Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Anderson D, Tretiakova M. Tubulocystic. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumormalignanttubulocystic.html. Accessed January 6th, 2025.
Definition / general
- Renal epithelial neoplasm composed exclusively of tubules and cysts lined by a single layer of cells with prominent nucleoli (equivalent to ISUP / WHO grade 3) and abundant eosinophilic cytoplasm (Eur Urol 2016;70:93)
- Relatively indolent with < 10% cases showing disease progression, local recurrence or metastasis to bone, liver and lymph nodes (Eur Urol 2016;70:93)
Essential features
- Well circumscribed tumor with spongy bubble wrap appearance
- Male predominance
- Cystic and tubular architecture; no solid areas, hemorrhage or necrosis
- Single layer of flat, cuboidal or hobnailed eosinophilic cells with large nucleoli and lining fibrotic septa
- According to the ISUP, tubulocystic renal cell carcinoma terminology should not be used when there is a tubulocystic pattern admixed with the usual elements of papillary renal cell carcinoma or collecting duct carcinoma (Mod Pathol 2019;32:701)
Terminology
- Originally named Bellinien epithelioma or collecting duct carcinoma, by Pierre Masson in the 1950s (Am J Surg Pathol 2016;40:1457)
- Low grade collecting duct carcinoma (McLennan) (Urology 1997;50:679)
- Termed tubulocystic renal cell carcinoma and considered a distinct entity since 2009 (Am J Surg Pathol 2008;32:177)
- Recognized by the 2016 WHO classification
ICD coding
- ICD-O: 8316/3 - cyst associated renal cell carcinoma
- ICD-10: C64 - malignant neoplasm of kidney, except renal pelvis
- ICD-11: 2C90.0 & XH7K79 - malignant neoplasms of kidney, except renal pelvis & tubulocystic renal cell carcinoma
