Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chan AWH. Autoimmune hepatitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverautoimmune.html. Accessed March 31st, 2025.
Definition / general
- Immune mediated inflammatory liver disease of uncertain cause (Hepatology 2020;72:671)
Essential features
- Diagnosis is based on combination of clinical, laboratory and histological features
- More common in female patients
- Classic (but not sole) serologic association is with anti smooth muscle antibody
- Typical histological features include interface hepatitis, portal lymphocytic or lymphoplasmacytic infiltrate, hepatocyte rosetting and emperipolesis (though latter 2 falling out of favor)
Terminology
- Previously known as lupoid hepatitis
ICD coding
- ICD-10: K75.4 - autoimmune hepatitis
Epidemiology
- Incidence is highest in North America (42.9/100,000), followed by Europe (10.7 - 23.9/100,000) (J Gastroenterol Hepatol 2015;30:1230)
- M:F = 1:4 - 6
- Usual age of presentation depends on subtype:
- Type 1: bimodal (10 - 25 years and 45 - 70 years)
- Type 2: < 15 years
Sites
- Liver
Etiology
- Unknown; genetic and environmental factors may play roles in pathogenesis (J Hepatol 2015;62:S100)
- Genetic predisposition:
- North America / Europe: HLA-DR3 (DRB1*0301) and HLA-DR4 (DRB1*0401)
- China / Japan: HLA-DR4 (DRB1*0405)
Clinical features
- Most patients have nonspecific symptoms: fatigue (85%), anorexia, nausea, weight loss, jaundice, pruritus, amenorrhea
- 25 - 34% are asymptomatic
- 25 - 75% have episodes of acute / fulminant hepatitis
