Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Tretiakova M. Multilocular cystic renal neoplasm of low malignant potential. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumormcrnlow.html. Accessed April 2nd, 2025.
Definition / general
- Indolent neoplasm composed of low grade clear cells with pure multicystic architecture
Essential features
- Exclusively cystic, multiloculated renal tumor devoid of any expansile solid growth
- Clear cells lining with low grade nuclei (WHO / ISUP grade 1 or 2)
- No progression or metastases when diagnosed on strict criteria
- Distinguish from regressing clear cell renal cell carcinoma (CCRCC) with cystic degeneration or extensive cystic architecture
- Diagnosis should not be made in needle biopsy alone because of limited sampling
Terminology
- Use of multilocular cystic renal cell carcinoma is considered obsolete (WHO 2016); some literature references in this topic use the older terminology
ICD coding
- ICD-O: 8316/1 - multilocular cystic renal neoplasm of low malignant potential
- ICD-11: 2F35 & XH7PR9 - benign neoplasm of urinary organs & multilocular cystic renal neoplasm of low malignant potential
Epidemiology
- Accounts for 0.5 - 2.5% of all renal tumors; 10% of all cystic renal neoplasms (BMC Urol 2014;14:87, Clin Genitourin Cancer 2016;14:e553, Urology 2019;133:145, Diagn Histopathol 2020;26:320)