Epidemiology
- Rare (< 1% of renal tumors)
- Mean age: 58.4 years (range: 30 - 74 years)
- M:F = 7:1 (Am J Surg Pathol 2009;33:384)
Sites
- Left kidney predominance with involvement of the cortex and corticomedullary junction
Pathophysiology
- Histogenesis remains unclear; cells have some features of proximal nephron differentiation and others related to distal nephron (Can Urol Assoc J 2015;9:E654)
Clinical features
- Often an incidental finding
- Less commonly presents with abdominal pain, distention, hematuria, weight loss
- Prognosis is typically excellent with only rare reports of clinical progression and aggressive behavior (Am J Surg Pathol 2016;40:1457)
- References: Am J Surg Pathol 2009;33:384, Mod Pathol 2019;32:701, Am J Surg Pathol 2016;40:1457
Diagnosis
- Diagnosis is made on gross and H&E with attention paid to strict criteria of tubular and cystic growth
- Adequate sampling should be applied in order to exclude possible mimics
- Use of immunohistochemistry is limited but fumarate hydratase (FH) and S-(2-succino)-cysteine (2SC) could be considered to exclude FH deficient RCC, a lookalike
Radiology description
- MRI superior to CT; characterized by multilocular cystic lesions, Bosniak classification II - IV, with hypovascular septa (Abdom Radiol (NY) 2018;43:1540)
- Ultrasonography (US) pattern may exhibit high echogenicity and posterior acoustic enhancement (Eur Radiol 2016;26:1108)
Case reports
- 34 year old man with a 1.4 cm mass (Case #484)
- 40 year old man with end stage renal disease and incidental mass of the native left kidney (GUPS: Case of the Week [Accessed 18 August 2022])