- 14 - 44% have concurrent extrahepatic autoimmune disorders, including autoimmune thyroiditis, rheumatoid arthritis, Sjögren syndrome, vitiligo or ulcerative colitis (Hepatology 2020;72:671)
- Incidence of cirrhosis at presentation varies widely: North America (59 - 85%), Middle East (22.2 - 45.5%), China (24.8%), Japan (6.4 - 12.8%) (J Gastroenterol Hepatol 2015;30:1230)
- Burnt out autoimmune hepatitis is one of the most common causes of cryptogenic cirrhosis (Scand J Gastroenterol 2010;45:60)
- Hepatocellular carcinoma risk: pooled incidence of 3.06/1,000 patient years; 10.07/1,000 patient years in cirrhotic patients (Clin Gastroenterol Hepatol 2017;15:1207)
Diagnosis
- Diagnosis is based on combination of clinical, laboratory and histological features
- Revised diagnostic International Autoimmune Hepatitis Group (IAIHG) scoring system (J Hepatol 1999;31:929):
- Complex system evaluating 11 clinical, laboratory and histological factors
- For research purposes; not designed for clinical practice
- Simplified diagnostic International Autoimmune Hepatitis Group scoring system (Hepatology 2008;48:169):
- Simple system evaluating 4 laboratory and histological factors: serum autoantibodies, IgG, liver histology and viral hepatitis serology
- Cutoff values for probable and definite autoimmune hepatitis are 6 points (88% sensitivity and 97% specificity) and 7 points (81% sensitivity and 99% specificity), respectively
- American Association for the Study of Liver Diseases (AASLD) guidance statement (Hepatology 2020;72:671):
- Compatible histological findings
- Elevated aspartate aminotransferase / alanine aminotransferase
