Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Miller TI, Tretiakova M. Micropapillary. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumormalignanturothelialcarcinomasubtypesmicropap.html. Accessed March 30th, 2025.
Definition / general
- Aggressive histologic subtype of urothelial carcinoma (UC) comprised of small papillary clusters of neoplastic cells within lacunae and without fibrovascular cores (Am J Surg Pathol 1994;18:1224)
- If noninvasive, appears as slender, delicate filiform processes on surface (Am J Surg Pathol 1994;18:1224)
Essential features
- Uncommon histologic subtype of UC with micropapillary architecture lacking fibrovascular cores
- Multiple clusters of tumor cells with peripherally oriented nuclei sharing cleft-like spaces or lacunae, often resembling vascular invasion
- More likely to be diagnosed at an advanced stage compared with conventional UC, conferring a poorer prognosis
- If micropapillary urothelial carcinoma (MPUC) is seen on biopsy, it is highly associated with muscularis propria invasive disease
Terminology
- Micropapillary urothelial carcinoma (MPUC)
- Conventional urothelial carcinoma (CUC)
ICD coding
- ICD-O: 8120/3 - transitional cell carcinoma, NOS
Epidemiology
- ~2 - 5% of urothelial carcinoma (Eur Urol Focus 2020;6:653)
- M > F (74 - 97%) (Eur Urol 2019;75:649)
- Mean age of ~65 years (Pathol Res Pract 2009;205:807)
Sites
- Bladder
- Renal pelvis
- Ureter
Pathophysiology
- In situ micropapillary component may be present but not necessary (Am J Surg Pathol 1994;18:1224)
- May be more aggressive due to reverse polarity of cells; basal surface acquires apical secretory proteins that allow for stromal invasion (Arch Pathol Lab Med 2009;133:62)
