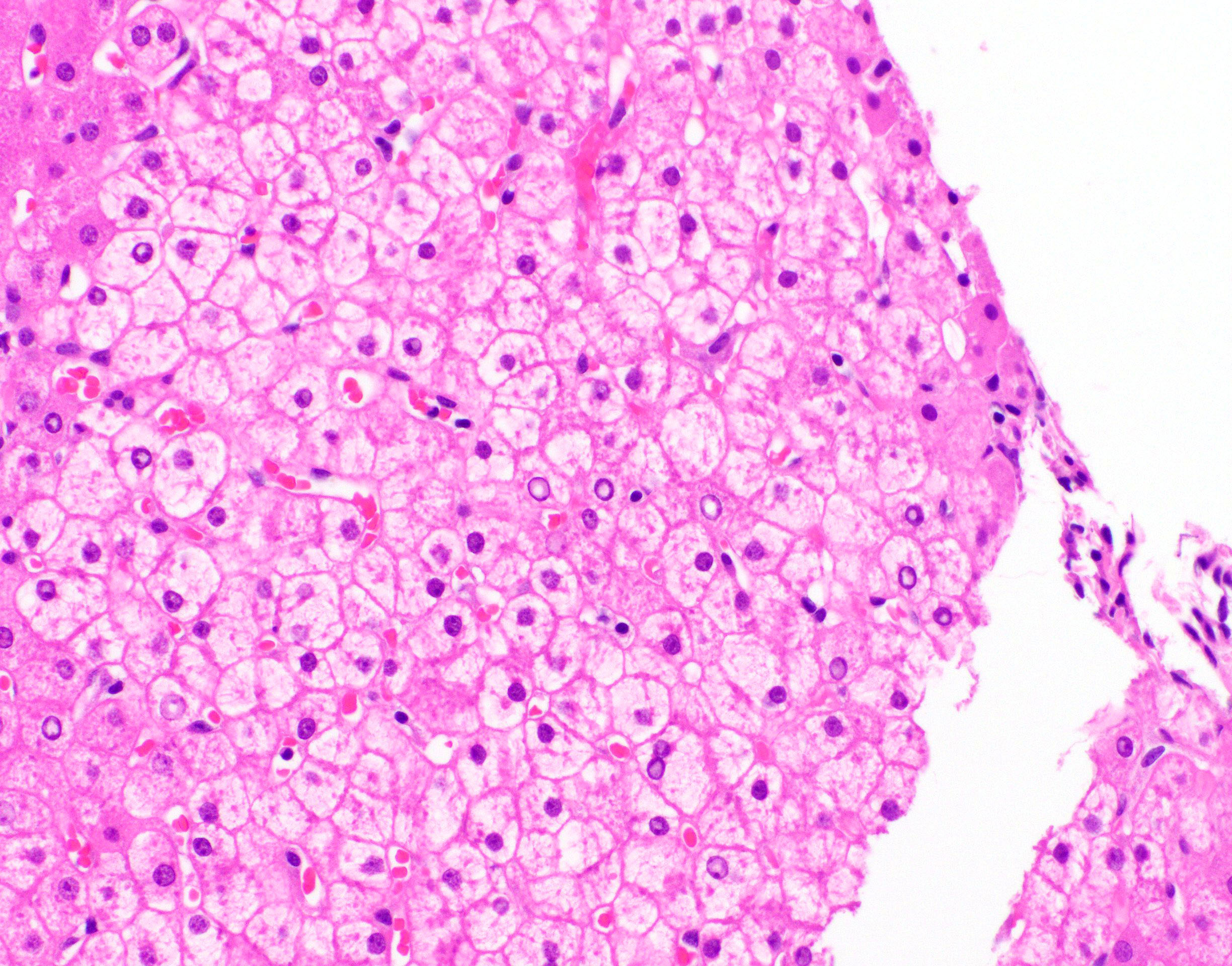
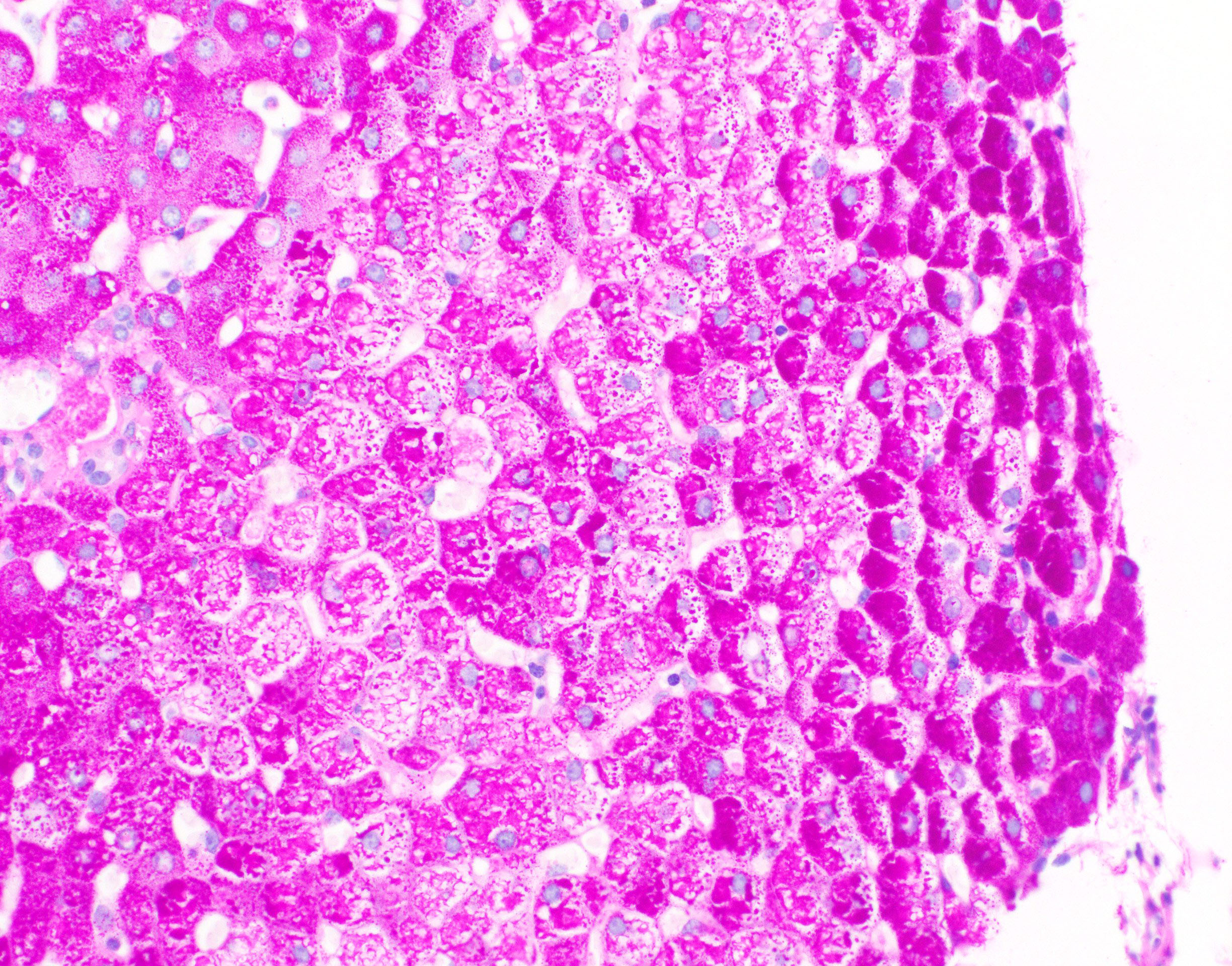
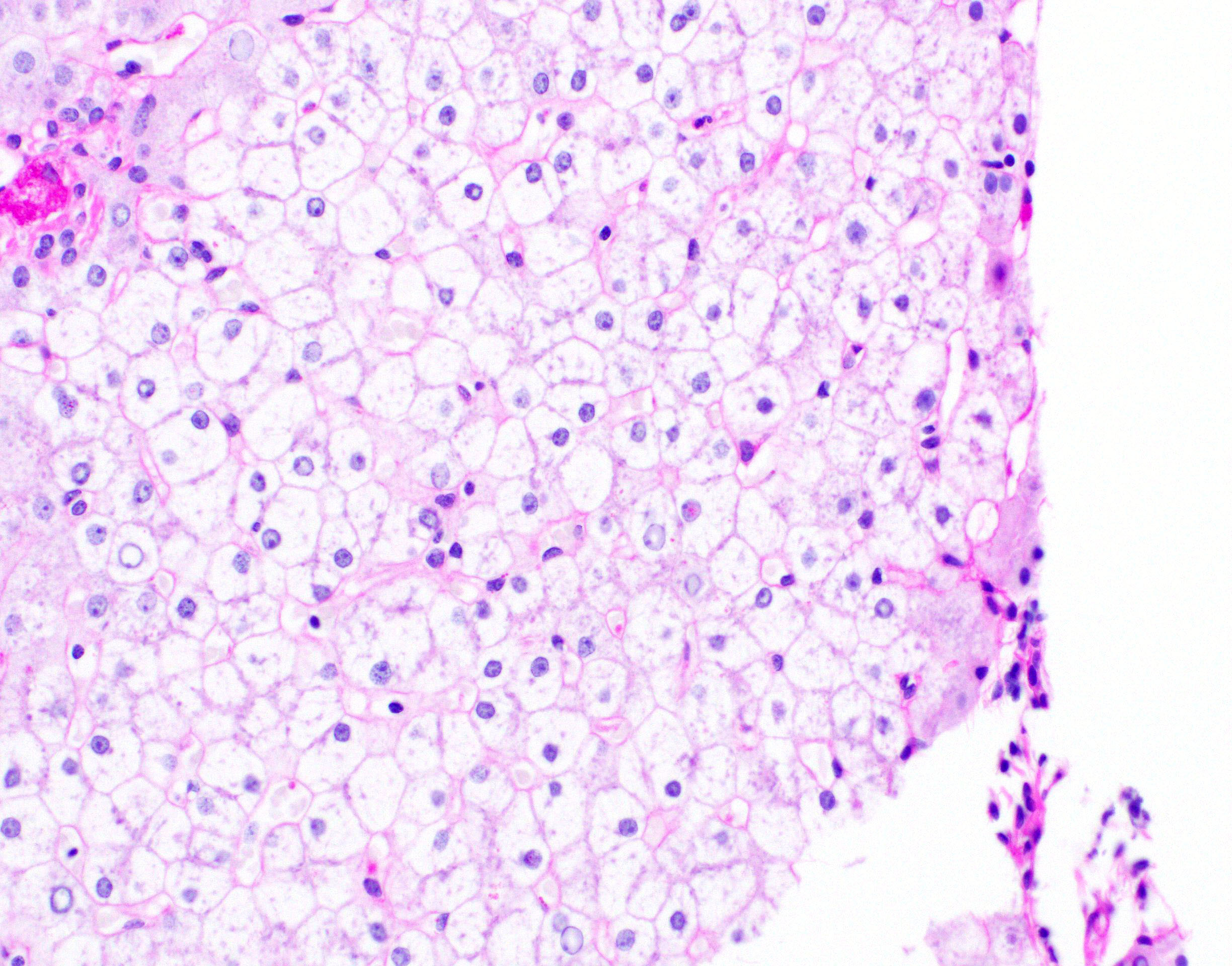
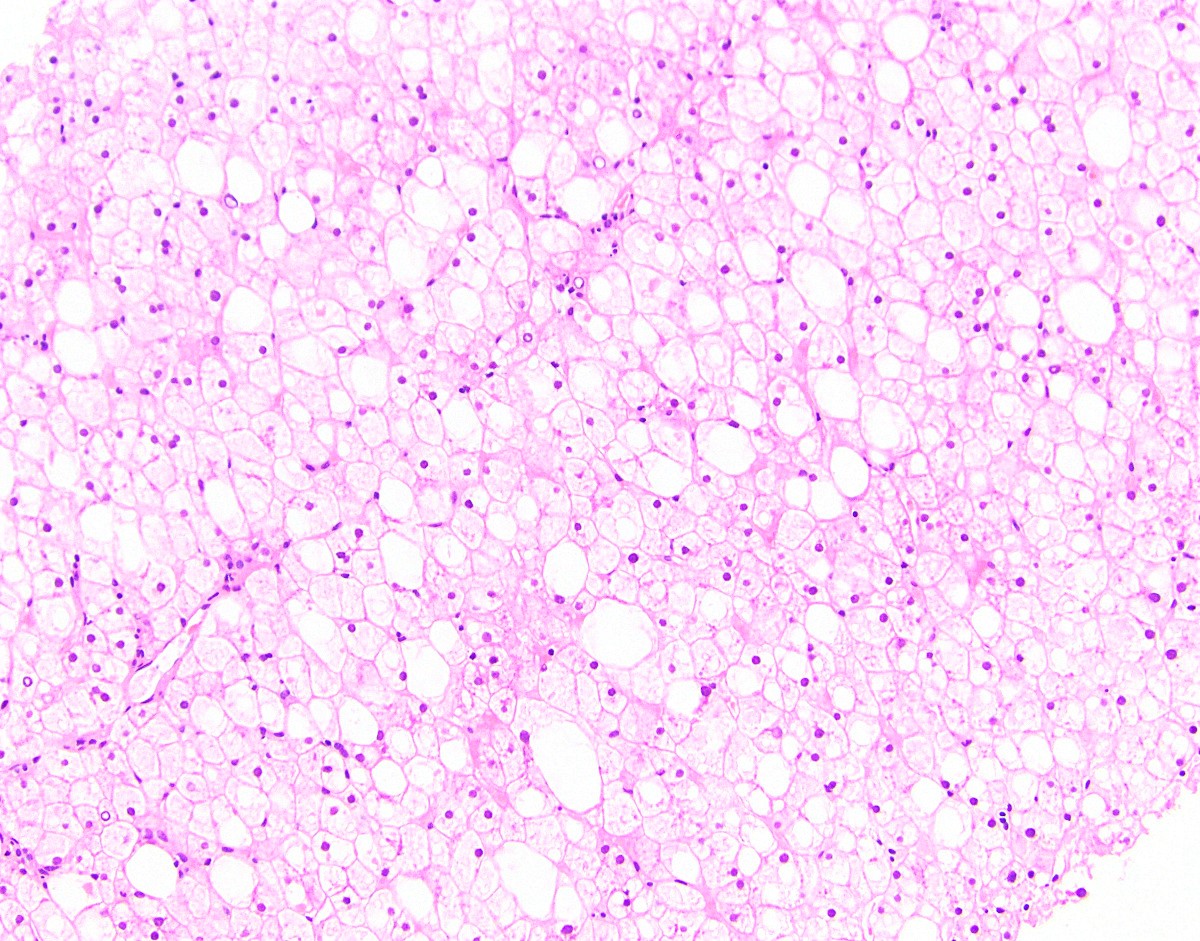
- Hepatocytes are enlarged / swollen with pale cytoplasm, glycogenated nuclei, giant mitochondria and accentuated cytoplasmic membranes (Am J Surg Pathol 2006;30:508)
- Mosaic appearance of parenchyma due to compression of sinusoids, resulting in a sheet-like appearance of the hepatocyte architecture
- Macrovesicular steatosis may be present
- No or minimal inflammation or fibrosis
