Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Napit AR, Mannan R. Cytomegalovirus hepatitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverCMV.html. Accessed March 29th, 2025.
Definition / general
- Infection of the liver caused by cytomegalovirus (CMV), causing liver damage, ranging from asymptomatic to liver inflammation, failure and even death
- Most clinically significant infections are seen in immune compromised hosts, such as in AIDS, organ transplant recipients, hematopoietic stem cell transplantation, pregnancy and congenital infection (Microbiol Spectr 2016;4:1)
Essential features
- Mostly seen in immunocompromised hosts (AIDS, organ transplant recipient, hematopoietic stem cell transplantation)
- Histopathology characterized by cytomegaly, with cytoplasmic and nuclear inclusions
Terminology
- CMV hepatitis
- HHV5 hepatitis
ICD coding
- ICD-10: B25.1 - cytomegaloviral hepatitis
Epidemiology
- Seroprevalence of cytomegalovirus ranges from 45 to 100%, with higher prevalence in South America, Africa and Asia and lowest in Western Europe and the United States
- Seropositivity is independently associated with advancing age, female sex, foreign birthplace, high household crowding and low socioeconomic status (Gastroenterol Clin North Am 2020;49:331)
- Incidence of cytomegalovirus hepatitis in immunocompromised hosts ranges from 2 to 34% due to reactivation or reinfection (Clinics (Sao Paulo) 2015;70:515, Cureus 2020;12:e10745)
- Cytomegalovirus hepatitis is noted in 17% of liver transplant recipients (Clin Infect Dis 1996;22:537)
Sites
- Liver parenchyma (hepatocytes, Kupffer cells, biliary epithelium, endothelial cells)
Pathophysiology
- Can be acquired before birth, at birth or later in life
- Following initial active infection, it may remain latent for years; reactivation usually occurs in the setting of immune compromise
- Hematogenous spread leads to systematic viral dissemination involving the liver as well
- Direct cytopathogenicity: cytolytic process of cytomegalovirus
- Indirect cytopathogenicity
- Host mediated defense against virus
- Cytolytic effect of CD8+ and cytokines (IL17, IFNγ and TNF) mediated damage by CD4+
- Leading to
- Acute hepatitis
- Granulomatous hepatitis