Clinical features
- Most common presenting symptom: painless gross hematuria
- Other urinary symptoms: dysuria, urgency, frequency, painful micturition
- More likely to present at advanced stage with extravesical disease and lymph node metastases (Urol Oncol 2019;37:48, Urol Oncol 2014;32:110, World J Urol 2012;30:801)
- Meta analysis: at diagnosis, median rate of muscle invasive disease is 41%, lymph node involvement is 12.5% and metastasis is 5% (Eur Urol 2019;75:649)
Diagnosis
- Clinical symptoms prompt cystoscopy, which then results in a transurethral biopsy or resection of tumor
- Imaging may show mass in bladder wall or diffuse bladder wall thickening, which results in cystoscopy with biopsy
Laboratory
- Hematuria
- Case report demonstrating serum CA 15-3 correlated with disease progression (Case Rep Oncol 2021;14:1019)
Radiology description
- May not form a mass lesion on CT and can appear normal (J Urol 2000;163:748, Int J Urol 2005;12:506)
- May appear as a distorted / thickened bladder wall or a projection into bladder lumen (Int J Urol 2005;12:506)
- Computed tomography based texture analysis (CTTA) may be able to differentiate MPUC from CUC, as MPUC has greater texture heterogeneity than CUC (Abdom Radiol (NY) 2019;44:201)
Radiology images
Prognostic factors
- Some studies independently suggest a poorer prognosis than CUC (Cancer Med 2020;9:4897)
- However, other studies show that this is likely because it is diagnosed at advanced stage; when controlling for pathologic stage, patients have similar outcomes (Urol Oncol 2019;37:48, Urol Oncol 2014;32:110, World J Urol 2012;30:801)
