Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Szeto W, Mannan R. Chronic viral hepatitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverchronicviralhep.html. Accessed April 3rd, 2025.
Definition / general
- Chronic viral hepatitis is defined as inflammation of the liver due to persistent viral replication for at least 6 months
- Inflammatory process results in progressive liver damage and fibrosis
Essential features
- Chronic viral hepatitis is commonly caused by 3 viruses: hepatitis B, hepatitis C and hepatitis D virus; other chronic viral hepatitides are less common
- Long term infection results in chronic inflammation of the liver parenchyma that is characterized by portal inflammation, interface hepatitis and fibrosis
- Progressive fibrosis may result in cirrhosis and increases risk for developing hepatocellular carcinoma
- Reference: Infect Dis Clin North Am 2019;33:1045
ICD coding
Epidemiology
- Chronic viral hepatitis is a major global public health problem that affects hundreds of millions of people
- An estimated 257 million people are living with chronic hepatitis B infection
- 71 million are living with chronic hepatitis C infection (Infect Dis Clin North Am 2019;33:1045)
- Results in long term liver inflammation that may lead to cirrhosis or hepatocellular carcinoma, causing an estimated 1.4 million deaths annually (Curr Opin HIV AIDS 2017;12:302)
- Hepatitis B virus (HBV) (JAMA 2018;319:1802, Infect Dis Clin North Am 2019;33:1045)
- Chronic HBV infection has high endemicity in Central and East Asia, sub-Saharan Africa and the Western Pacific Regions
- Transmitted through sexual contact, blood and vertically from mother to child
- HBV usually causes an acute hepatitis but chronic hepatitis develops in ~90% of infected infants versus ~10% of adult patients
- There are 8 genotypes (A - H) in humans; type A responds favorably to interferon based therapy and type C is associated with more advanced liver fibrosis and increased risk of hepatocellular carcinoma
- Up to 40% of untreated patients may develop cirrhosis
- Hepatitis C virus (HCV)
- Transmission is primarily bloodborne (Infect Dis Clin North Am 2019;33:1045)
- Increased risk of transmission via sexual intercourse is reported in HIV positive men who have sex with men (Infect Dis Clin North Am 2019;33:1045)