- Necrotizing hepatitis (J Clin Transl Hepatol 2021;9:106)
- Portal vein thrombosis associated hepatitis and Budd-Chiari syndrome (Gastroenterol Clin North Am 2020;49:331)
Etiology
- Cytomegalovirus (CMV or HHV5) - a double stranded DNA virus
- Belongs to the Herpesviridae family
- Transmission through saliva, tears, urine, breast milk, semen and other body fluids
- Primary infection followed by lifelong latency
- Reactivation with visible presentation mostly in an immune compromised state (Pathogens 2019;8:213)
Clinical features
- Immunocompetent hosts can often be clinically silent
- In immunocompromised hosts, mononucleosis-like illness is a common presentation with fever, malaise, myalgia, nausea and abdominal pain
- Jaundice
- Congenital infection is characterized by asymptomatic to severe infection with jaundice, hepatosplenomegaly, encephalitis and chorioamnionitis
- Liver transplant patients can present with the symptoms of acute cellular rejection (Gastroenterol Clin North Am 2020;49:331)
Diagnosis
- Serology: titer of cytomegalovirus specific IgM and IgG (ELISA)
- Antigen detection: by immunofluorescence technique using an antibody against CMV pp65 and immediate / early antigens of cytomegalovirus
- PCR: qualitative and quantitative
- Histopathology (gold standard): H&E and immunohistochemistry
- Viral culture is an obsolete technique due to low sensitivity and longer time for diagnosis (Inflamm Intest Dis 2016;1:15)
Laboratory
- Subclinical elevation of transaminases (alanine transaminase [ALT] > aspartate aminotransferase [AST]) (J Clin Transl Hepatol 2021;9:106)
- Elevation is higher in immunocompetent patients in comparison to immunocompromised patients
- 3 - 9% of patients show an elevation in alkaline phosphatase and total bilirubin (jaundice)
- Serology
- IgM positivity indicates primary infection or viral reactivation
Radiology description
- Nonspecific findings of acute hepatitis (Radiopaedia: Acute Hepatitis [Accessed 21 February 2023])
- Ultrasound findings
- Hepatomegaly with hypoechoic echotexture
- Raised periportal echogenicity
- CT scan: not a first line imaging modality
- Hepatomegaly with possible decreased parenchymal attenuation