- Activated wild type p53 expression signature is more likely to be resistant to chemotherapy and associated with poorer survival outcome (Eur Urol 2019;75:649)
- Micropapillary component comprising < 10% of tumor cells is associated with lower stage (Histopathology 2004;45:55)
- > 50% associated with increased mortality risk (Ann Diagn Pathol 2005;9:1)
Case reports
- 70 year old man presented with hematuria and found to have a bladder tumor involving the dome and extending to the perivesical fat (Can Urol Assoc J 2008;2:540)
- 70 year old woman hospitalized for dyspnea with pulmonary microangiopathy from metastases and at autopsy, found to have MPUC in the bladder (Intern Med 2021;60:2843)
- 73 year old woman presented with hematuria and found to have a mass of the left renal pelvis (Med Sci Monit 2007;13:CS47)
- 74 year old man hospitalized for hematuria found to have multifocal papillary bladder tumors with histology showing both micropapillary and plasmacytoid urothelial carcinoma (Diagn Cytopathol 2016;44:124)
- 82 year old man with end stage kidney disease on hemodialysis and found to have a sessile papillary tumor on the left bladder wall (Case Rep Oncol 2022;15:462)
Treatment
- Transurethral resection of bladder cancer (TURB) with intravesical bacillus Calmette-Guérin (BCG) may not be as effective (Eur Urol Focus 2020;6:653)
- Although, a meta analysis questions this (Eur Urol 2019;75:649)
- May be more effective if micropapillary component is < 25% (Eur Urol 2019;75:649)
- Early radial cystectomy (RC) may improve survival (J Urol 2015;193:1129)
- Many patients are immediately upstaged at RC compared with TURB stage, suggesting one reason why RC is the preferred option (Pathology 2010;42:650)
