Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Alexander A, Pezhouh MK. Acute T cell mediated rejection. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liveracutetcellmediatedrejection.html. Accessed April 2nd, 2025.
Definition / general
- Immune mediated inflammatory response to the allograft liver by the recipient's immune system
Essential features
- Manifests as sudden elevation in liver enzymes
- Classic histologic findings include mixed portal inflammatory infiltrate, bile duct damage and endothelialitis
- Must be distinguished from recurrent disease and complications of transplant procedure (vascular / biliary damage)
Terminology
- Synonyms include acute cellular rejection, nonductopenic rejection, reversible rejection (Am J Transplant 2016;16:2816, Hepatology 1997;25:658, Liver Transpl 2012;18:1154)
ICD coding
- ICD-10: T86.41 - liver transplant rejection
Epidemiology
- Clinically significant T cell mediated rejection occurs in 20 - 40% of liver transplants with current immunosuppressive regimens
- Usually occurs 5 - 30 days after transplant but can occur months to years later (Am J Transplant 2009;9:301)
Pathophysiology
- Host T cells interact with donor HLA, become activated, then recruit macrophages and granulocytes which mediate tissue destruction (Clin Biochem 2016;49:320)
Clinical features
- Generally mild and nonspecific
- Can be asymptomatic or present with fever, abdominal pain, hepatomegaly or fatigue
Diagnosis
- Requires histologic confirmation on liver biopsy
Laboratory
- In most cases, acute T cell mediated rejection is suspected when there is a relatively abrupt increase in liver enzymes above their baseline (Surg Pathol Clin 2018;11:431)
- Patients may have subtherapeutic levels of antirejection medications (e.g., tacrolimus)
Prognostic factors
- Risk factors and demographics have not been clearly defined, though increased severity of histologic rejection indicates worse outcome for graft if not treated (Am J Med Sci 2018;356:23)
Case reports
- 21 month old girl with nonanastomotic biliary stricture and acute cellular rejection (Exp Clin Transplant 2012;10:176)
- 2 year old girl with HHV 6 infection after liver transplantation with acute graft rejection (Pediatr Transplant 2011;15:E126)