- Median age: 54 (range: 18 - 84 years), M > F (~2:1) (Virchows Arch 2018;473:85, J Urol 2016;196:1350, BMC Urol 2014;14:87, Am J Clin Pathol 2006;125:217)
Sites
- Kidney only, no side preference
- Solitary and unilateral > 95%
- Bilateral or multifocal 2 - 5%
- References: Virchows Arch 2018;473:85, Clin Genitourin Cancer 2016;14:e553, Am J Clin Pathol 2006;125:217, BMC Urol 2014;14:87
Pathophysiology
- Several mechanisms of pathogenesis described:
- Cyst dependent, VHL associated pathway in which cysts represent a precursor of CCRCC: abnormal microtubule formation and degeneration of primary cilia
- Tumor arising in a preexisting simple renal cyst
- Intrinsic cystic growth as unilocular fluid filled mass
- Intrinsic multilocular cystic growth in proximal convoluted tubules
- Tumor growth causing obstruction of kidney tubules and cyst formation
- Cystic regression
- Most likely represent low grade spectrum in development of CCRCC with ~40% overlapping genes detected both in multilocular cystic renal neoplasm of low malignant potential (MCNLMP) and in cystic CCRCC by next generation sequencing
- References: Diagn Histopathol 2020;26:320, Virchows Arch 2018;473:85, Annu Rev Pathol 2015;10:263, Investig Clin Urol 2019;60:148
Etiology
- VHL gene alterations or 3p loss in 25 - 77% of cases
- Concurrent CCRCC in ~5% of cases
- Could develop in von Hippel-Lindau (VHL) syndrome