- Infection causes acute hepatitis and the virus is cleared in some (Nat Rev Dis Primers 2017;3:17006)
- Acute HCV infection leads to chronic HCV in 75% to 85% of people (Nat Rev Dis Primers 2017;3:17006)
- Percentage of transition to chronic infection is higher for patients coinfected with HIV and ~2.6 million people are estimated to be coinfected (Nat Rev Dis Primers 2017;3:17006)
- 10% to 30% of patients develop cirrhosis over 30 years (N Engl J Med 2011;364:2429)
- People with HCV cirrhosis have a 4% to 5% cumulative annual incidence of hepatocellular carcinoma (Nat Rev Dis Primers 2017;3:17006)
- Hepatitis D virus (HDV)
- HDV infection is higher in areas where HBV is endemic and transmission is similar to HBV (Gut 2021;70:1782)
- High prevalence areas include the Mediterranean region, Middle East, the Indian subcontinent, Japan, Taiwan, Greenland, the Horn of Africa, West Africa, the Amazon and certain areas of the Pacific (Infect Dis Clin North Am 2019;33:1045)
- HDV superinfection in chronic HBV usually results in chronic HDV infection, occurring in 80% of cases (Cold Spring Harb Perspect Med 2014;4:a021550)
- Compared with chronic HBV infection, chronic HBV / HDV coinfection is associated with a higher risk of cirrhosis, occurring in 50% to 70% of cases within 5 to 10 years of diagnosis (Gut 2021;70:1782)
- ~12 million people infected with HBV are coinfected with HDV (Gut 2021;70:1782)
- Hepatitis E virus (HEV) (Infect Dis Clin North Am 2019;33:1045)
- Uncommon cause of chronic viral hepatitis
- 8 HEV genotypes but only HEV1 and HEV2 are human viruses
- Typically causes acute hepatitis and is self limiting
- Chronic infection in the immunocompromised or during pregnancy
- Primarily waterborne, shed in feces
- Outbreaks in Asia, Africa and Latin America
Sites
- Liver parenchyma
Pathophysiology
- Chronic viral hepatitis is associated with chronic inflammation of the hepatocytes as a result of oxidative stress and immune response directed to infected hepatocytes
- Growth factors, chemokines and cytokines produced by infected hepatocytes recruit immune cells, resulting in a local inflammatory response
- Hepatocellular damage and proinflammatory signaling activates hepatic stellate cells to differentiate to myofibroblasts, resulting in fibrinogenesis (Front Cell Infect Microbiol 2020;10:587628)