- 48 year old man with acute rejection and novel H1N1 influenza A infection (Hepatobiliary Pancreat Dis Int 2010;9:658)
- 53 year old man with acute graft rejection triggered by interferon treatment for hepatitis C (Transplant Proc 2017;49:1634)
- 67 year old woman with acute liver graft rejection after ipilimumab therapy (Ann Oncol 2017;28:2619)
Treatment
- Most patients with histologically mild rejection do not require additional immunosuppression and show no adverse outcomes
- Moderate and severe rejection are usually treated with additional immunosuppression (Hepatology 1997;25:658)
Microscopic (histologic) description
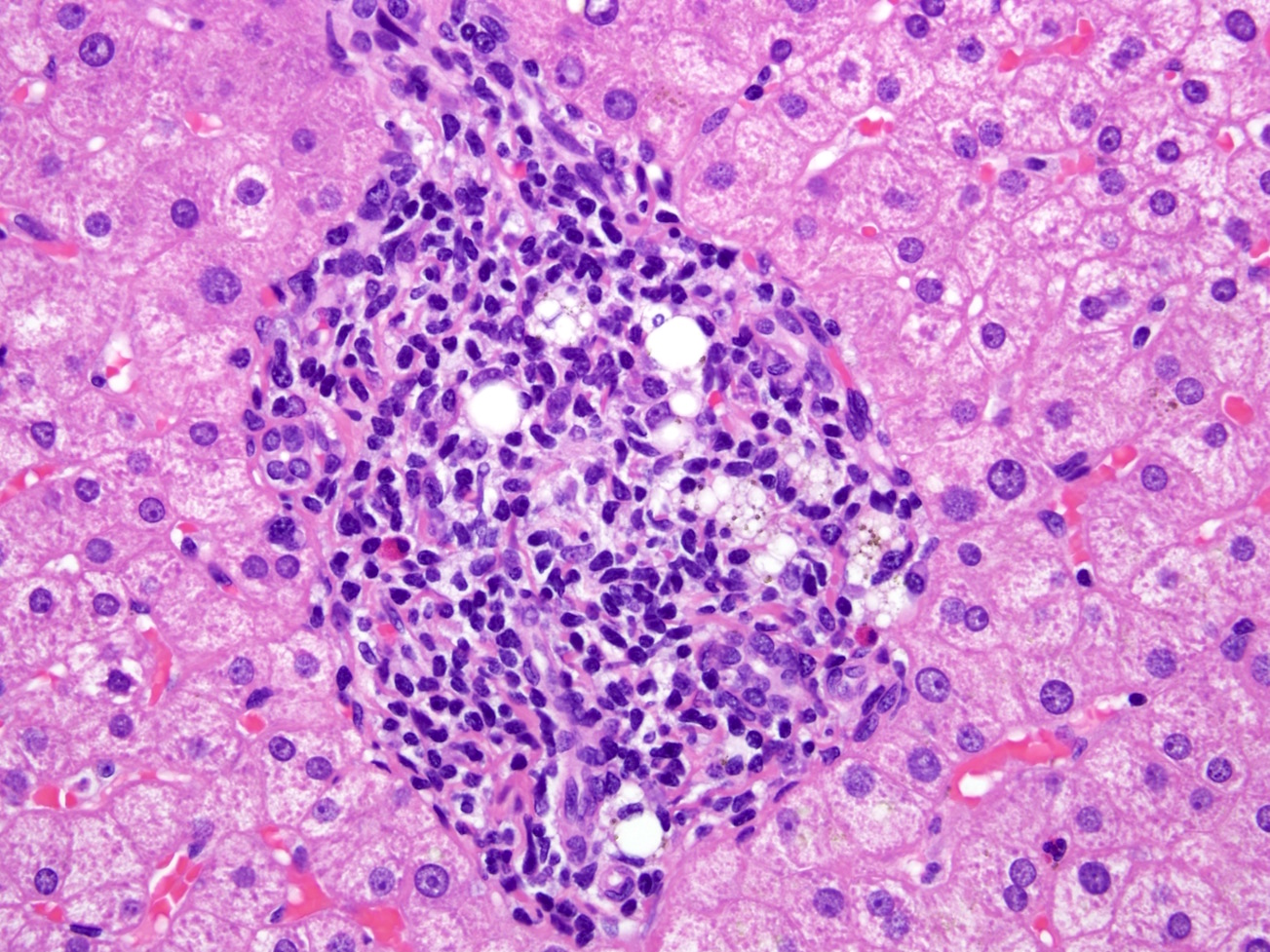
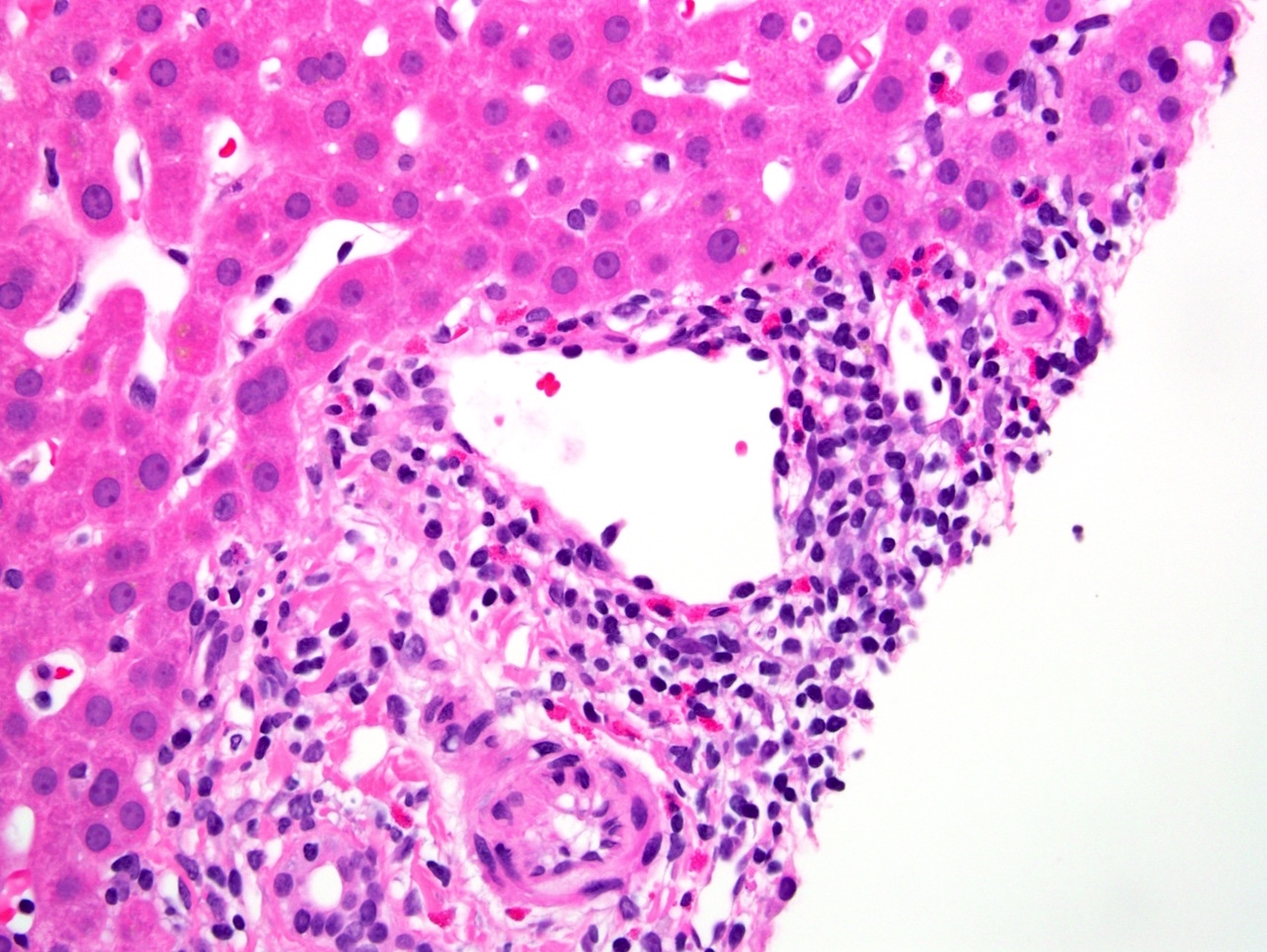
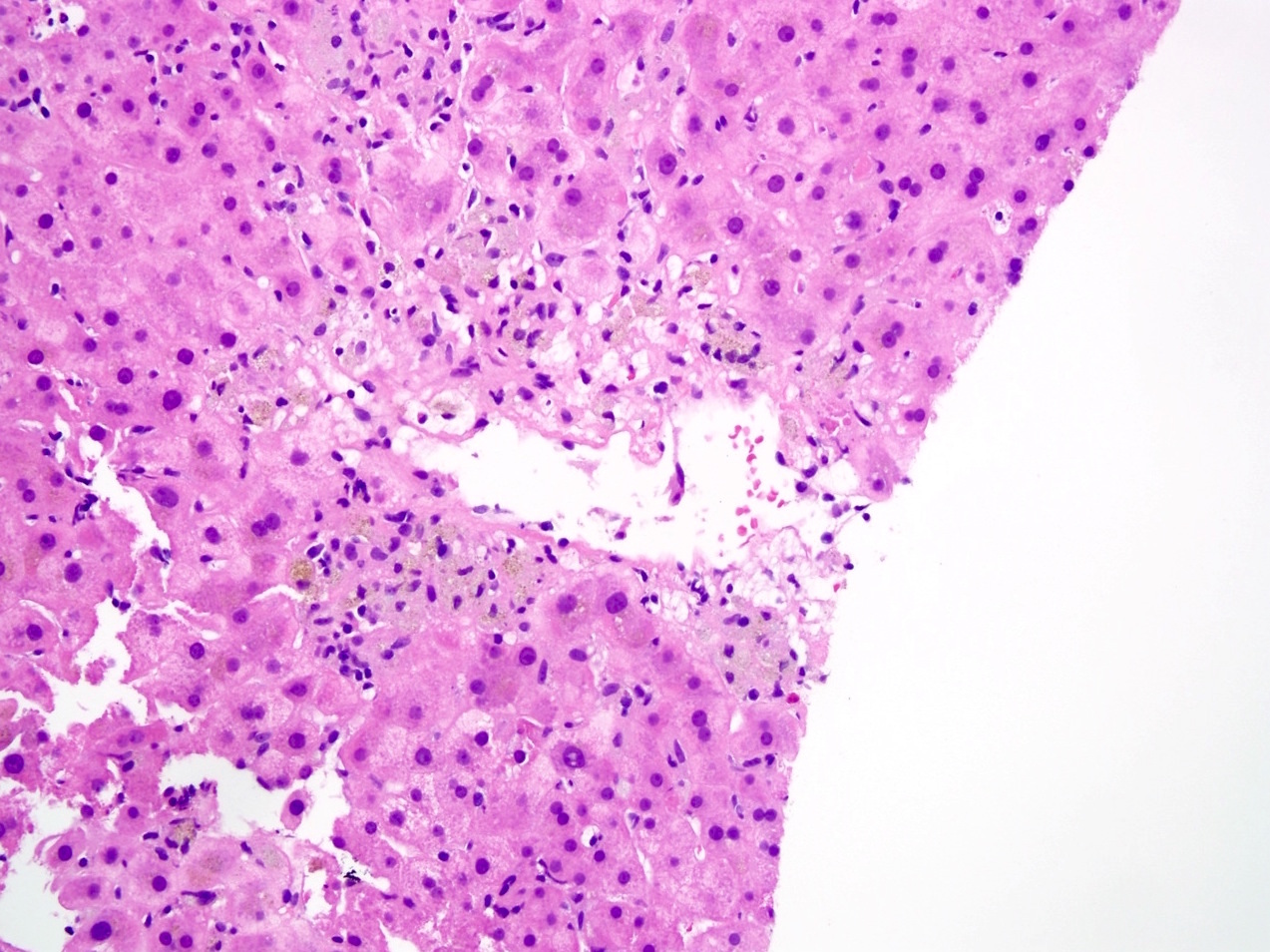
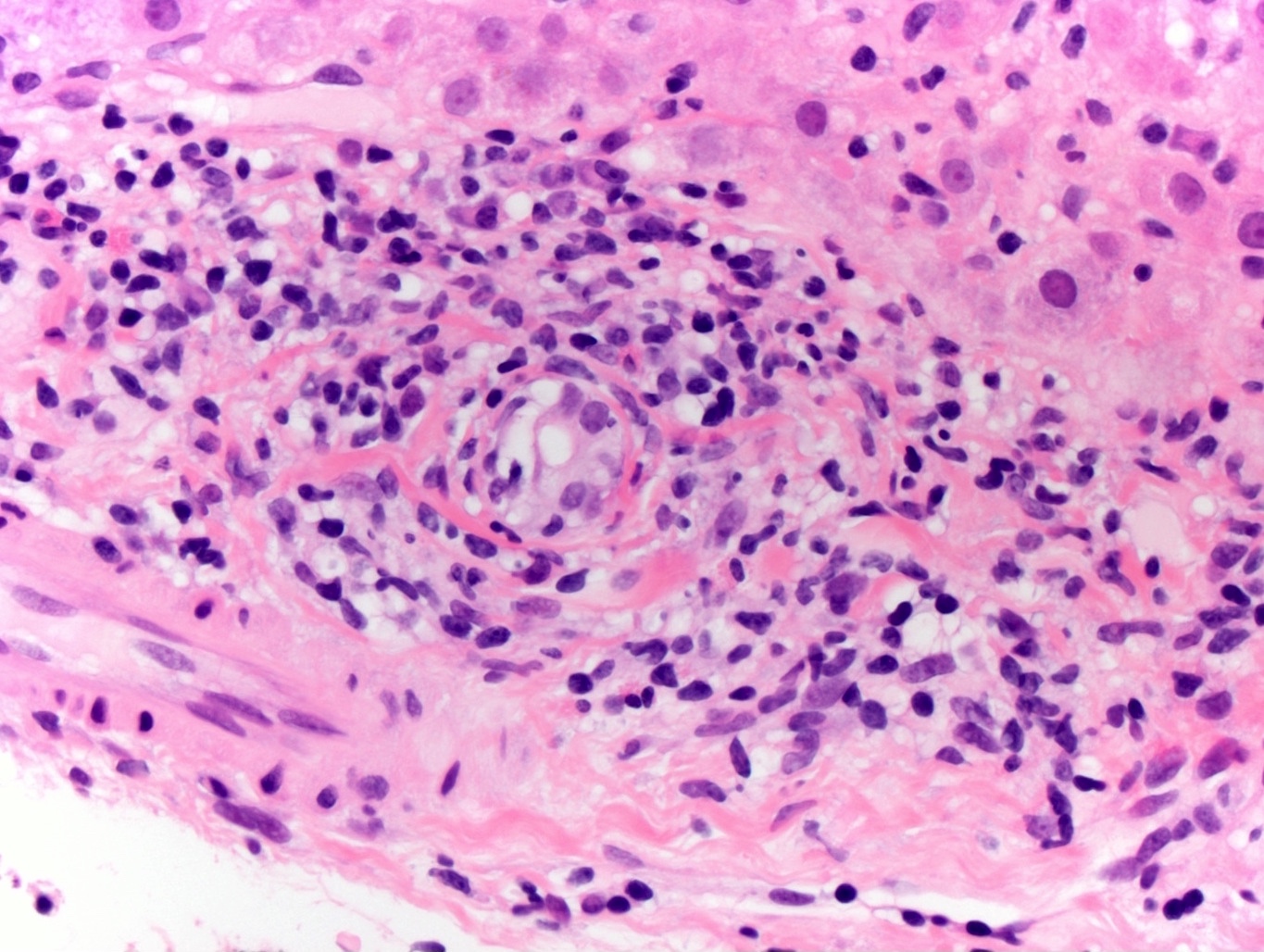
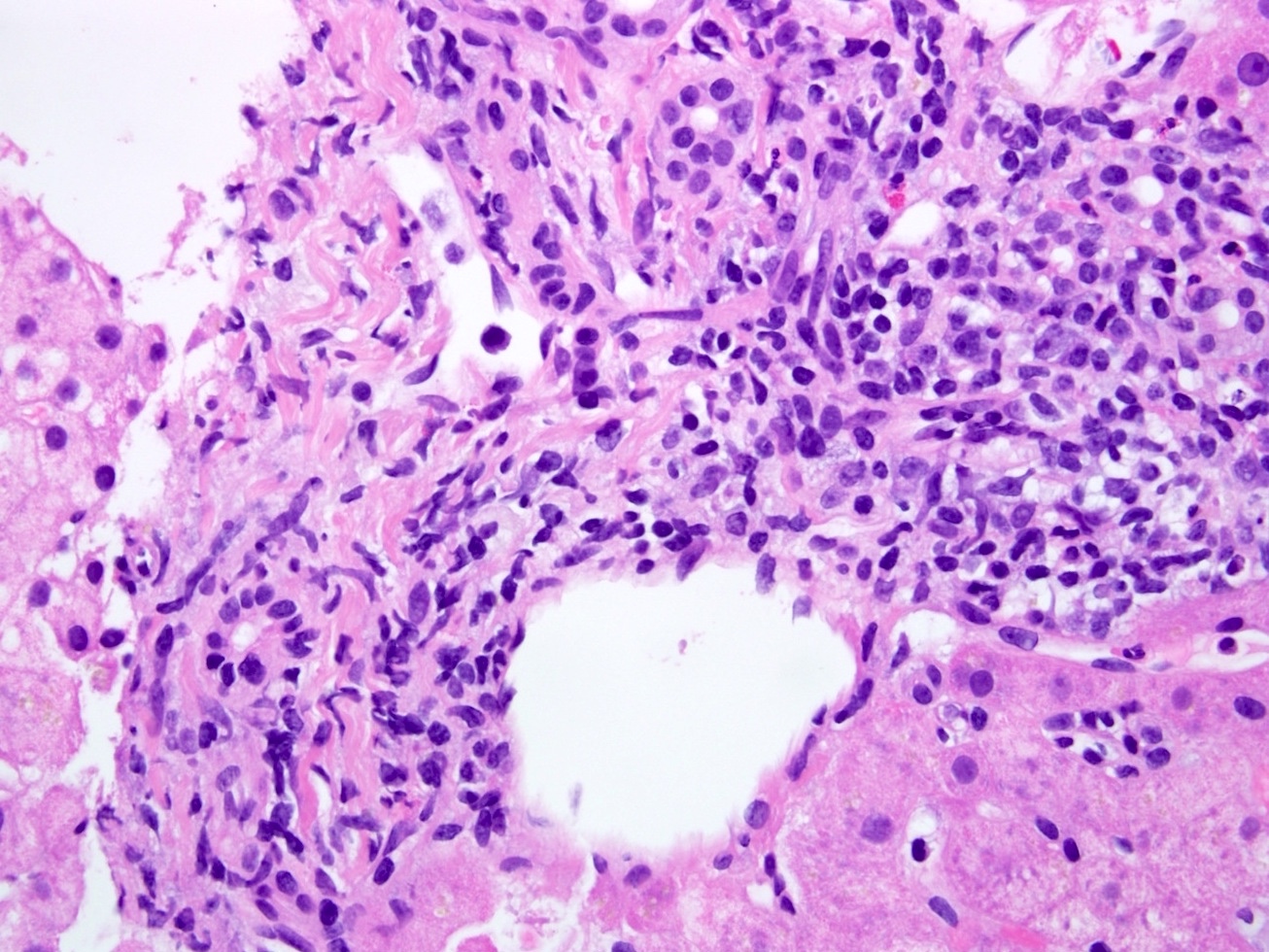
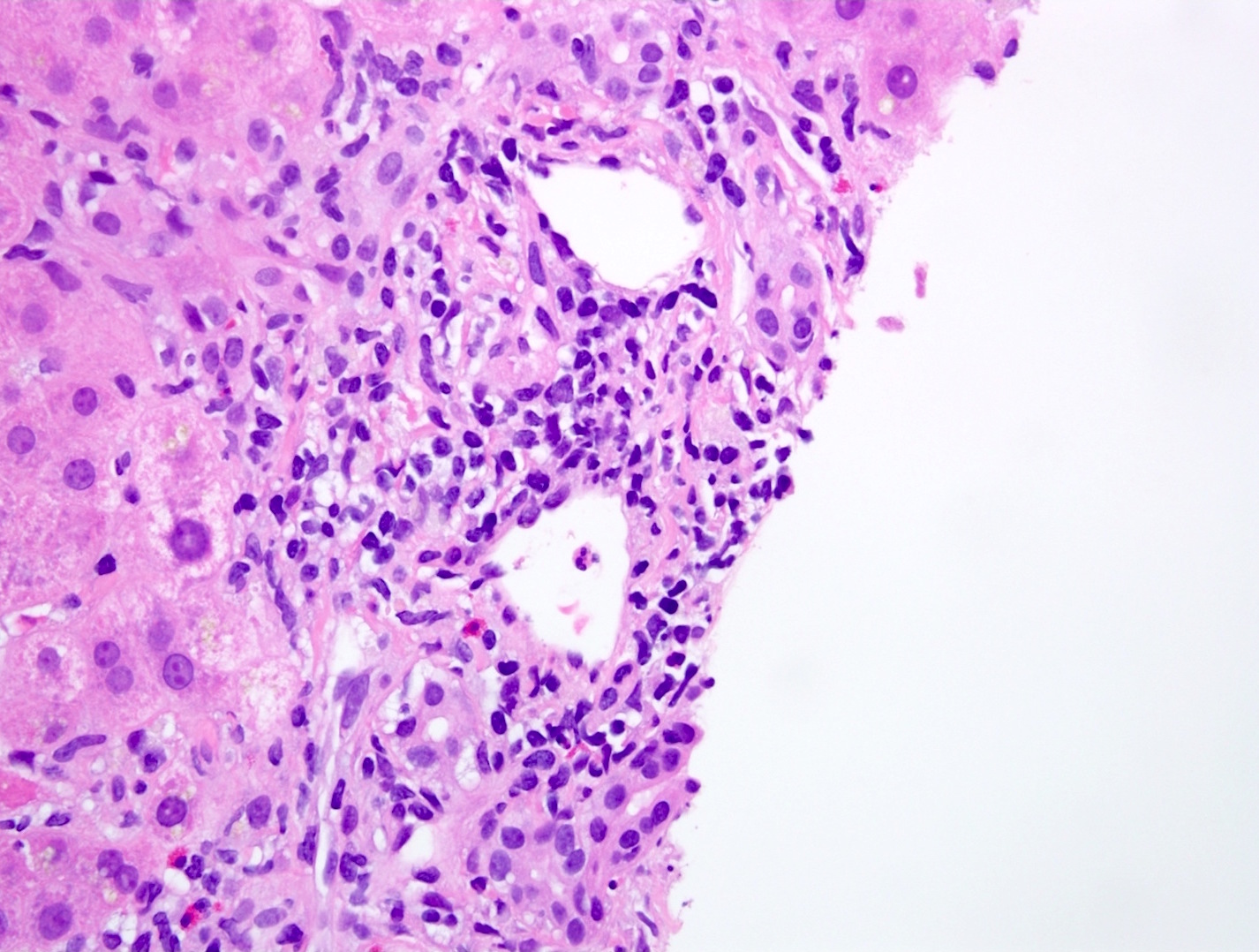
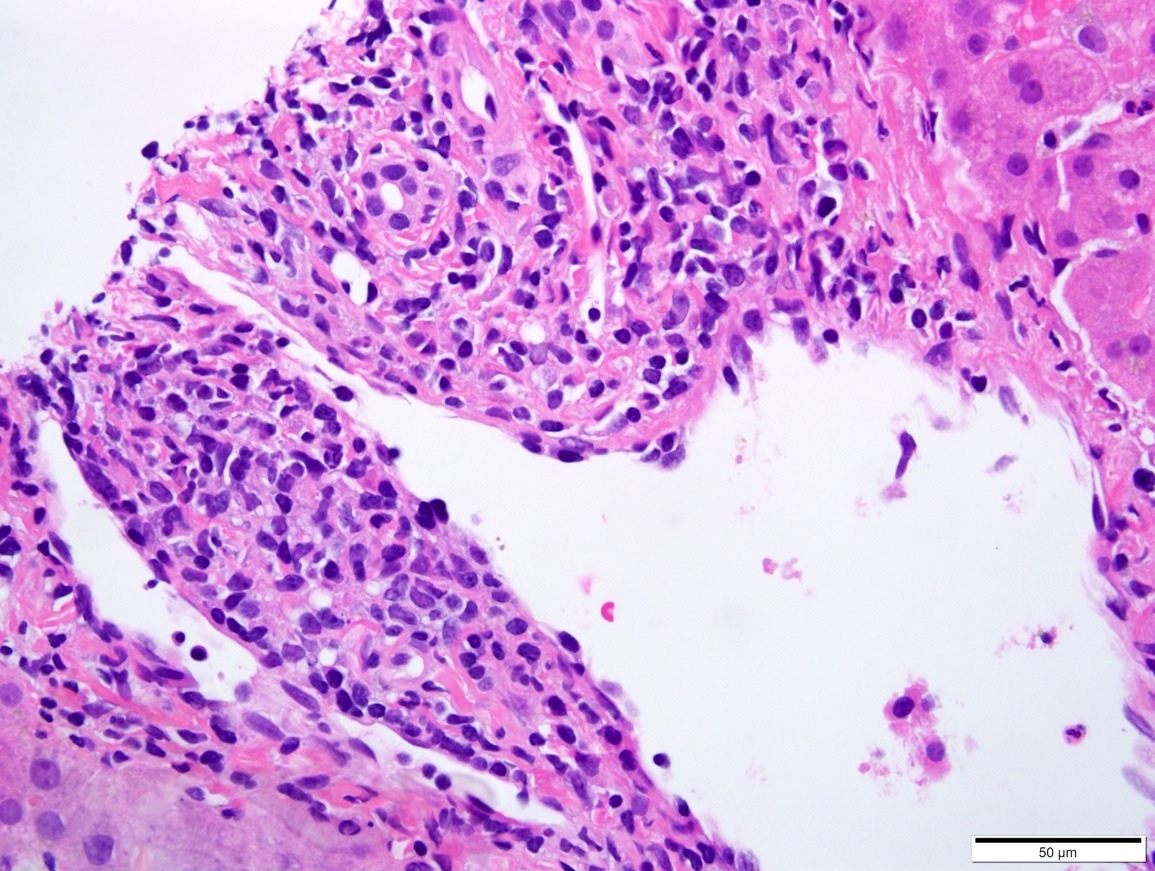
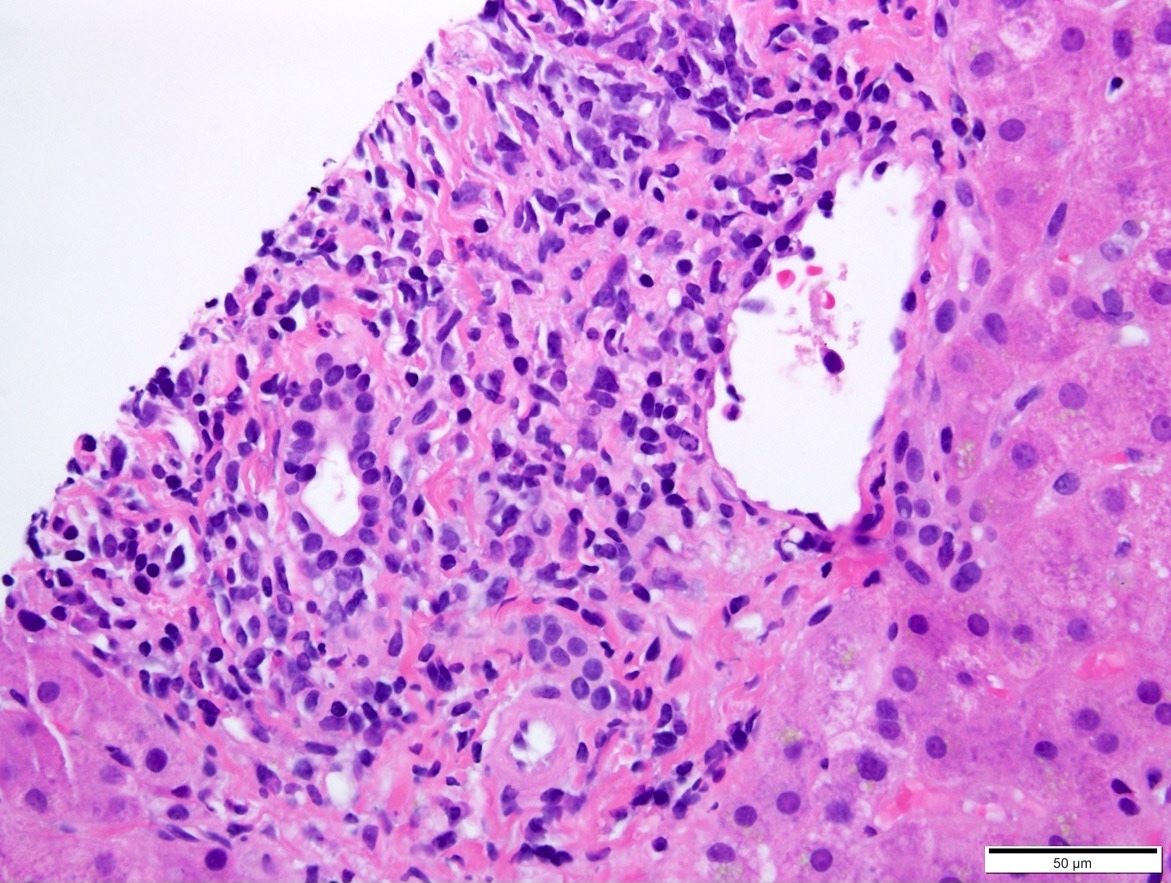
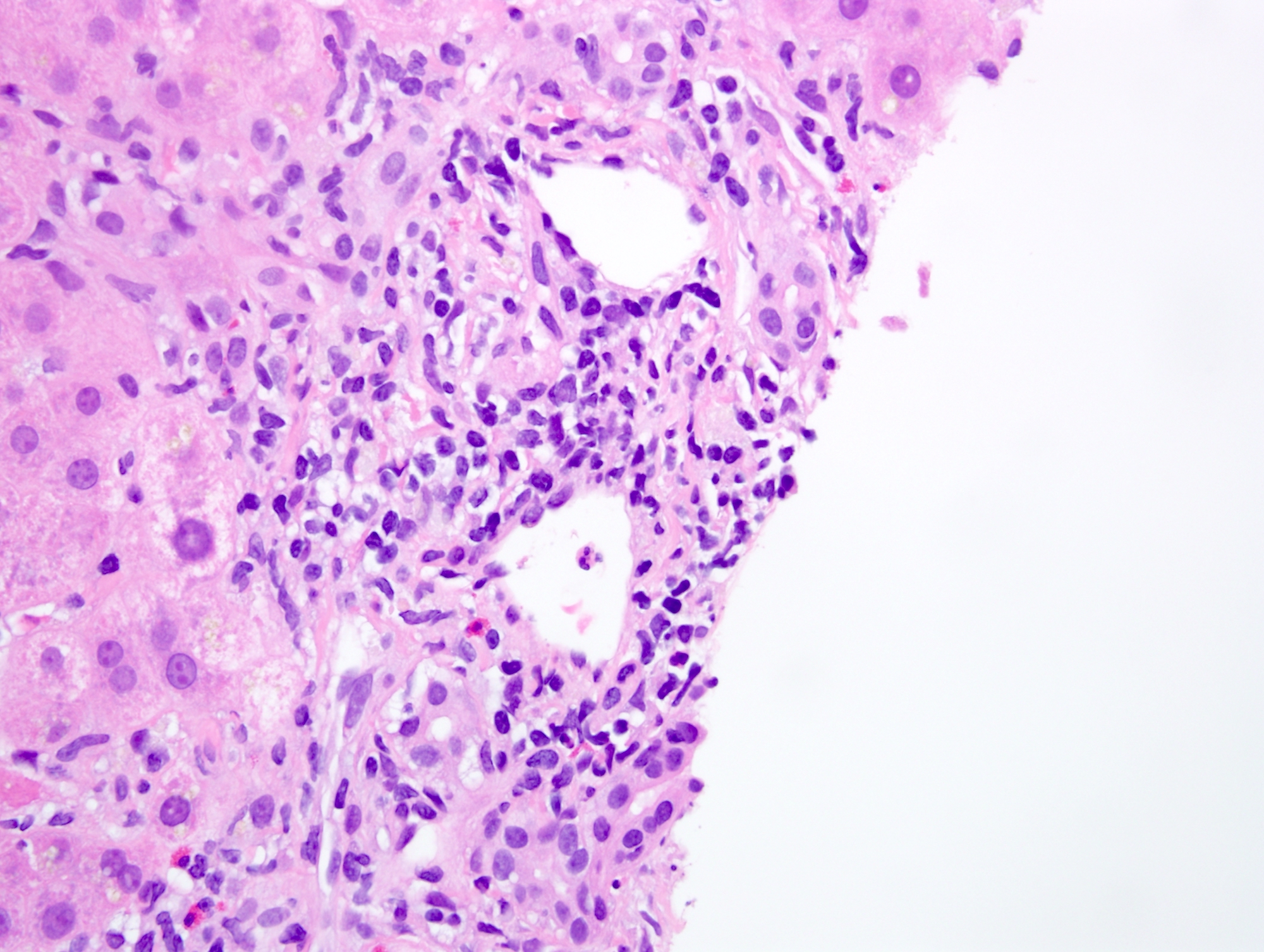
- Typical T cell mediated rejection is characterized by (at least 2 out of 3):
- Mixed portal inflammatory infiltrates: mainly lymphocytes (can appear activated, with larger nuclei and prominent nucleoli) with few eosinophils, plasma cells and possibly neutrophils