- References: Histol Histopathol 2012;27:969, BMC Urol 2014;14:87, Virchows Arch 2018;473:85
Clinical features
- 90% are discovered incidentally, on radiology for other purposes
- Asymptomatic in > 80% of cases
- Up to 20% of patients present with symptoms such as hypertension, hematuria, a palpable mass, flank or abdominal pain but not the classic renal cell carcinoma (RCC) triad of gross hematuria, pain and a palpable mass
- References: J Cancer Res Clin Oncol 2008;134:433, Histol Histopathol 2012;27:969, Am J Surg Pathol 2013;37:1469, Virchows Arch 2018;473:85, Clin Genitourin Cancer 2016;14:e553
Diagnosis
- Radiographic studies: contrast enhanced CT, MRI or ultrasound
- Bosniak IIF - III cysts (World J Urol 2018;36:1643, Diagn Histopathol 2020;26:320, J Urol 2017;198:12, Medicine (Baltimore) 2020;99:e23110)
- There are no current guidelines or definitive evidence regarding the question of whether complete histologic examination is required for diagnosis (Am J Surg Pathol 2013;37:1469)
Radiology description
- Moderately complex, multilocular, cystic
- Well defined margins
- Minimal thickening of wall and smooth septa
- Moderately enhancing fluid equivalent and atypical cysts
- No intracystic enhancement (J Urol 2017;198:12)
Prognostic factors