Etiology
- 3 viruses are known to commonly cause chronic hepatitis (Infect Dis Clin North Am 2019;33:1045)
- Hepatitis B virus (HBV) (JAMA 2018;319:1802)
- Small enveloped, partially double stranded DNA virus
- HBV consists of an inner nucleocapsid composed of hepatitis B core antigen (HBcAg) that is complexed with a polymerase and circular viral DNA ~3.2 kb in size, all contained within an outer envelope embedded with hepatitis B surface antigen (HBsAg)
- Hepatitis B envelope antigen (HBeAg) located between core and lipid membrane, secreted and accumulates in serum
- Hepatitis C virus (HCV)
- HCV is a positive sense, single stranded RNA virus of 9.6 kb (Infect Dis Clin North Am 2019;33:1045)
- Hepatitis D virus (HDV) (Gut 2021;70:1782)
- Negative sense single stranded RNA virus of 1.7 kb and 35 to 36 nm in diameter
- HDV utilizes HBsAg for entry and infection of hepatocytes, with HBsAg incorporated in its viral envelope and thus requires HBV coinfection for transmission and replication
- Hepatitis E virus (HEV) (Infect Dis Clin North Am 2019;33:1045)
- Single stranded, positive sense RNA virus of 7.2 kb
- Shed in feces as a nonenveloped virus but are in lipid enveloped form in blood
- HEV is noncytopathic and clinical presentation is determined by host response
- Typically causes acute infection and is self limiting but can cause chronic infection in immunosuppressed patients (Cold Spring Harb Perspect Med 2019;9:a031872)
Clinical features
- Clinical presentation can vary between individuals
- Some patients can be asymptomatic for several years but a small number can progress rapidly to cirrhosis (Infect Dis Clin North Am 2019;33:1045)
- Characteristic symptoms include anorexia, malaise and fatigue (JAMA 2018;319:1802)
- Some patients develop right upper quadrant pain due to hepatic inflammation
- Jaundice is typically absent in the chronic phase of infection (Nat Rev Dis Primers 2017;3:17006)
- Hepatomegaly, ascites and peripheral edema may be observed in later stages (Infect Dis Clin North Am 2019;33:1045)
- Alanine aminotransferase level may be within reference range in chronic infection but can fluctuate between mild elevation and > 2 times the upper limit of normal (Infect Dis Clin North Am 2019;33:1045)
- Extrahepatic manifestations can occur in multiple organs