- Role of neoadjuvant chemotherapy before RC is not clear, although it is associated with pathological downstaging, it does not show increased overall survival (Eur Urol 2019;75:649)
Gross description
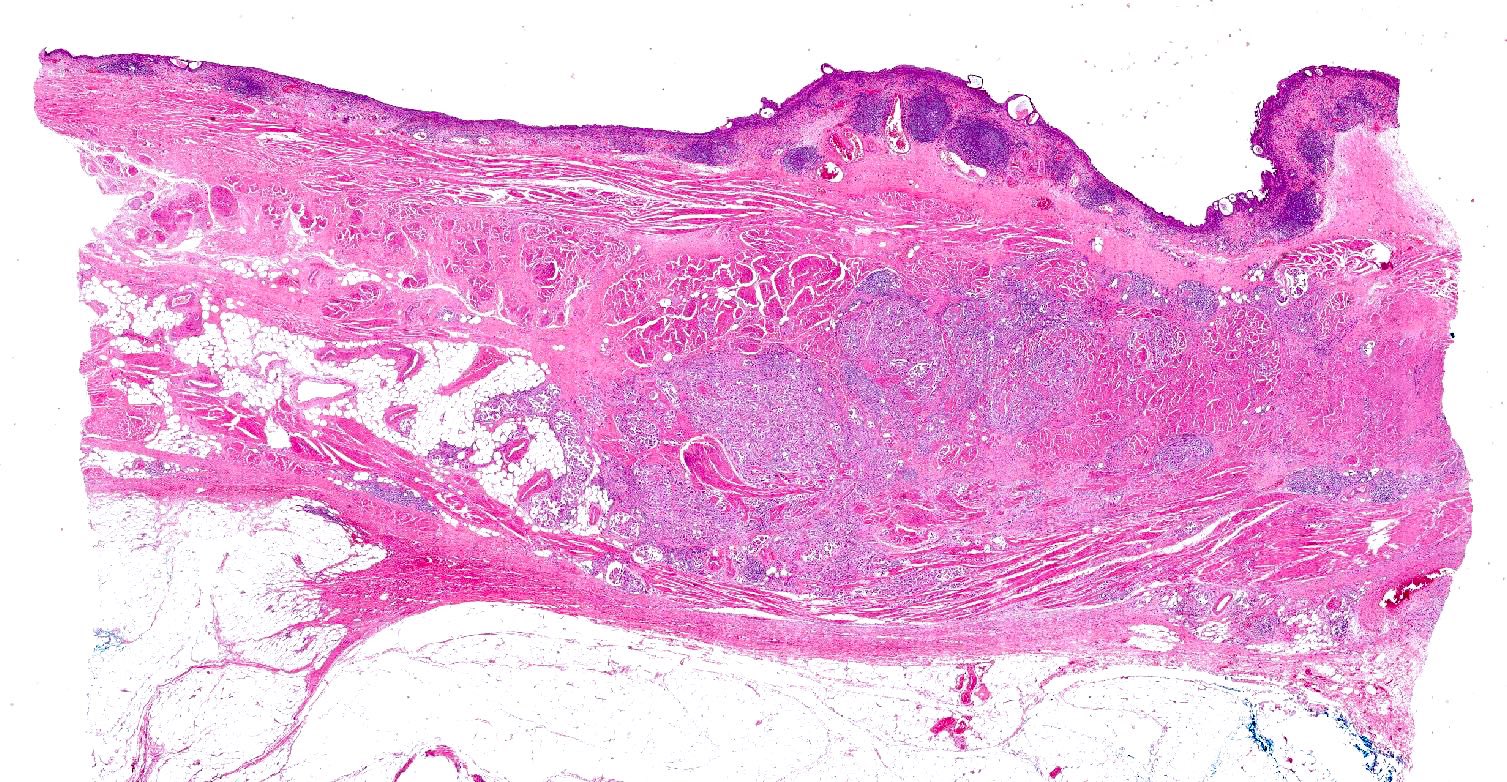
- No definite features to differentiate from CUC (Adv Anat Pathol 2010;17:182)
- Lesions may be ulcerated, polypoid, sessile or even with subtle granularity on mucosal surface (Adv Anat Pathol 2010;17:182)
Microscopic (histologic) description
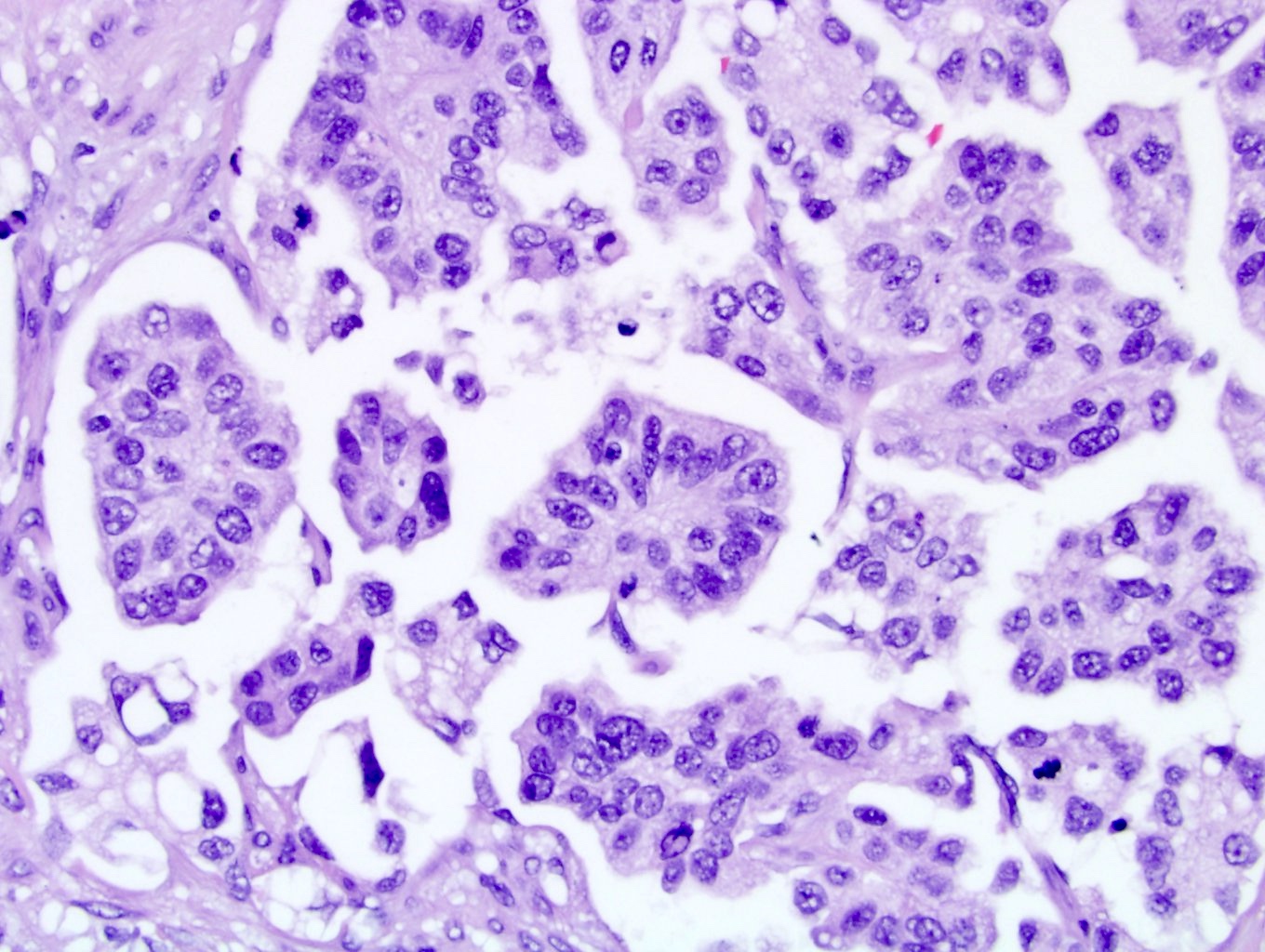
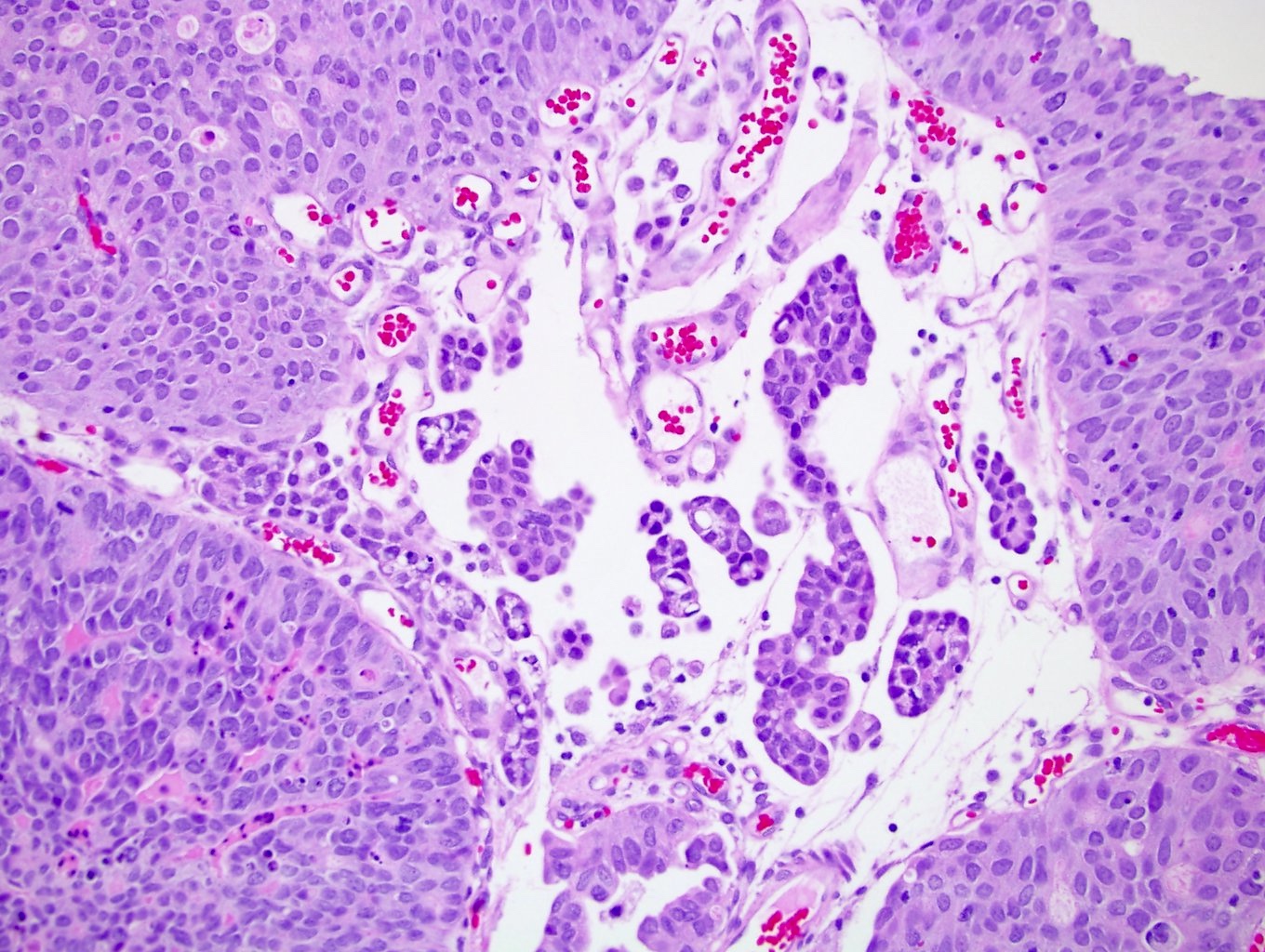
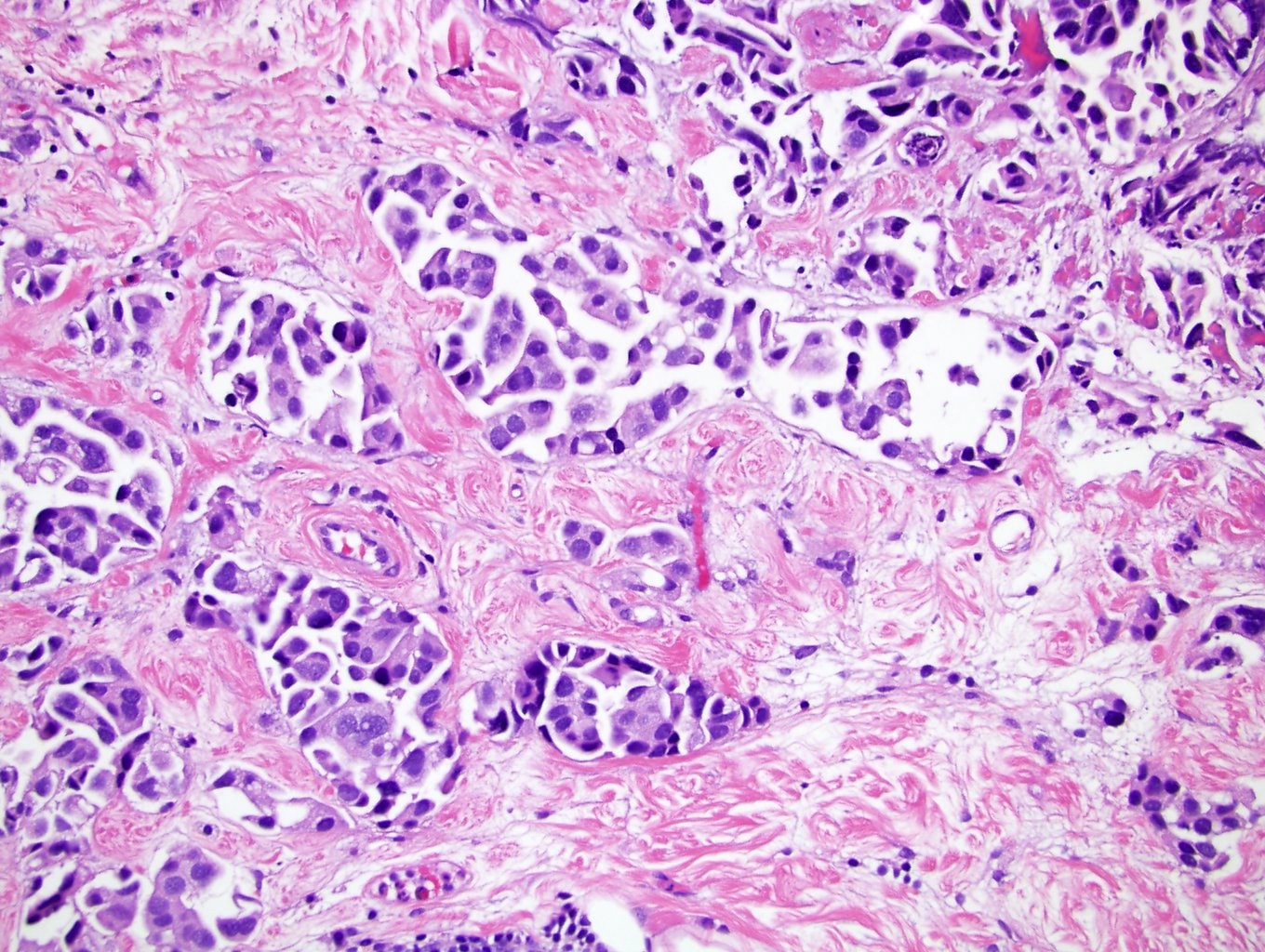
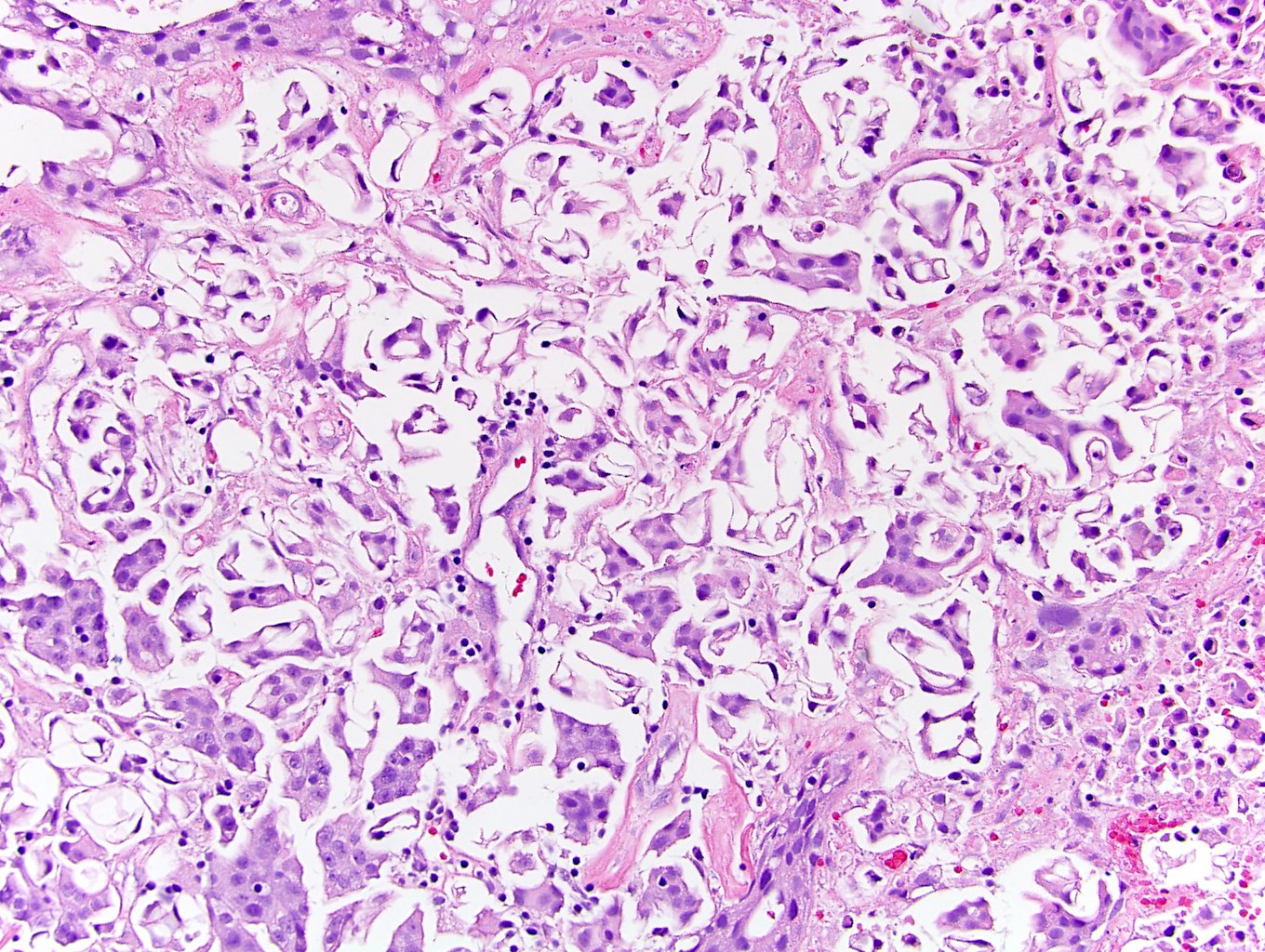
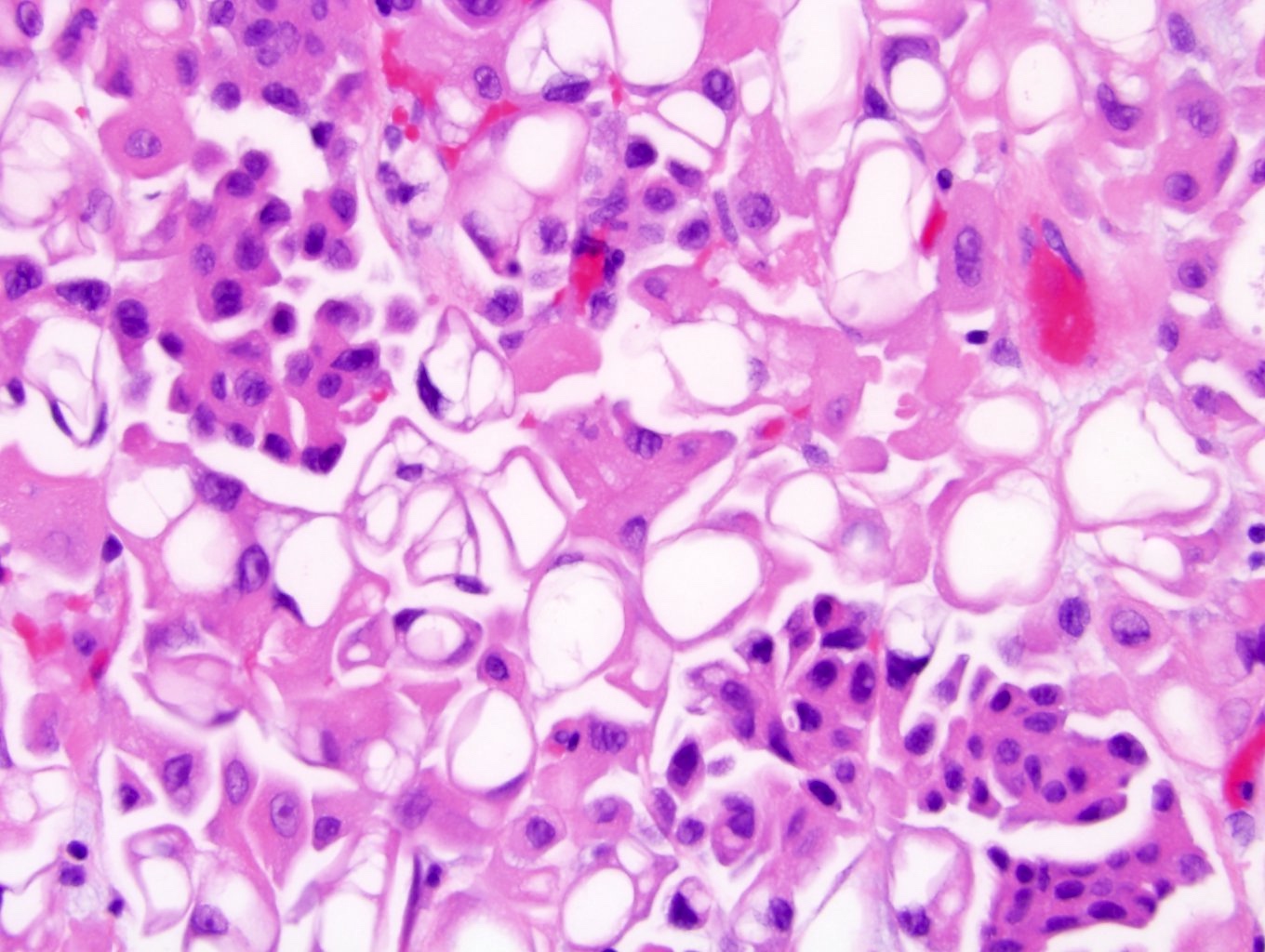
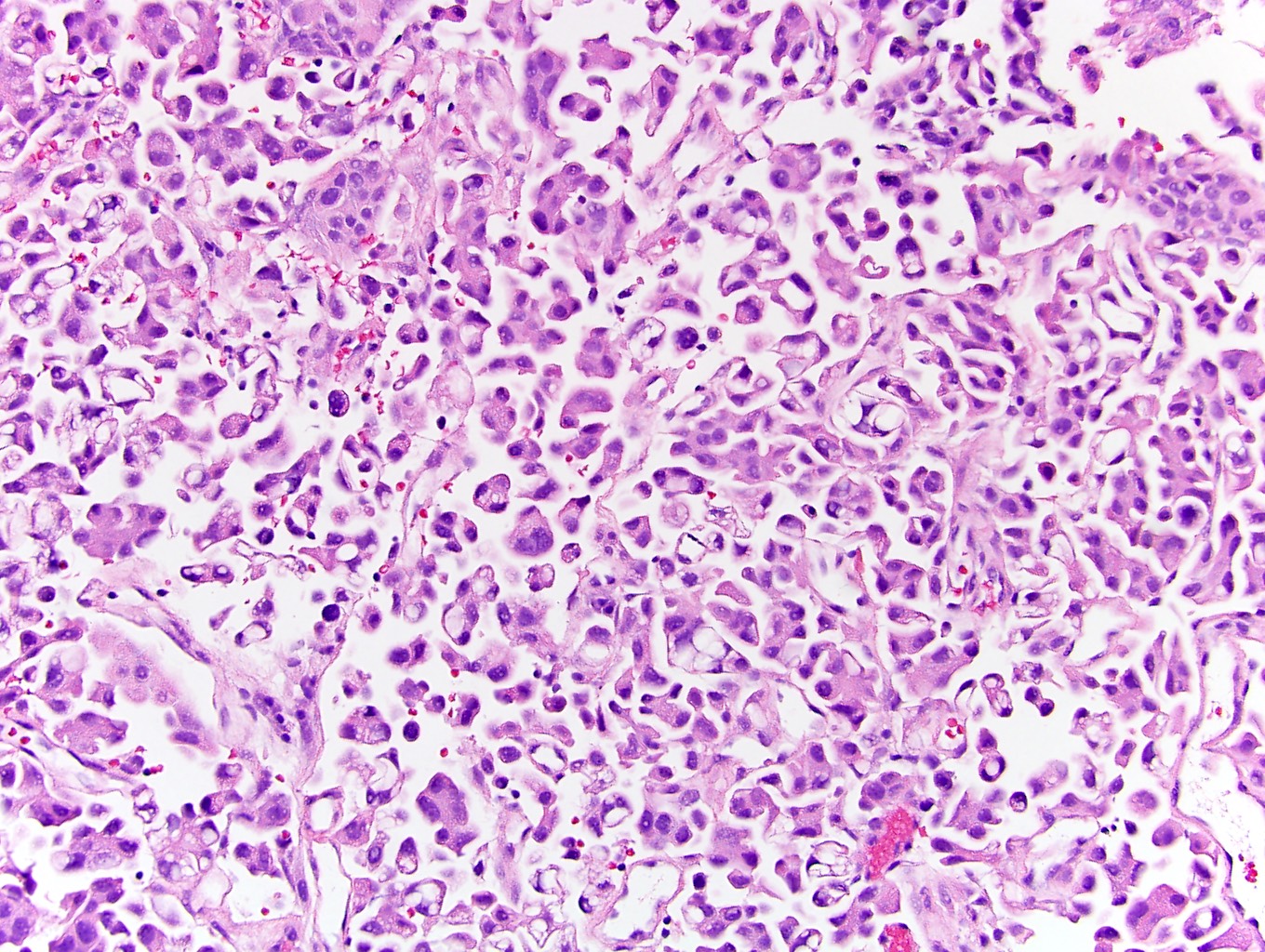
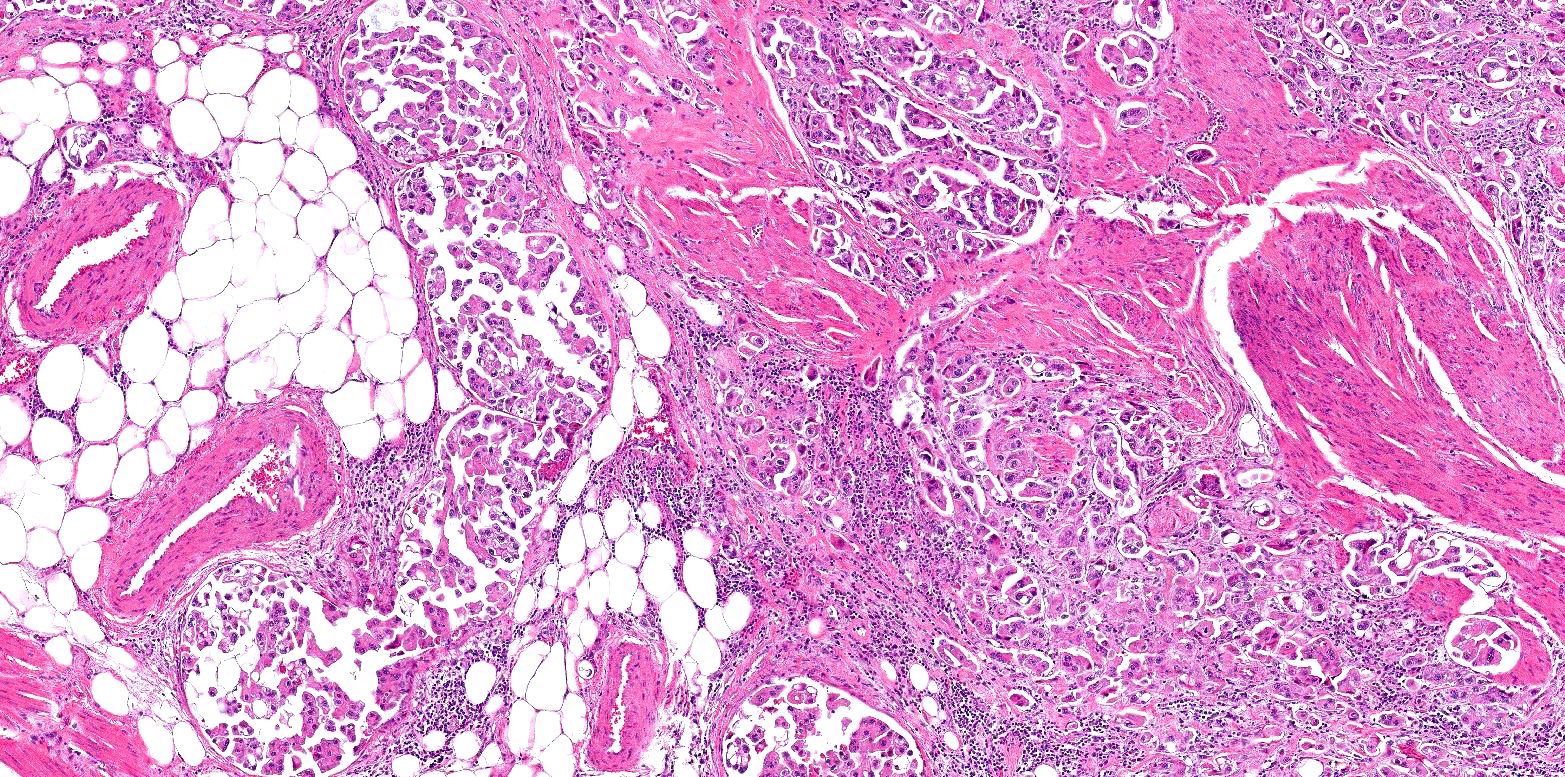
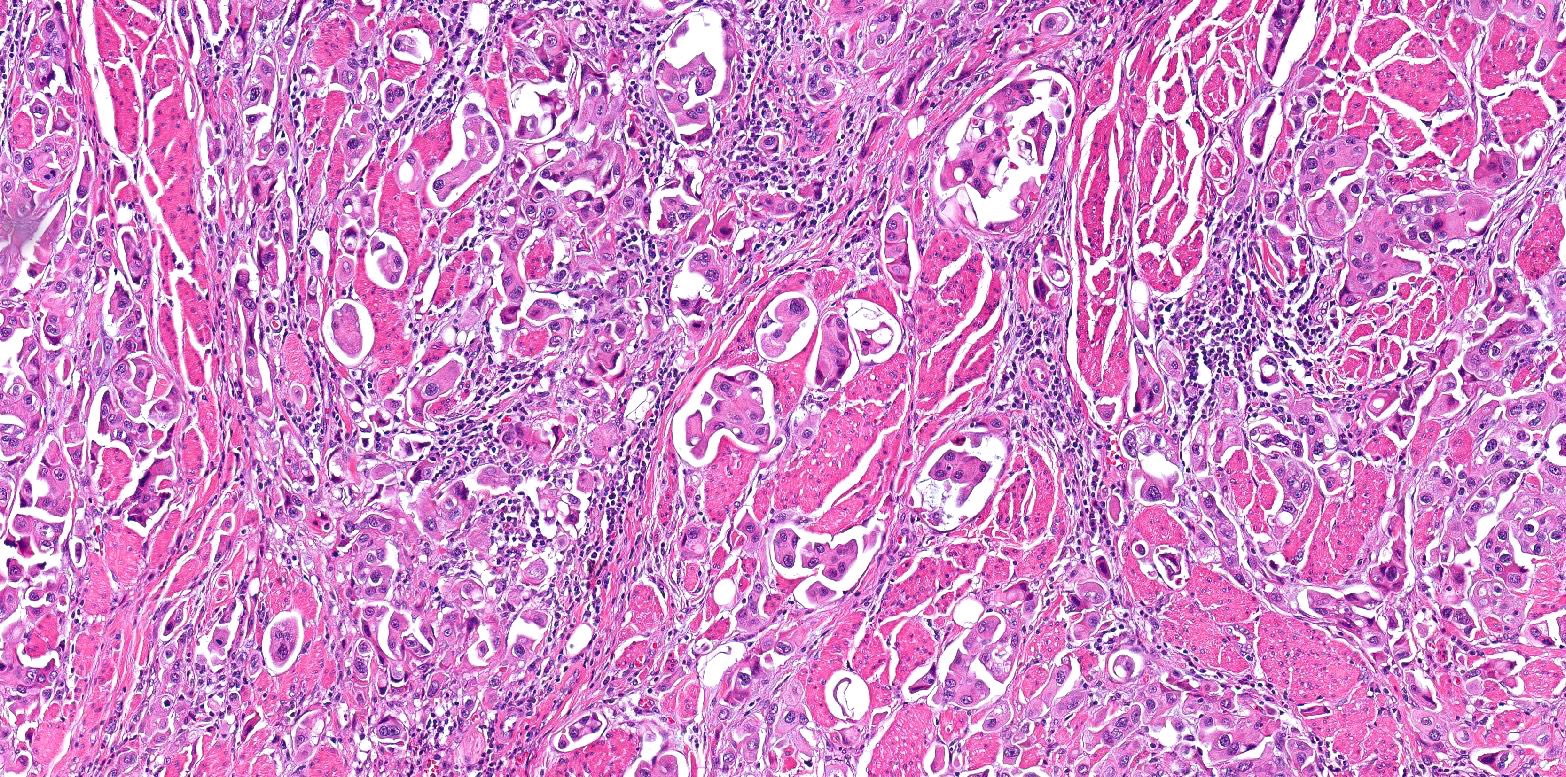
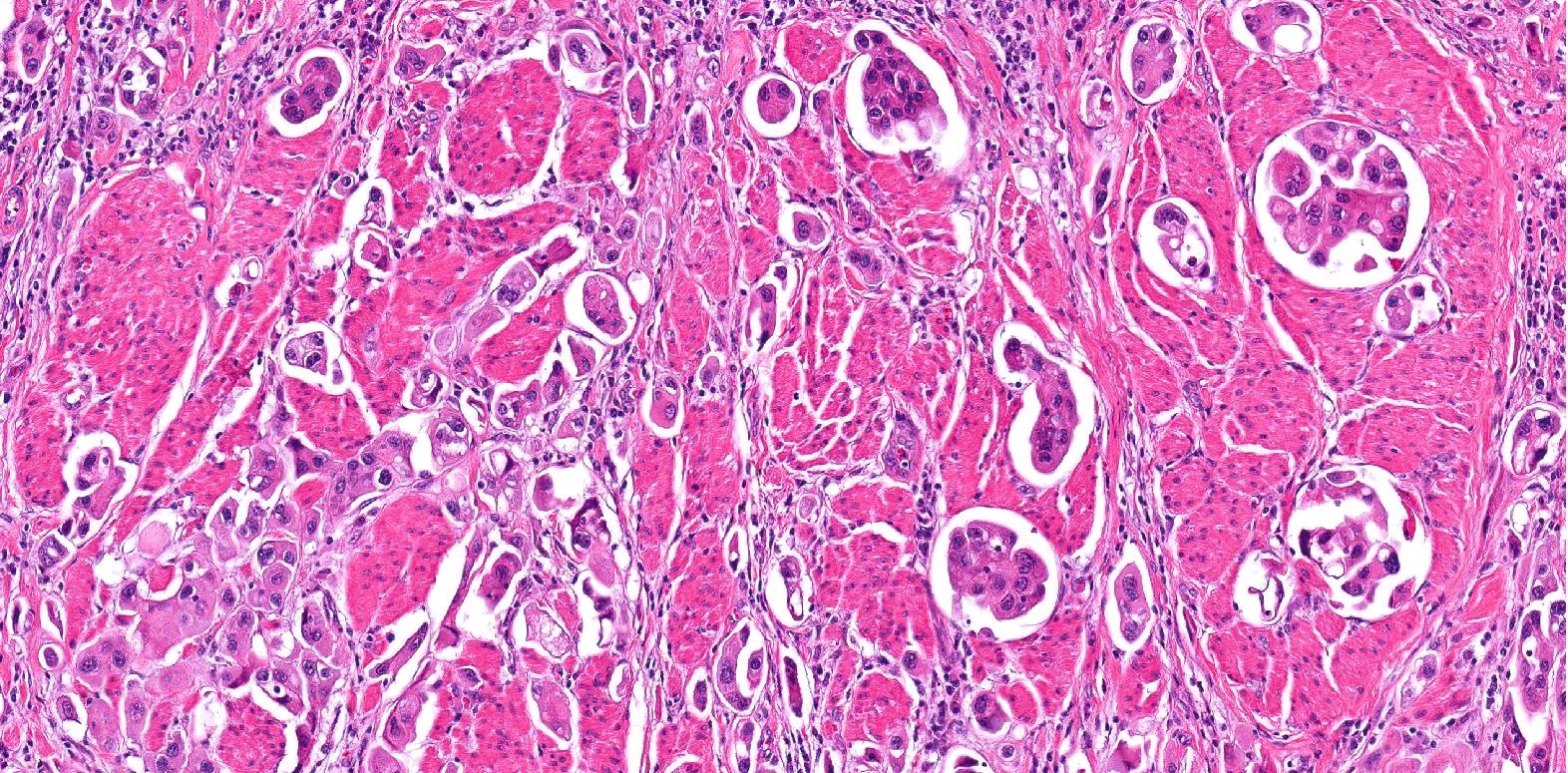
- Small nests of tumor cells with surrounding lacunar (empty) space and without fibrovascular cores (Eur Urol Focus 2020;6:653)
- Presence of multiple nests in one lacunae is a classic feature and may be the most helpful feature in making the diagnosis (Am J Surg Pathol 2010;34:1367)
- Must be careful not to confuse lacunae with lymphovascular invasion; lacunae may be lined with flattened endothelial type cells that are not lymphovascular in origin
- Epithelial ring forms and intracytoplasmic vacuolization may also be present (Eur Urol Focus 2020;6:653)
- Stromal reaction to tumor cells may be absent (Mod Pathol 2009;22:S96)
- Usually has high nuclear grade (Mod Pathol 2009;22:S96)
Microscopic (histologic) images