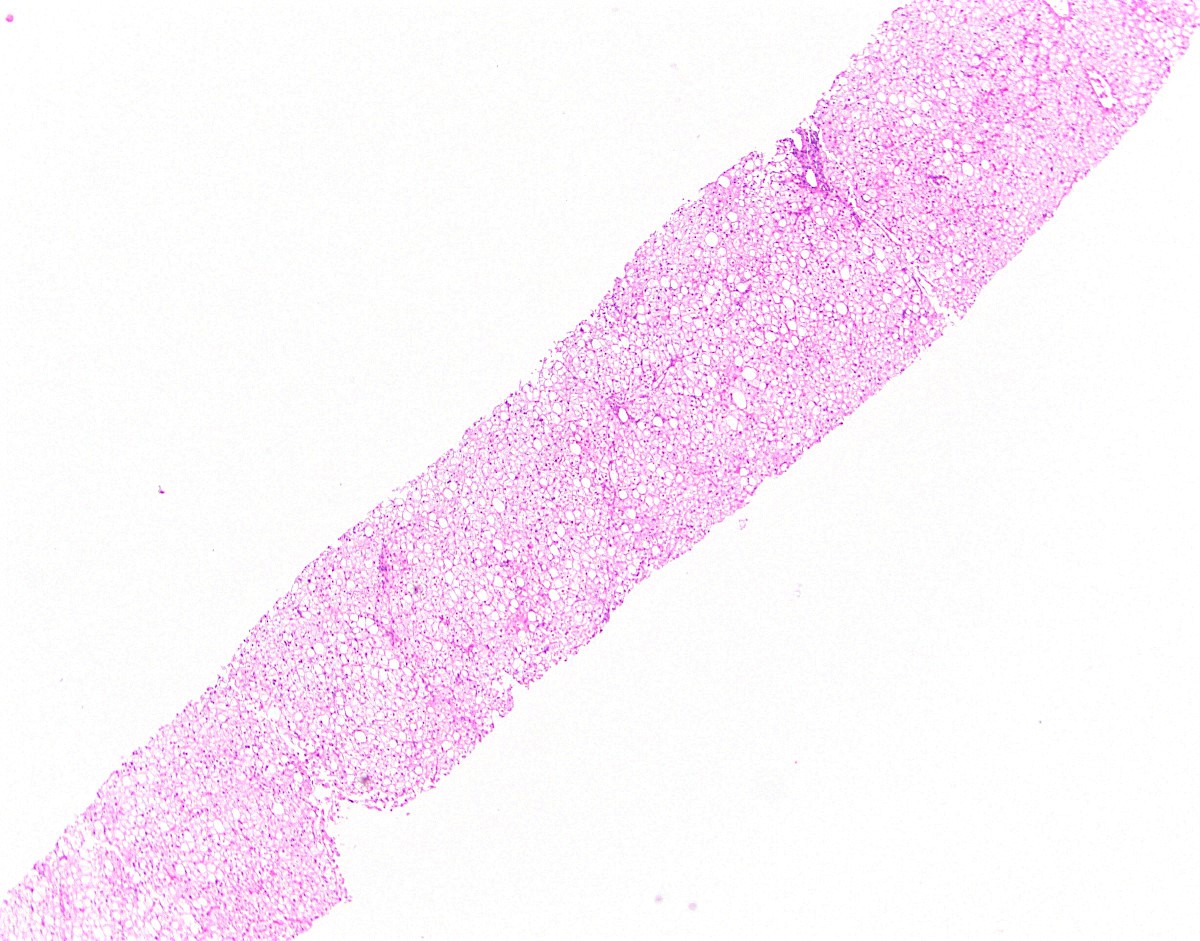
Microscopic (histologic) images
Positive stains
- PAS stain shows glycogen in hepatocytes
Negative stains
- PASD stain is unremarkable (glycogen is digested by diastase)
Electron microscopy description
- Excessive glycogen in hepatocyte cytoplasm and nuclei
Sample pathology report
- Liver, biopsy:
- Glycogenic hepatopathy (see comment)
- Comment: Sections show diffuse hepatocyte enlargement with pale cytoplasm and prominent cytoplasmic membranes. A PAS stain shows glycogen accumulation in hepatocytes. The findings are consistent