Table of Contents
Definition / general | Diagrams / tables | Diagnosis | Prognostic factors | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Peripheral smear images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Differential diagnosisCite this page: Mihova D. T lymphoblastic lymphoma / leukemia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/leukemiaTall.Html. Accessed March 31st, 2025.
Definition / general
- Neoplasm of T lineage lymphoblasts which may form lymphomatous masses, involve blood and bone marrow (Stanford School of Medicine: Precursor T Lymphoblastic Leukemia / Lymphoma [Accessed 13 April 2018])
- Also called pre T cell acute lymphocytic leukemia / lymphoma (pre-T ALL), T lymphoblastic leukemia / lymphoma (T LBL)
- Teens and young men (older than B ALL)
- Most cases begin after birth (Blood 2007;110:3036)
- T ALL versus T LBL: T ALL has more immature phenotype, CD47 expression, no 11q23 rearrangement, different gene expression profile and may derive from T cell progenitor of bone marrow; T LBL is derived from thymocytes (Pediatr Blood Cancer 2006;47:130, Leuk Lymphoma 2007;48:1745)
- T ALL constitutes 15% of childhood and 20 - 25% of adult ALL cases
- T LBL constitutes 85 - 95% of LBL, usually presents as mediastinal mass with no / minimal marrow involvement
- CNS involvement if untreated
- T LBL frequently presents with mass in anterior mediastinum, rapid growth, respiratory emergency, pleural effusion
- Younger (age 16 - 60 years) patients compared to older (61+ years) patients have more hepatosplenomegaly, present with mediastinal mass and lymphadenopathy; myeloid antigens and lineage inappropriate gene rearrangements are less common (Am J Clin Pathol 2002;117:252)
Diagnosis
- T ALL if lymphoblasts are 25% or more of marrow cells; T LBL otherwise
Prognostic factors
- Good prognostic factors: HOX11 overexpression in adults (Am J Clin Pathol 2007;127:528)
- Poor prognostic factors: expression of CFLAR, NOTCH2 and BTG3 genes, 3+ methylated genes, residual disease after treatment (even if minimal) (Br J Haematol 2007;137:319, J Clin Oncol 2005;23:7043)
- Pediatric patients with T ALL: TLX1 (HOX11)+ was associated with favorable outcome and TAL1+ and LYL1+ were associated with unfavorable outcome (Atlas of Genetics and Cytogenetics: T Lineage Acute Lymphoblastic Leukemia (T-ALL) [Accessed 13 April 2018])
- Higher risk than B ALL due to presence of high risk features but T ALL without high risk clinical features has survival comparable to B ALL