- HBV infection may cause rash, fever, arthralgia, glomerulonephritis, acute necrotizing vasculitis (polyarteritis nodosa) (Hepatology 2009;49:S13)
- HCV has been associated with cryoglobulinemia, non-Hodgkin lymphoma, glomerulonephritis, insulin resistance and diabetes (Nat Rev Dis Primers 2017;3:17006)
Diagnosis
- Clinical history and physical exam
- Laboratory evaluation
- Biopsy is the gold standard for staging liver fibrosis
- Liver biopsy for diagnosis is no longer commonly performed due to availability of reliable serological and virological tests (World J Gastroenterol 2015;21:12141)
- Transient elastography (World J Gastroenterol 2014;20:11033)
Laboratory
- Liver function tests
- Aminotransferases typically normal in chronic infection but can be mildly elevated to > 2 times the upper limit of normal (Infect Dis Clin North Am 2019;33:1045)
- Serological testing for HBV, HCV and HDV antibodies
- Viral PCR if serology positive (Infect Dis Clin North Am 2019;33:1045, JAMA 2018;319:1802, Nat Rev Dis Primers 2017;3:17006, Gut 2021;70:1782)
Radiology description
- In the acute phase, imaging features are nonspecific and diagnosis is based on serologic, virologic and clinical findings (Radiographics 2004;24:937)
- Morphologic features of cirrhosis on CT, MRI and ultrasound include (Abdom Radiol (NY) 2017;42:2037)
- Liver surface nodularity
- Atrophic right lobe and segment IV
- Hypertrophy of the caudate and lateral left lobes
- Right hepatic posterior notch
- Expanded gallbladder fossa
- Narrow hepatic veins < 5 mm
- Enlargement of the hilar periportal space > 10 mm
- Additionally, ultrasound may show (Abdom Radiol (NY) 2017;42:2037)
- Heterogeneous or coarsened echotexture
- Color Doppler flow changes that are suggestive of portal hypertension
- Fatty appearance
Prognostic factors
- Fibrosis stage is a key prognostic factor and patients with cirrhosis have greater risk of hepatic decompensation
- Active inflammation drives the development of fibrosis (Hepatology 2009;49:S61)
- Serologic and virologic response to treatment affects rate of progression (JAMA 2018;319:1802)
- In HBV, HBeAg positive chronic hepatitis is characterized by sustained viral replication and may result in significant liver damage (Infect Dis Clin North Am 2019;33:1045)