- Elevated IgG or positive serological marker(s)
- Exclusion of other diseases resembling autoimmune hepatitis
- Subtypes:
- Type 1: positive for antinuclear antibody or anti smooth muscle antibody; 10% have other autoimmune disorders
- Type 2: positive for anti liver kidney microsomal antibody or anti liver cytosol type 1 antibody positive; often presents with acute or fulminant hepatitis; 17% have other autoimmune disorders
- Type 3: controversial subtype. positive for antisoluble liver antigen / liver pancreas; clinical and laboratory features indistinguishable from type 1 (Gut 2001;49:589)
- About 10% of autoimmune hepatitis fits into following scenarios
- Overlap syndrome
- Autoimmune hepatitis / primary biliary cholangitis (PBC)
- Autoimmune hepatitis / primary sclerosing cholangitis (PSC)
- Variant syndromes
- Seronegative autoimmune hepatitis (Gut 2001;49:589)
- Antimitochondrial antibody positive autoimmune hepatitis (Gut 2001;49:589)
- IgG4 associated autoimmune hepatitis (J Gastroenterol Hepatol 2019;34:742)
- Overlap syndrome
Laboratory
- Serum autoantibodies (J Autoimmun 2013;46:17):
- Antinuclear antibody: positive in 75% of type 1 autoimmune hepatitis; not associated with disease course or outcome
- Anti smooth muscle antibody: positive in 95% of type 1 autoimmune hepatitis; not associated with disease course or outcome
- Anti liver kidney microsomal: diagnostic for type 2 autoimmune hepatitis; associated with younger age at presentation, fulminant hepatic failure and partial IgA deficiency
- Anti liver cytosol type 1: diagnostic for type 2 autoimmune hepatitis; associated with more severe inflammation and rapid progression to cirrhosis