Contributed by Timothy Isaac Miller, M.D., M.A., Maria Tretiakova, M.D., Ph.D. and @katcollmd on Twitter
Cytology description
- Cells forming a papillae or spheroid without fibrovascular cores (Diagn Cytopathol 2020;48:111)
- Nuclei are highly pleomorphic with hyperchromasia, thickened nuclear membrane and prominent nucleoli (Diagn Cytopathol 2020;48:111, Am J Surg Pathol 1994;18:1224)
- Abundant eosinophilic or slightly clear cytoplasm (Am J Surg Pathol 1994;18:1224)
Positive stains
- CK7, CK20 (Diagn Cytopathol 2020;48:111, Hum Pathol 2010;41:1159, Histopathology 2004;45:55)
- GATA3, S100P, p63 (27 - 54%) (Hum Pathol 2014;45:1473)
- Uroplakin II and III (Hum Pathol 2010;41:1159, Am J Clin Pathol 2014;142:864)
- MUC1 and MUC2 (Urol Oncol 2020;38:449, Diagn Cytopathol 2020;48:111, Hum Pathol 2010;41:1159)
- PTEN (Diagn Cytopathol 2020;48:111, Hum Pathol 2010;41:1159)
- E-cadherin (Diagn Cytopathol 2020;48:111)
- EMA, CEA (Histopathology 2004;45:55)
- CA-125 (33 - 43%) (Histopathology 2004;45:55, Mod Pathol 2009;22:660)
- HER2 IHC studies have overall given conflicting results; it is inconclusive if HER2 is more likely to be expressed by IHC compared with CUC (Mol Clin Oncol 2019;10:205)
Negative stains
- CD31, including on any cells lining the lacunae (J Urol 2000;163:748)
- CDX2, villin (Urol Oncol 2020;38:449, Diagn Cytopathol 2020;48:111)
- MUC5AC, MUC6 (Diagn Cytopathol 2020;48:111, Hum Pathol 2010;41:1159)
- TTF1 (Am J Surg Pathol 2009;33:1037)
- ER, mammaglobin (Am J Surg Pathol 2009;33:1037)
- WT1, PAX8 (Am J Surg Pathol 2009;33:1037)
Molecular / cytogenetics description
- Almost exclusively luminal subtype (as opposed to basal) with increased peroxisome proliferator activated receptor γ and downregulation of p63 genes (Eur Urol 2016;70:611)
