Table of Contents
Definition / general | Important features to include in the synoptic report | Features to report by organization | Gross images | Microscopic (histologic) images | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Rizkalla C, Tretiakova M. Features to report. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumormalignantreport.html. Accessed March 31st, 2025.
Definition / general
- The College of American Pathologists (CAP) synoptic protocol for kidney tumors outlines the essential elements that should be included in a pathology report to ensure complete and accurate communication of diagnostic and prognostic information
- A synoptic format is indicated if this is the definitive primary cancer resection specimen
Important features to include in the synoptic report
- Procedure type
- Partial nephrectomy
- Can usually be performed if a tumor is ≤ 4 cm, localized to 1 pole of the kidney and without radiologic renal sinus involvement
- Radical nephrectomy
- Includes entire kidney, variable lengths of the major renal vessels at the hilus, variable length of ureter and perirenal fatty tissue
- Partial nephrectomy
- Tumor focality
- Multifocality and multinodularity is a frequent sign of intravenous renal cell carcinoma (RCC) spread with complete filling of the vascular lumina
- As intravenous nodules enlarge, they can merge with the primary tumor, leading them to be falsely included in the measurement of the primary tumor size if the process of venous invasion is not recognized (Mod Pathol 2011;24:1578)
- Recognizing venous involvement is best assessed during gross examination when the kidney is bivalved (see Grossing)
- CD31 immunohistochemical stain can be useful in demonstrating the intravenous nature of the tumor nodules, which may be partially lost as intravenous tumors enlarge and obliterate the endothelial cell lining
- If the tumor is truly multifocal, it is more likely to be associated with a syndrome
- Multifocality and multinodularity is a frequent sign of intravenous renal cell carcinoma (RCC) spread with complete filling of the vascular lumina
- Tumor size
- Greatest dimension in centimeters with cutoffs of 4, 7 and 10 cm
- pT1 and pT2 are categories based on size of tumor when limited to kidney (see Staging)
- pT1: tumor ≤ 7 cm and limited to kidney
- pT1a: tumor ≤ 4 cm, limited to kidney
- pT1b: tumor > 4 cm but ≤ 7 cm, limited to kidney
- pT2: tumor > 7 cm and limited to kidney
- pT2a: tumor > 7 cm but ≤ 10 cm, limited to kidney
- pT2b: tumor > 10 cm, limited to kidney
- pT1: tumor ≤ 7 cm and limited to kidney
- Tumor extent
- Careful gross analysis is key (see Grossing)