- HBeAg negative seroconversion is characterized by suppression of viral replication, reduction in liver inflammation and association with a lower risk of disease progression (Infect Dis Clin North Am 2019;33:1045)
Case reports
- 27 year old woman with acalculous cholecystitis secondary to chronic HCV (Cureus 2022;14:e26484)
- 39 year old woman with HEV superinfection leading to reactivation of chronic HBV (BMJ Case Rep 2018;2018:bcr2017223616)
- 48 year old man with chronic HBV and terbinafine induced HBV reactivation (Cureus 2020;12:e11958)
- 50 year old woman with a history of chronic HBV with negative seroconversion of autoantibodies following antiviral treatment (World J Clin Cases 2021;9:1196)
Treatment
- Hepatitis B virus (Infect Dis Clin North Am 2019;33:1045)
- Vaccination is key to prevention
- Nucleoside / nucleotide analogs such as entecavir, tenofovir disoproxil or tenofovir alafenamide in chronic HBV
- Pegylated interferon alpha (treatment of choice in HDV infection)
- Hepatitis C virus
- Direct acting antivirals (DAA) in combination to target specific steps in HCV replication (Infect Dis Clin North Am 2019;33:1045)
- 3 proteins targeted: NS3/4A protease, NS5B polymerase and NS5A protein
- Combination therapy such as elbavir / grazoprevir or sofosbuvir / velpatasvir (Nat Rev Dis Primers 2017;3:17006, Infect Dis Clin North Am 2019;33:1045)
- Addition of ribavirin to DAA regimen depending on viral genotype and if patient has developed cirrhosis (Nat Rev Dis Primers 2017;3:17006)
- Interferon therapy is still the most frequently used treatment in several Asian countries (Nat Rev Dis Primers 2017;3:17006)
Gross description
- Nonspecific changes in early stages
- Enlarged and yellow (fatty change) or green (cholestasis)
- Firm, nodular appearance with a micronodular or macronodular pattern in later stages (World J Gastroenterol 2016;22:1357, StatPearls: Hepatic Cirrhosis [Accessed 15 February 2023])
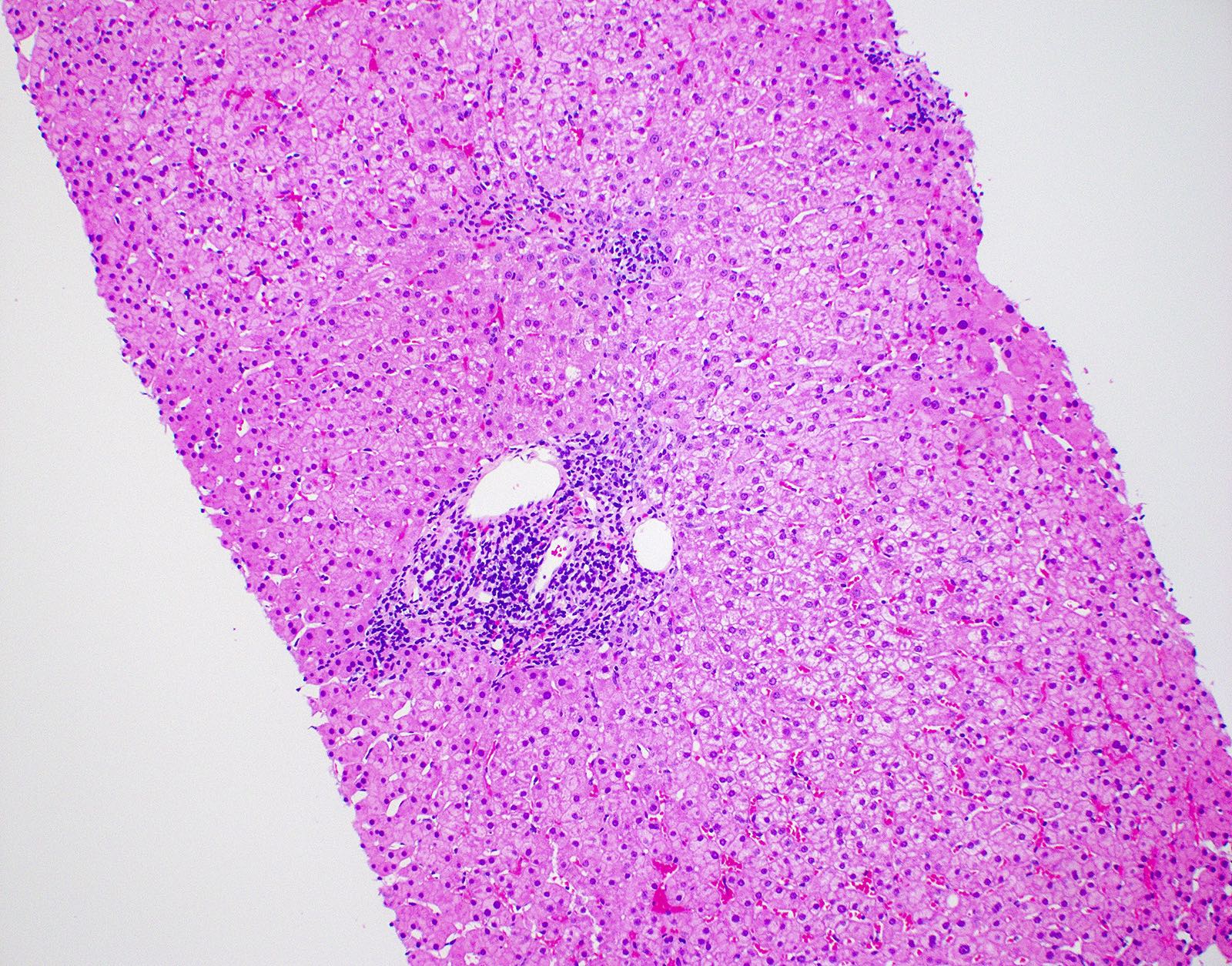
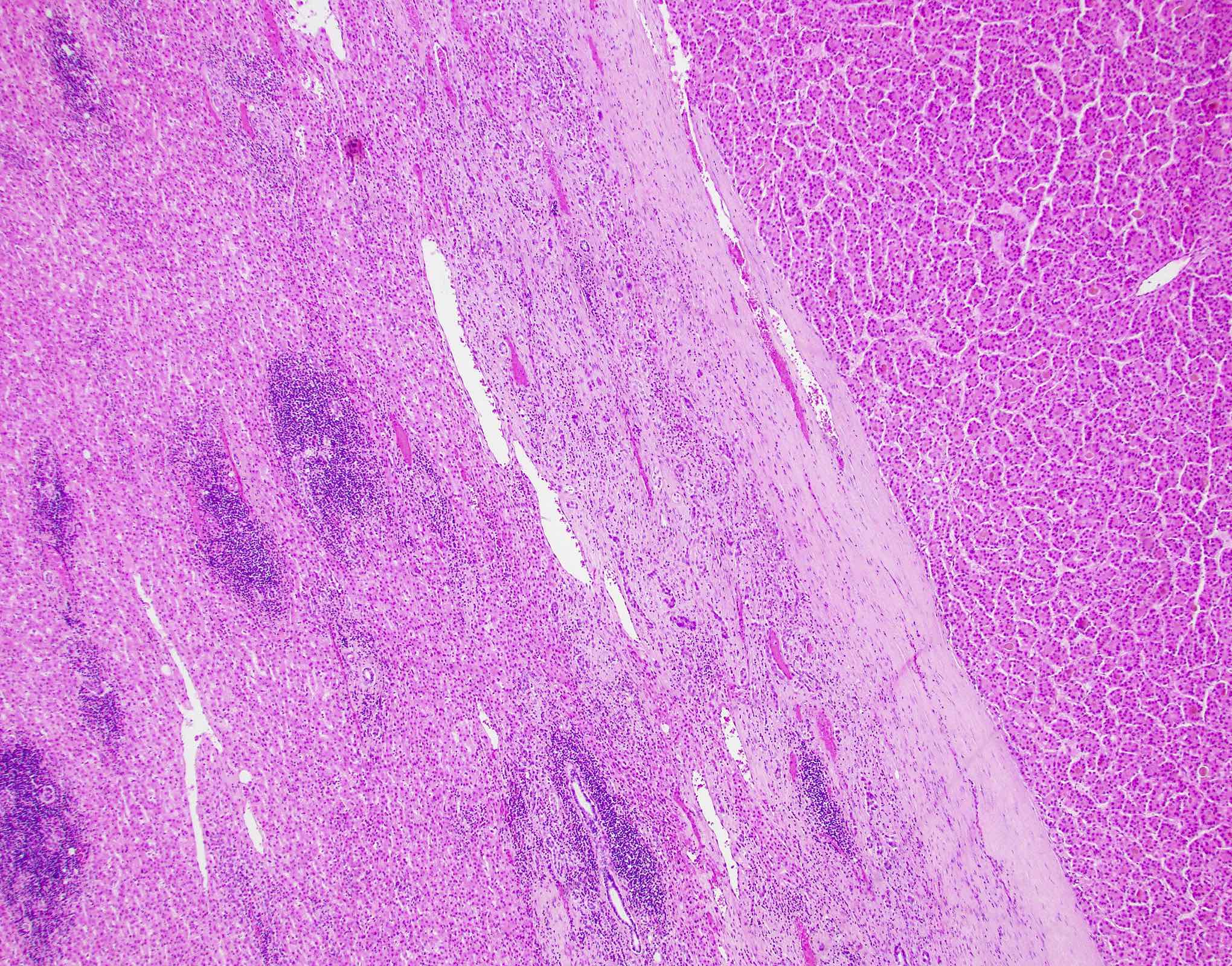
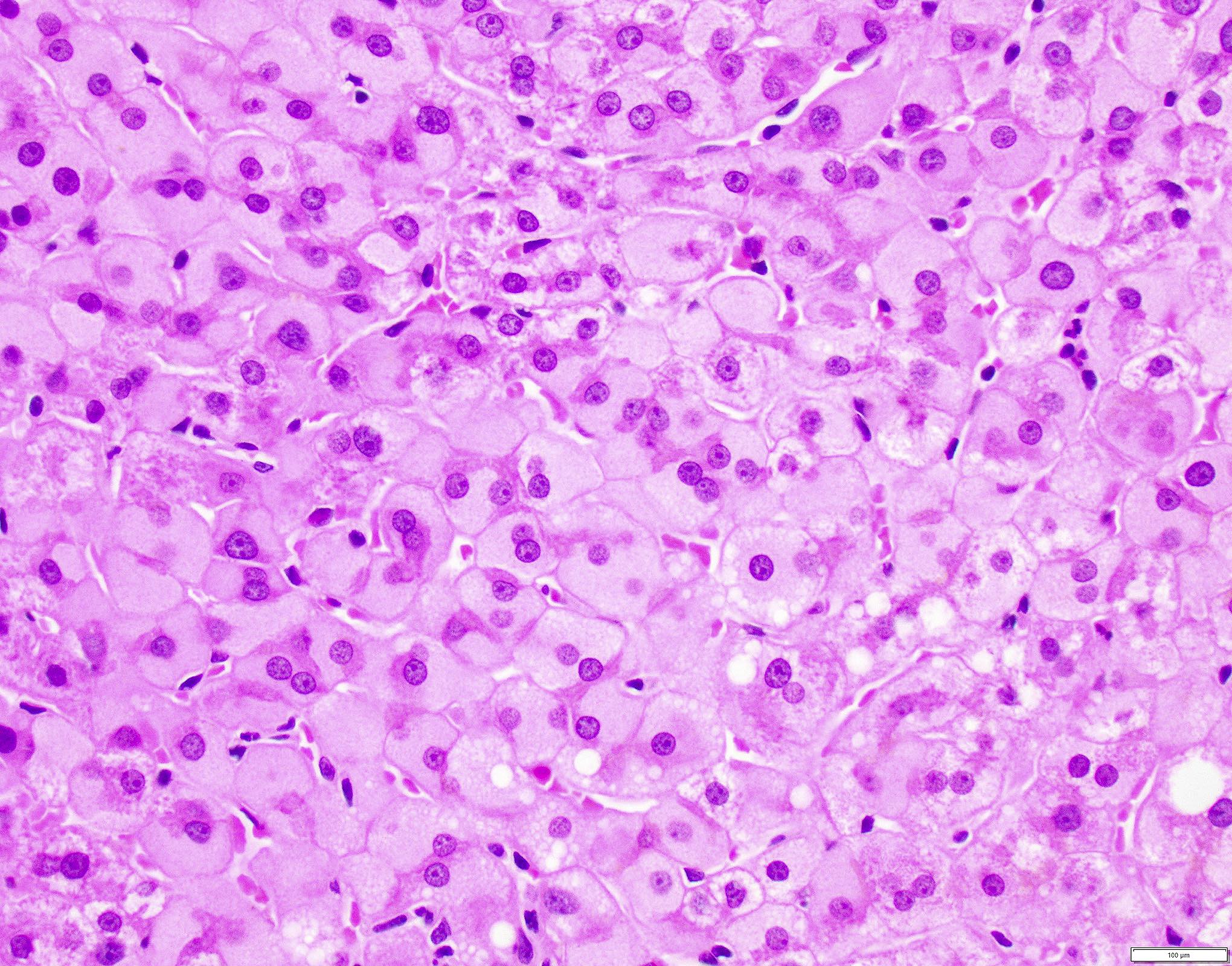
Microscopic (histologic) description
- Histologic appearance of chronic viral hepatitis includes patterns that are common to all etiologies of chronic hepatitis
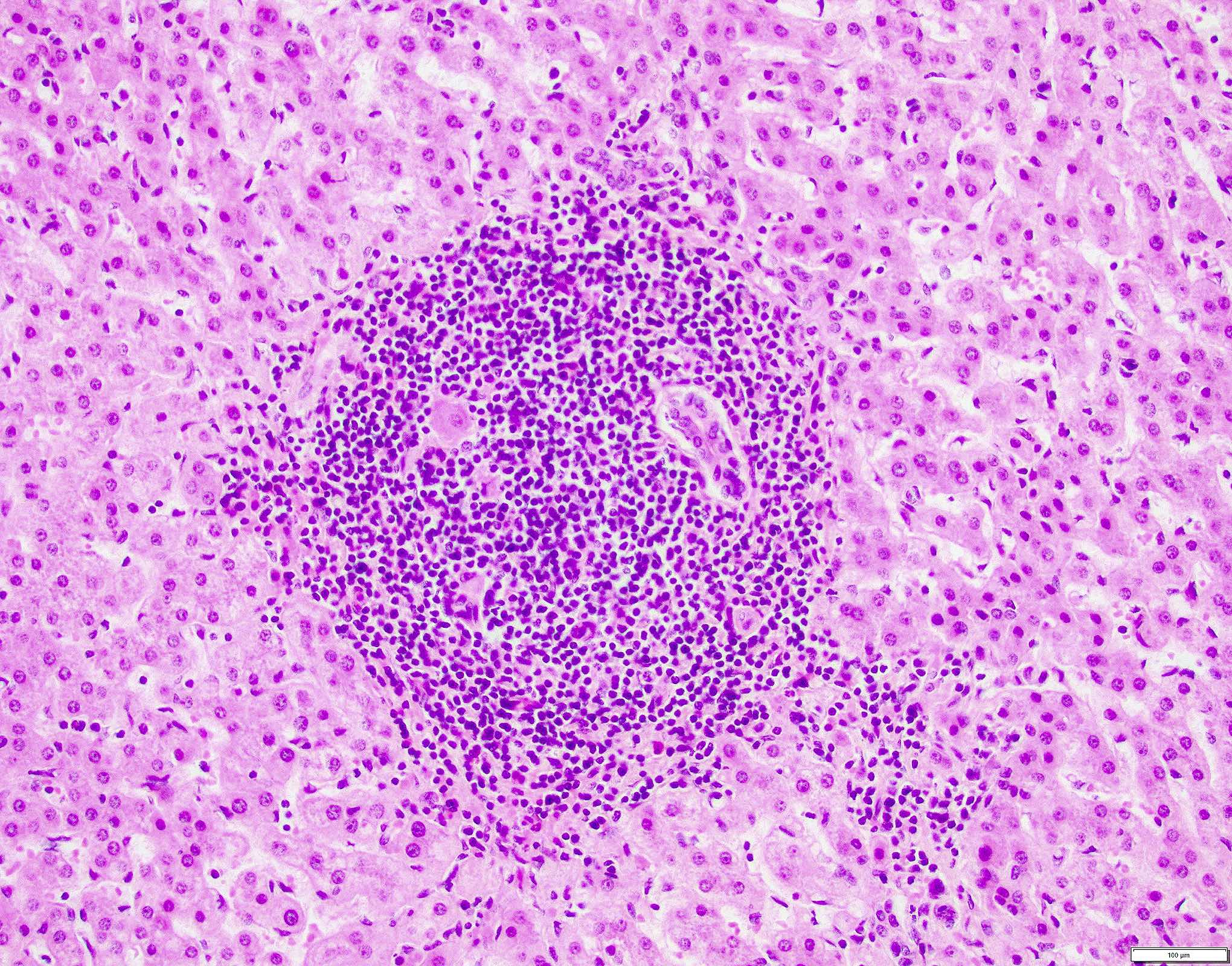
- Portal inflammation
- Predominantly consisting of lymphocytes with few admixed plasma cells and histiocytes (Dig Liver Dis 2011;43:S331)