- Antisoluble liver antigen / liver pancreas: positive in 20 - 50% of autoimmune hepatitis; associated with more severe disease, treatment dependence, relapse after drug withdrawal and need for transplantation
- Elevated liver enzymes; ALT / AST > ALP
- Serum immunoglobulin G (IgG): marker for diagnosis (> 1.1 x upper limit of normal [ULN]) and monitoring treatment response (Hepatology 2010;51:2193)
Prognostic factors
- Good prognostic factor: IgG4 associated autoimmune hepatitis (J Gastroenterol Hepatol 2019;34:742)
- Poor prognostic factors: extreme age (≤ 20 years or ≥ 60 years), failure to normalize alanine aminotransferase within 6 months of onset of therapy, serum albumin ≤ 35 g/L (J Gastroenterol Hepatol 2015;30:1230)
Case reports
- 32 year old man with concurrent autoimmune hepatitis and advanced AIDS (Case Reports Hepatol 2019;2019:5326428)
- 48 year old woman with autoimmune hepatitis with overlap systemic lupus erythematosus (BMJ Case Rep 2020;13:e237341)
- 65 year old man with IgG4 associated autoimmune hepatitis (BMC Gastroenterol 2020;20:420)
Treatment
- Corticosteroids alone or with azathioprine to achieve normalization of serum transaminases and IgG
- If no response, add other immunosuppressants (e.g. cyclosporine, tacrolimus or mycophenolate mofetil) and consider liver transplantation
- Good long term prognosis with 10 year survival rate of 80 - 100% (J Gastroenterol Hepatol 2015;30:1230, Hepatology 2010;51:2193)
- Treatment outcome
- Biochemical remission: aspartate aminotransferase, alanine aminotransferase and IgG normalization