- 45 year old man initially misdiagnosed with a Bosniak type II renal cyst (Rev Urol 2016;18:118)
- 59 year old man with features of cystic renal oncocytoma (Case Rep Urol 2019;2019:2919686)
- 62 year old man with bilateral tumors in diabetic end stage renal disease (Rare Tumors 2013;5:e57)
- 65 year old man with a large cystic tumor (Can Urol Assoc J 2015;9:E654)
- 65 year old man with tubulocystic renal cell carcinoma of the native kidney (Case Rep Nephrol 2020;2020:7145652)
Treatment
- Radical or partial nephrectomy depending on tumor size and location in the kidney
Gross description
- Well circumscribed but not encapsulated
- Cut surface that is gray-white with multilocular cystic spaces resembling Swiss cheese, sponge or bubble wrap-like appearance, usually containing clear fluid
- Mean size 4 cm (range 0.2 - 17 cm)
- No hemorrhage or necrosis
- References: Am J Surg Pathol 2009;33:384, Mod Pathol 2019;32:701, Am J Surg Pathol 2016;40:1457
Gross images
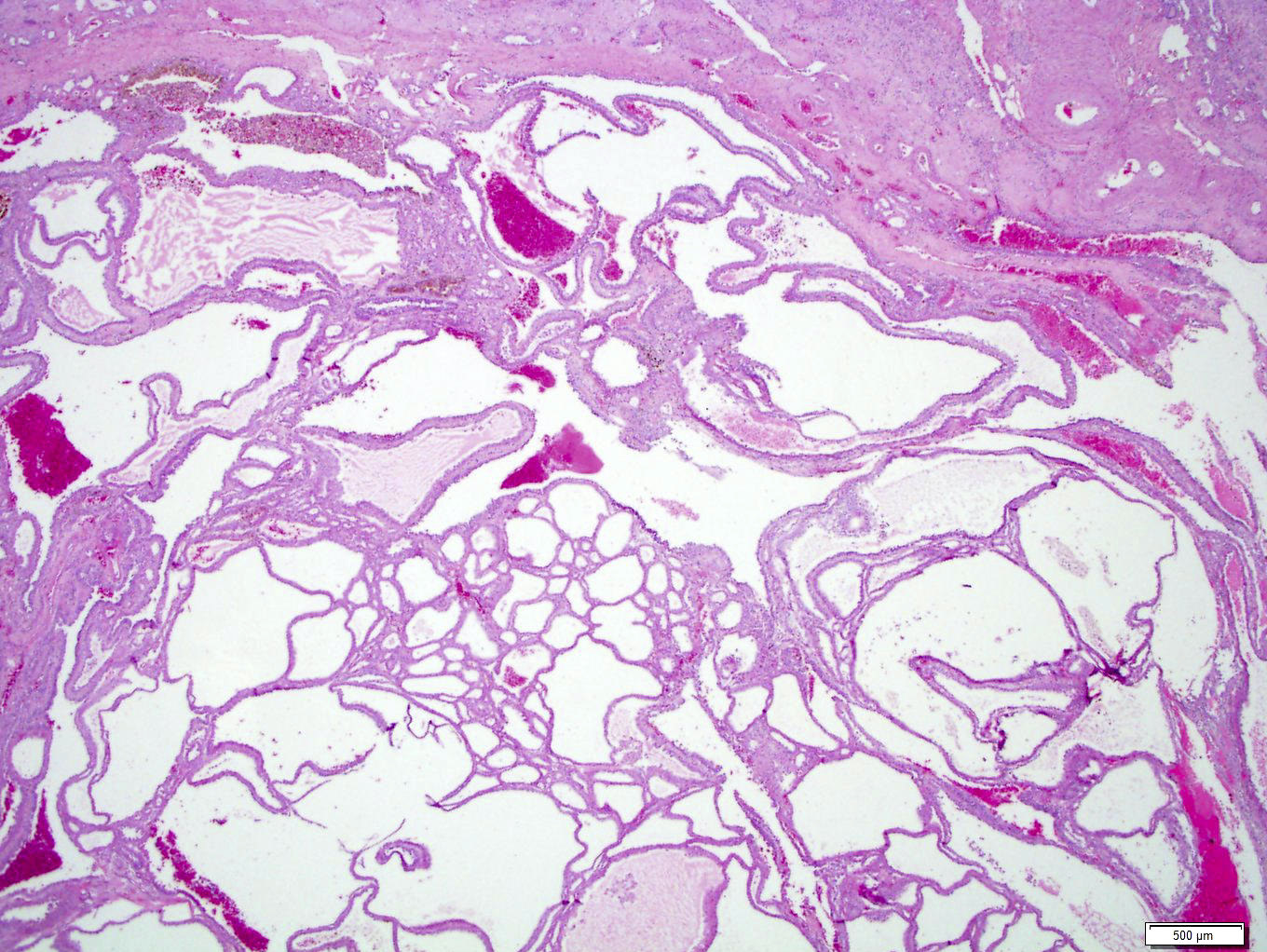
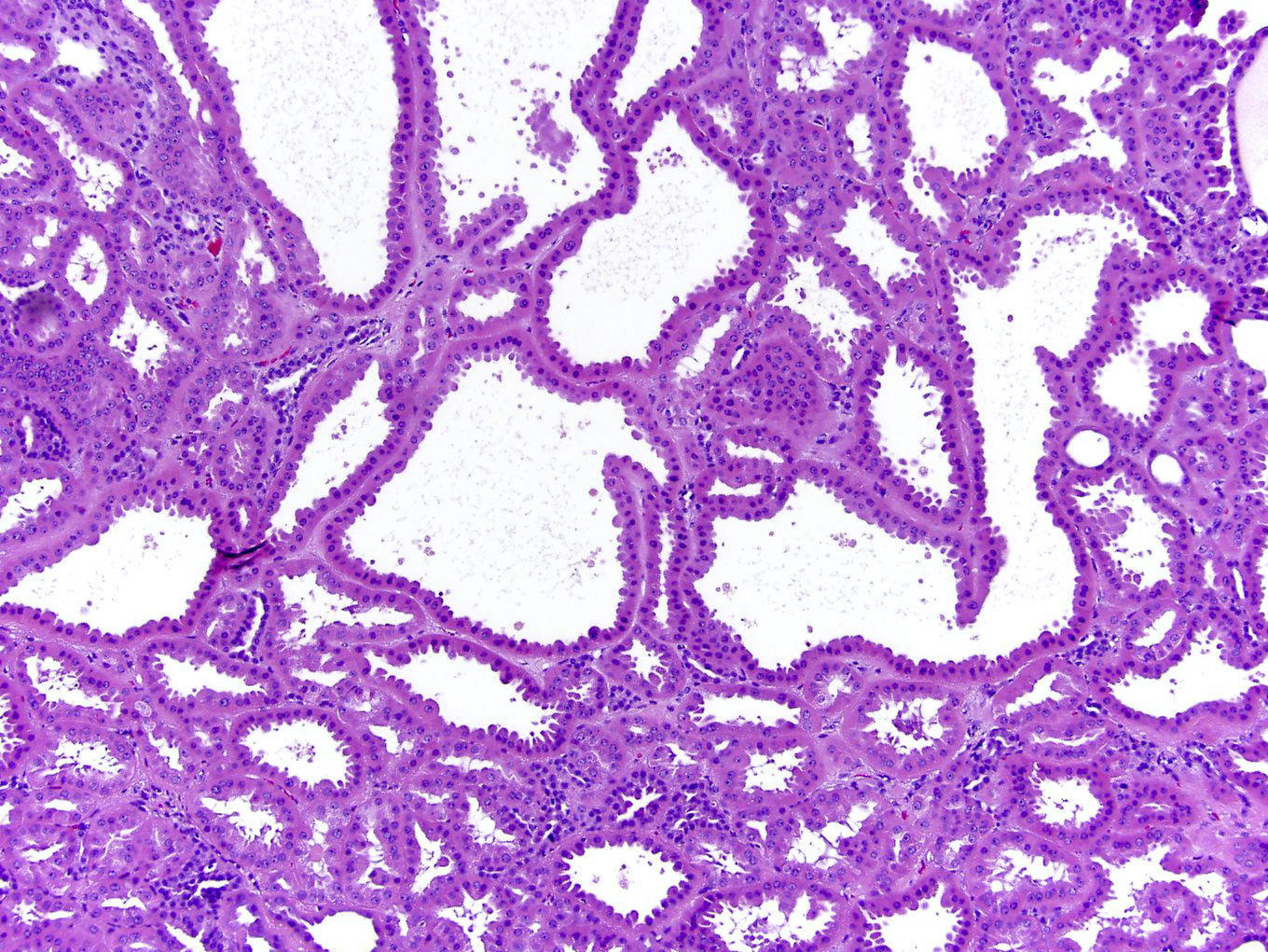
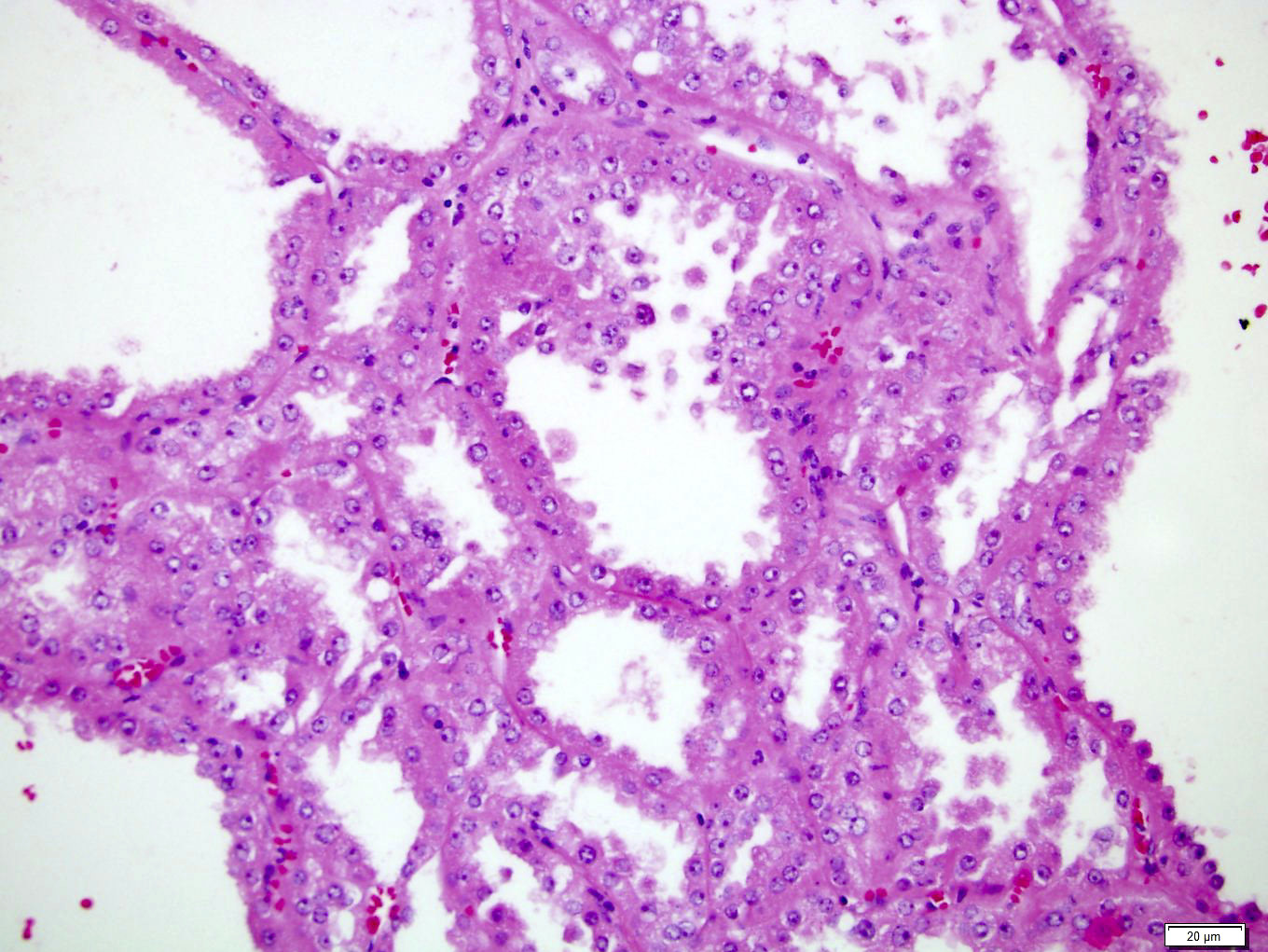
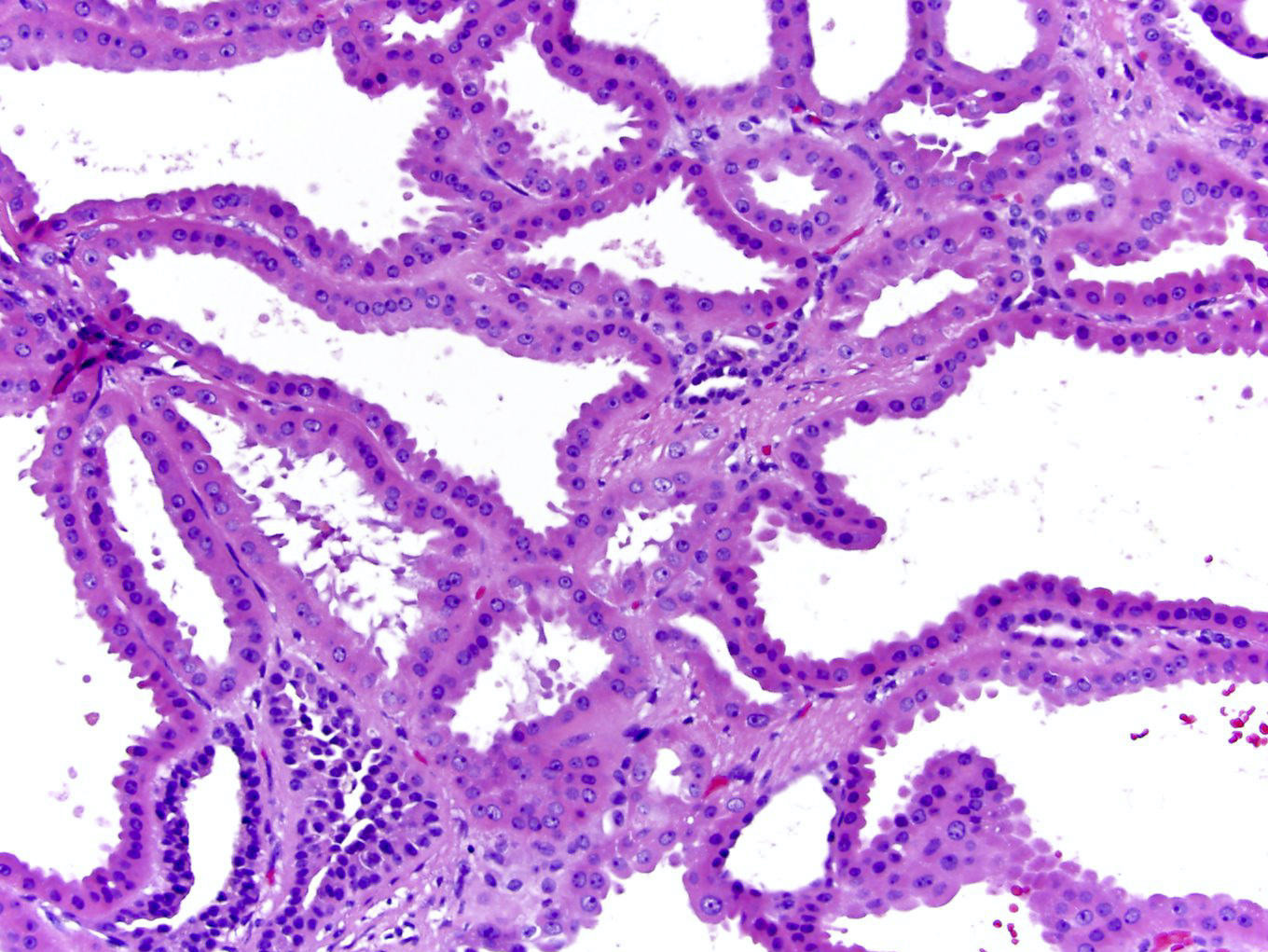
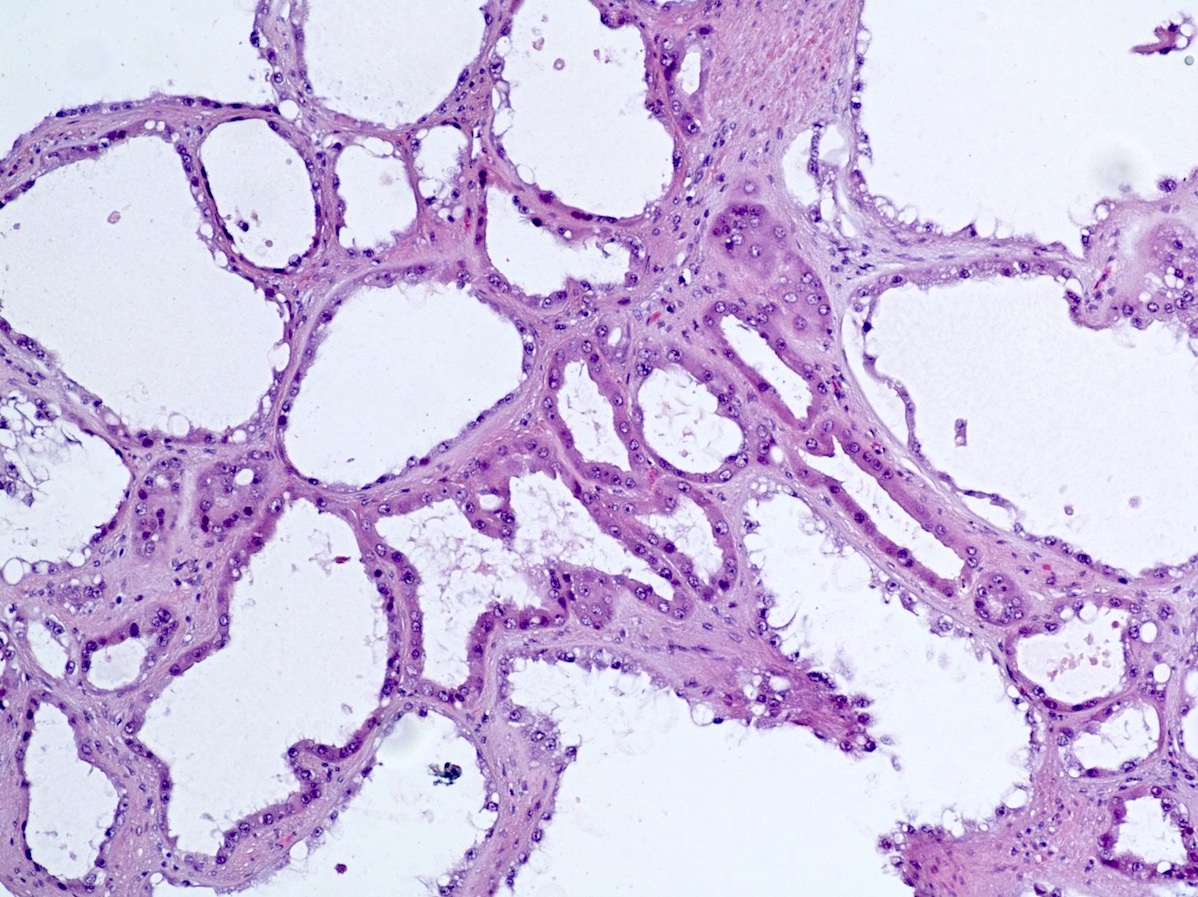
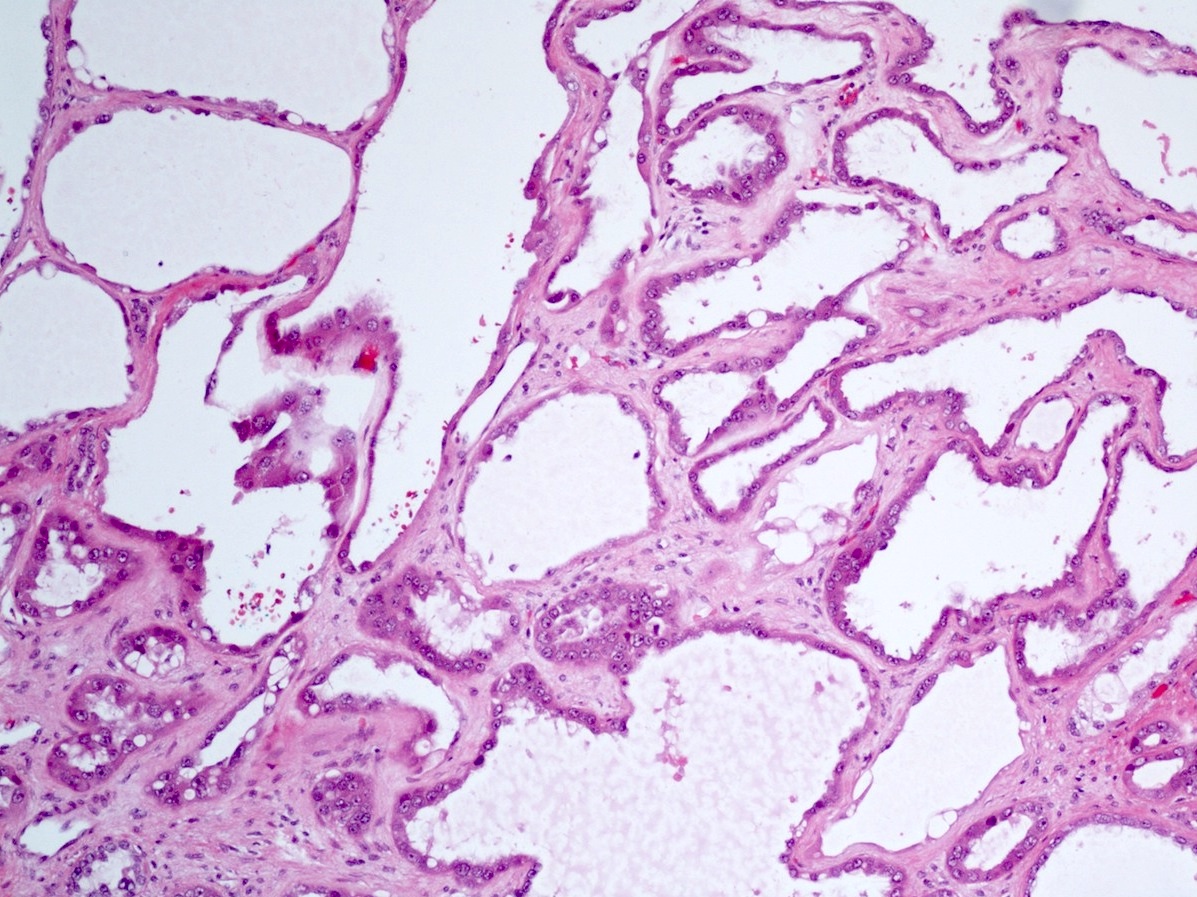
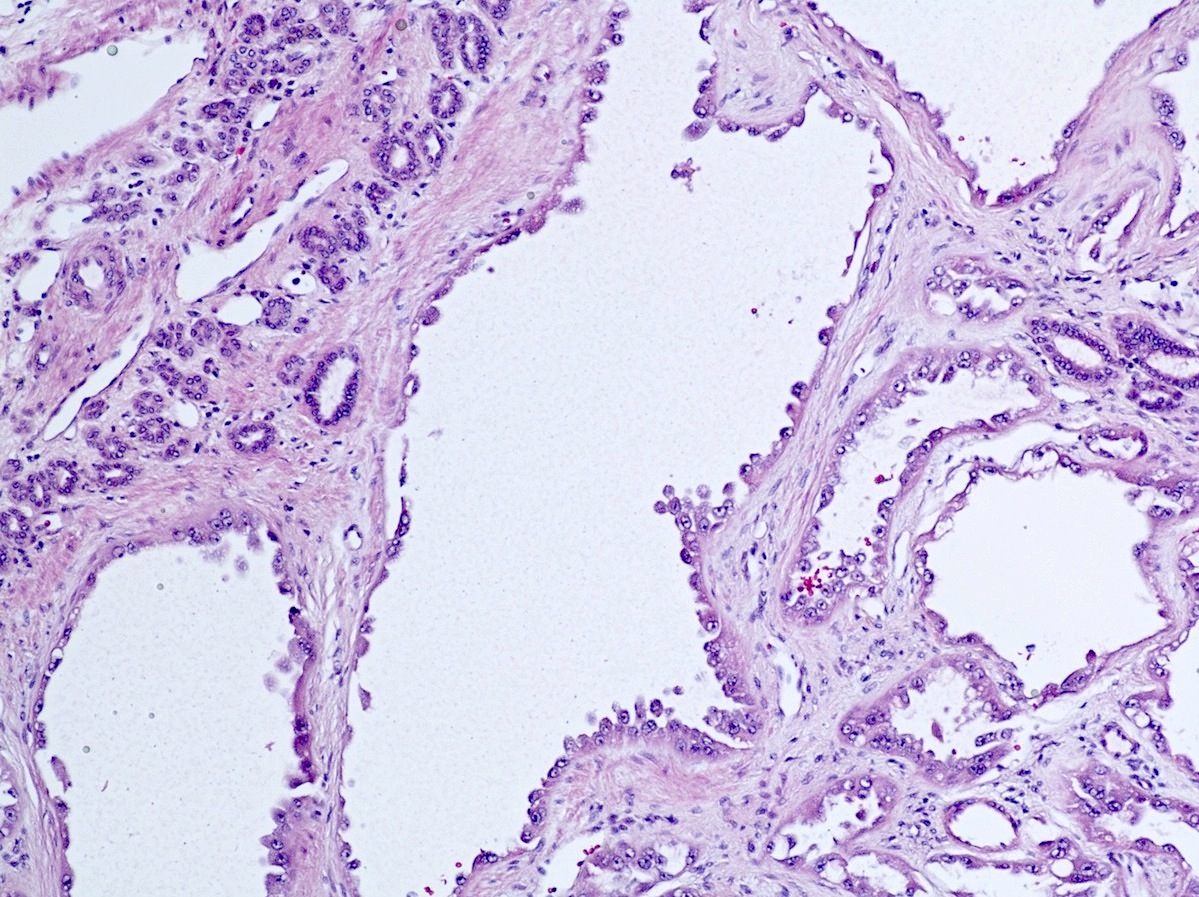
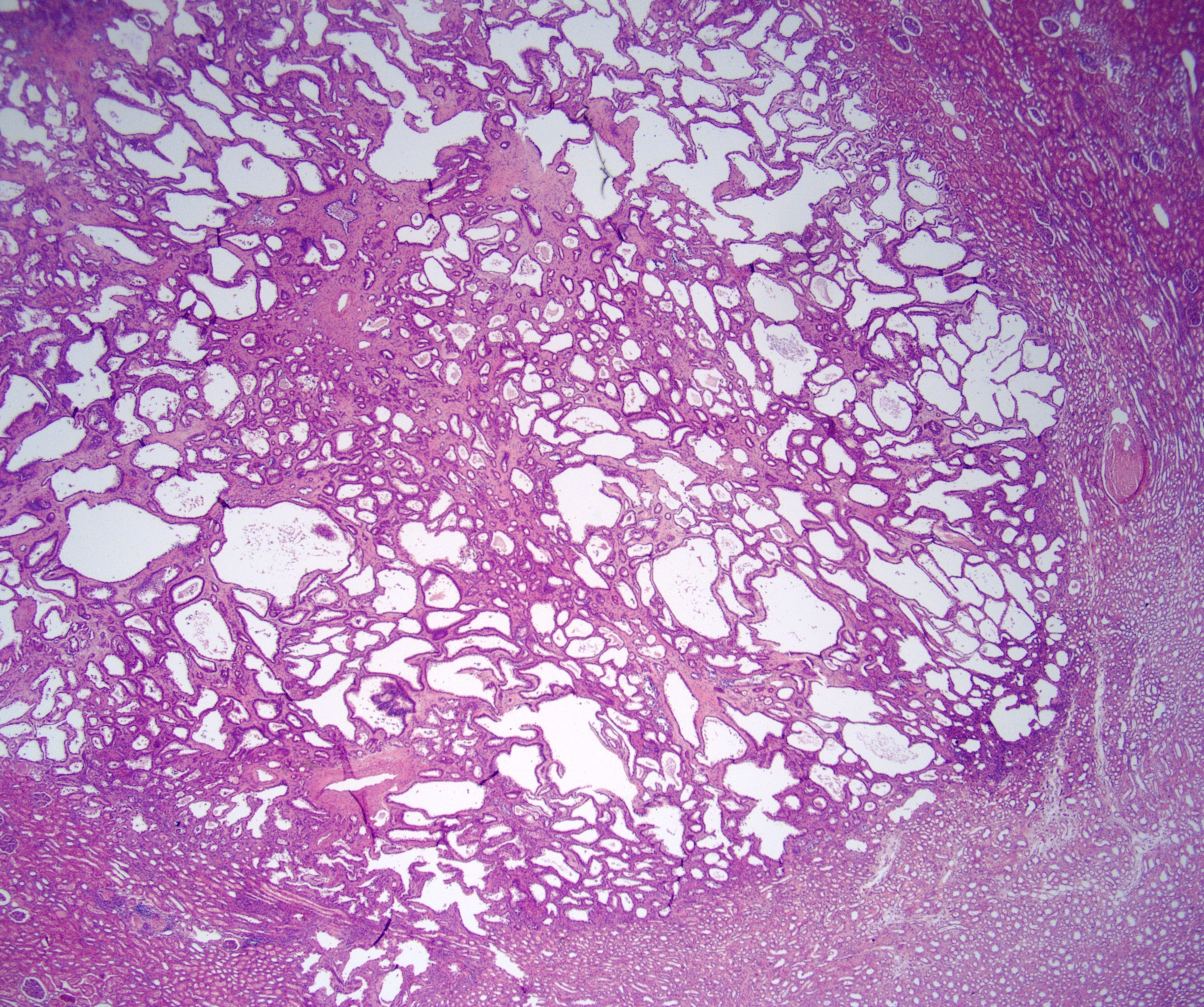
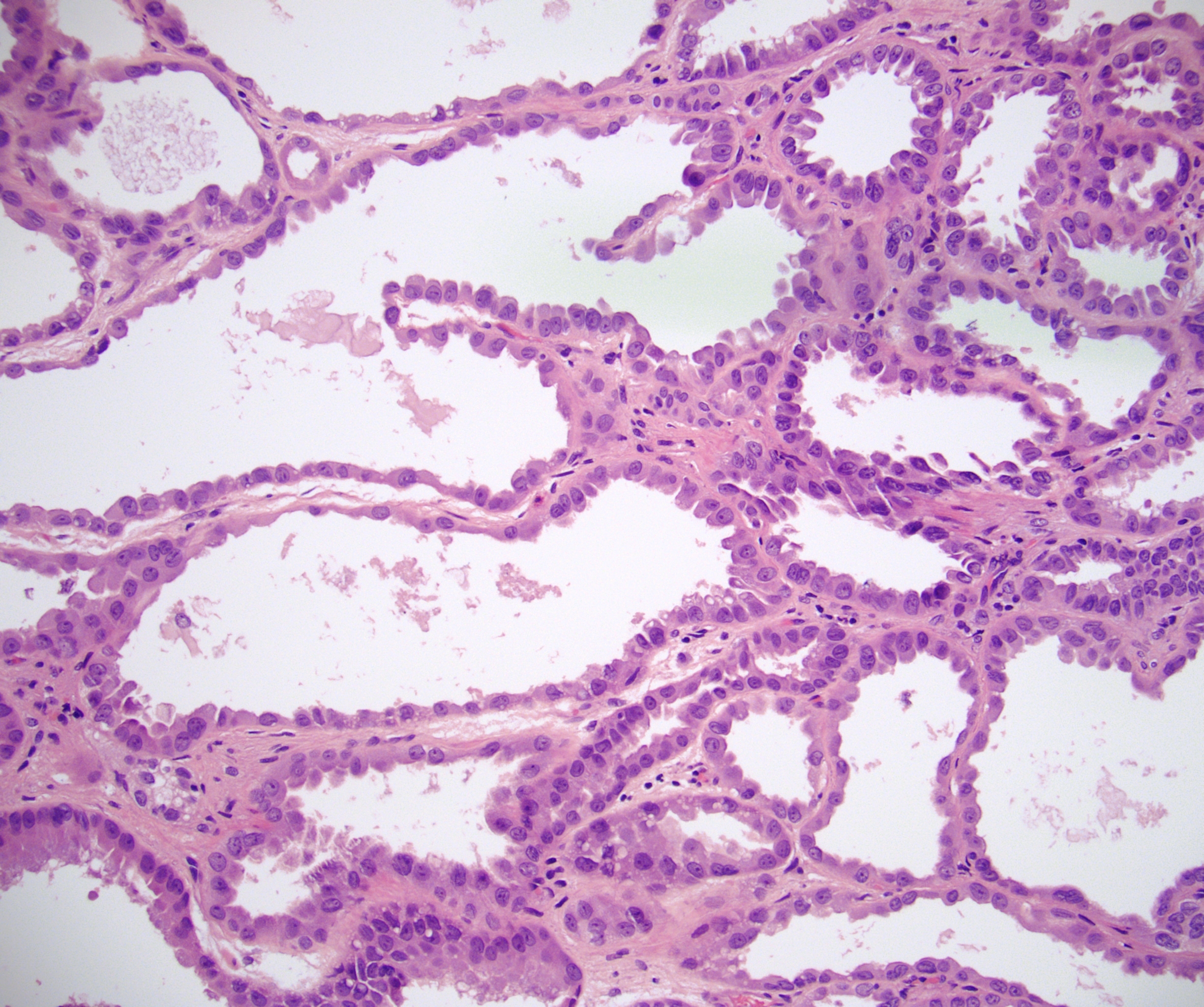
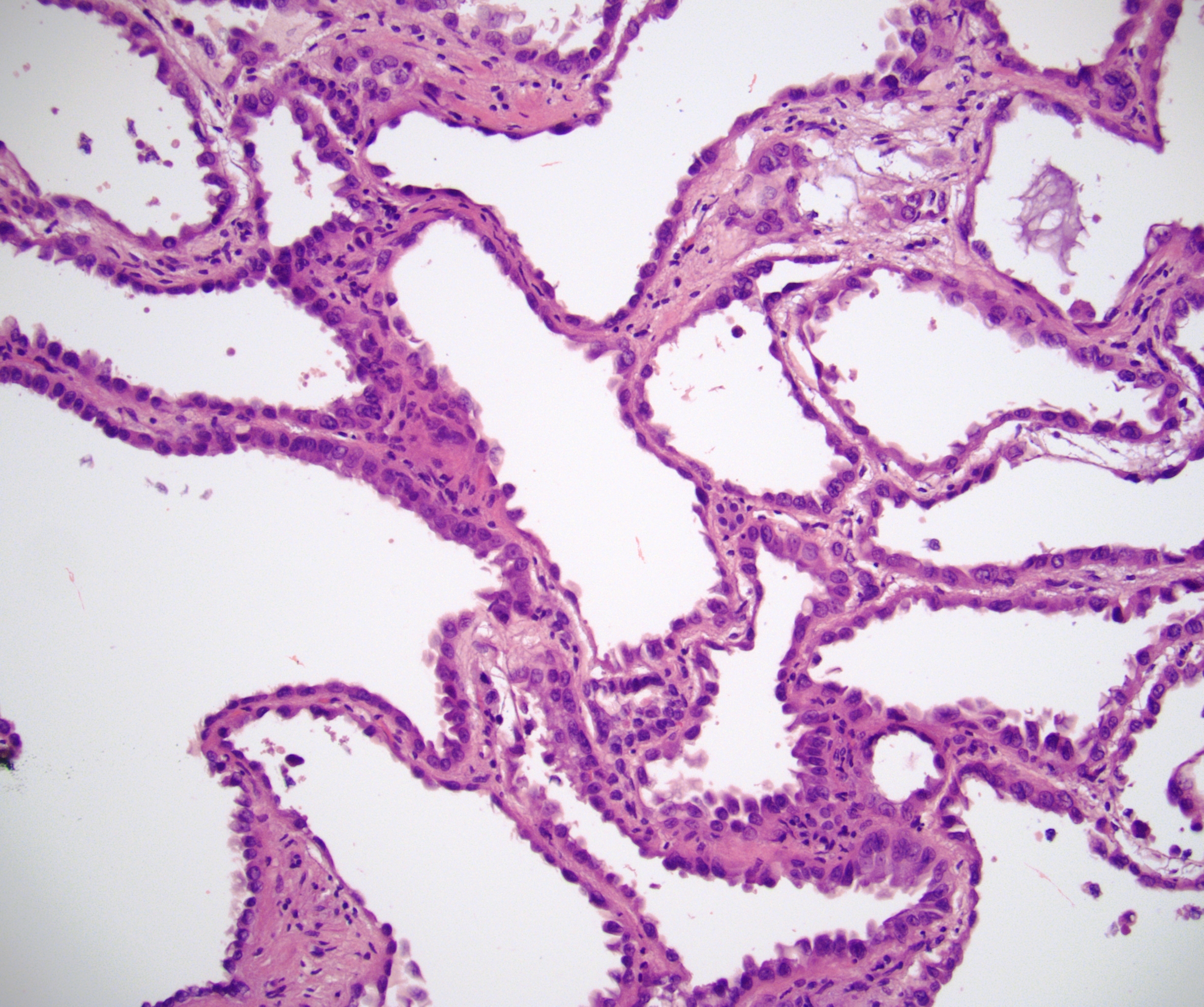
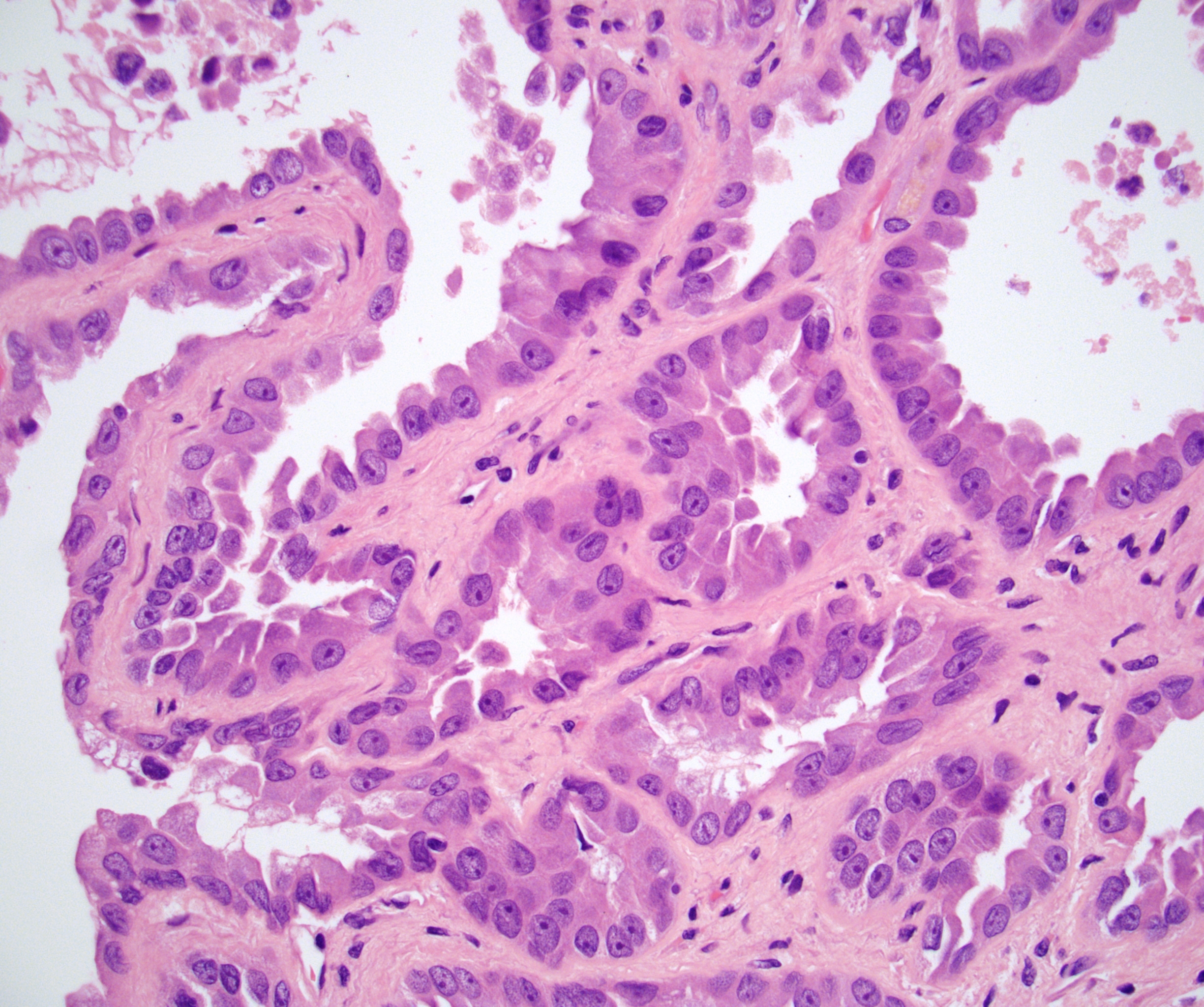
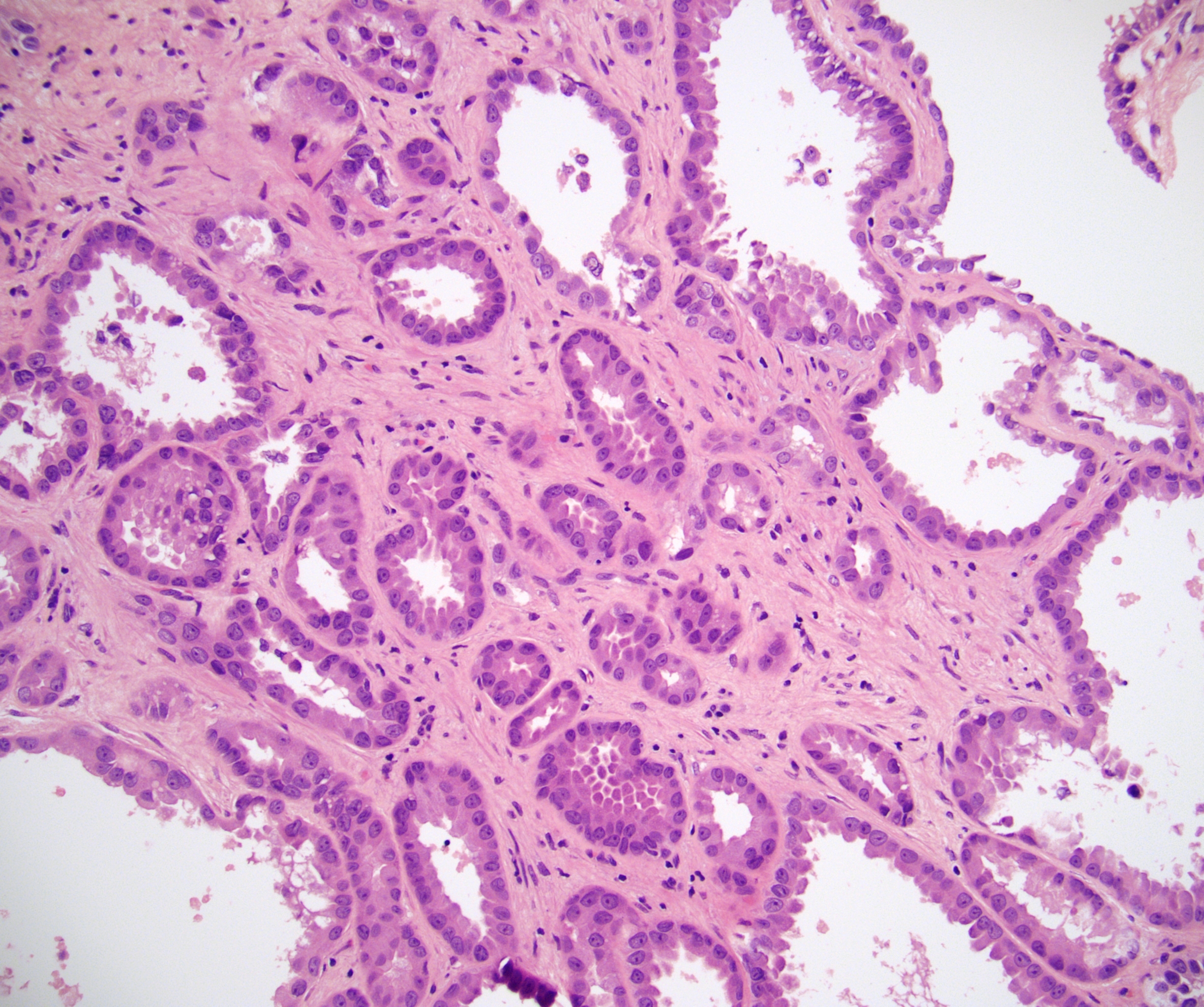
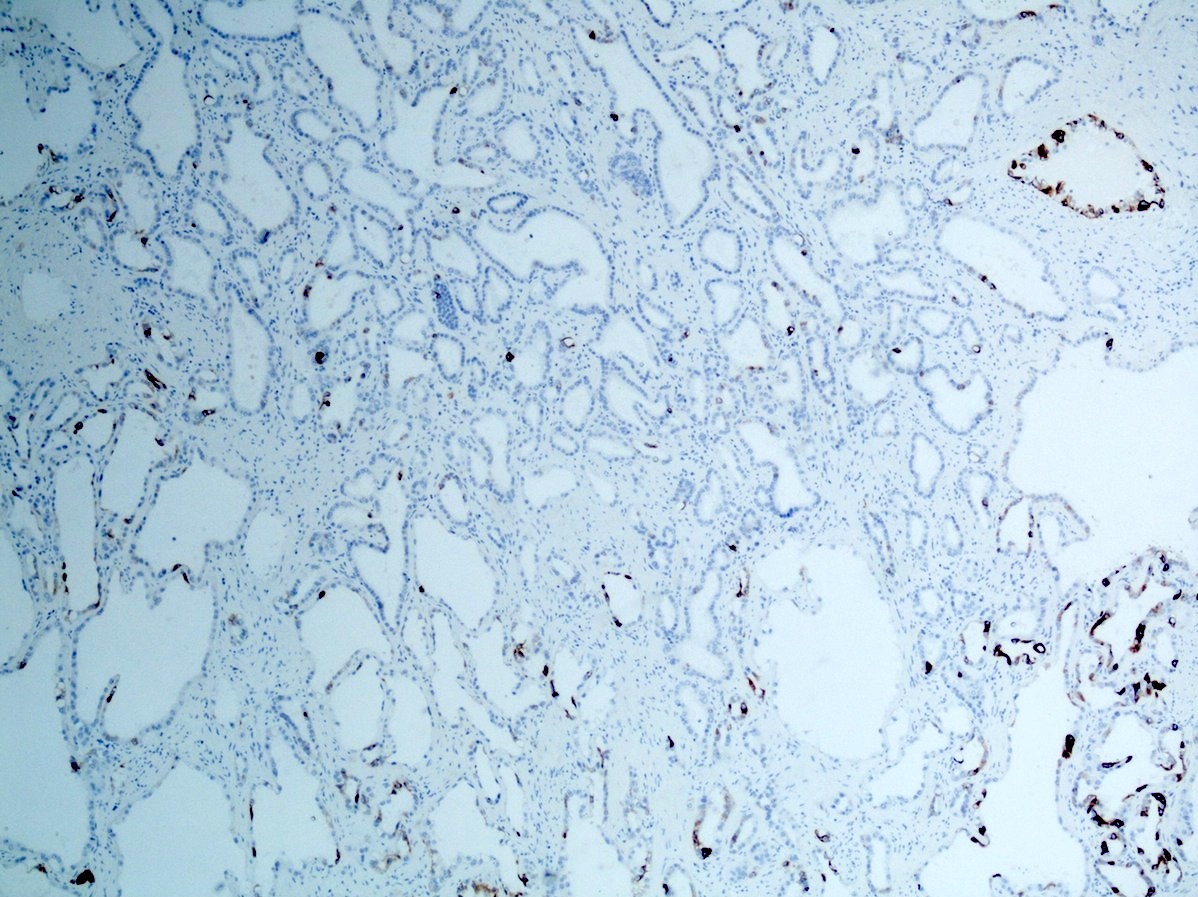
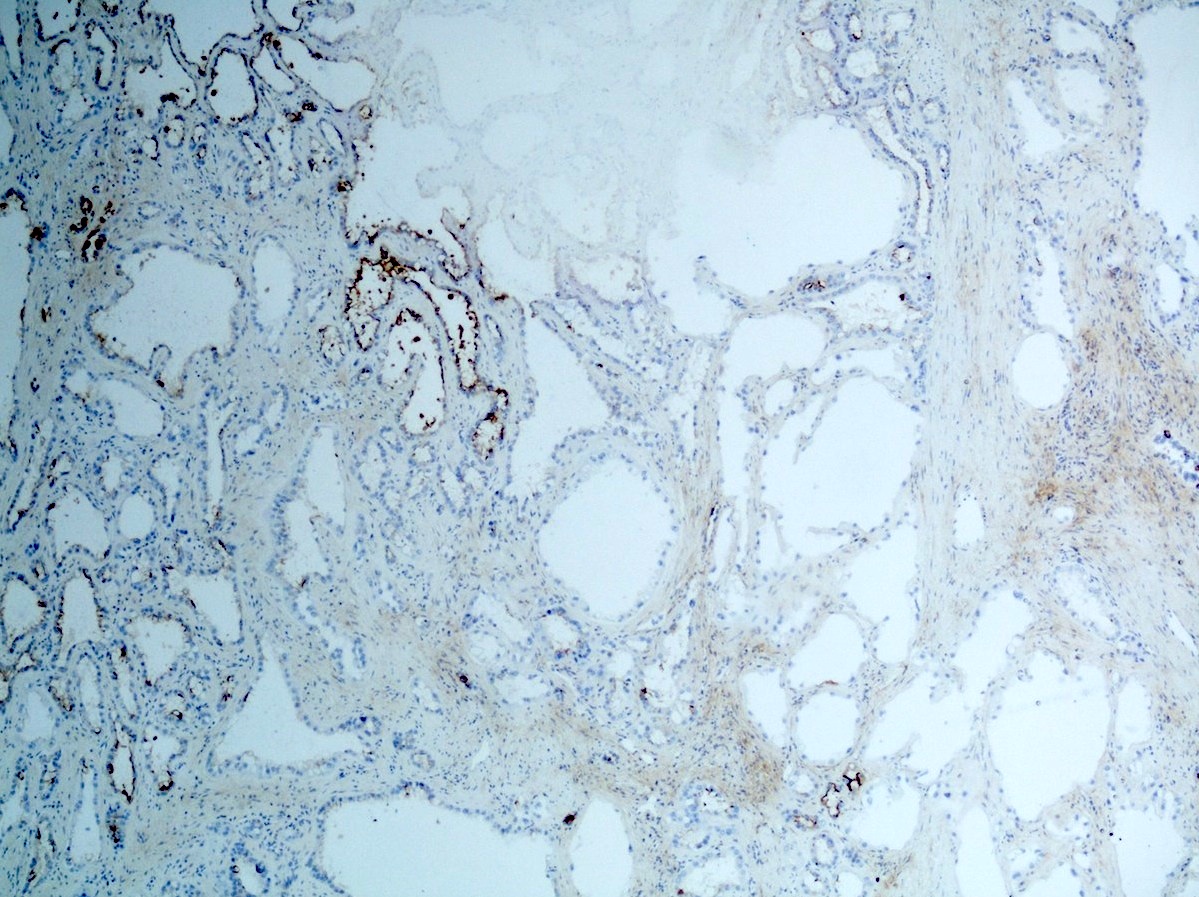
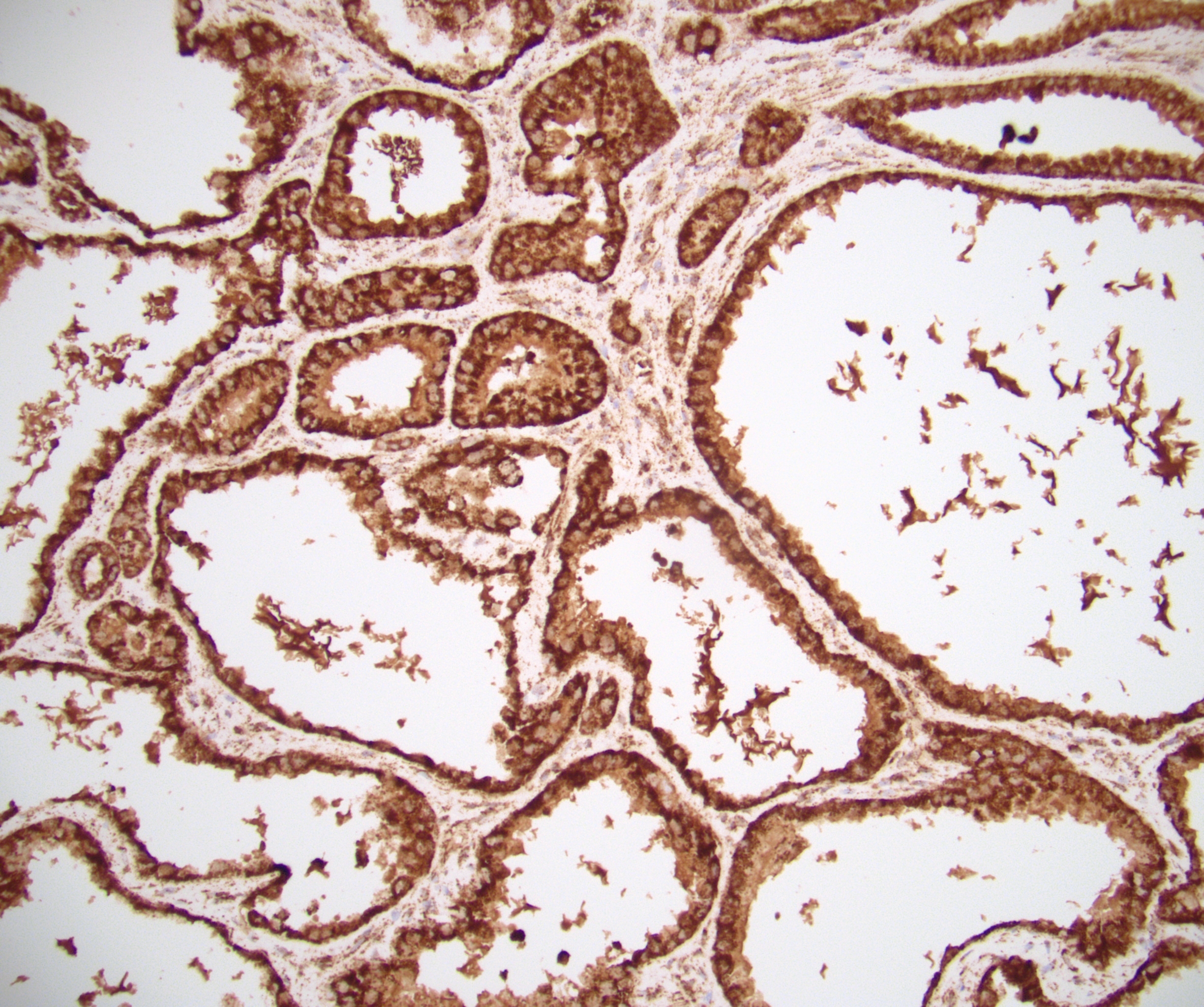
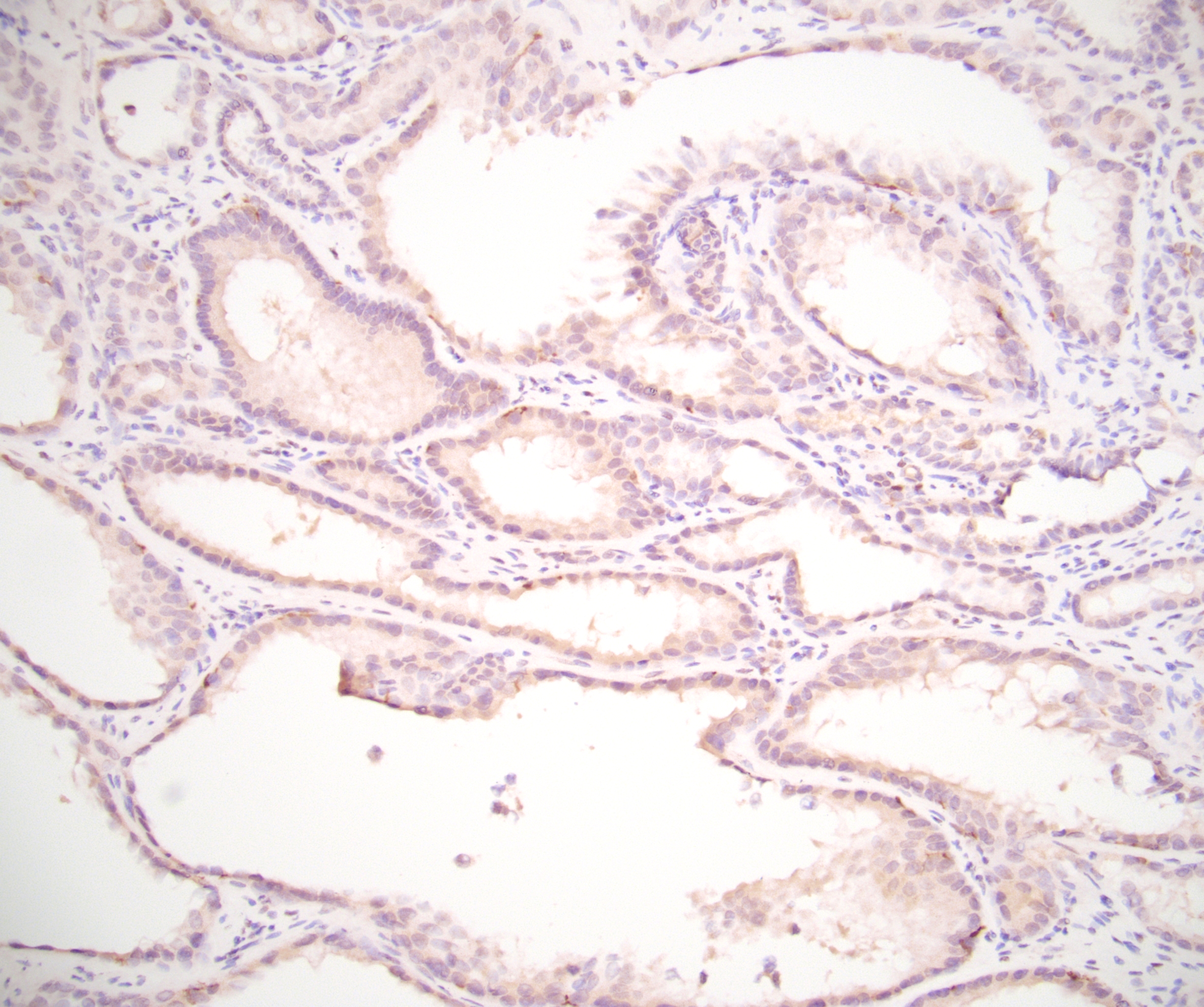
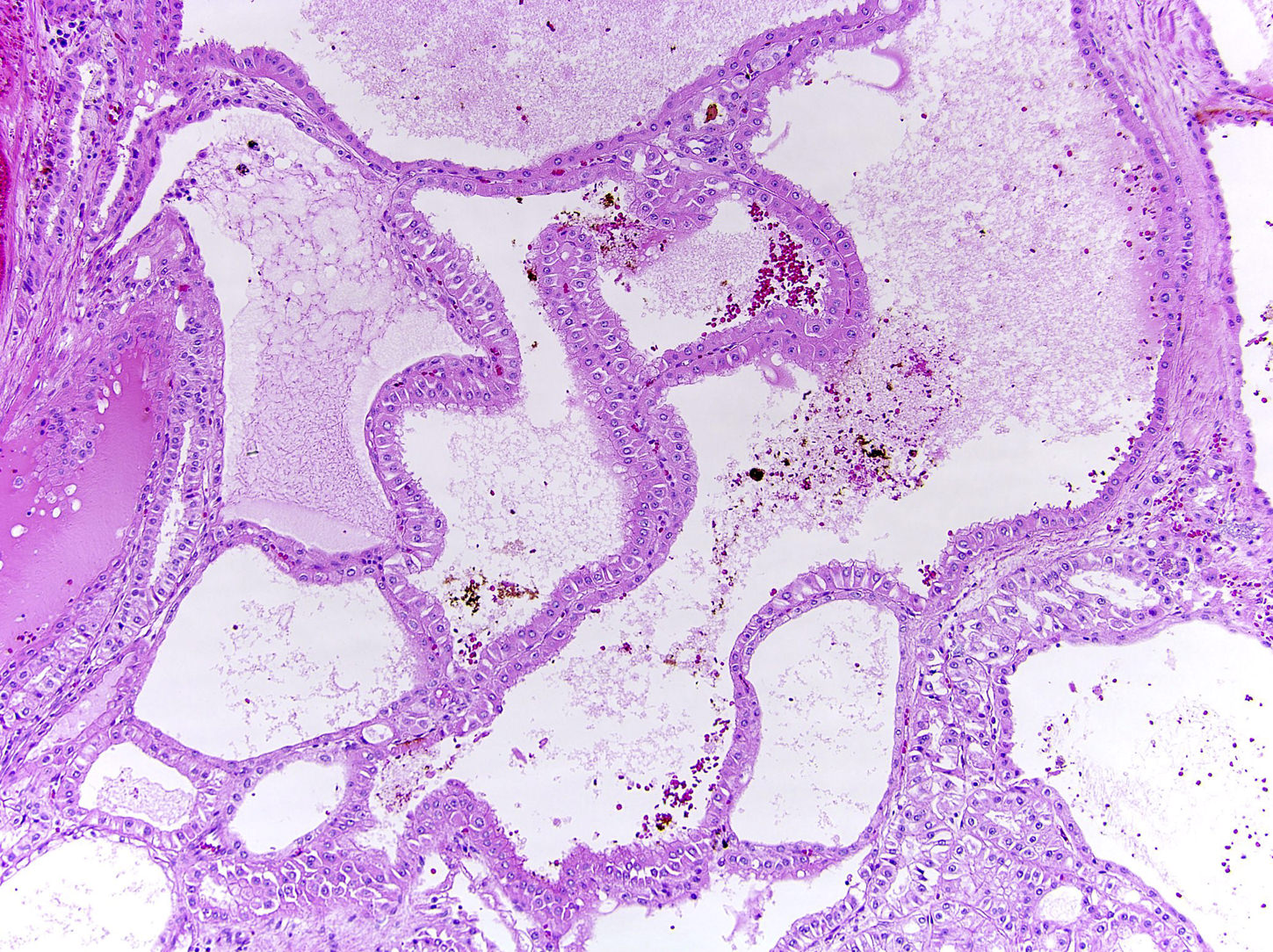
Microscopic (histologic) description
- Mixture of closely packed small to intermediate tubules and variably sized cysts (Urology 1997;50:679)