- Excellent prognosis with no reports of progression, metastases or cancer related death in multiple case series when diagnosed on strict criteria (Virchows Arch 2018;473:85, Clin Genitourin Cancer 2016;14:e553)
- Recurrence reported in rare cases (J Cancer Res Clin Oncol 2008;134:433, Urology 2019;133:145)
Case reports
- 30 year old man with 2 year history of intermittent right flank pain and gross hematuria (Can Urol Assoc J 2014;8:E545)
- 38 year old man with concurrent MCNLMP with leiomyoma (Case Rep Oncol 2010;3:218)
- 48 year old man with MCNLMP in a duplex kidney (Int J Surg Pathol 2012;20:613)
- 55 year old man with pain in left lumbar region and hematuria since 2 months (J Lab Physicians 2014;6:50)
- 70 year old man with 5 asynchronous independent tumors, including 3 MCNLMP (APMIS 2016;124:619)
Treatment
- Resection, preferably nephron sparing surgery (Cancers (Basel) 2022;14:831)
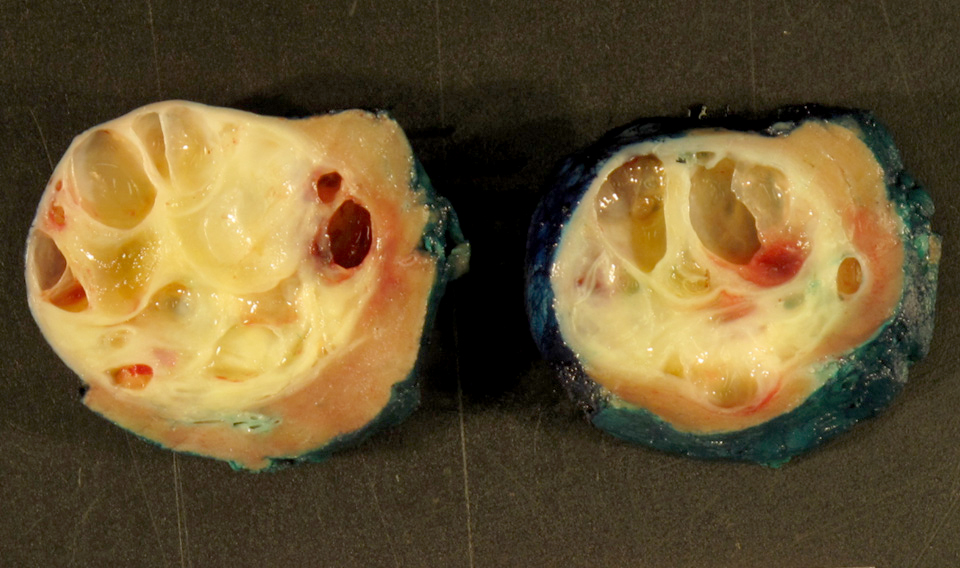
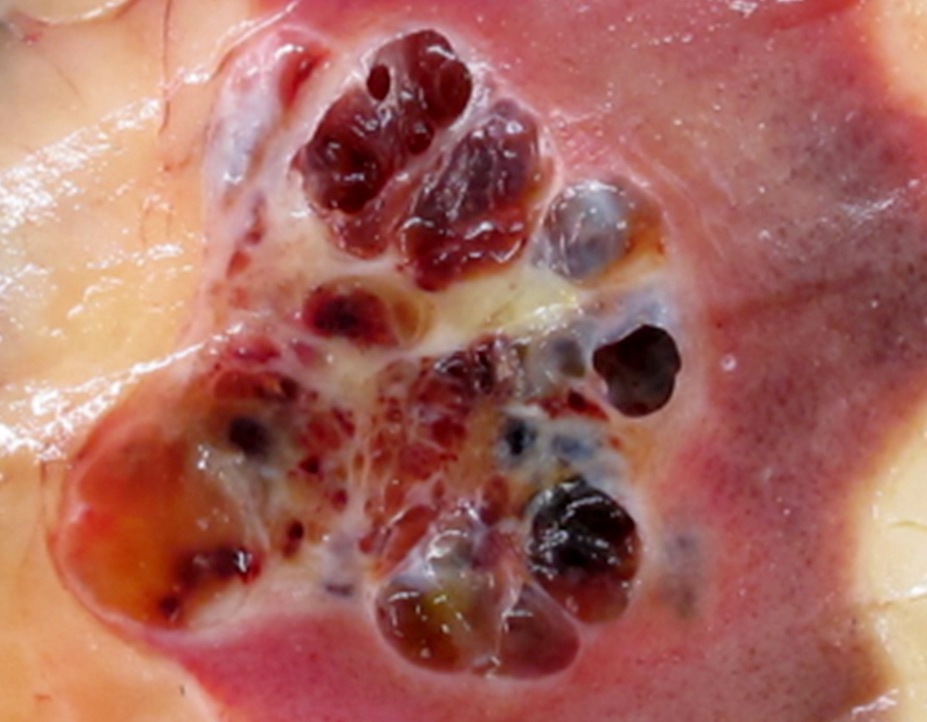
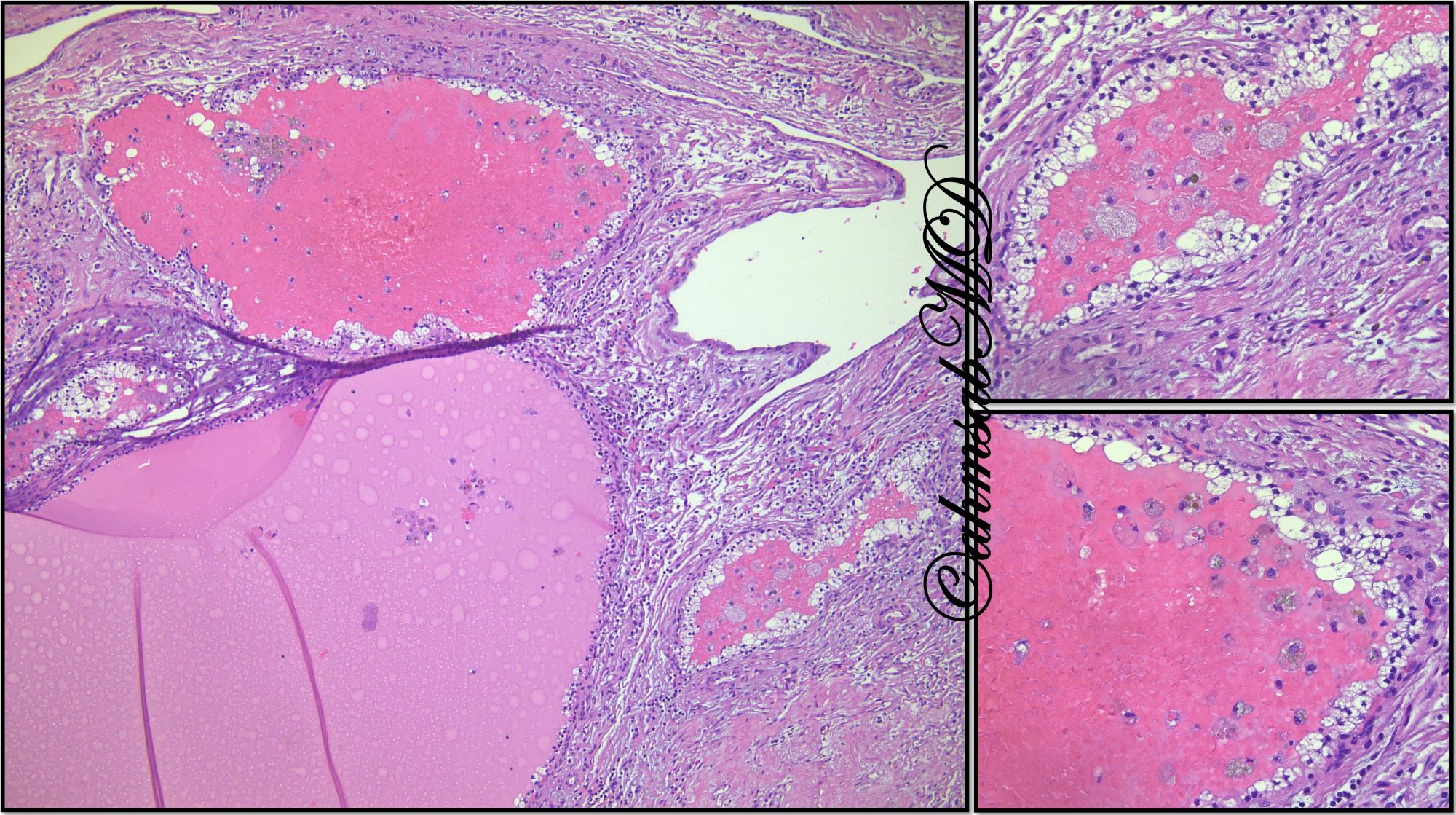
Gross description
- Usually unilateral and < 5 cm (mean size: 4 cm)
- Well circumscribed with fibrous pseudocapsule
- Variably sized cysts with thin septa
- Cysts filled with clear, serous, gelatinous or hemorrhagic fluid
- No mural solid nodules or areas of necrosis
- Reference: Histol Histopathol 2012;27:969
Gross images
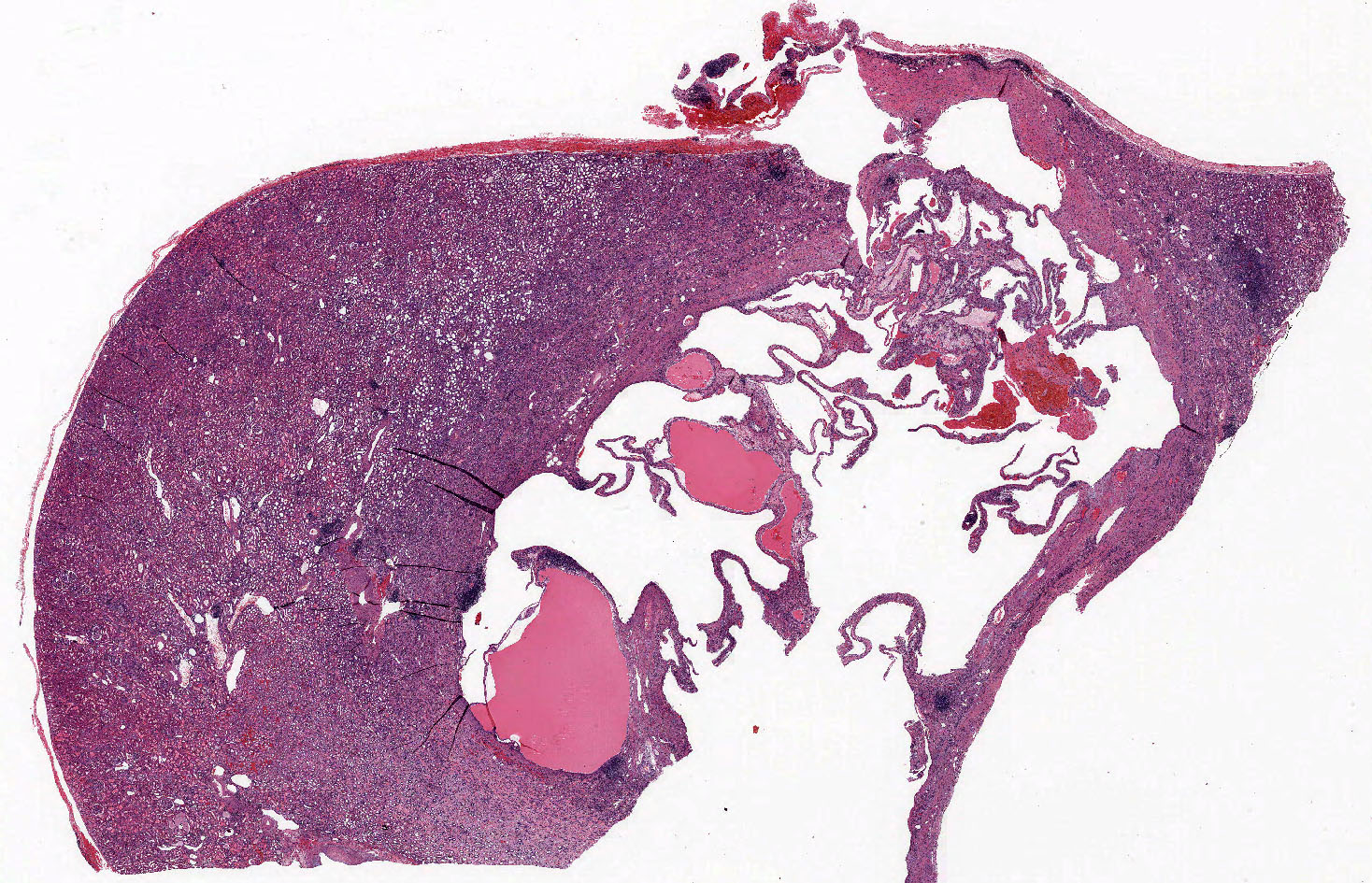
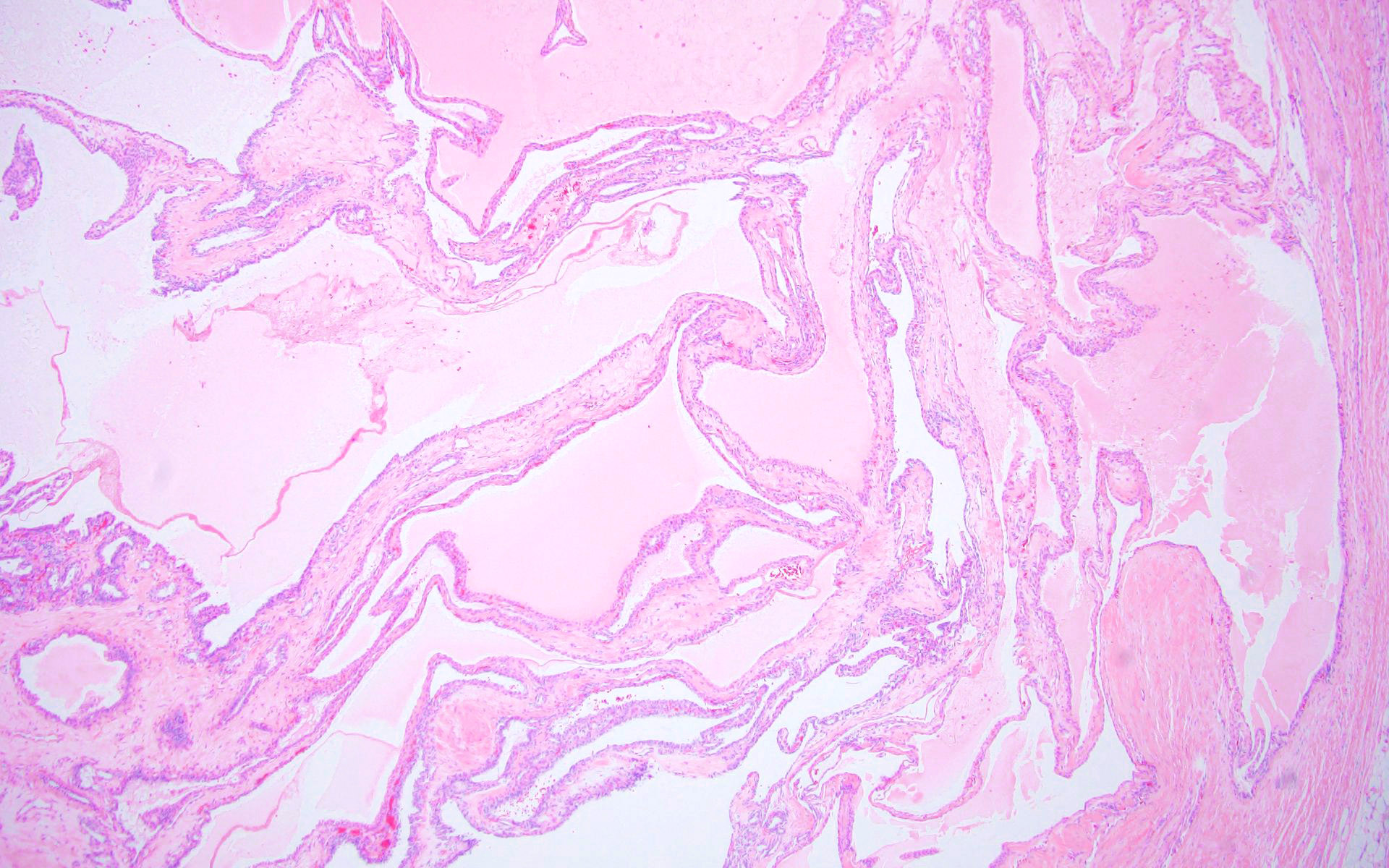
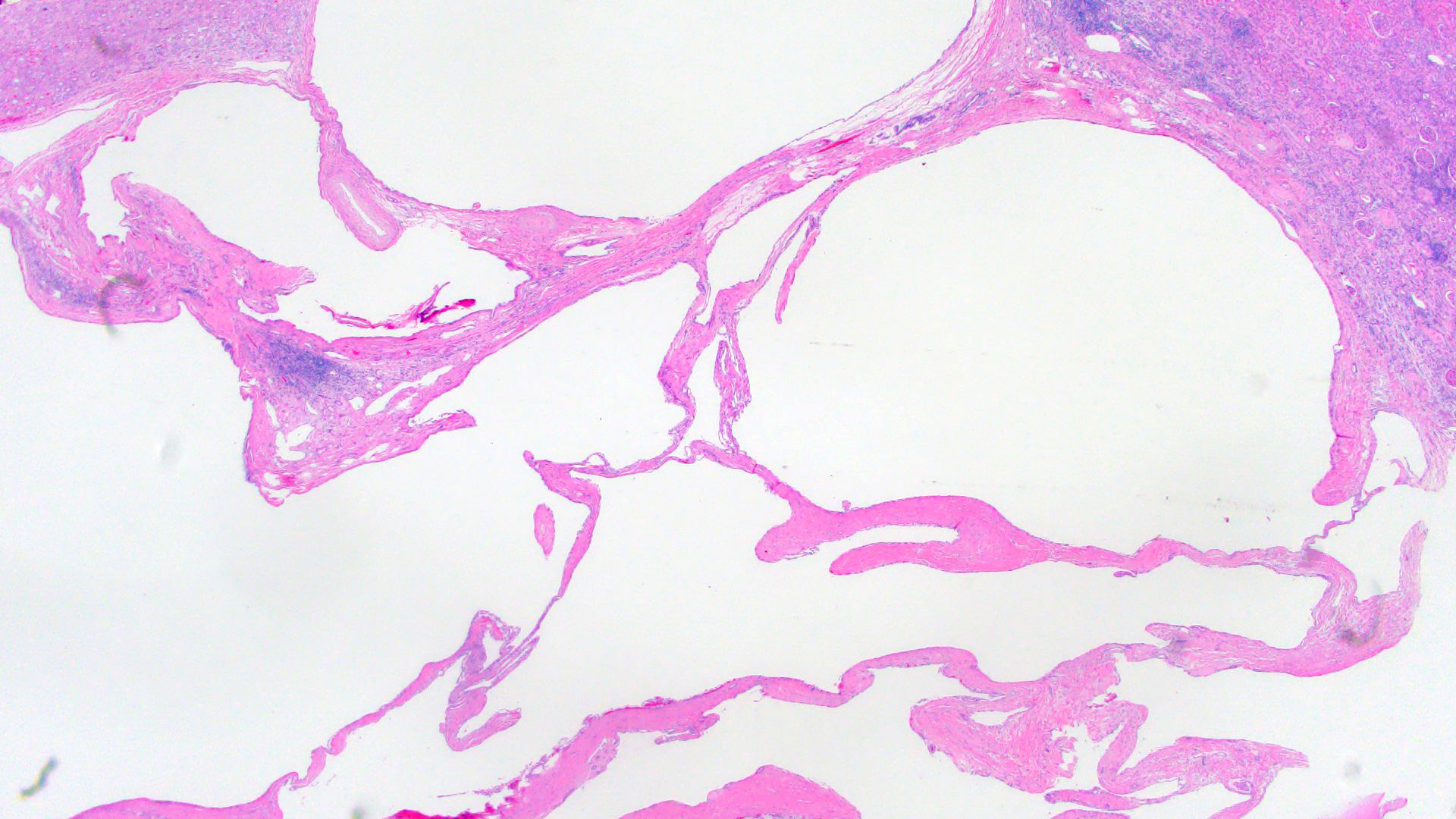