- Bile duct injury: intraepithelial lymphocytes in bile duct epithelium with injury such as apoptosis, disordered polarity, vacuolization and increased N:C ratio of the epithelial cells
- Endothelialitis (either in portal veins or central veins): injured / reactive appearing endothelial cells with lymphocytes adjacent and underneath, lifting the endothelial cells from the basement membrane or lymphocytes within the lumen, adherent to endothelial cells
- Other rare patterns of acute T cell mediated rejection include central perivenulitis variant and lobular variant (Transpl Int 2010;23:971, Mod Pathol 2015;28:1275)
- Banff criteria for acute T cell mediate rejection grading (Am J Transplant 2016;16:2816)
- Indeterminate: portal or perivenular inflammatory infiltrate without sufficient tissue damage to meet criteria for a diagnosis of rejection
- Mild: rejection type infiltrate in less than 50% of the portal tracts (often mild and confined to the portal tracts) or less than 50% of the perivenular areas without confluent necrosis / hepatocyte dropout (in cases with isolated perivenular infiltrates)
- Moderate: rejection type infiltrate, expanding more than 50% of portal tracts or perivenular areas with confluent necrosis / hepatocyte dropout limited to a minority of perivenular areas
- Severe: similar to moderate rejection but with spillover into periportal areas or moderate to severe perivenular inflammation extending into the hepatic parenchyma with perivenular hepatocyte necrosis of majority of perivenular areas
- Some centers also report the rejection activity score (Liver Transpl 2006;12:1144):
Portal inflammation Bile duct injury Venous endothelial inflammation Score 1 Mostly lymphocytic inflammation involving minority of portal tracts without expansion A minority of the ducts are cuffed and infiltrated by inflammatory cells with mild reactive changes such as increased N:C ratio of the epithelial cells Subendothelial lymphocytic infiltration involving some but not a majority of the portal or hepatic venules Score 2 Expansion of most or all portal tracts by a mixed infiltrate (containing lymphocytes with occasional blasts, neutrophils and eosinophils)