- Histological remission: absence of inflammation in liver biopsy
Microscopic (histologic) description
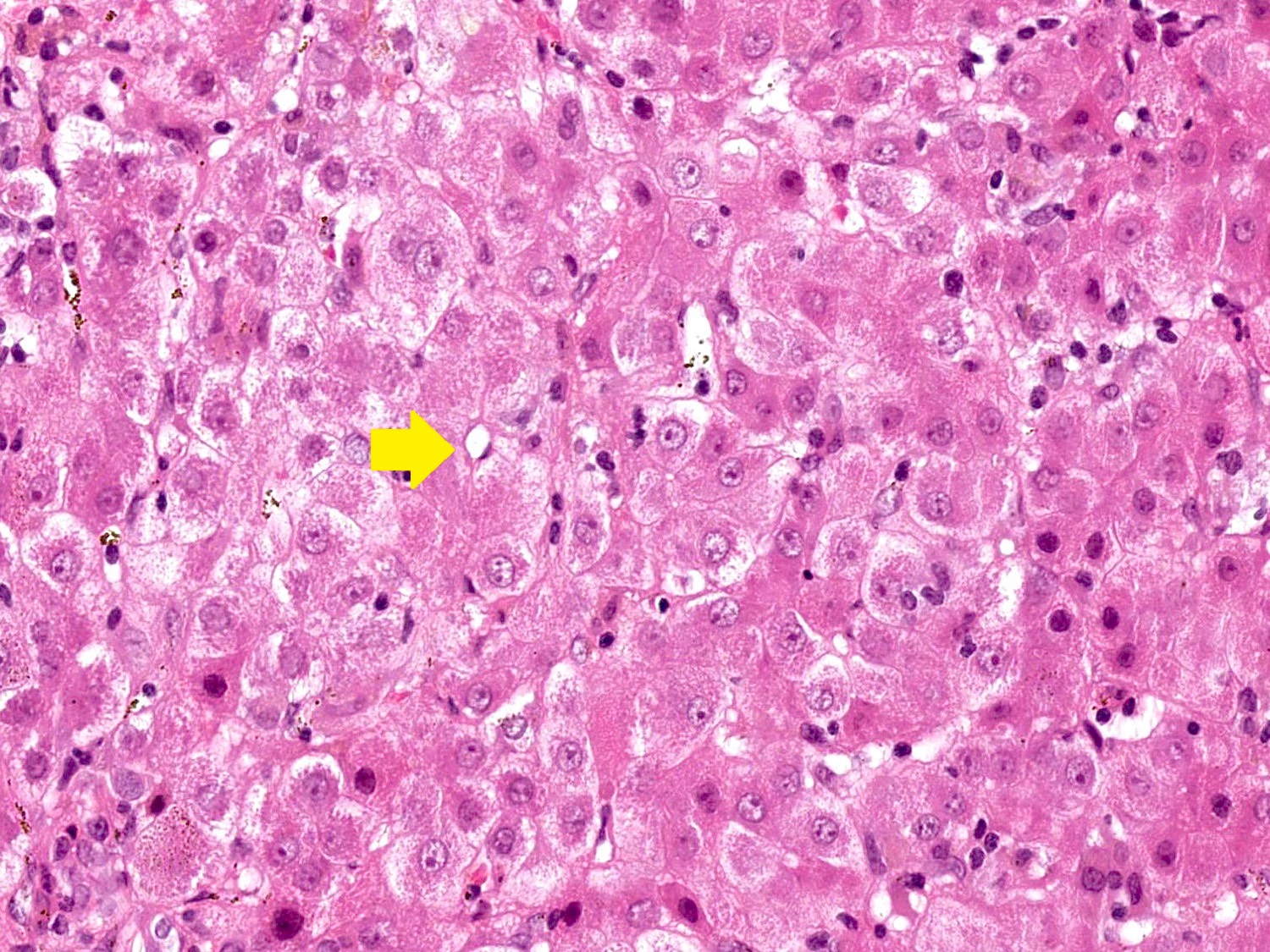
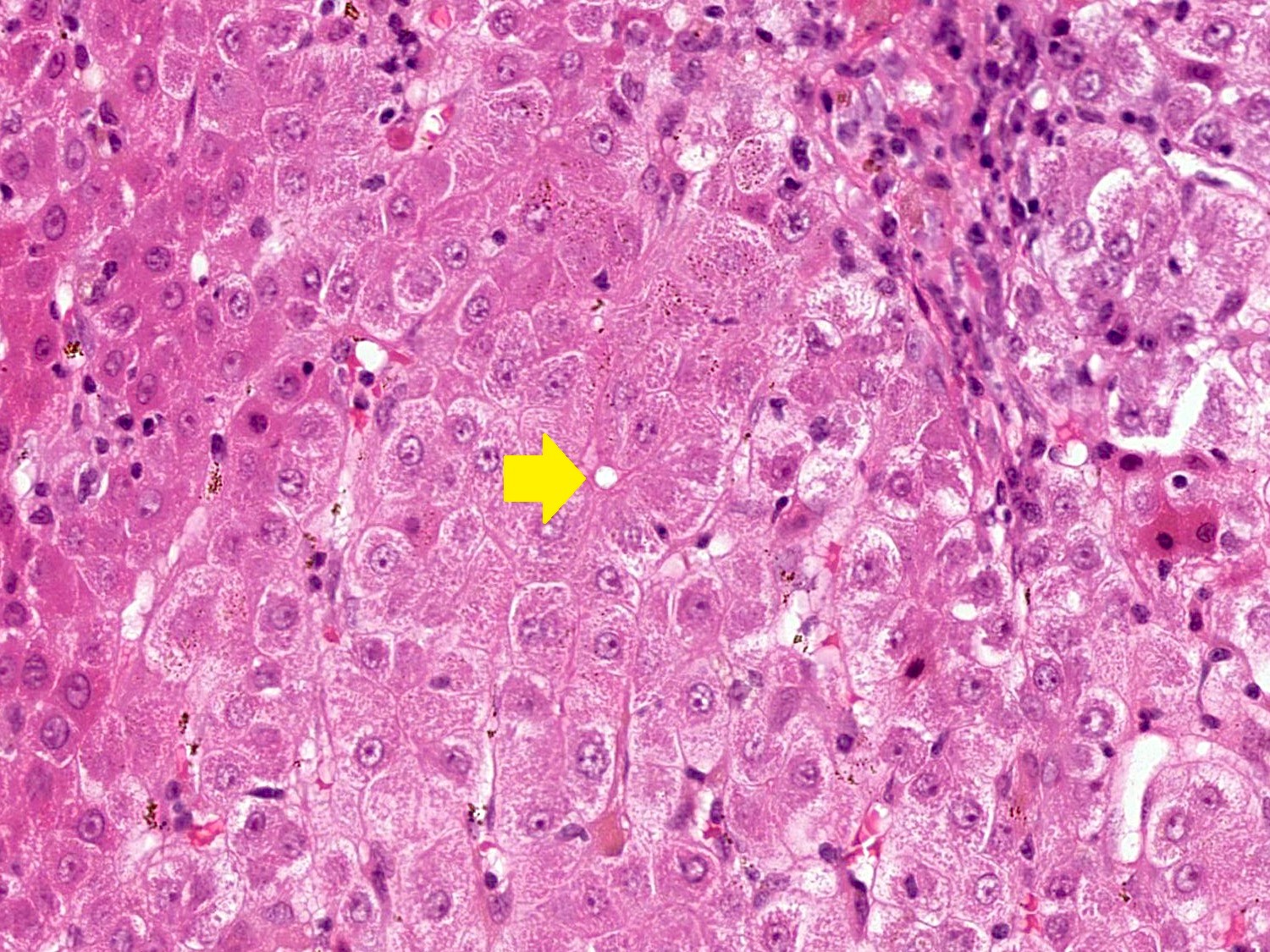
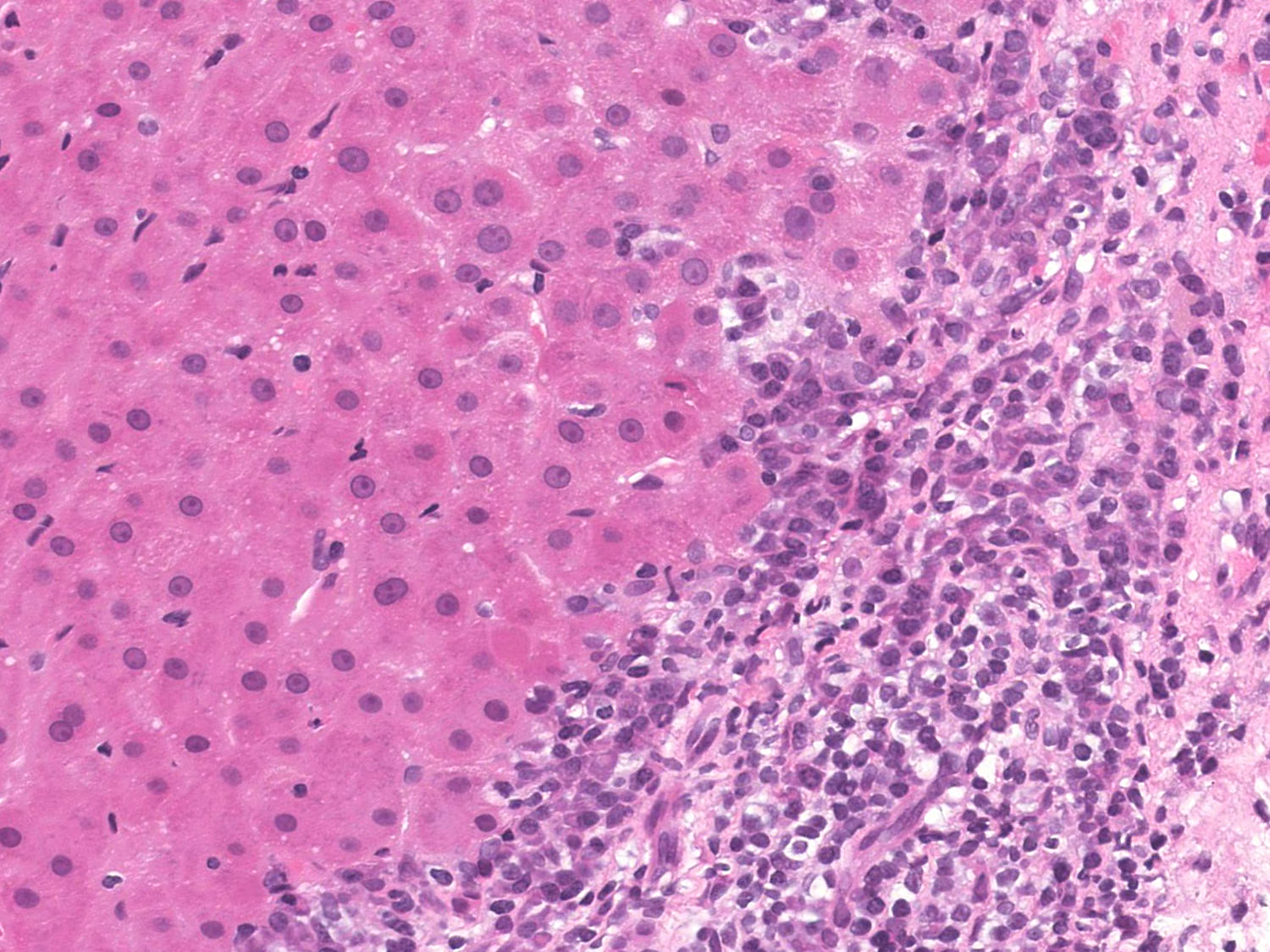
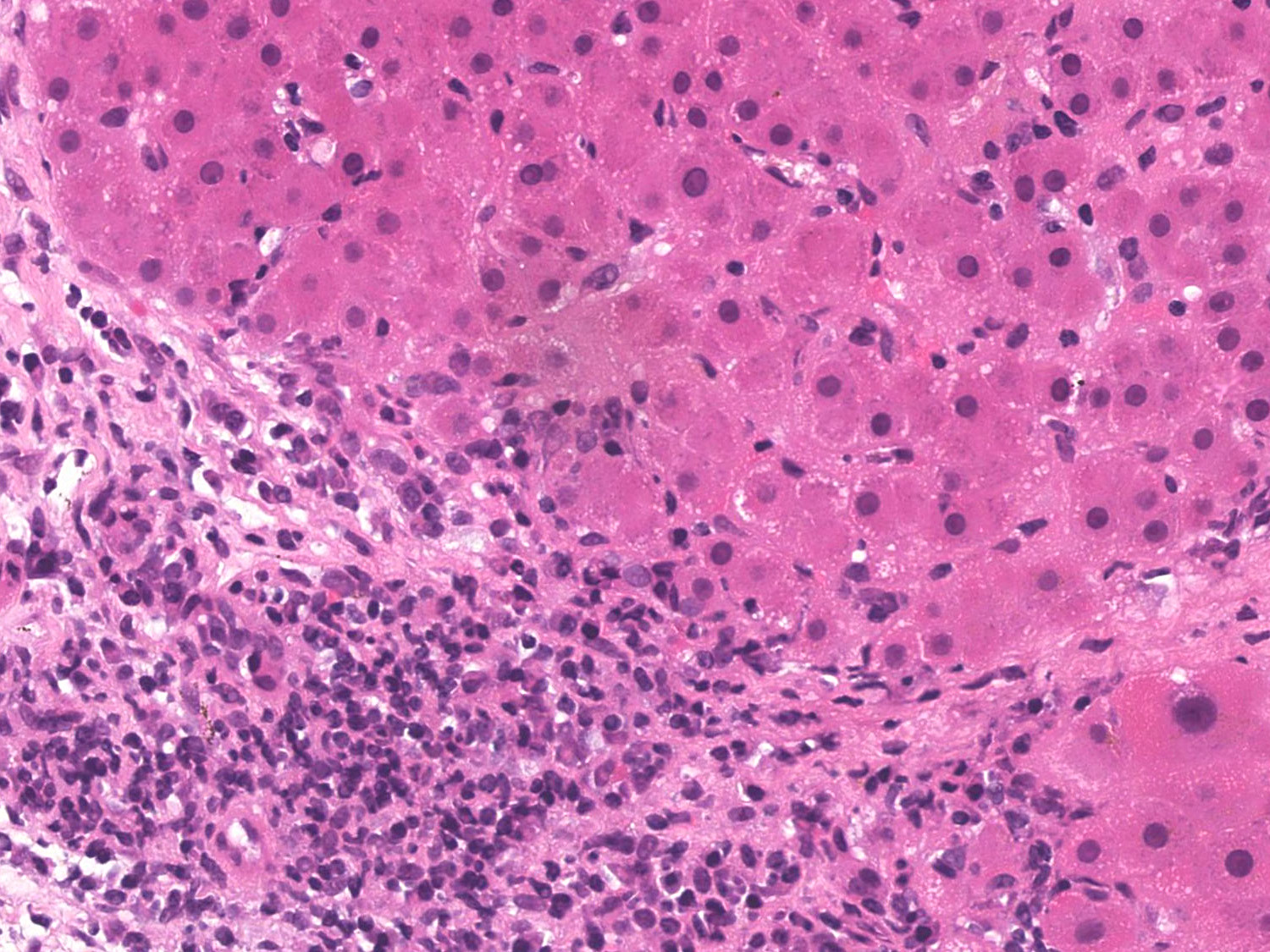
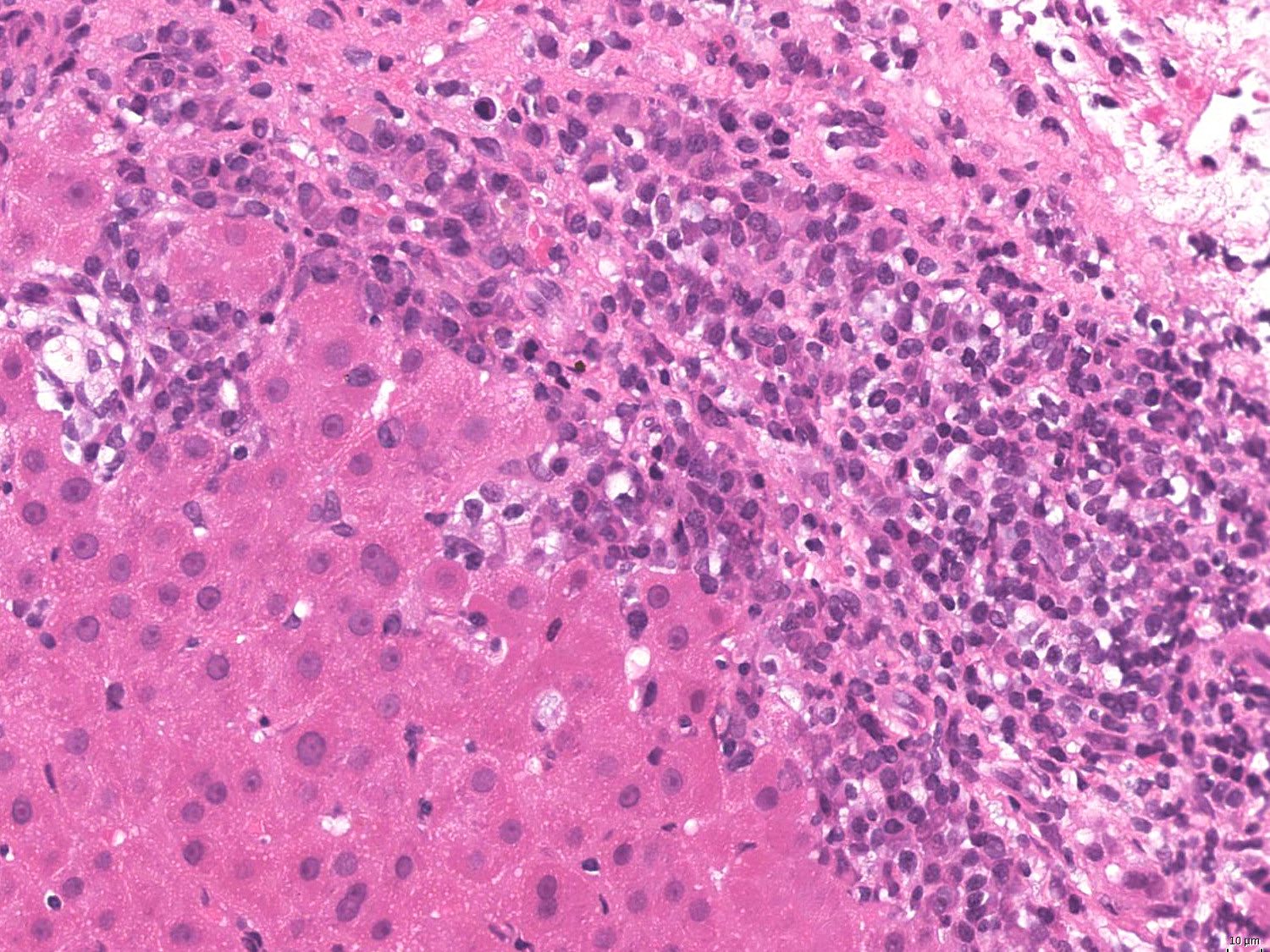
- Typical morphological changes:
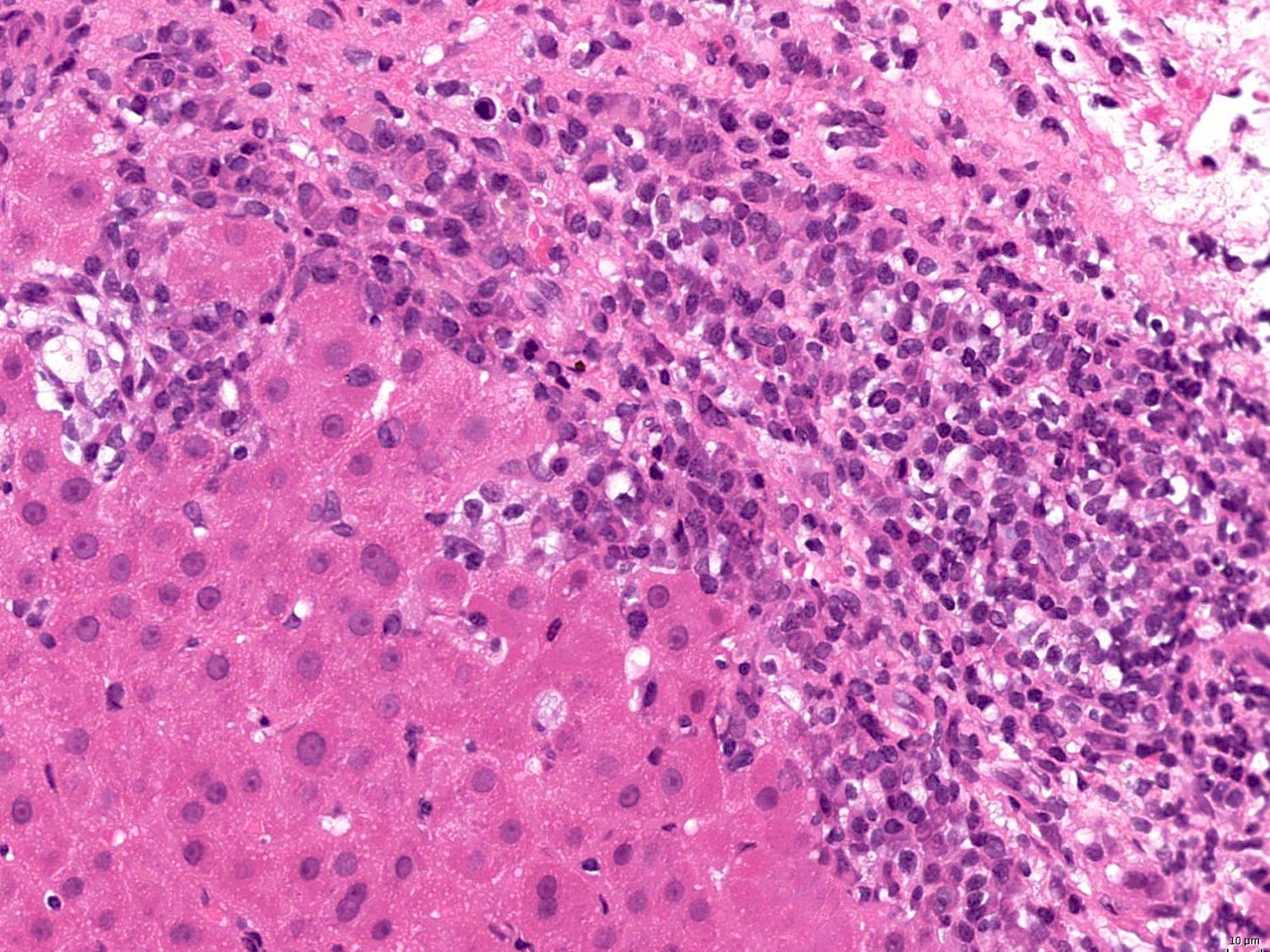
- Portal plasma cell rich inflammation
- Interface hepatitis, formerly referred to as piecemeal necrosis: portal inflammatory cells eroding through the limiting plate between the portal tract and liver parenchyma
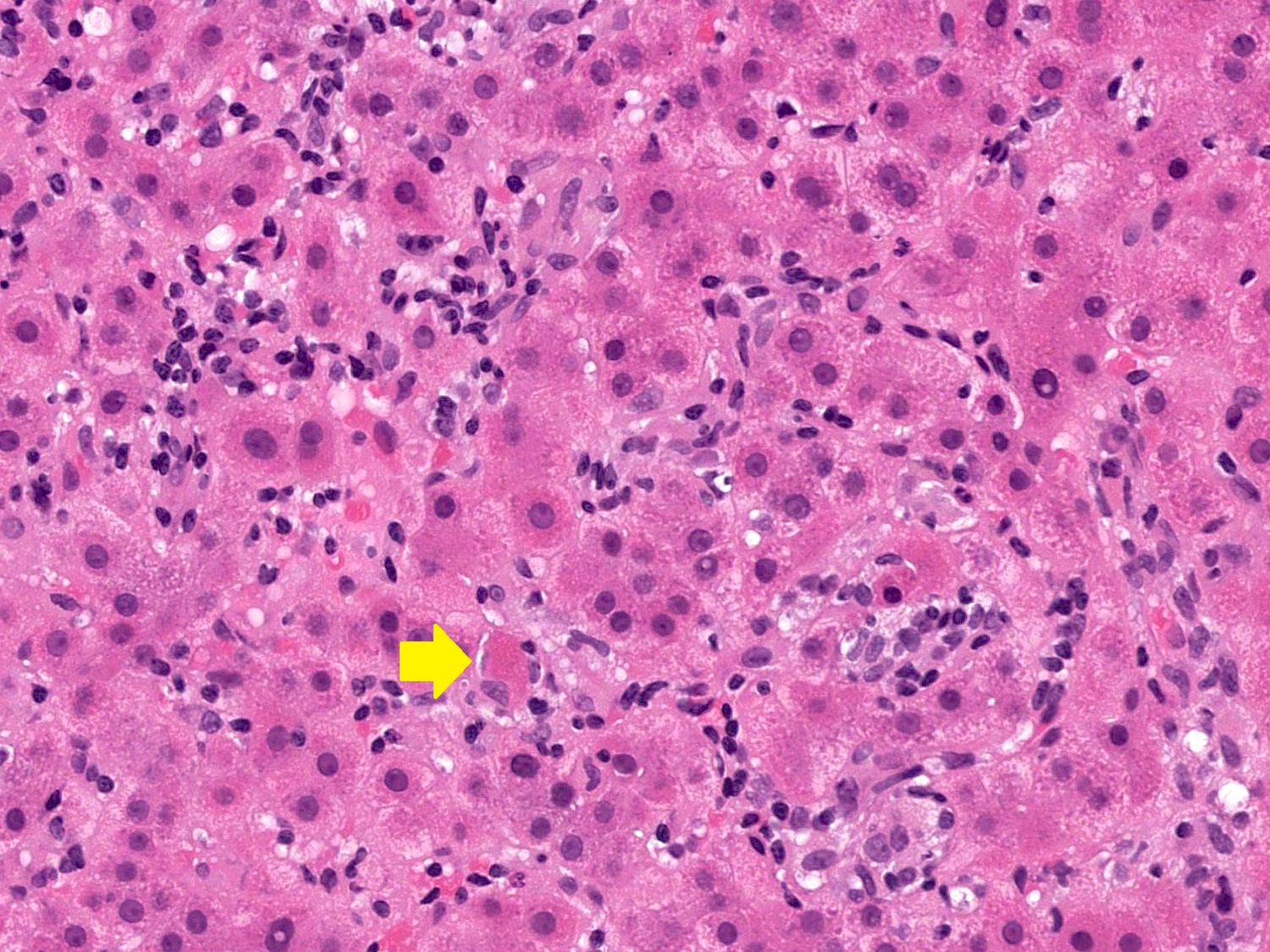
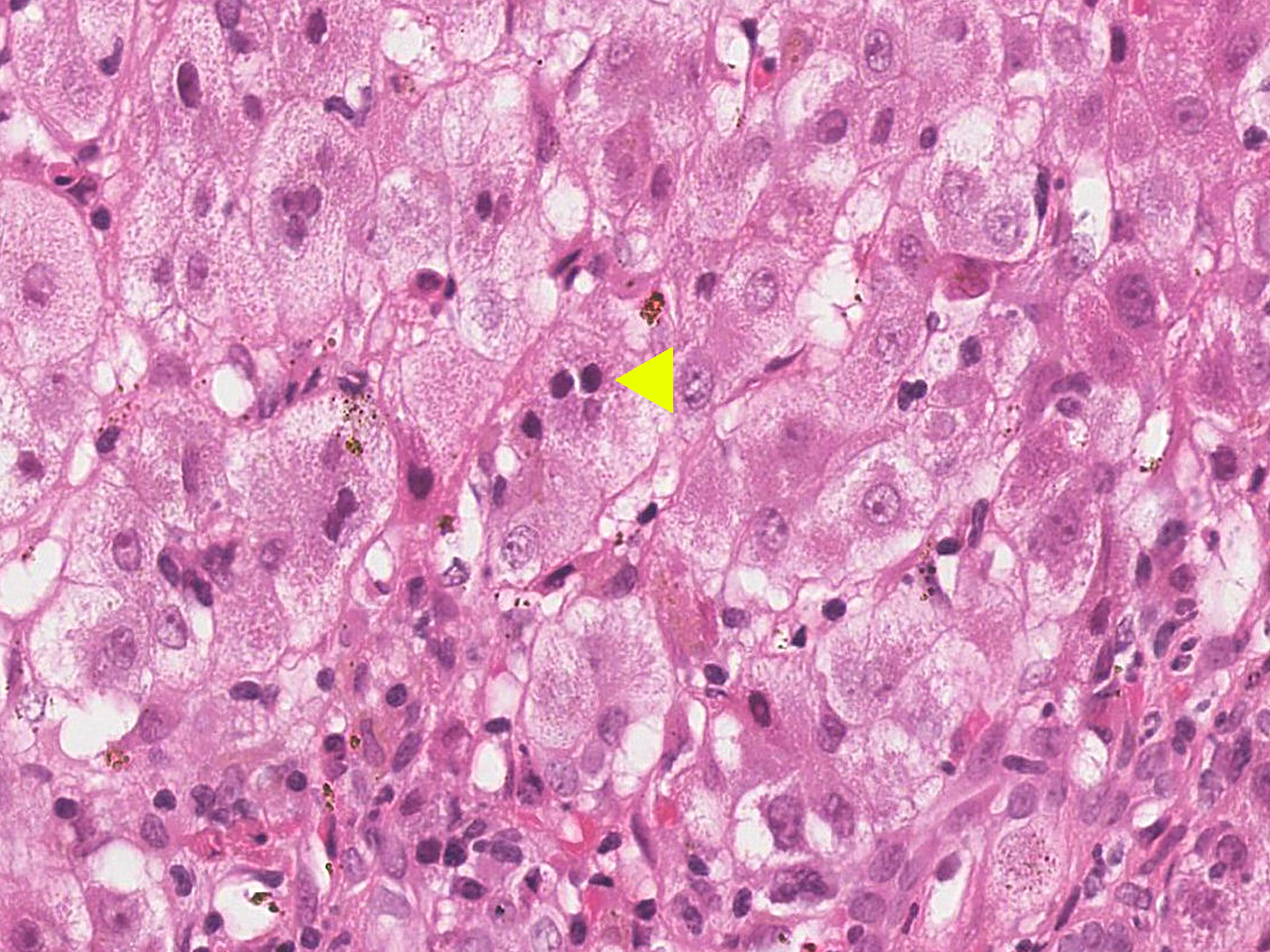
- Emperipolesis: active penetration of lymphocytes into and through a hepatocyte
- Hepatocyte rosettes
- Variable fibrosis (about 10% of autoimmune hepatitis does not show any fibrosis at initial presentation)
- Lobular necroinflammatory activity: usually accompanied by portal and periportal inflammation
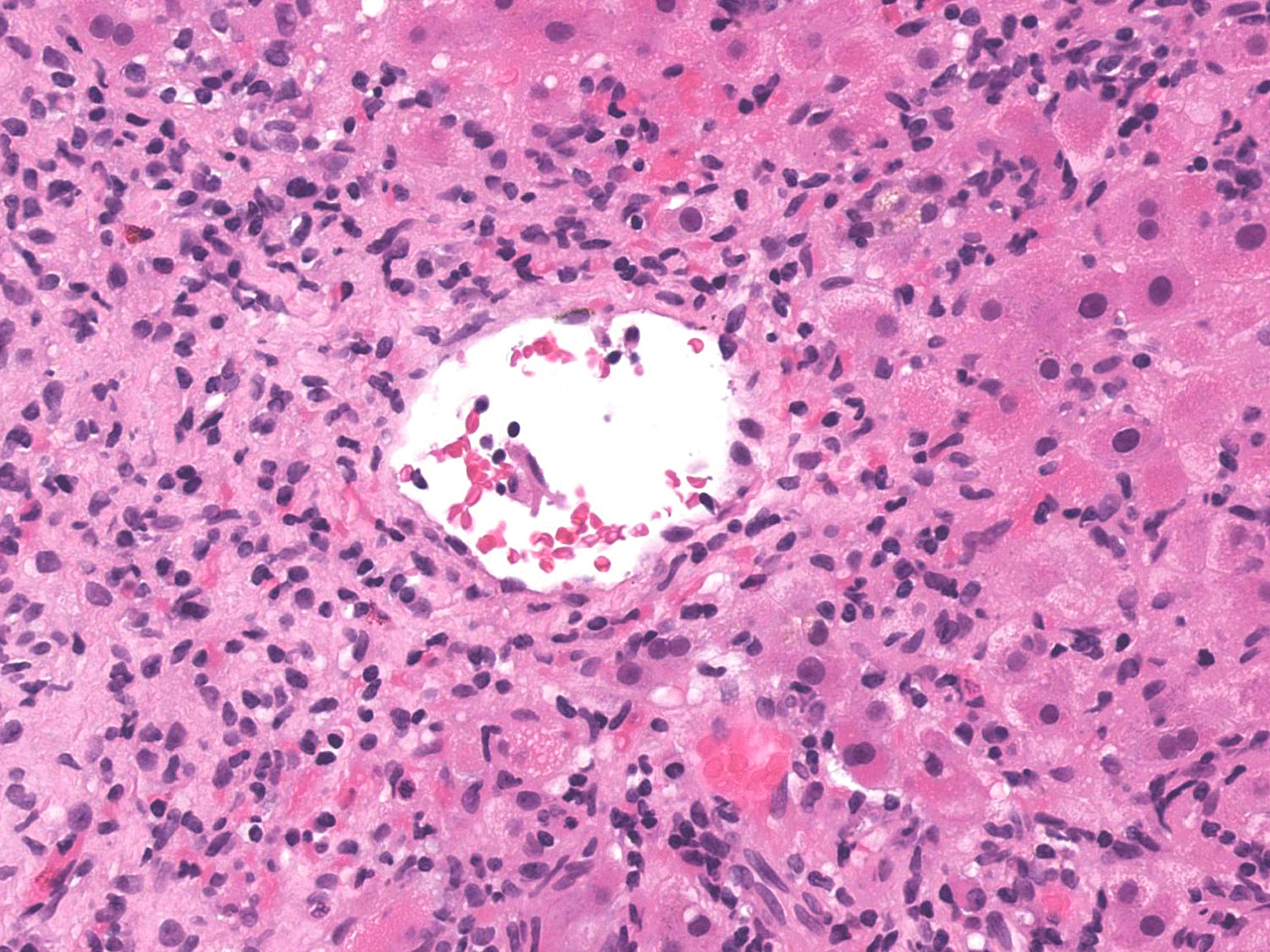
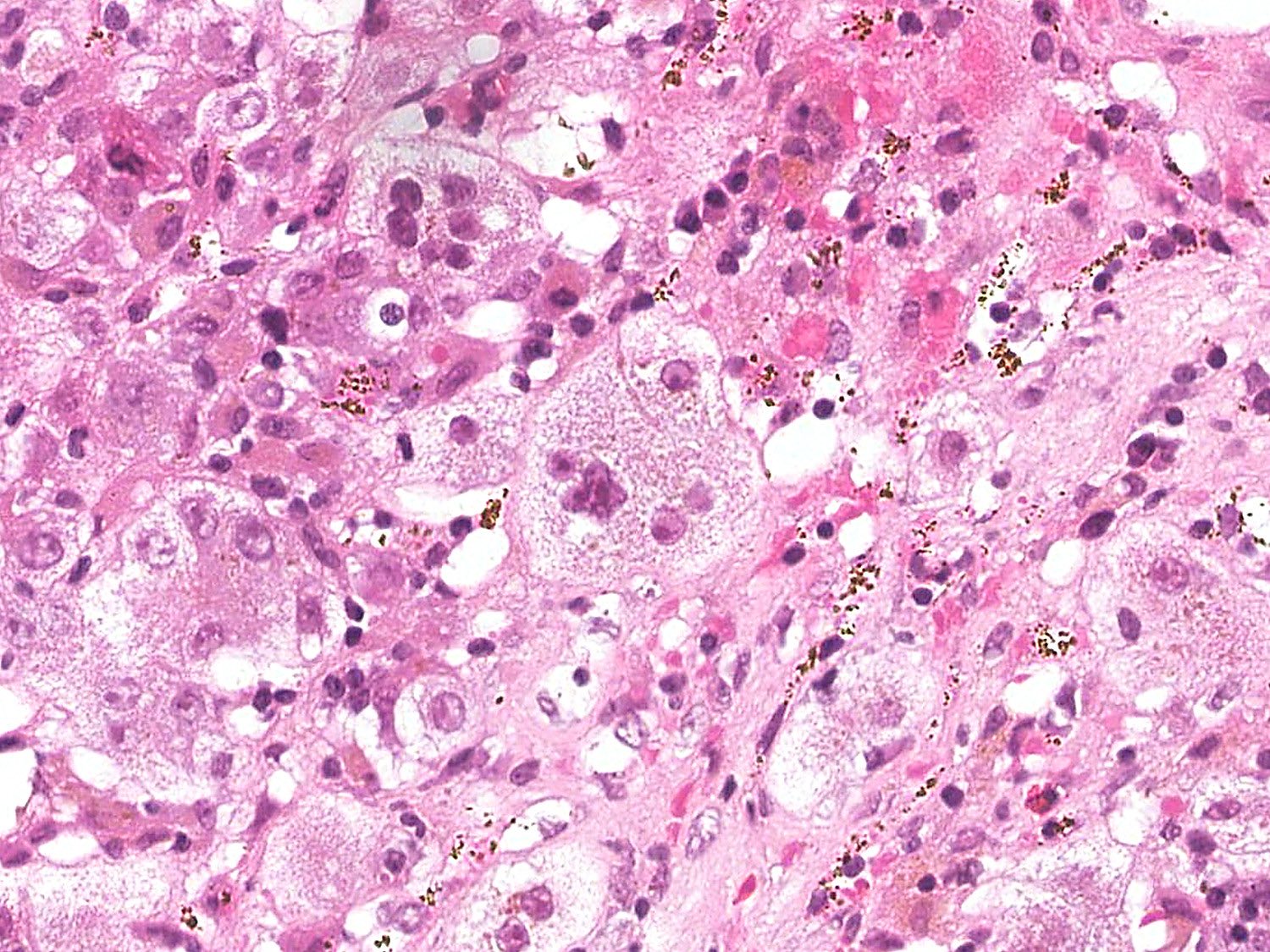
- Uncommon morphological changes:
- Perivenular necrosis: up to 17% of autoimmune hepatitis with or without typical portal and periportal changes; associated with more severe disease activity and lower histological stage
- Intrahepatic cholestasis (bilirubinostasis)
- Syncytial multinucleated giant cells: autoimmune hepatitis is the most common cause (30%) of postinfantile giant cell hepatitis, which is rare in adults (0.1 - 0.25% of all hepatitis) (Hepat Res Treat 2013;2013:601290)