- Interface hepatitis (piecemeal necrosis)
- Lymphocytic infiltrate at the boundary of the portal tract extending into the liver parenchyma with associated hepatocyte damage (Dig Liver Dis 2011;43:S331)
- Lobular changes that include
- Inflammation of the liver parenchyma (variable)
- Focal and confluent necrosis
- Apoptosis (apoptotic / councilman bodies) (Dig Liver Dis 2011;43:S331)
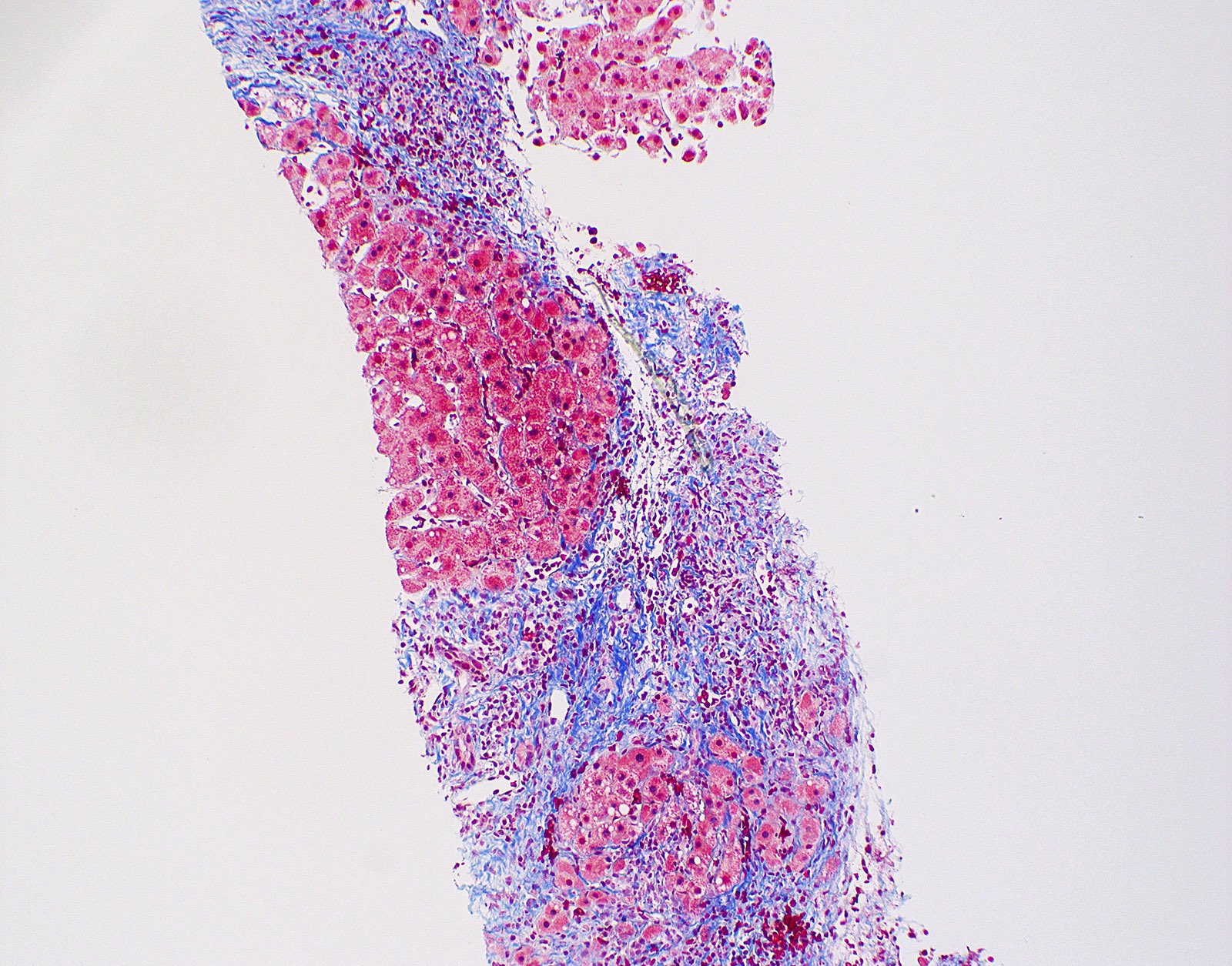
- Fibrosis
- Is seen in varying degrees depending on the stage of the disease and is progressive
- Fibrous portal expansion seen in earlier stages, progressing with the formation of fibrous septa that may lead to bridging fibrosis and ending with cirrhosis (Dig Liver Dis 2011;43:S331)
- Cirrhosis characterized by fibrotic bands with loss of architecture and nodule formation (Hepatology 2009;49:S61)
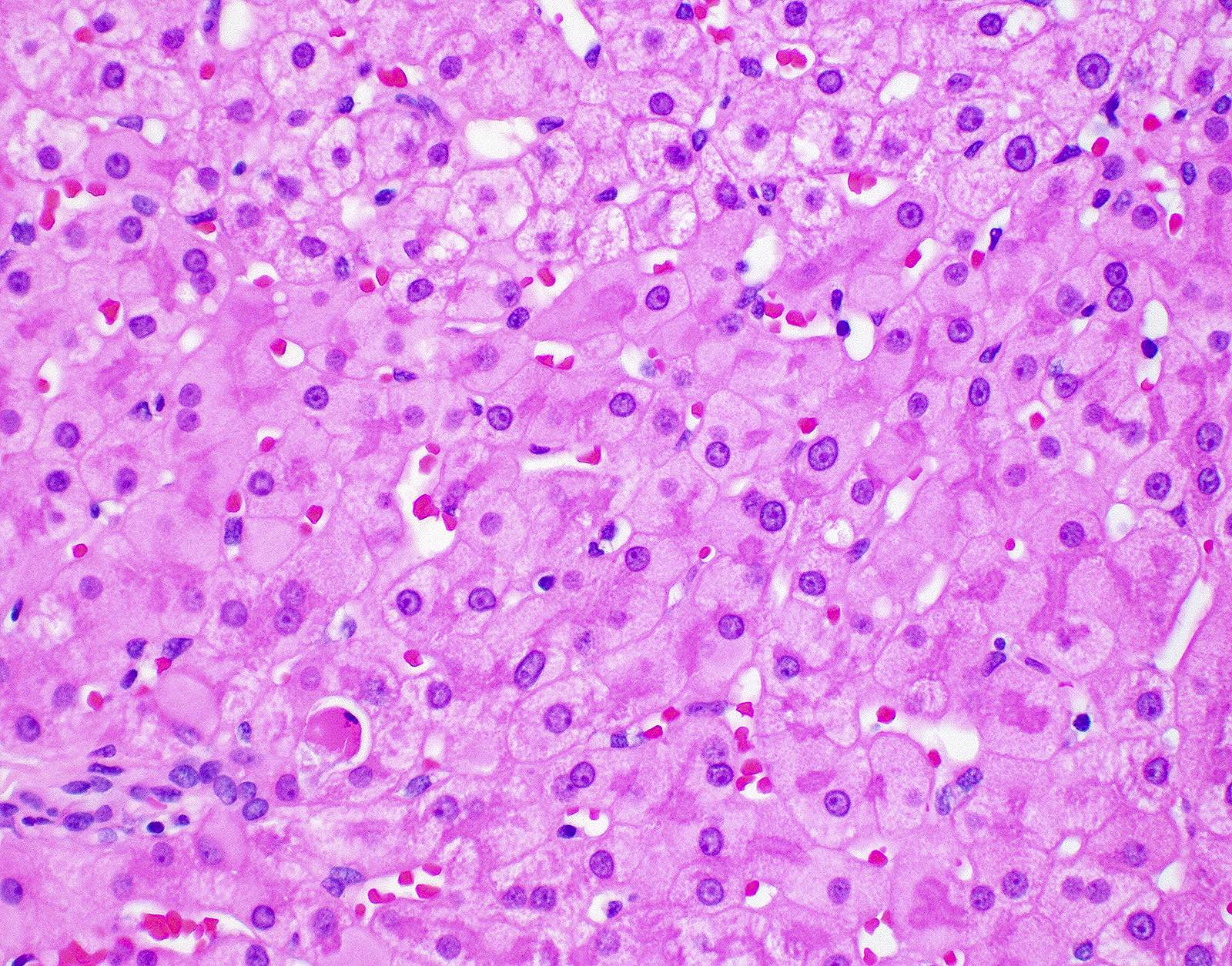
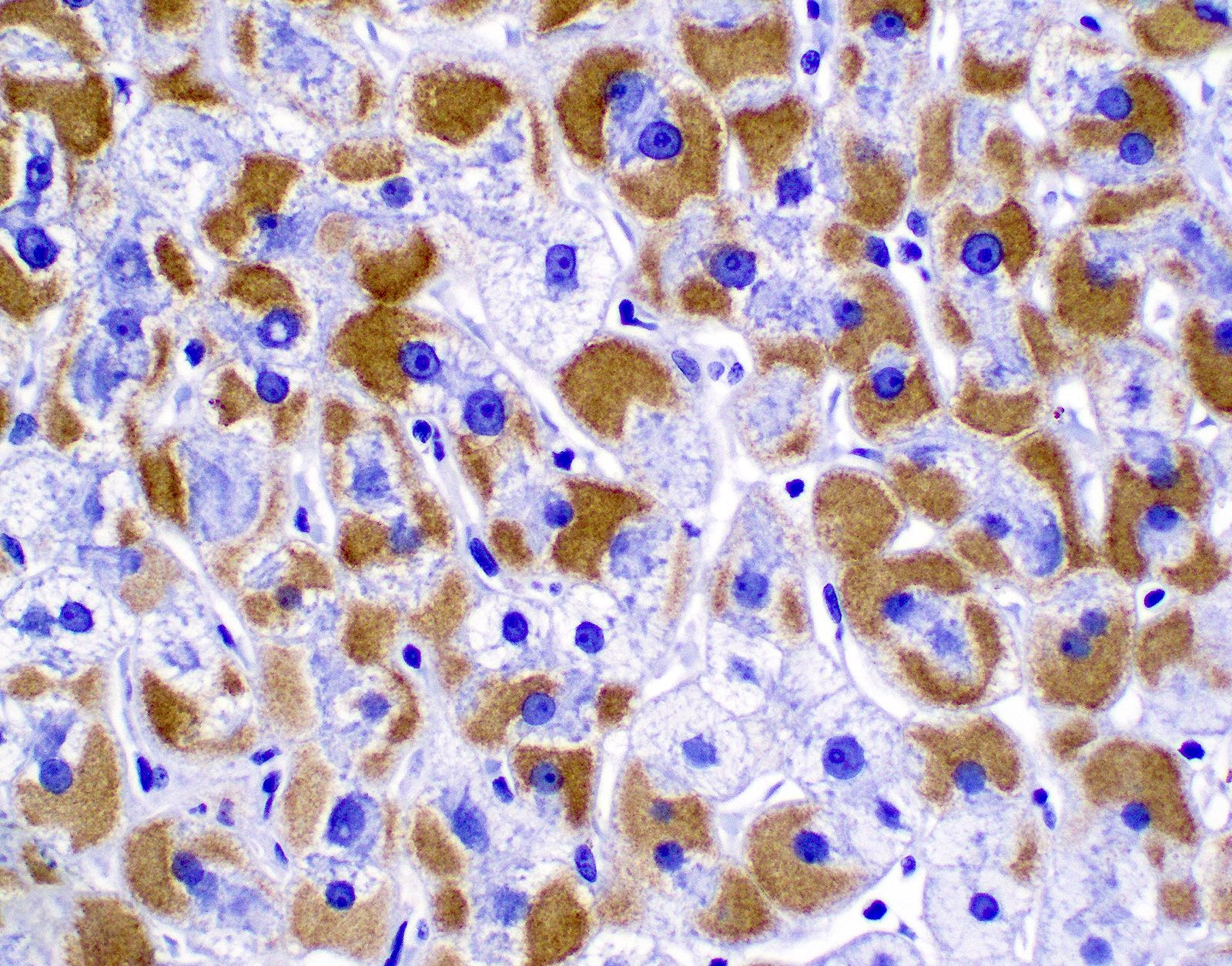
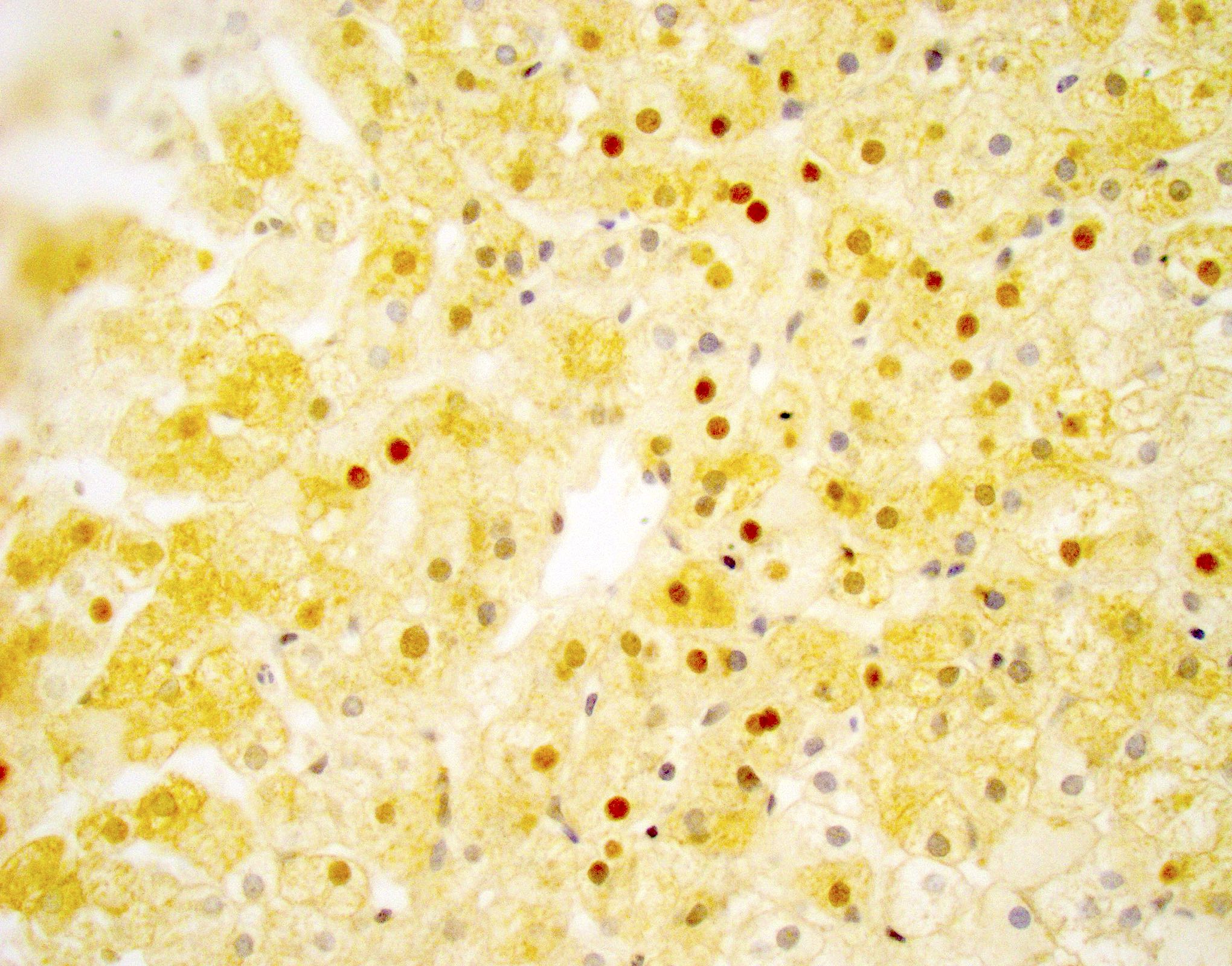
- Certain morphologic features are characteristic but not diagnostic of a particular viral etiology
- HBV (Dig Liver Dis 2011;43:S331, Hepatology 2009;49:S61)
- Ground glass appearance of hepatocytes due to proliferation of smooth endoplasmic reticulum containing HBsAg
- Lafora disease and fibrinogen storage disease also demonstrate ground glass hepatocytes
- Both will be highlighted by Shikata orcein and Victoria blue stain
- Can be distinguished with immunohistochemical stains for HBsAg or HBcAg
- Sanded nuclei (eosinophilic nuclear inclusions)
- HDV coinfection is associated with relatively high necroinflammation
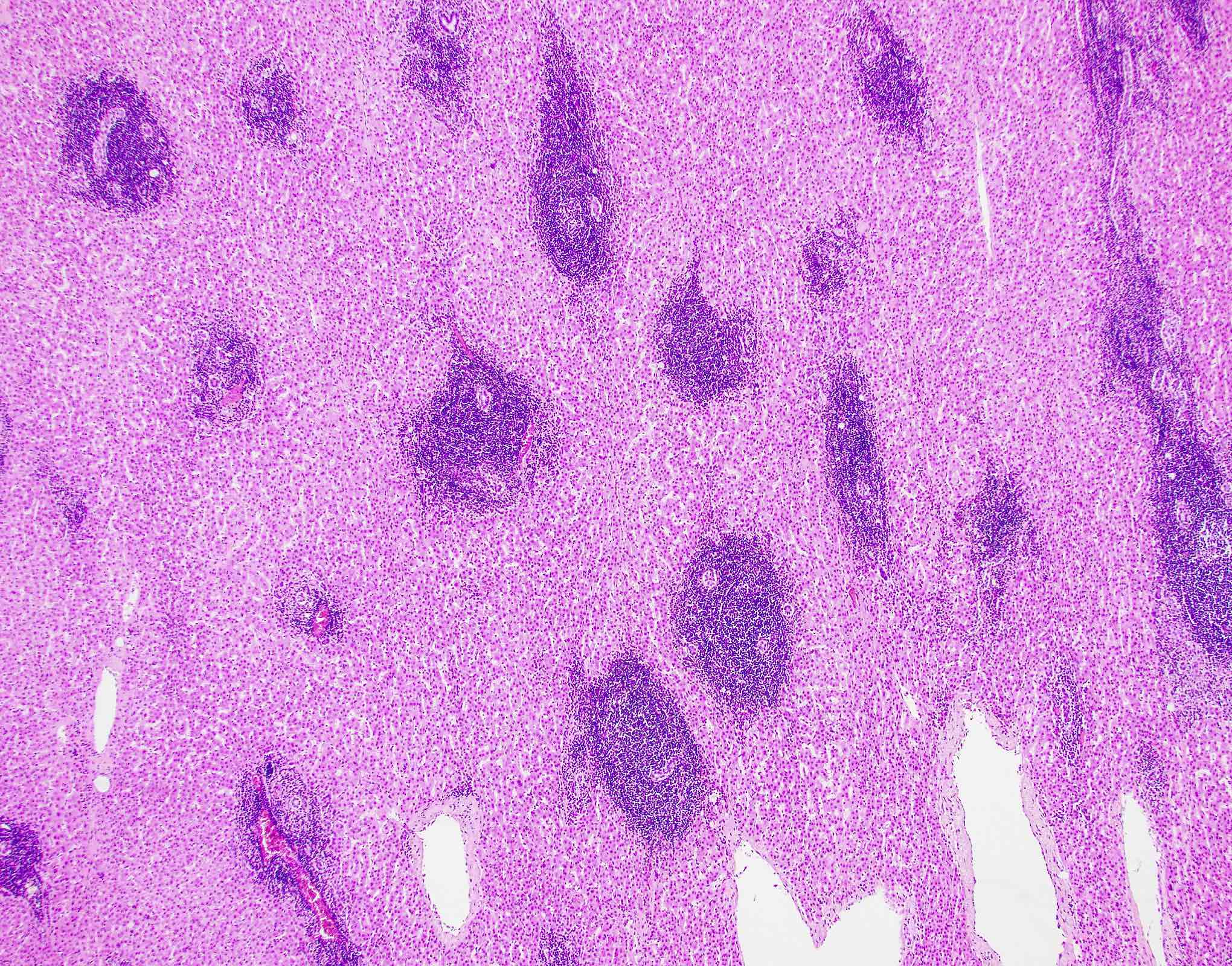
- HCV (Hepatology 2009;49:S61, Dig Liver Dis 2011;43:S331, World J Gastroenterol 2016;22:1357)
- Nodular lymphoid aggregates
- Bile duct damage (Poulsen-Christofferson lesion) with lymphocytic infiltrate
- Steatosis, macrovesicular or mixed macrovesicular and microvesicular (more common in HCV but may also be seen in HBV)
- Iron deposition
Microscopic (histologic) images
Positive stains
- Trichrome stain is used to evaluate the degree of fibrosis present
- HBsAg immunohistochemical stain shows cytoplasmic staining (diffuse or focal) (Trop Gastroenterol 2002;23:16, Clin Liver Dis (Hoboken) 2013;2:S8)
- HBcAg immunohistochemical stain shows nuclear staining (Trop Gastroenterol 2002;23:16, Clin Liver Dis (Hoboken) 2013;2:S8)