- Cysts are separated by fibrous septa; no desmoplasia or cellular stroma
- Tubules and cysts are lined by a single layer of flattened, cuboidal or columnar cells with enlarged, irregular nuclei with modest to abundant amounts of eosinophilic cytoplasm; hobnailing may be present
- Distinct nucleoli (equivalent to ISUP / WHO grade 3)
- Cysts are separated by hypocellular, fibrous septa
- Minimal mitotic activity
- Strict morphologic criteria should be used; cases with papillary growth, poor differentiation or sarcomatoid component usually exclude the diagnosis (Mod Pathol 2019;32:701)
- Histologic grading not necessary
Microscopic (histologic) images
Contributed by Maria Tretiakova, M.D., Ph.D., Sabrina Sopha, M.D. and Debra Zynger, M.D. (Case #484)
Cytology description
- Sheets of cells with granular cytoplasm, distinct borders, intracellular windows between cells, distinct nucleoli, rare cytoplasmic vacuoles and rare nuclear grooves (Diagn Cytopathol 2018;46:707)
Positive stains
- Keratins (AE1 / AE3, CAM 5.2, CK8 / 18, CK19, EMA) (Am J Surg Pathol 2005;29:747)
- PAX8, vimentin
- AMACR (racemase), fumarate hydratase (retained)
- CK7 and CD10 may be patchy (Mod Pathol 2019;32:701)
- Variable 34 beta E12 (usually less diffuse than CK7 and CD10) (Mod Pathol 2019;32:701)
Electron microscopy description
- Ultrastructural features may resemble cells of the proximal tubules and collecting ducts
- Type I cells:
- Resemble proximal convoluted tubules and are seen in tubular component
- Cuboidal cells with luminal surface tight junction, short microvilli with brush border
- Type II cells:
- Ultrastructural features resemble distal nephrons