- Mild bile duct injury / inflammation: present in up to 24% of classical autoimmune hepatitis (Hepatology 2001;34:659)
- Chronic biliary disease or overlap syndrome only need to be considered in the presence of more extensive bile duct injury, florid duct lesions, ductular reaction, ductopenia, chronic cholestasis, portal granulomas or periductal fibrosis (clinical and laboratory findings must separately be met for both autoimmune hepatitis and primary sclerosing cholangitis / primary biliary cholangitis)
- IgG4 associated autoimmune hepatitis: > 10 IgG4 positive plasma cells/high power field
- Simplified International Autoimmune Hepatitis Group scoring system:
- Typical of autoimmune hepatitis (sensitivity: 40 - 59%; specificity: 55 - 96%) (Mod Pathol 2017;30:773, Hepatology 2008;48:169)
- Interface hepatitis with lymphocytic or lymphoplasmacytic infiltrate
- Hepatocyte rosettes
- Emperipolesis
- Compatible with autoimmune hepatitis
- Chronic hepatitis with lymphocytic infiltrate
- Without all 3 typical features
- Typical of autoimmune hepatitis (sensitivity: 40 - 59%; specificity: 55 - 96%) (Mod Pathol 2017;30:773, Hepatology 2008;48:169)
- Recent studies have suggested hepatocyte rosettes and emperipolesis are not specific features of autoimmune hepatitis (Hum Pathol 2018;82:51, Mod Pathol 2017;30:773)
- Grading and staging is usually performed according to systems developed for viral hepatitis, such as Batts and Ludwig
Microscopic (histologic) images
Negative stains
- CK7 (negative in periportal hepatocytes)
- Copper
- Reference: Mod Pathol 2017;30:773
Sample pathology report
- Liver, biopsy:
- Chronic hepatitis with dense portal lymphoplasmacytic infiltrate, moderate interface hepatitis, mild lobular necroinflammatory activity and moderate periportal fibrosis (see comment)
- Comment: In view of hepatitic liver enzyme derangement, serum antinuclear antibody titer (1:320), seropositivity of smooth muscle antibody and elevated serum IgG (1.2 x ULN), the overall features are consistent with autoimmune hepatitis.
Differential diagnosis
- Clinical presentation, including serology, is very important for resolving the differential diagnosis
- Chronic hepatitis C:
- Portal lymphocytic infiltrate with lymphoid follicles
- Less severe interface hepatitis
- Mild bile duct injury
- Mild steatosis
- Drug / toxin reaction:
- No reliable histological features differentiating autoimmune hepatitis and drug induced liver injury
- Clinical correlation with drug history is essential
- Hepatitis A:
- May resemble acute / early phase of autoimmune hepatitis (prominent plasma cells and interface hepatitis)
- No fibrosis
- Viral serology is crucial
- Overlap syndromes (Ulster Med J 2011;80:15)
- Primary biliary cholangitis:
- Unequivocal bile duct injury with chronic cholatestasis
- Only mild interface hepatitis and lobular necroinflammatory activity
- Cholestatic liver enzyme derangement or seropositivity of antimitochondrial antibody
- Primary sclerosing cholangitis:
- Periductal fibrosis with chronic cholatestasis
- Only mild interface hepatitis and lobular necroinflammatory activity
- Cholestatic liver enzyme derangement or seropositivity of antineutrophil cytoplasmic antibodies
- Classic liver imaging findings helpful to establish this diagnosis