- Might show reduced attenuation around the portal system and hepatic hilum suggestive of periportal edema
- Might show lymphadenopathy (periportal and hepatoduodenal)
Radiology images
Prognostic factors
- Determined by underlying immunocompromised conditions and the type of immunosuppressive regimens in use
- Spontaneous resolution in immunocompetent hosts
- Mononucleosis-like pattern usually resolves within a few weeks
- Chronic liver disease is uncommon
- Reference: J Clin Transl Hepatol 2021;9:106
Case reports
- 35 year old obese woman with epigastric pain and vomiting for 2 months (Case Rep Gastroenterol 2016;10:36)
- 35 year old man presented to the emergency department with a 2 week history of low grade fever (Am J Case Rep 2020;21:e925495)
- 59 year old man with complaints of fever for 3 weeks (Cureus 2020;12:e10745)
- 64 year old woman presented with a 1 week history of lethargy and fever (BMJ Case Rep 2020;13:e234811)
- 66 year old woman presented with a 1 month history of yellow coloration of the eyes and skin, abdominal distension, dark colored stool and pale urine (World J Gastroenterol 2015;21:12505)
Treatment
- Immunocompetent patients do not need treatment and can recover without intervention
- In immunocompromised patients, treatment focuses on prevention and involves
- Prophylaxis treatment: after organ transplant with antivirals, prescribed for at least 3 months
- Preemptive treatment: for organ transplant and immunocompromised patients
- Antiviral drugs used are
- Intravenous ganciclovir
- Valganciclovir (J Clin Transl Hepatol 2021;9:106)
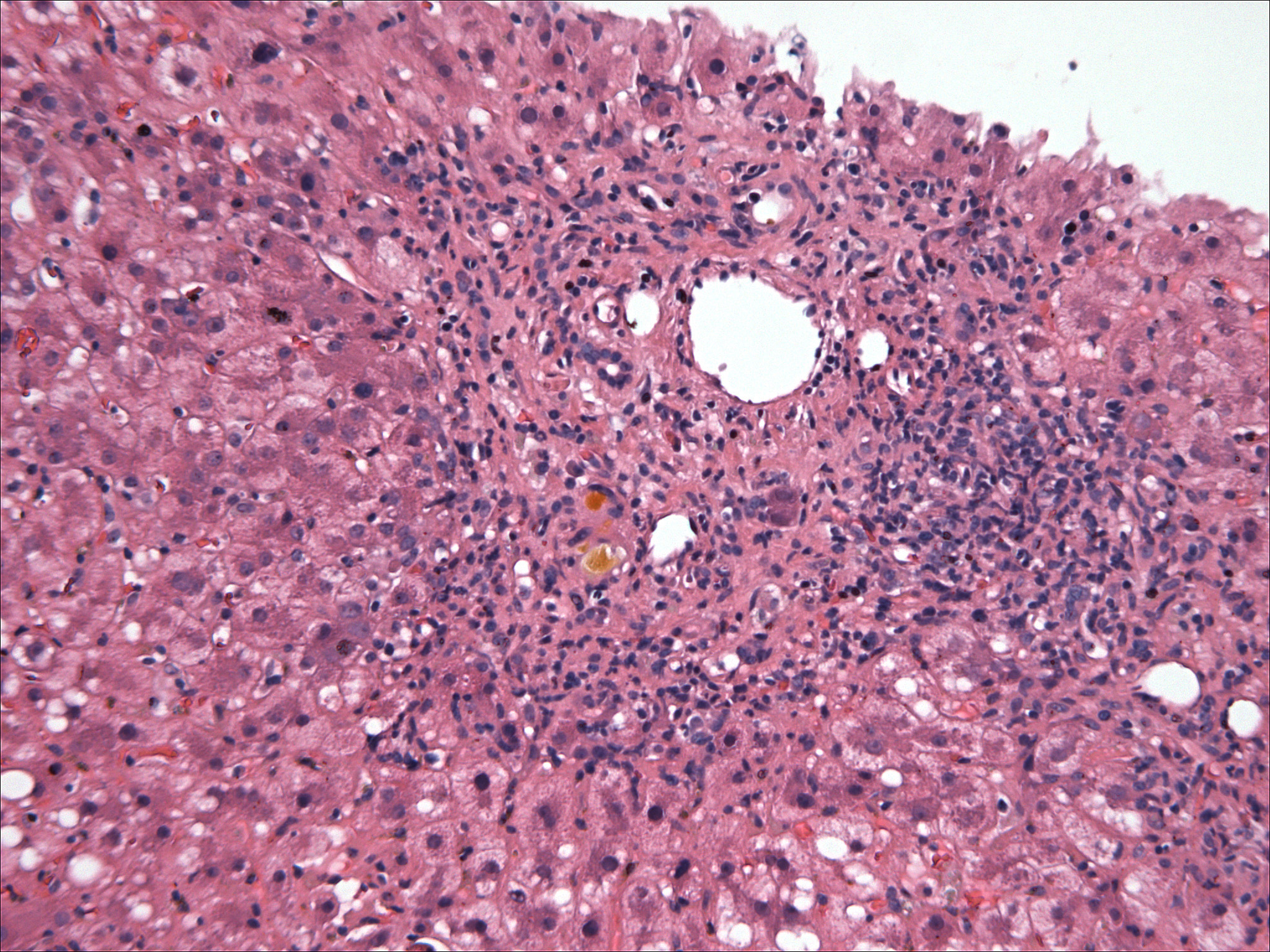
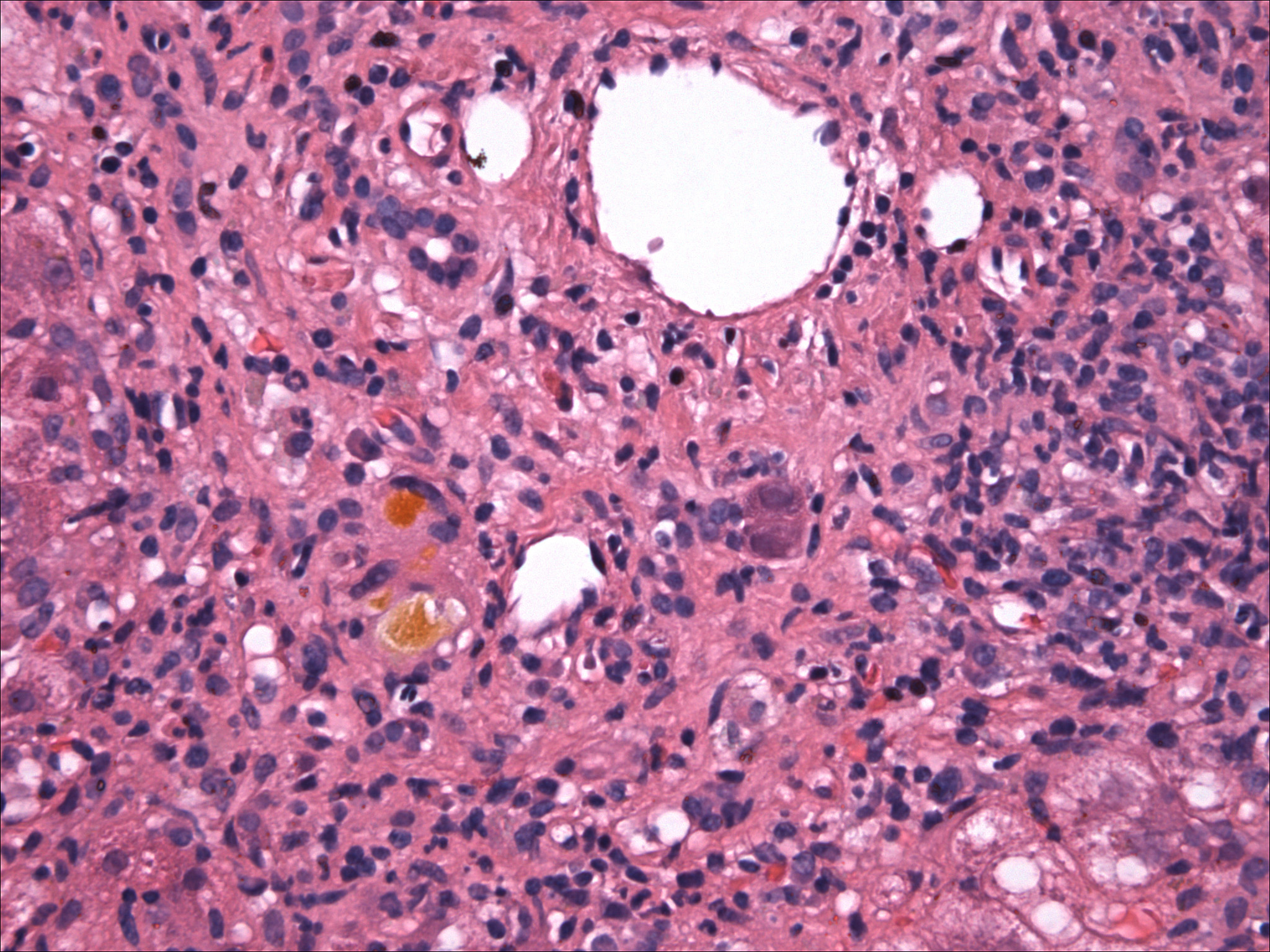
Microscopic (histologic) description
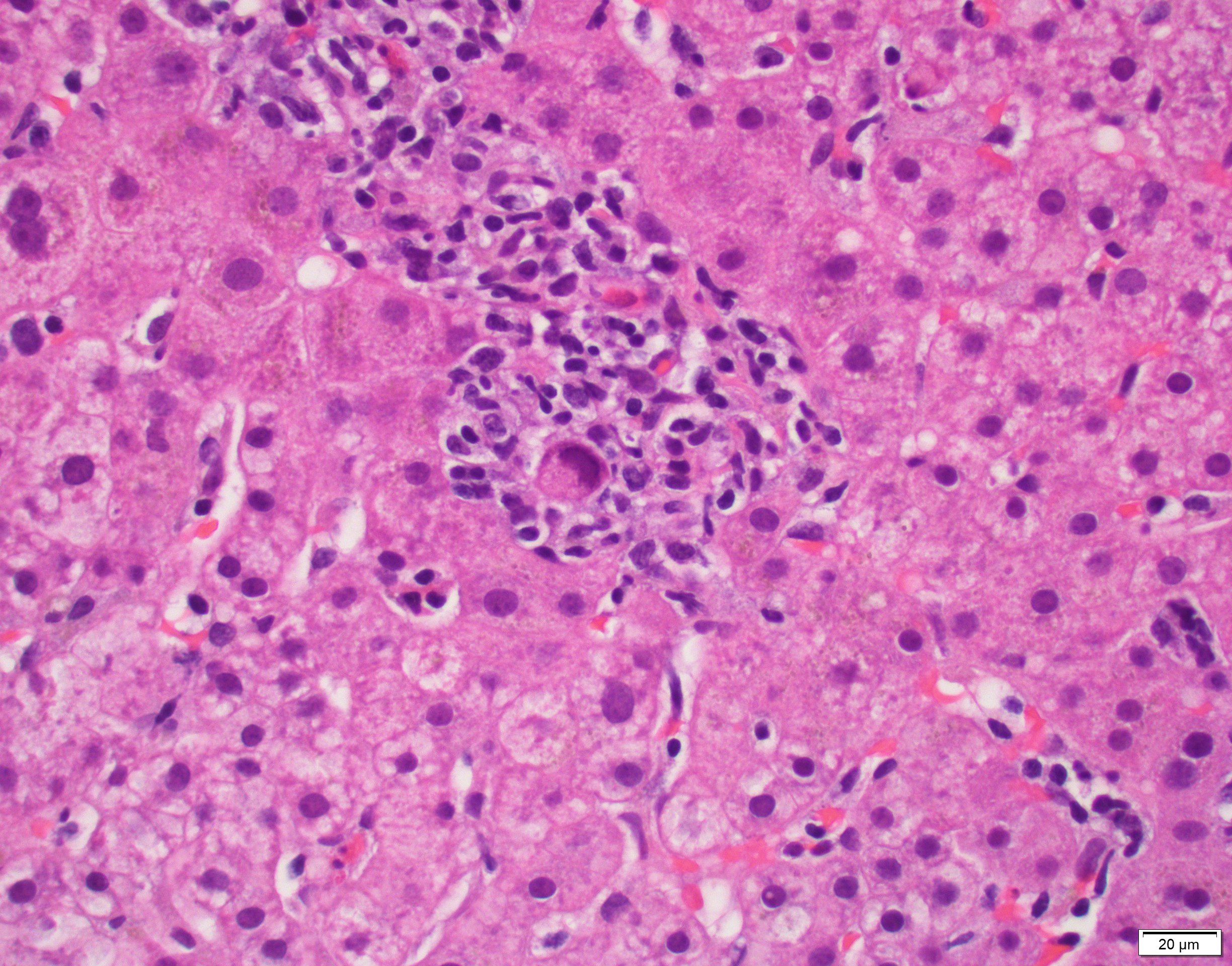
- Classic cytomegalovirus specific cytopathic effects are seen in hepatocytes, biliary epithelium, Kupffer cells and endothelial cells (Gastroenterol Clin North Am 2020;49:331)
- Infected cells have both cytoplasmic and nuclear enlargement, with cytoplasmic and nuclear inclusions, respectively (characteristic feature)
- Cytoplasmic inclusions are multiple, smaller, light staining, intracytoplasmic and basophilic / amphophilic granules of various size