- Renal sinus involvement is a main route for extrarenal extension; involvement of the renal sinus predicts a more aggressive outcome than perinephric fat invasion due to increased access to lymphovascular structures in that area (J Urol 2005;174:1218)
- Renal sinus involvement usually present if renal tumor size is > 7 cm
- Multinodularity or finger-like extensions from a renal mass should be viewed with great suspicion for the possibility of vein or renal sinus invasion (Histopathology 2019;74:18)
- If invasion of the renal sinus is unclear, it is recommended that at least 3 blocks of the tumor renal sinus interface is submitted; if invasion is grossly evident or grossly absent, only 1 block is needed to confirm gross inspection (Am J Surg Pathol 2013;37:1505)
- Renal sinus involvement includes tumor in contact with renal sinus fat, tumor present in loose connective tissue of renal sinus beyond the renal parenchyma, tumor involves endothelial lined spaces
- pT3: tumor is locally invasive (see Staging)
- pT3a: involves renal vein or its segmental branches, renal sinus, pelvicalyceal system or perinephric fat; perinephric fat invasion defined as either the tumor touching the fat or extending as irregular tongues into the perinephric tissue (Am J Surg Pathol 2013;37:1505)
- T3b: involves inferior vena cava (below diaphragm)
- T3c: involves inferior vena cava (above diaphragm) or invades the wall of vena cava
- pT4: tumor is invading surrounding organs
- Invades beyond Gerota fascia
- Contiguous spread to ipsilateral adrenal gland
- If there is noncontiguous spread involving adrenal gland, this is considered pM1 disease
- Histologic subtype
- Refer to the most up to date version of WHO for tumor classifications (Pathologica 2022;115:8) (see WHO classification)
- Depending on the subtype, the clinical behavior, prognosis and management can vary widely
- Histologic grade (see Grading)
- Based on a single high power field showing the greatest degree of pleomorphism
- Grade 1 - 3: based on greatest degree of nucleolar prominence (Histopathology 2019;74:4)
- Grade 4: based on nuclear pleomorphism, anaplastic giant cells, rhabdoid morphology and sarcomatoid differentiation (Histol Histopathol 2004;19:113, Histopathology 2019;74:4)
- Tumor necrosis
- Has prognostic implications: tumors with microscopic tumor necrosis behave as tumors with 1 grade level higher (Am J Surg Pathol 2013;37:311)
- If patient has undergone presurgical renal embolization, tumor necrosis cannot be assessed
- Margin status
- In radical nephrectomy specimens, margins include ureter, major vessels (renal vein, renal artery) and soft tissue (Gerota fascia, renal sinus)