- More common in male patients
Additional references
Board review style question #1
Which of the following features are considered typical for autoimmune hepatitis?
- Florid duct lesion and seropositivity for antimitochondrial antibody
- Interface hepatitis and seropositivity for smooth muscle antibody
- Pericellular fibrosis and seropositivity for antinuclear antibody
- Periductal concentric onion skin fibrosis and seropositivity for antineutrophil cytoplasmic antibodies
Board review style answer #1
B. Interface hepatitis and seropositivity for smooth muscle antibody
Comment Here
Reference: Autoimmune hepatitis
Comment Here
Reference: Autoimmune hepatitis
Board review style question #2
A middle aged woman without significant past medical history presents with acute onset of fatigue and jaundice. Blood tests show markedly elevated aspartate aminotransferase and alanine aminotransferase and high titer antinuclear antibody. Serology for smooth muscle antibody and antimitochondrial antibody are both negative. A liver biopsy demonstrates the above finding. Which of the following laboratory results should be assessed before issuing the diagnosis of consistent with autoimmune hepatitis?
- Elevated serum IgG
- Negative serology for viral hepatitis A
- Normal serum alkaline phosphatase
- Positive serology for liver kidney microsomal
Board review style answer #2
B. Negative serology for viral hepatitis A. Portal plasmacytic infiltration with interface hepatitis may also occur in viral hepatitis A.
Comment Here
Reference: Autoimmune hepatitis
Comment Here
Reference: Autoimmune hepatitis