- HBV ground glass hepatocytes can be highlighted with Shikata orcein and Victoria blue stains (Hepatology 2009;49:S61)
Videos
Viral hepatitis
Chronic hepatitis histopathology
Sample pathology report
- Liver, biopsy:
- Chronic hepatitis with mild activity (METAVIR grade A1) and moderate periportal fibrosis with focal bridging (Scheuer stage 2/4) (see comment)
- Comment: The findings are consistent with the patient's history of chronic hepatitis B infection.
Differential diagnosis
- Other nonviral causes of chronic hepatitis
- Autoimmune hepatitis:
- Inflammatory infiltrates in autoimmune hepatitis tend to be plasma cell rich (Hepatology 2009;49:S61)
- Nonalcoholic or alcoholic steatohepatitis (Metabolism 2016;65:1080):
- Steatosis and ballooned hepatocytes are usually present but may be absent in late stage disease
- Centrizonal pattern of injury and fibrosis
- Primary biliary cholangitis (Dig Liver Dis 2011;43:S331, Clin Liver Dis (Hoboken) 2021;17:227):
- Granulomatous destruction of bile ducts, cholate stasis and accumulation of copper associated proteins in periportal hepatocytes are suggestive of primary biliary cirrhosis
- Florid duct lesions, which are not seen in chronic viral hepatitis
- May have positive serology for antimitochondrial antibodies
- Elevated alkaline phosphatase
- Primary sclerosing cholangitis (Dig Liver Dis 2011;43:S331, Clin Liver Dis (Hoboken) 2021;17:227):
- Onion skin fibrosis of medium sized bile ducts
- May be positive for antineutrophil cytoplasmic antibodies
- Elevated alkaline phosphatase
- Alpha-1 antitrypsin deficiency (Hepatology 2009;49:S61, Dig Liver Dis 2011;43:S331):
- Presence of periportal eosinophilic globules with PASD stain
- Hemochromatosis (Mod Pathol 2007;20:S3, Dig Liver Dis 2011;43:S331):
- Hemosiderin accumulation in hepatocytes and Kupffer cells
- Can be highlighted with Prussian blue stain
- Wilson disease (Dig Liver Dis 2011;43:S331, Mo Med 2010;107:113):
- Histopathologic findings are not specific
- Positive copper stain in hepatocytes and Kupffer cells
- A negative stain does not exclude Wilson disease
- Laboratory findings (ceruloplasmin, serum / urine copper) and clinical findings (Kayser-Fleischer rings)
- Drug induced liver injury (Hepatology 2009;49:S61, US Gastroenterol Hepatol Rev