- Regional lymph nodes
- Regional lymphadenectomy is not performed in radical nephrectomies; however, a lymph node search during gross examination is recommended with a focus at the renal hilum
- Lymph nodes are found in < 10% of radical nephrectomy specimens (Am J Surg Pathol 2013;37:1505)
- Additional findings in nonneoplastic kidney
- Examination of nonneoplastic renal parenchyma may reveal medical diseases and shed light on the risk of progressive renal disease in the contralateral kidney and opportunities for medical intervention (Am J Surg Pathol 2006;30:575, Arch Pathol Lab Med 2009;133:1012, Semin Nephrol 2020;40:69)
- Refer to the most up to date version of WHO for tumor classifications (Pathologica 2022;115:8) (see WHO classification)
Features to report by organization
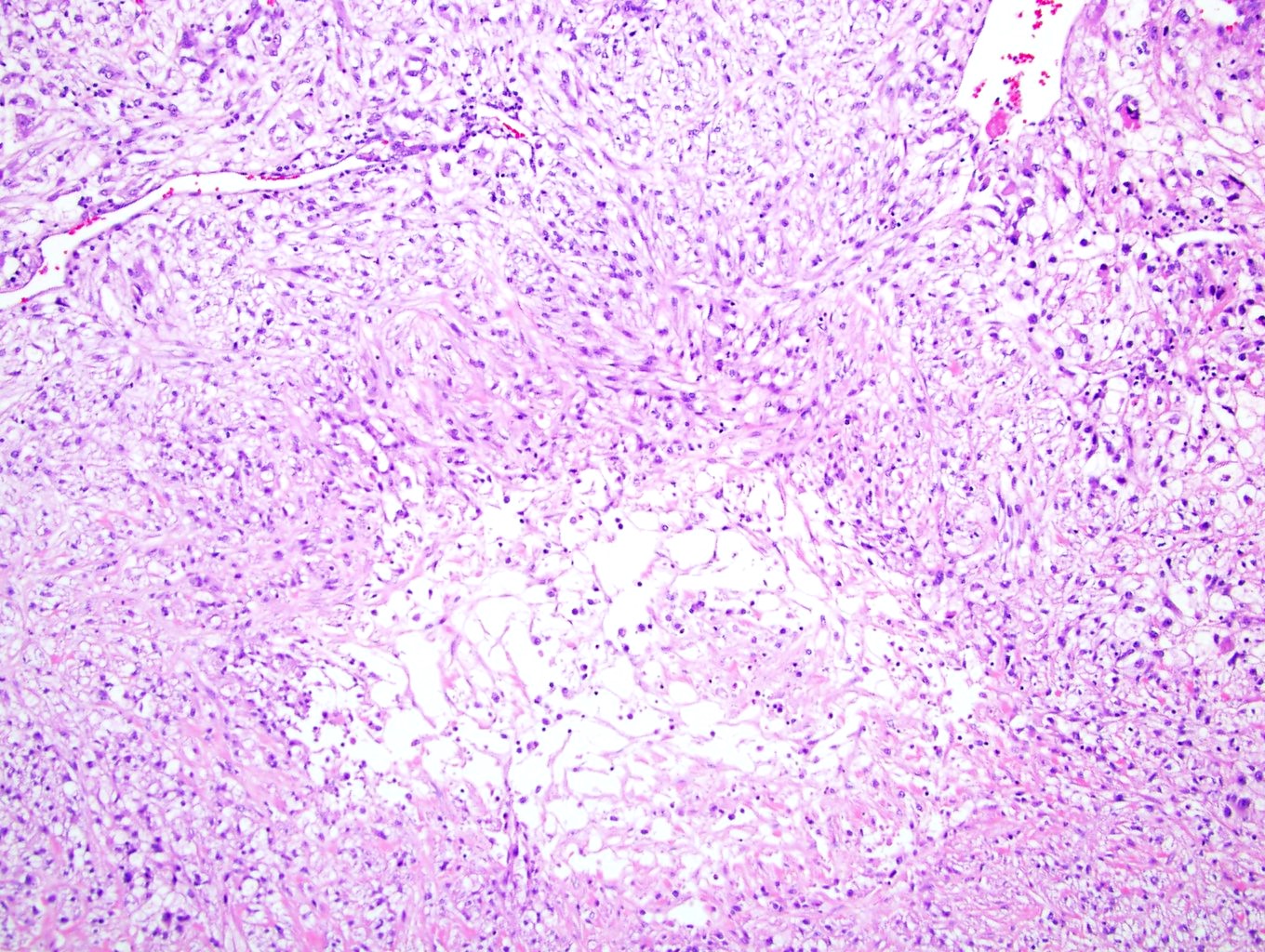
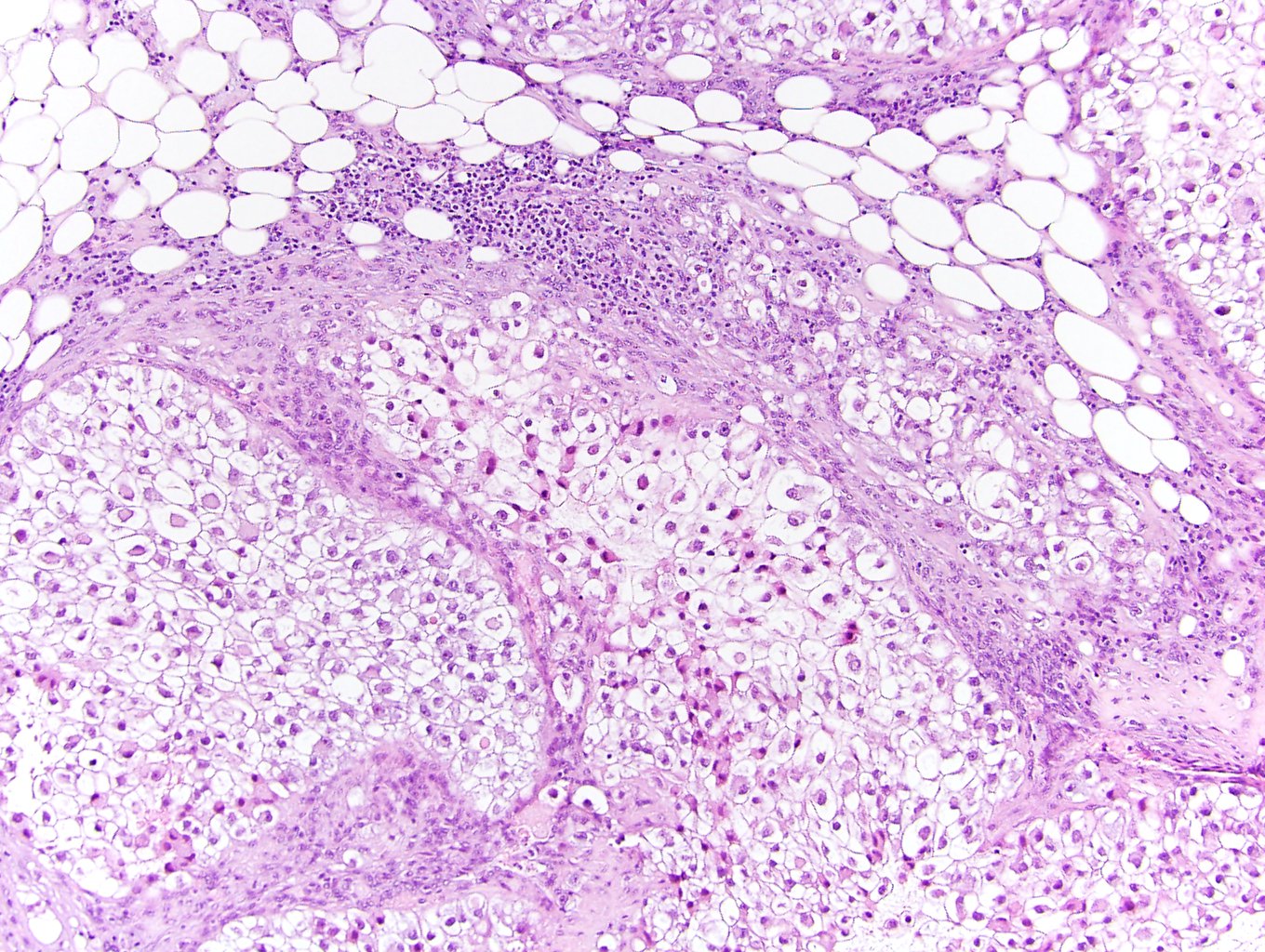
Microscopic (histologic) images
Sample pathology report
- Left kidney, radical nephrectomy:
- Clear cell renal cell carcinoma, grade 3 (see synoptic report)
Board review style question #1
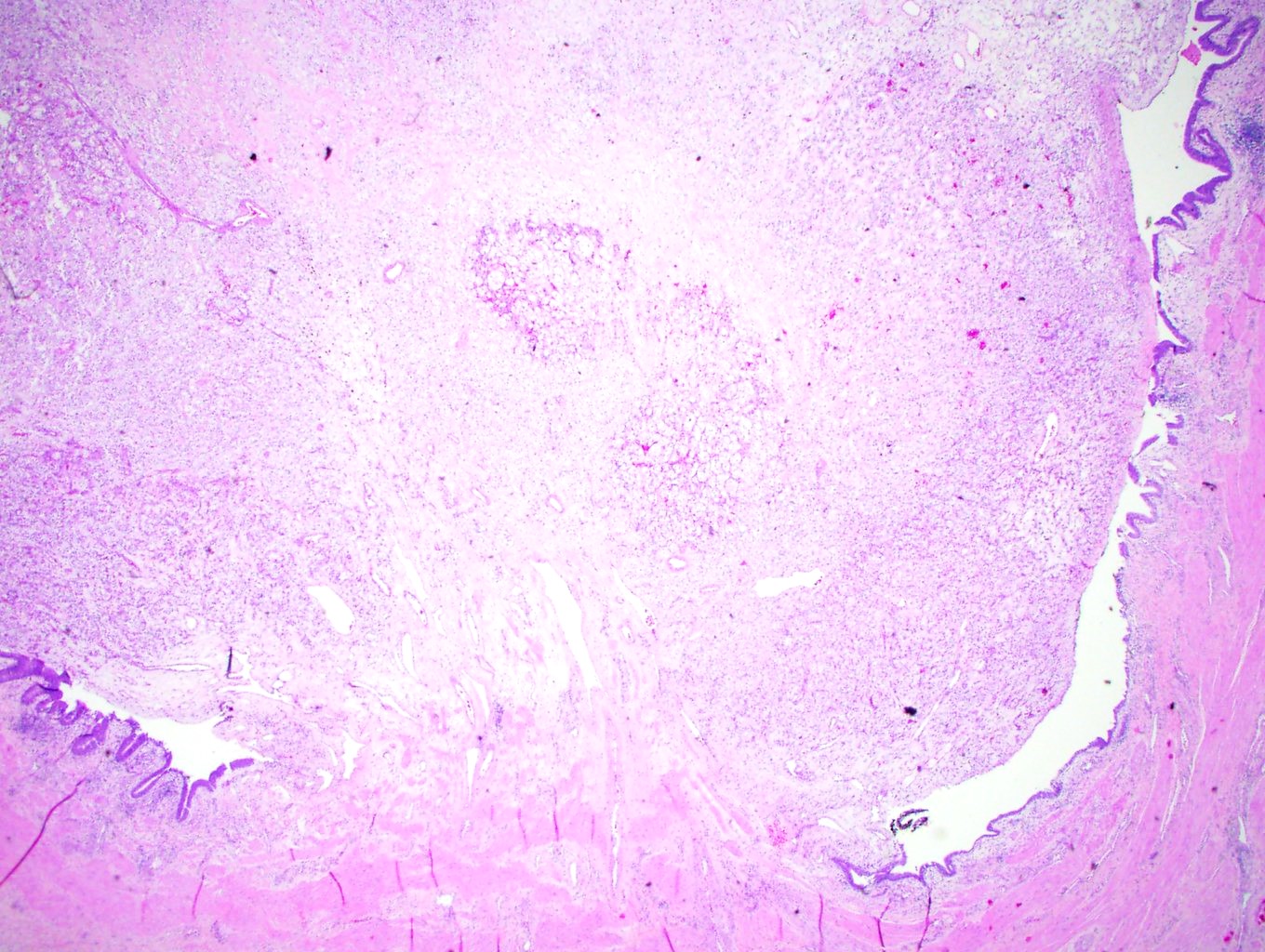
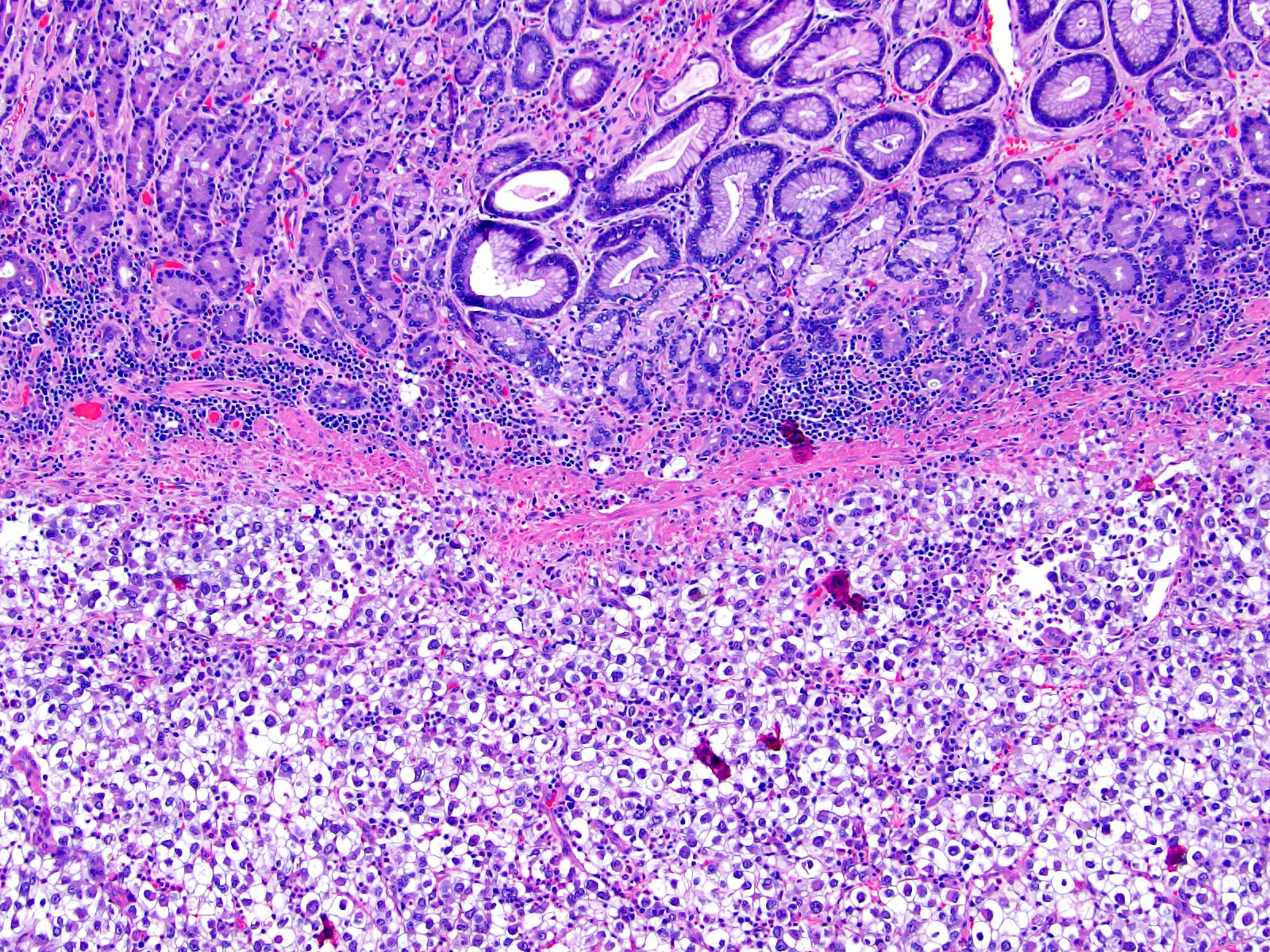
This patient (image shown above) has clear cell renal cell carcinoma with involvement of the adrenal gland. How would you classify this?