- Found in the cystic component
- Single layer of cells with desmosomal junction and luminal surfaces bound by tight junctions
- Contain rough endoplasmic reticulum, mitochondria and lipid droplets
- No microvilli
- Base bound by basement membrane
- Type I cells:
- Reference: Rare Tumors 2013;5:e57
Molecular / cytogenetics description
- Has a distinct genetic signature from other carcinomas (J Mol Diagn 2018;20:34, Mod Pathol 2019;32:701)
- Initially a close relationship to papillary renal cell carcinoma postulated based on gains of chromosome 7, 17, loss of Y but other studies lacked gains of chromosomes 7, 17 by FISH (Am J Surg Pathol 2009;33:1840, Am J Surg Pathol 2008;32:177, Histopathology 2016;68:850)
- Recent study showed chromosome 9 loss and chromosome 17 gain were found in all tumors by next generation sequencing (NGS) (Mod Pathol 2019;32:701)
- Consistent loss of Y chromosome was observed in all tumor cells tested by FISH
- Mutations were found in lysine N methyltransferase (KMT2C), a histone methyltransferase and lysine specific demethylase 5 C (KDM5C) in 2 of 9 (22%) cases
- Other known or likely oncogenic mutations detected in PMS2, RAD21, TP53, FBXW7 and KEAP1 were also detected (Mod Pathol 2019;32:701)
- Noncoding RNA sequencing has identified distinct patterns of small nucleolar RNA and mature and pre-miRNAs as well as mutations (> 60%) of ABL1 and PDFGRA genes; recent study did not identify somatic mutations in ABL1 and PDGGRA genes in 9 cases (J Mol Diagn 2018;20:34, Mod Pathol 2019;32:701)
- Lack of overlap in results is possibly indicative of genetic diversity and requires further study (Mod Pathol 2021;34:1392)
Molecular / cytogenetics images
Videos