2010;6:73, Dig Liver Dis 2011;43:S331):
- Can show varying histology; histopathologic findings are not specific
- Strong clinical suspicion and chronologic relationship between drug administration and onset of pathology
- Autoimmune hepatitis:
- Acute hepatitis with bridging fibrosis:
- Bridging necrosis seen in acute hepatitis can mimic the appearance of bridging fibrous septa seen in chronic hepatitis
- Trichrome stain can help distinguish
- Lymphoma or leukemic involvement of the liver (Am J Hematol 2017;92:1362, Am J Clin Pathol 2014;141:119):
- Infiltrate consists of atypical lymphocytes; may be monomorphic
- Immunohistochemistry and gene rearrangement studies to identify aberrancy
Board review style question #1
Board review style answer #1
D. Hepatitis B surface antigen. The ground glass appearance is due to the proliferation of smooth endoplasmic reticulum and the accumulation of intracellular HBsAg. While HBcAg expression in HBeAg positive individuals is correlated with increased DNA titer and increased hepatic activity index, the accumulation of HBcAg, HBeAg and HBV DNA does not produce the characteristic ground glass appearance of hepatocytes in chronic HBV.
Comment Here
Reference: Chronic viral hepatitis
Comment Here
Reference: Chronic viral hepatitis
Board review style question #2
In a patient with chronic viral hepatitis, which of the following combinations of findings on a liver biopsy would be most suggestive of a chronic hepatitis C infection?
- Ground glass hepatocytes with sanded nuclei
- Portal based inflammation with interface activity
- Portal expansion with bridging fibrous septa
- Nodular lymphoid aggregates, bile duct damage (Poulsen lesion) and steatosis
Board review style answer #2
D. Nodular lymphoid aggregates, bile duct damage (Poulsen lesion) and steatosis. While not diagnostic, the presence of nodular lymphoid aggregates, bile duct damage (Poulsen lesion) and steatosis are considered characteristic of HCV infection. Ground glass hepatocytes are seen in HBV infection and represent the accumulation of HBsAg. Portal based inflammation with interface activity and fibrosis are general features of chronic viral hepatitis and are not specific to HCV.
Comment Here
Reference: Chronic viral hepatitis
Comment Here
Reference: Chronic viral hepatitis