- Subset has wild type p53 upregulation, which is associated with shorter survival (Eur Urol 2019;75:649)
- Unique activating mutations in the extracellular HER2 domain are more likely in MPUC than CUC (Clin Cancer Res 2014;20:68)
- HER2 amplification by FISH at higher frequency (< 42%) compared with CUC (< 14%) (Mol Clin Oncol 2019;10:205)
- Overexpression of Aurora A compared with CUC (Urol Int 2009;82:312)
- Point mutations in HRAS (exon 1) and KRAS (exon 1) (Pathol Int 2011;61:723)
- Downregulation of miR-296 and upregulation of RUVBL1 (chromatin remodeling complex) (Eur Urol 2016;70:611)
- TERT mutation (C228T or C250T) (Virchows Arch 2016;469:427)
- FABP3, CD36 and RAET1E gene expression found to be associated with faster time to progression (Sci Rep 2020;10:20135)
Videos
Bladder urothelial carcinoma
Sample pathology report
- Bladder, transurethral resection:
- Urothelial carcinoma, high grade
- Histologic component: micropapillary (90%)
- Adjacent flat carcinoma in situ: absent
- Angiolymphatic invasion: absent
- Muscularis propria: present, invaded by carcinoma
- Depth of invasion: invasive of muscularis propria (pT2)
- Urothelial carcinoma, high grade
- Bladder, cystectomy:
- Invasive high grade urothelial carcinoma, micropapillary subtype (see synoptic report)
Differential diagnosis
- Factors favoring micropapillary urothelial cell carcinoma:
- Multiple small nests in lacunar space
- In situ urothelial carcinoma present
- Foci of cohesive growth
- Consistent immunohistochemical profile for urothelial carcinoma (uroplakin II, GATA3, CK7, CK20 positive)
- Other urothelial carcinoma histologic subtypes present