- Nuclear inclusion is distinct, single, large, dense, intranuclear and has owl eye morphology: large glassy round to oval masses within the nucleus separated by a clear halo from the thickened nuclear membrane
- Mononucleosis-like pattern is characterized by a prominent mononuclear infiltrate within portal tracts and sinusoids; granulomas may also be present but viral inclusions are usually absent
- Immunocompromised patients have an overall low degree of inflammatory mononuclear infiltrate (J Clin Transl Hepatol 2021;9:106)
- Other nonspecific changes include mild lobular hepatitis, hepatocellular necrosis, patchy portal mononuclear infiltrate and microabscesses
- Immunohistochemistry is used when cytomegalovirus inclusion is not seen in H&E stain
- Cytomegalovirus antibody (DDG9 and CCH2) immunostain is utilized
Microscopic (histologic) images
Virtual slides
Immunofluorescence description
- A pp65 CMV antigenemia assay detects CMV antigens in peripheral blood polymorphonuclear cells
- Indirect immunofluorescence staining using monoclonal antibody
- In solid organ transplantation, a small number of antigen positive cells (10 per 50,000 polymorphonuclear cells) generally indicates asymptomatic infection, whereas a large number (> 50 antigen positive cells per 50,000 polymorphonuclear cells) indicates a 60% likelihood of CMV disease (Clin Infect Dis 1996;22:537)
Positive stains
- CMV immunohistochemistry (nuclear and cytoplasmic staining)
Negative stains
Molecular / cytogenetics description
- Qualitative PCR is used to detect cytomegalovirus in a tissue sample
Videos
Histopathology liver - congenital cytomegalovirus disease
Sample pathology report
- Liver, biopsy:
- Consistent with cytomegalovirus (CMV) hepatitis (positive CMV immunostain) (see comment)
- Comment: The patient's history of liver transplantation and being under the treatment of immunosuppressive drugs, along with positive CMV PCR for cytomegalovirus is noted. CMV immunostain highlights intranuclear and intracytoplasmic inclusions within portal tracts.
Differential diagnosis
- EBV associated hepatitis:
- Mimics mononuclear pattern of CMV hepatitis
- Distinguished by positive EBV in situ hybridization and positive heterophil antibodies
- Herpes simplex virus hepatitis:
- Foci of geographic necrosis