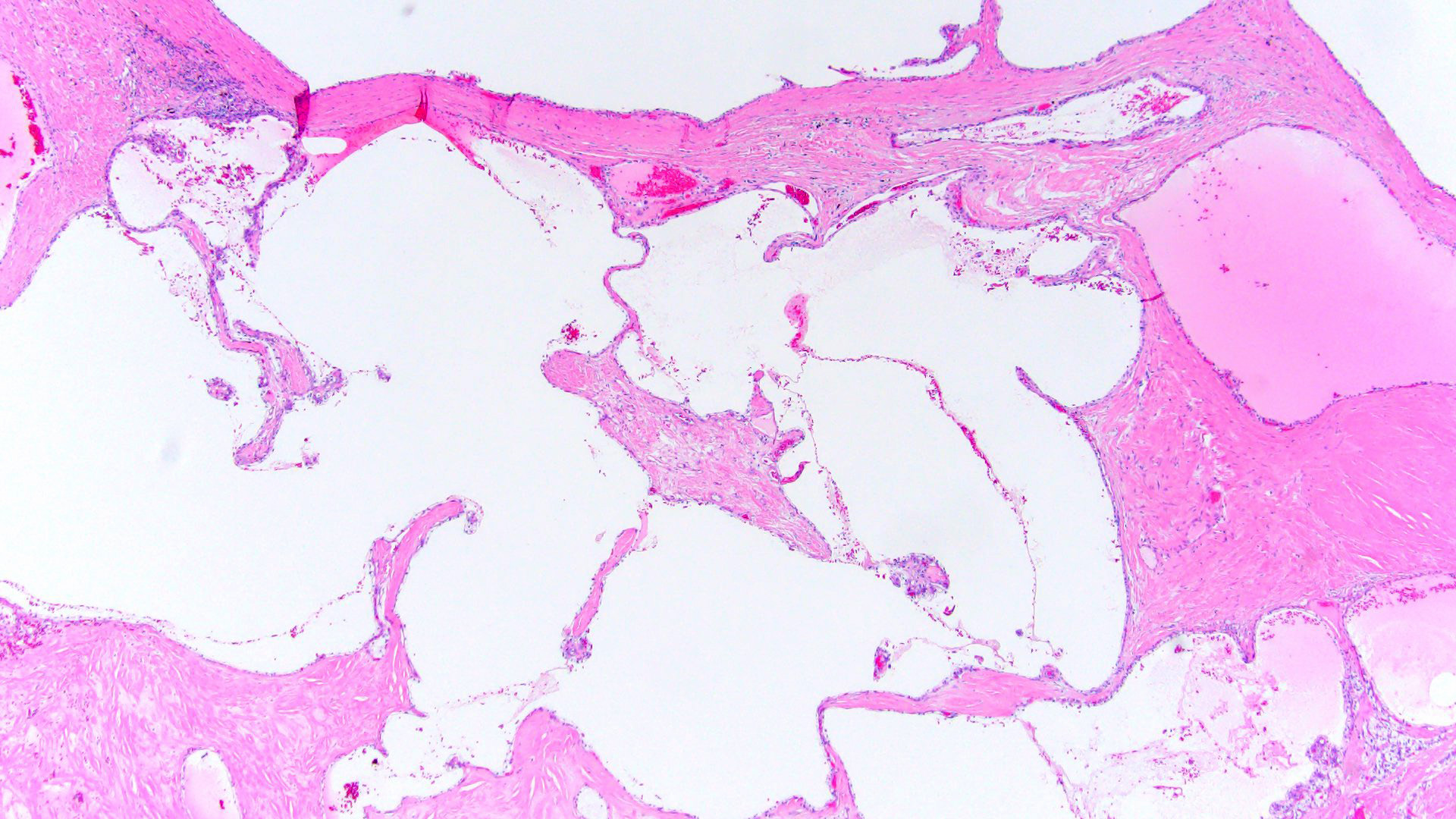
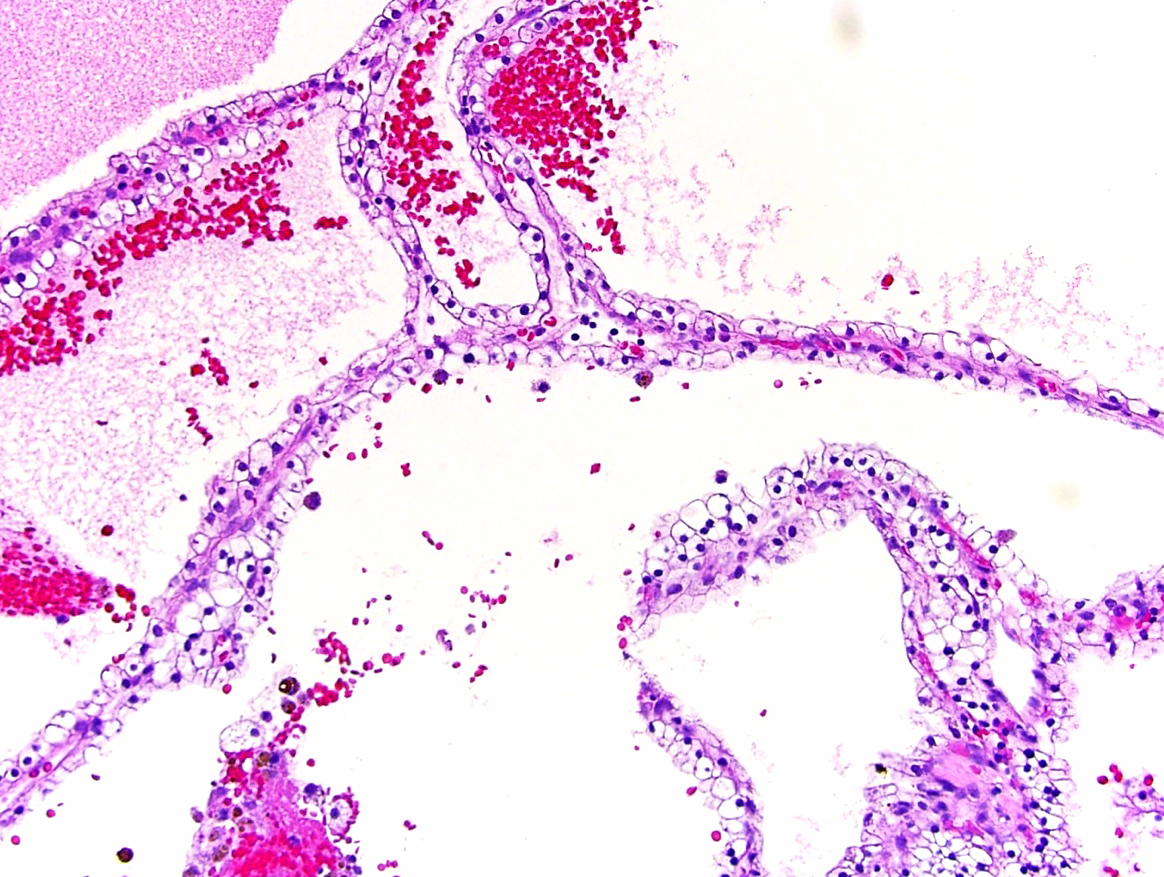
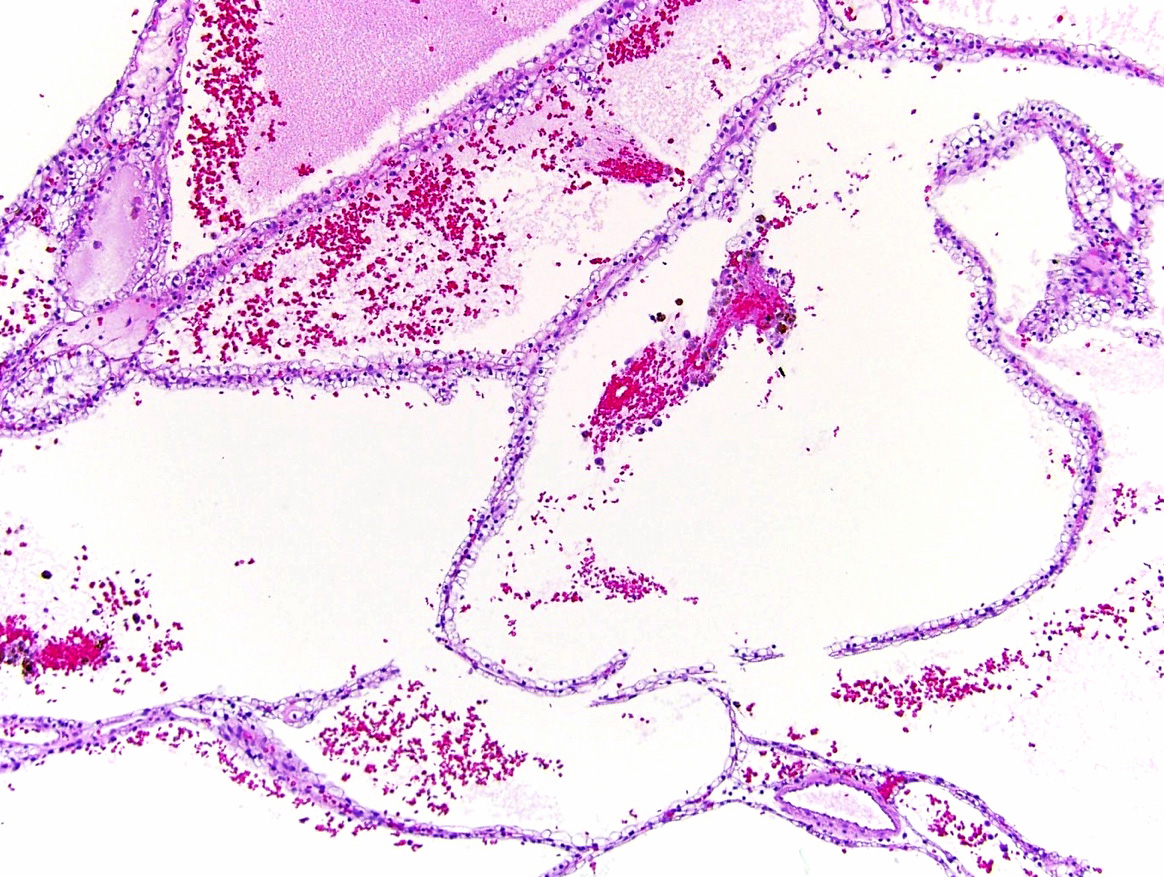
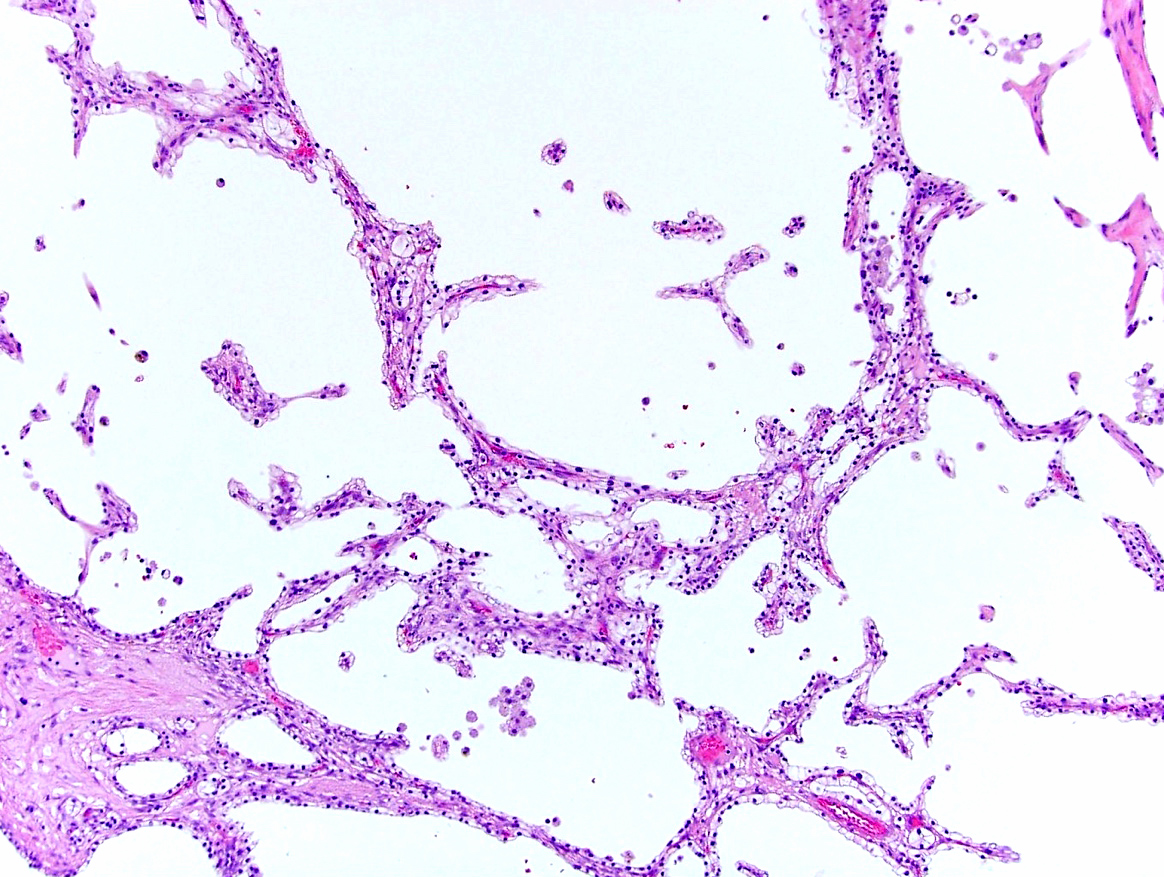
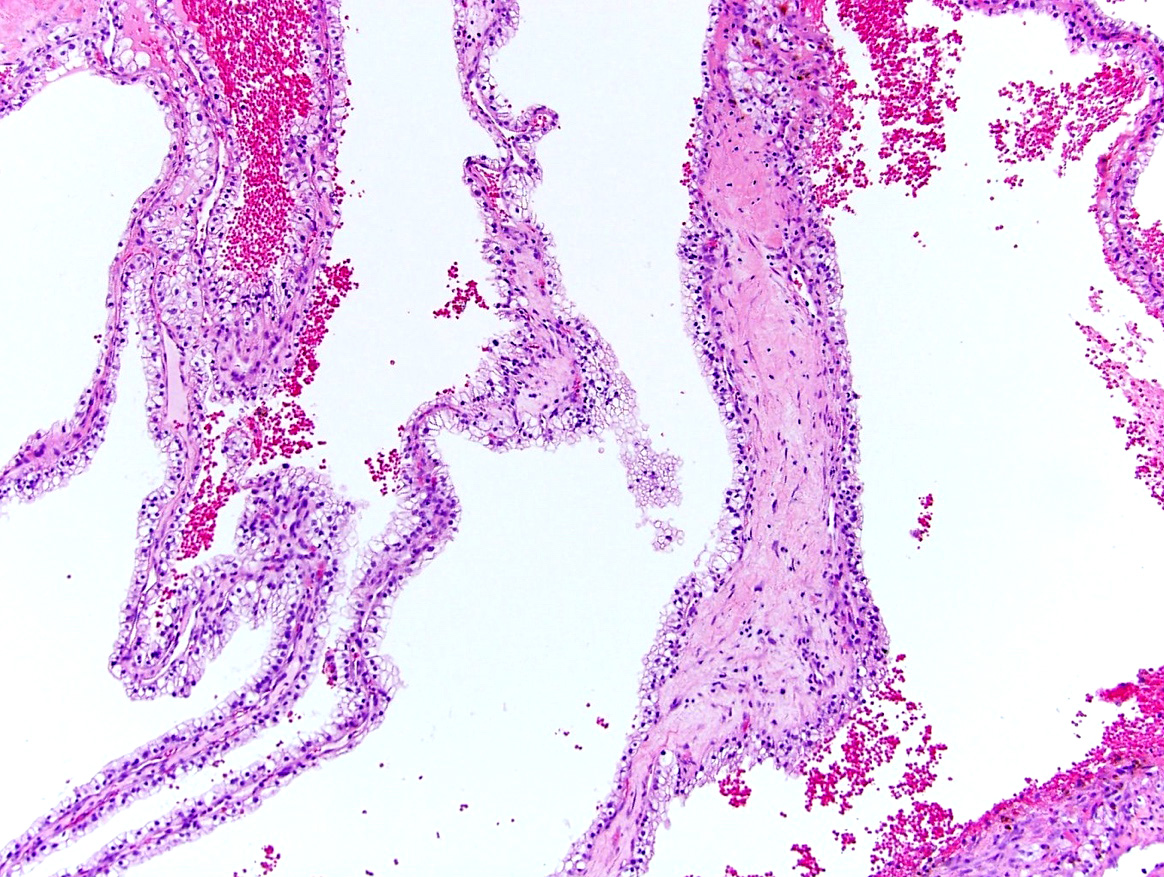
Microscopic (histologic) description
- Thin, fibrous septa lined by clear cells
- Low grade nuclei without prominent nucleoli (WHO / ISUP grade 1 - 2)
- Clear cell clusters may be present within thin septations or fibrous capsule but they should not alter their contours by expansile growth or exceed 1 mm (20x field of view)
- In rare cases, lining of cysts may show focal multilayering, cells with granular cytoplasm and small intracystic papillations
- Septa may contain calcification or ossification
- Presence of necrosis, frequent or atypical mitoses, lymphovascular or fat invasion, rhabdoid or sarcomatoid change are incompatible with diagnosis
- Reference: Virchows Arch 2018;473:85
Microscopic (histologic) images
Positive stains
Negative stains
- AMACR in 80%
- ER, PR, TFE3, GATA3
- Ki67 very low
- References: Histol Histopathol 2018;33:589, Am J Surg Pathol 2012;36:1425
Molecular / cytogenetics description
- Genetically related to CCRCC: 74 - 77% of cases demonstrate 3p loss (by FISH) and VHL mutations identified in 25 - 40% of cases
- Next generation sequencing study identified 6 candidate genes (SETD2, GIGYF2, FGFR3, BCR, KMT2C and TSC2) for differentiating MCNLMP from CCRCC with cystic change