- Conventional urothelial carcinoma with stromal retraction:
- Anastomosing cords without multiple small nests in lacunar spaces
- Nephrogenic metaplasia (adenoma) with papillary growth:
- Papillary renal cell carcinoma:
- Metastatic ovarian high grade serous carcinoma:
- Has psammoma bodies (Am J Surg Pathol 1994;18:1224)
- Positive for WT1, PAX8, negative for GATA3
- Metastatic breast micropapillary carcinoma:
- Metastatic lung micropapillary carcinoma:
Board review style question #1
Which of the following is true regarding the histologic subtype of urothelial carcinoma shown above?
- Fibrovascular cores should be present in order to call it this histologic subtype
- Neoadjuvant chemotherapy is the standard of care for this subtype
- Patients are more likely to have better outcomes if this subtype represents > 10% of the tumor content
- Patients are more likely to present at an advanced stage compared with conventional urothelial carcinoma
- There is no concordant in situ histologic correlation to this subtype
Board review style answer #1
D. Patients are more likely to present at an advanced stage compared with conventional urothelial carcinoma
The image above is the micropapillary histologic subtype of urothelial carcinoma. When micropapillary histology is found on biopsy, patients are more likely to already have muscularis propria invasion, lymph node metastasis and extravesicular extension, overall conferring a worse prognosis and why it is important to report this subtype. The role of neoadjuvant therapy before radical cystectomy in micropapillary cases is not clear and may not actually improve overall survival (choice