with the reported history of poorly controlled type 1 diabetes. The differential diagnosis includes glycogen storage diseases.
Differential diagnosis
- Normal liver:
- Pale or enlarged hepatocytes can be confused with normal or fixation artifact
- Fatty liver disease:
- Predominant finding is macrovesicular steatosis; background hepatocytes may be ballooned or have giant mitochondria but this should not be diffuse
- Fatty liver disease also shows Mallory hyaline and zone 3 pericellular fibrosis
- Glycogen storage diseases:
- Inherited disease in children without diabetes history
- Liver enzyme deficiency (glucose 6-phosphatase catalytic activity)
- Mutations in G6PC or G6PT1 genes (EXCLI J 2019;18:30)
- Electron microscopy shows cytoplasmic inclusions consisting of fibrillar glycogen
Board review style question #1
A 15 year old boy with diabetes presented with nausea, vomiting and hepatomegaly. Lab testing reveals HbA1C = 11, aspartate aminotransferase (AST) = 130, alanine aminotransferase (ALT) = 146. Liver biopsy shows excessive glycogen accumulation in hepatocytes. Which of the following is the best initial management?
- Blood sugar control
- Interferon
- Liver transplant
- Pancreas transplant
Board review style answer #1
Board review style question #2
A 21 year old woman with insulin dependent diabetes mellitus presented with abdominal pain, ketoacidosis and hepatomegaly. Her liver biopsy demonstrated pale, enlarged hepatocytes that were strikingly positive on PAS stain. Which of the following is the most likely diagnosis?
- Alcoholic fatty liver disease
- Glycogen storage disease
- Glycogenic hepatopathy
- Hepatitis A
Board review style answer #2