- HSV cytopathic effect characterized by multinucleation, margination of chromatin and ground glass nuclei
- HSV immunostain positive
- Adenovirus hepatitis:
- Focal to massive coagulative necrosis
- Immunostain for adenovirus is positive
- Transplant rejection:
- Pericentral ballooning degeneration and single cell apoptosis
- No viral cytopathic effect
- Mixed inflammatory cell infiltrate, endothelialitis and bile duct damage / injury would be expected in acute cellular rejection
Additional references
Board review style question #1
A 43 year old man with a known case of HIV and type 1 diabetes mellitus, under treatment, presented with complaints of decreased appetite and fatigue for 2 weeks. The abdomen was soft with mild hepatomegaly. Baseline liver profile showed the following: total bilirubin 72 (2 - 21) mg/dL, alanine transaminase (ALT) 54 (0 - 42) U/L, alkaline phosphatase 619 (40 - 129) U/L, gamma glutamyl transferase (GGT) 952 (8 - 61) U/L, lactate dehydrogenase (LDH) 247 (135 - 225) U/L, albumin 26 (35 - 52) g/L and direct bilirubin 95 (0 - 5) µmol/L. The histopathology of ultrasound guided liver biopsy is depicted in the image shown above. What characteristic finding is highlighted in the figure?
- Cytoplasmic and nuclear inclusions
- Diffuse lymphocytic sinusoidal infiltrate
- Foci of geographic necrosis
- Pericentral ballooning degeneration
Board review style answer #1
A. Cytoplasmic and nuclear inclusions. The image shows inclusion bodies visible in the nucleus and the cytoplasm, consistent with cytomegalovirus. Answers B - D are incorrect because the image does not show diffuse lymphocytic sinusoidal infiltrate, foci of geographic necrosis or pericentral ballooning degeneration.
Comment Here
Reference: Cytomegalovirus hepatitis
Comment Here
Reference: Cytomegalovirus hepatitis
Board review style question #2
Board review style answer #2
A. Cytomegalovirus hepatitis. The histology findings described above and the immunocompromised condition of the patient signify cytomegalovirus hepatitis. Answers B - D are incorrect because such inclusions are not observed in drug induced hepatitis, EBV hepatitis or hepatitis A.
Comment Here
Reference: Cytomegalovirus hepatitis
Comment Here
Reference: Cytomegalovirus hepatitis