Tubulocystic renal cell carcinoma
by Dr. Rajal Shah
Sample pathology report
- Kidney, partial nephrectomy:
- Tubulocystic renal cell carcinoma (x cm); margins are negative (see comment) (see synoptic report)
- Comment: Immunohistochemistry shows the tumor cells to be negative for 2SC with positive (retained) staining for fumarate hydratase.
Differential diagnosis
- Care should be taken when making the diagnosis, as tubulocystic architecture may be variably present in many renal tumors including those listed below
- Fumarate hydratase deficient renal cell carcinoma / hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome associated renal cancer:
- High grade tumors with solid, papillary and glandular architecture
- Characteristic large cytomegalovirus-like nucleoli with perinuclear halos
- FH gene mutations
- Will show loss of fumarate hydratase staining (highly specific but not sensitive) with aberrant positive staining for 2SC (sensitive but less specific) (Am J Surg Pathol 2016;40:1457)
- Prior cases described as as tubulocystic RCC with poorly differentiated foci may actually represent FH deficient RCC (Am J Surg Pathol 2016;40:1457)
- Adult cystic nephroma (mixed epithelial and stromal tumor):
- In adults, predominance in women
- Biphasic tumors with epithelial and stromal components
- Multilocular cysts are lined by attenuated cells with inconspicuous nucleoli
- Nonepithelial component could be very prominent with hyalinization, fibrosis and ovarian type cellular stroma
- Overlapping expression profile
- Multilocular cystic clear cell renal neoplasm of low malignant potential:
- Cysts lined by clear cells with low grade nuclei (ISUP grade 1 - 2), nests of clear cells in stroma
- CAIX positive