Treatment
- Chemotherapy cures 60%
- Patients have earlier relapse, induction failure and isolated CNS relapse compared to pre-B ALL
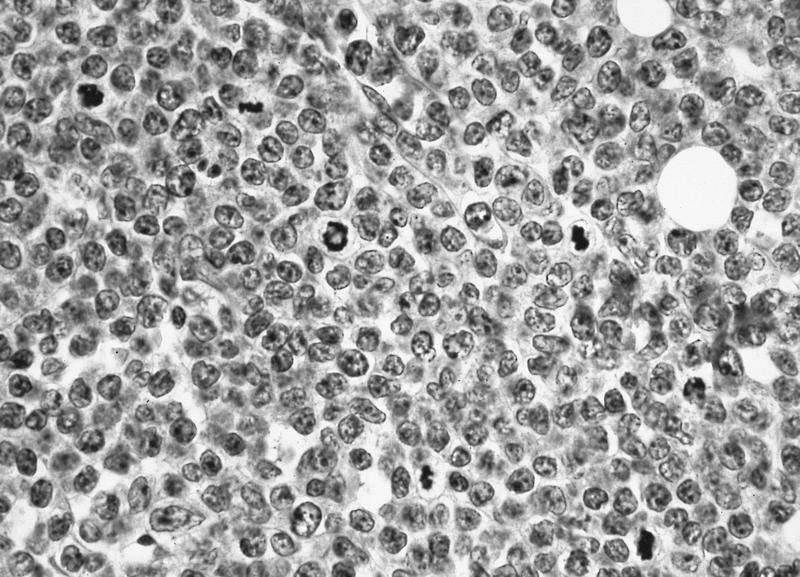
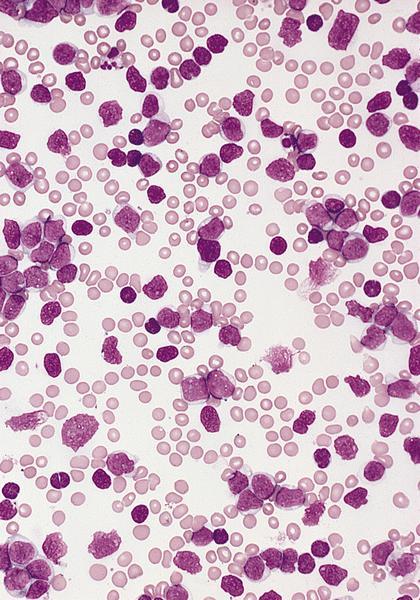
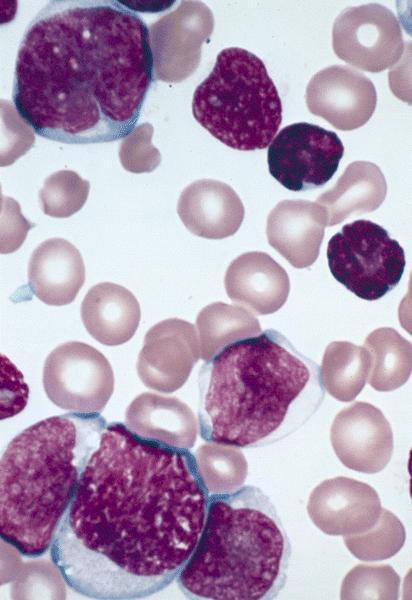
Microscopic (histologic) description
- Similar to B cell disease; scant cytoplasm, delicate chromatin, indistinct nucleoli, convoluted nuclear membrane and grooves
- Frequent mitotic figures; starry sky pattern produced by interspersed benign macrophages
- Usually features of FAB L1 or L2; pattern in marrow is usually interstitial
- Lymph nodes: complete architectural effacement or partial involvement with paracortical infiltrate with germinal center sparing
- Thymus: replacement of normal parenchyma
- Occasionally eosinophilia and myeloid hyperplasia with variable t(8;13)(p11.2;q11-22) involving FGFR1 gene; some develop myeloid malignancy (MDS, AML or myeloid sarcoma)
Microscopic (histologic) images
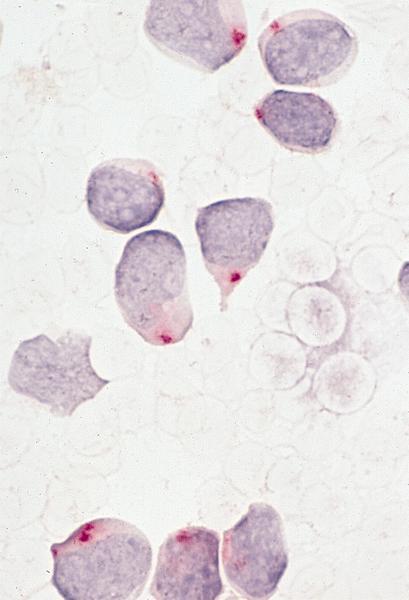
Positive stains
- CD1a, CD2 (78%), CD3 (cytoplasmic, not surface in 100%), CD5 (100%), CD7 (100%), TdT (73%)
- CD4 and CD8 both positive in 22%
- Variable CD10 (47%), CD13 (6%), CD16, CD33 (12%), CD56, CD57, CD79a+ (40 - 60%), CD117 (12%) (Haematologica 2009;94:160, Am J Clin Pathol 2000;113:823, Exp Mol Pathol 2006;81:162)
- CD117 associated with activating mutations of FLT3, CD4 (10%) and CD8 (< 10%)
Negative stains
Molecular / cytogenetics description
- Different cytogenetic abnormalities than B ALL, often are cryptic and identified only by FISH or PCR (Atlas of Genetics and Cytogenetics: T Lineage Acute Lymphoblastic Leukemia (T-ALL) [Accessed 13 April 2018])
- t(1;14)(p32;q11) involving SCL (TAL1) and T cell receptor delta / alpha in 15 - 30%
- t(10;14)(q24;q11) involving HOX11 (TLX1) and T cell receptor delta / alpha in 7%
- Activating mutations of NOTCH1 in 50% (Science 2004;306:269)
- CDKN2A (INK4A) deletions in up to 80% (Blood 1995;85:2321)
- TCR: may have rearrangement but is not lineage specific
- TCR loci (1/3 of T ALL)
- 14q11.2 (alpha, delta)
- 7q35 (beta)
- 7p(14-15) (gamma)
Genes:
- MYC (8q24.1)
- TAL1 (1p32)
- RBTN1 (LMO1) (11p15)
- RBTN2 (LMO2) (11p13)
- HOX11 (TLX1) (10q24)
- HOX11L2 (TLX3) (5q35)
- LYL1 (19p13)
- LCK (1p34.3-35)
Differential diagnosis
- Burkitt leukemia:
- B cell phenotype
- Granulocytic sarcoma:
- Positive for myeloid markers
- Mantle cell lymphoma-blastoid:
- B cell phenotype
- Thymoma (Am J Clin Pathol 2004;121:268)