Consider acute antibody mediated rejection (AMR) if eosinophils are conspicuous and accompanied by edema and microvascular endothelial cellMost or all of the ducts infiltrated by inflammatory cells with less than 50% showing degenerative changes such as nuclear pleomorphism, disordered polarity and cytoplasmic vacuolization of the epithelium Subendothelial infiltration involving most or all of the portal or hepatic venules with or without confluent hepatocyte necrosis / dropout involving a minority of perivenular regions Score 3 Same as score 2 with inflammatory spillover into the periportal parenchyma As above for score 2, with most or all of the ducts showing degenerative changes or focal luminal disruption As above for 2, with moderate or severe perivenular inflammation that extends into the perivenular parenchyma and is associated with perivenular hepatocyte necrosis involving a majority of perivenular regions
Microscopic (histologic) images
Positive stains
- Immunostains are not necessary and often not useful
- In cases where the differential includes lymphoproliferative disorders, immunophenotyping the lymphocytes can be helpful: acute cellular rejection is predominantly T cell infiltrate (CD3 positive)
- C4D stain can be considered in cases where an element of antibody mediated rejection is suspected (Am J Transplant 2016;16:2816)
Sample pathology report
- Liver, biopsy, __ days posttransplant:
- Mild mixed portal inflammation with rare ductitis and bile duct injury, favor acute cellular rejection (mild) (see comment)
- Comment: The biopsy is adequate, consisting of 1 core containing up to at least 13 portal tracts for evaluation. There is mixed mild portal inflammation, predominantly composed of lymphocytes with rare eosinophils, plasma cells and neutrophils. Although there is no definitive endothelialitis, rare ductitis and bile duct injury are identified. Native bile ducts are present in the majority of the portal tract. PAS and PASD stains illustrate bile ducts and show no PAS+, diastase resistant globules. Trichrome and reticulin stains are unremarkable. An iron stain is negative. Overall, the findings of portal inflammation, rare ductitis and bile duct injury raise the possibility of acute cellular rejection (favor mild). Clinical correlation is recommended.