- Mucinous tubular and spindle cell carcinoma:
- Predominantly women
- Typically long tubular profiles or cord-like growth pattern of uniform, low cuboidal cells with eosinophilic, focally vacuolated cytoplasm and spindling
- Stroma is myxoid and bubbly with abundant extracellular mucin
- Oncocytoma:
- Cut surfaces with dark brown appearance and central scar in 33% of cases
- Occasionally shows extrarenal extension into fat rather than organ confined
- Background has fibromyxoid / hyalinized appearance
- Uncommonly can have tubules with cystic dilation which can be a histologic mimic
- Large, round polygonal cells with eosinophilic cytoplasm
- Usually do not see prominent nucleoli or nuclear variability
- CK7 negative or scattered; positive KIT / CD117
- Chromophobe renal cell carcinoma:
- Usually solid / nested growth with distinct cell borders and raisinoid nuclei
- CK7 diffuse and KIT / CD117 positive
- Collecting duct carcinoma:
- Usually symptomatic (pain, hematuria)
- Grossly solid appearance with irregular, infiltrative borders, involves medulla and sometimes into perirenal adipose tissue
- Tubulopapillary structures, cords, glandular or solid sheets; lacks cyst formation; may have dysplastic medullary collecting duct structures
- Stroma is inflamed and desmoplastic
- Often obvious mitotic activity
- Acquired cystic disease associated renal cell carcinoma:
- Associated with end stage renal disease
- Cribriform appearance with calcium oxalate crystals
- Papillary renal cell carcinoma:
- Papillary growth with strong CK7 positivity, may contain foamy macrophages
- Overlapping expression profile
Additional references
Board review style question #1