B is incorrect). Fibrovascular cores should not be present within the clusters of cells (choice A is incorrect). If the micropapillary histology comprises > 10% of the tumor, then patients are more likely to have worse, not better outcomes (choice C is incorrect). There is an in situ micropapillary subtype that will look like slender filiform processes (choice E is incorrect) (Urol Oncol 2019;37:48, Urol Oncol 2014;32:110, World J Urol 2012;30:801, Eur Urol 2019;75:649, Histopathology 2004;45:55, Am J Surg Pathol 1994;18:1224).
Comment Here
Reference: Micropapillary urothelial carcinoma
The image above is the micropapillary histologic subtype of urothelial carcinoma. When micropapillary histology is found on biopsy, patients are more likely to already have muscularis propria invasion, lymph node metastasis and extravesicular extension, overall conferring a worse prognosis and why it is important to report this subtype. The role of neoadjuvant therapy before radical cystectomy in micropapillary cases is not clear and may not actually improve overall survival (choice B is incorrect). Fibrovascular cores should not be present within the clusters of cells (choice A is incorrect). If the micropapillary histology comprises > 10% of the tumor, then patients are more likely to have worse, not better outcomes (choice C is incorrect). There is an in situ micropapillary subtype that will look like slender filiform processes (choice E is incorrect) (Urol Oncol 2019;37:48, Urol Oncol 2014;32:110, World J Urol 2012;30:801, Eur Urol 2019;75:649, Histopathology 2004;45:55, Am J Surg Pathol 1994;18:1224).
Comment Here
Reference: Micropapillary urothelial carcinoma