Differential diagnosis
- Recurrent hepatitis C:
- Lobular inflammation with hepatocyte injury (single cell apoptosis or spotty necrosis involving groups of hepatocytes)
- In more severe cases, lymphocytic interface hepatitis can be seen (Ann Transplant 2008;13:12)
- Posttransplant lymphoproliferative disorder and Epstein-Barr virus:
- Monomorphic PTLD will have clonal B cell proliferation
- Polymorphic and nondestructive PLTD will show an inflammatory infiltrate consisting of lymphocytes and plasma cells; endothelialitis should not be present
- Immunophenotyping the lymphocytes can be helpful: T cell mediated rejection is predominantly T cell infiltrate (CD3 positive) (Pediatr Transplant 2019;23:e13357)
- Hepatitis E:
- Presentation is variable and can include lobular disarray, lobular and portal inflammation, hepatocyte necrosis / regeneration and potentially severe interface activity; immunohistochemistry or serology may be useful in diagnosis (Adv Anat Pathol 2018;25:273, Clin Res Hepatol Gastroenterol 2018;42:e68)
- Human herpesvirus 6:
- May show mild inflammation and hepatocyte injury; no endothelialitis or bile duct injury (Transpl Infect Dis 2019;21:e13014, Pediatr Transplant 2011;15:E126)
- Drug induced liver injury:
- Portal edema, portal and lobular mixed inflammatory infiltrate with lymphocytes, eosinophils and plasma; may show endothelialitis, bile duct injury, perivenular necrosis, hepatocyte injury
- Can often be difficult to differentiate histologically, requiring clinical correlation
- Late T cell mediated rejection:
- Characterized by loss of native small bile ducts in portal tracts
- Loss of portal arterioles and sinusoidal foam cell accumulation can also be seen (Hepatology 2000;31:792)
- Antibody mediated rejection:
- Evidence of vascular injury such as portal edema, endothelial cell hypertrophy and eosinophilia within portal microvasculature can be seen in addition to more nonspecific findings such as hepatocyte swelling, ductular reaction and cholestasis (J Immunol Res 2017;2017:3234906)
- Large bile duct injury:
- Large bile duct obstruction due to stricture, gallstones and malignancy can lead to cholestasis and bile ductular reaction
- Cholestasis usually more severe than seen in acute T cell mediated rejection (J Clin Pathol 2018;71:72)
Additional references
Board review style question #1
- A 45 year old man with a history of cirrhosis secondary to hepatitis C infection who is status post liver transplantation 3 years ago presents with mildly elevated liver enzymes (AST 78, ALT 75, ALK Phos 100). A liver biopsy is performed. Which of the following findings would support a diagnosis of acute T cell mediated rejection over a recurrent hepatitis C infection?
- Endothelialitis
- Hepatocyte apoptosis
- Interface hepatitis
- Lobular disarray
- Lobular lymphocytic inflammation
Board review style answer #1
A. Endothelialitis. Of the listed choices, endothelialitis is the most useful finding in supporting a diagnosis of acute cellular rejection. The other options can all be seen in hepatitis C infection, and in the absence of endothelialitis and bile duct injury, may suggest reactivation of hepatitis C infect in a posttransplant patient.
Comment Here
Reference: Acute T cell mediated rejection
Comment Here
Reference: Acute T cell mediated rejection
Board review style question #2
- Based on the grading system for acute T cell mediated rejection, which of the following findings would favor a diagnosis of moderate T cell mediated rejection?
- Diffuse portal inflammatory infiltrate consisting of lymphocytes and eosinophils. Over 50% of central veins show venulitis and perivenular hepatocyte necrosis.
- Endothelialitis in less than 50% of portal areas. No central venulitis or bile duct injury is seen, no significant inflammatory infiltrate is identified.
- Less than 50% of central veins show perivenular necrosis. No inflammation seen in portal areas, no endothelialitis, no bile duct injury.
- Less than 50% of portal areas show expansion by an inflammatory infiltrate consisting of lymphocytes and eosinophils. No endothelialitis or bile duct injury.
- More than 50% of portal areas show expansion by an inflammatory infiltrate consisting of lymphocytes and eosinophils with endothelialitis and occasional bile duct injury.
Board review style answer #2
E. Moderate T cell mediated rejection should involve at least 50% of portal areas and well as occasional central veins. Portal inflammatory infiltrates, endothelilaitis and bile duct injury should also be present.
Comment Here
Reference: Acute T cell mediated rejection
Comment Here
Reference: Acute T cell mediated rejection