A 50 year old man undergoes a nephrectomy for a 3 cm cystic mass of the left kidney. A representative photomicrograph of the neoplasm is shown. Which statement is true about this entity?
- Can have prominent papillary growth
- Can show fumarate hydratase loss by immunohistochemistry
- Demonstrates an increased metastatic potential
- May show gain of chromosome 17 and losses of chromosomes 9 and Y
- Shows solid growth often
Board review style answer #1
D. May show gain of chromosome 17 and losses of chromosomes 9 and Y. The photomicrograph shows a tubulocystic renal cell carcinoma. This neoplasm may demonstrate gains of chromosome 17 and loss of chromosomes 9 and Y according to a recent study. Strict criteria should be used in the diagnosis as this entity is purported to have a relatively indolent prognosis. As such, this neoplasm should be exclusively cystic and tubular growth without solid, sarcomatoid or papillary growth. Fumarate hydratase deficient renal cell carcinoma should be considered in the differential especially if solid growth, heterogenous architecture, high grade features and perinuclear halos are seen. In contrast to FH deficient RCC, tubulocystic renal cell carcinoma should demonstrate retained fumarate hydratase by immunohistochemistry.
Comment Here
Reference: Tubulocystic renal cell carcinoma
Comment Here
Reference: Tubulocystic renal cell carcinoma
Board review style question #2
Board review style answer #2
D. Well circumscribed mass with spongy or bubble wrap appearance. Tubulocystic carcinoma has a very peculiar gross morphology, often compared to bubble wrap, sponge and Swiss cheese.
Comment Here
Reference: Tubulocystic renal cell carcinoma
Comment Here
Reference: Tubulocystic renal cell carcinoma