- References: Mod Pathol 2011;24:571, Mod Pathol 2010;23:931, Virchows Arch 2018;473:85, Investig Clin Urol 2019;60:148
Sample pathology report
- Left kidney, partial nephrectomy:
- Multilocular cystic neoplasm of low malignant potential
- Tumor size: 3.7 cm
- Surgical margins: free of tumor
Differential diagnosis
- Benign renal cortical cyst:
- Usually unilocular and lacks clear cell changes
- Cyst lining is CK7 positive and CAIX negative and shows no loss of 3p (Appl Immunohistochem Mol Morphol 2019;27:549)
- Clear cell renal cell carcinoma (CCRCC) with cystic or regressive changes:
- Cysts filled with hemorrhagic or necrotic degenerated cells
- May have extensive hyalinization and has areas of expansile growth of neoplastic cells
- Clear cell papillary renal cell tumor (Hum Pathol 2017;66:152):
- Cystic nephroma (Int J Surg Pathol 2015;23:238):
- TFE3 translocation tumors (especially MED15::TFE3) (Adv Anat Pathol 2022;29:131):
- Usually high grade tumors with (at least) focal solid areas, papillary formation and psammoma bodies
- Diffusely positive for TFE3, variably positive for cathepsin K and melanocytic markers
- Negative for CAIX and CK7
- Tubulocystic renal cell carcinoma (Am J Surg Pathol 2013;37:1469):
Board review style question #1
Which of the following is true about this encapsulated multilocular cystic renal tumor with clear cell morphology?
- Does not require surgical treatment
- Frequently progresses to conventional clear cell renal cell carcinoma (CCRCC)
- Necrosis, solid growth and invasion are not allowed for this diagnosis
- Often associated with acquired cystic kidney disease
- VHL mutation or 3p loss are highly unlikely
Board review style answer #1
C. Necrosis, solid growth and invasion are not allowed for this diagnosis. Multilocular cystic renal neoplasm of low malignant potential (MCNLMP) has been excluded from the renal cell carcinoma category due to its uniformly good outcomes and has been renamed in the 2016 World Health Organization Classification. Histologically MCNLMP has pure cystic architecture and is composed of clear cells (similar to conventional CCRCC) but these cells are aligned in a single layer and do not form solid expansile nodules or tumor nests. Presence of necrosis, brisk or atypical mitoses, lymphovascular or fat invasion, sarcomatoid or rhabdoid dedifferentiation are incompatible with this diagnostic entity (C). However, despite its indolent behavior, MCNLMP is still treated surgically due to complex cystic morphology by radiologic imaging (Bosniak IIF - IV) (A). Immunostaining and molecular findings are similar to conventional CCRCC; VHL gene alteration due to mutation or 3p loss was documented in the majority of studied cases (E). Because of these similarities, there is a concept that MCNLMP, cystic CCRCC and conventional RCC represent a continuum of pathogenetic development with MCNLMP representing the most indolent end of tumor spectrum; however, no documented cases of actual MCNLMP progression to CCRCC have been reported (B). There is no known association between MCNLMP and acquired cystic kidney disease (D).
Comment Here
Reference: Multilocular cystic renal neoplasm of low malignant potential
Comment Here
Reference: Multilocular cystic renal neoplasm of low malignant potential
Board review style question #2
Board review style answer #2
A. CAIX+, CK7 variable, CD10+, RCC+. Immunostaining is rarely needed for establishing MCNLMP diagnosis, which is primarily based on morphologic assessment; however, if IHC is performed in an MCNLMP case, the expected immunoprofile will be diffuse expression of CAIX and CD10, as well as variable expression of CK7 and RCC (A). Coexpression of CAIX / CK7 plus variable expression of HMWCK and GATA3 are typically seen in clear cell papillary renal cell tumor (B). Conventional clear cell RCC could be distinguished from TFE3 rearranged RCC with panel results C and D, respectively.
Comment Here
Reference: Multilocular cystic renal neoplasm of low malignant potential
Comment Here
Reference: Multilocular cystic renal neoplasm of low malignant potential