- Either pM1 (separate metastatic nodule in the adrenal gland) or pT4 (direct tumor extension to the adrenal gland)
- Neither pM1 (separate metastatic nodule in the adrenal gland) nor pT4 (direct tumor extension to the adrenal gland)
- pM1 (direct tumor extension to the adrenal gland)
- pT4 (separate metastatic nodule in the adrenal gland)
Board review style answer #1
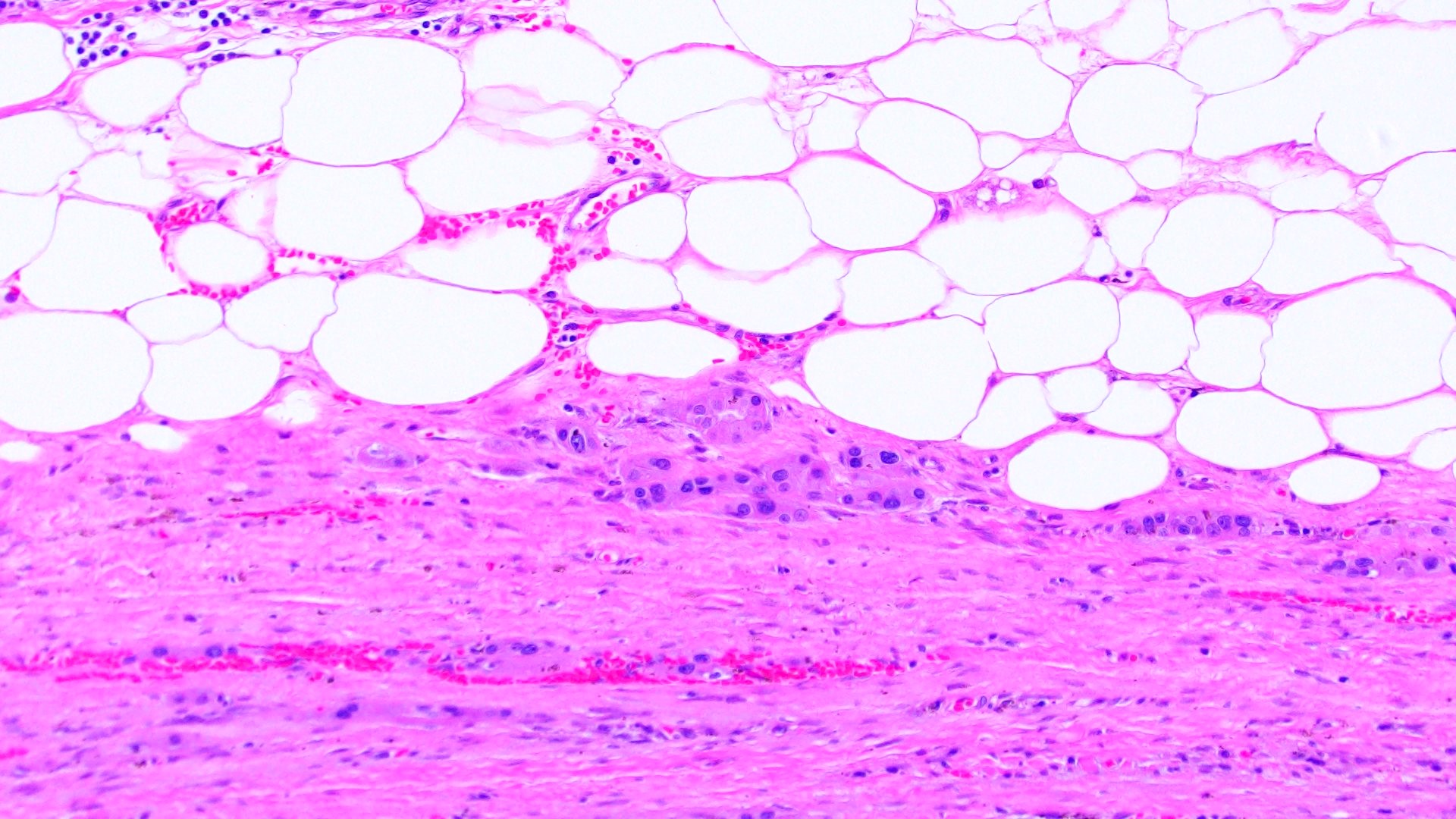
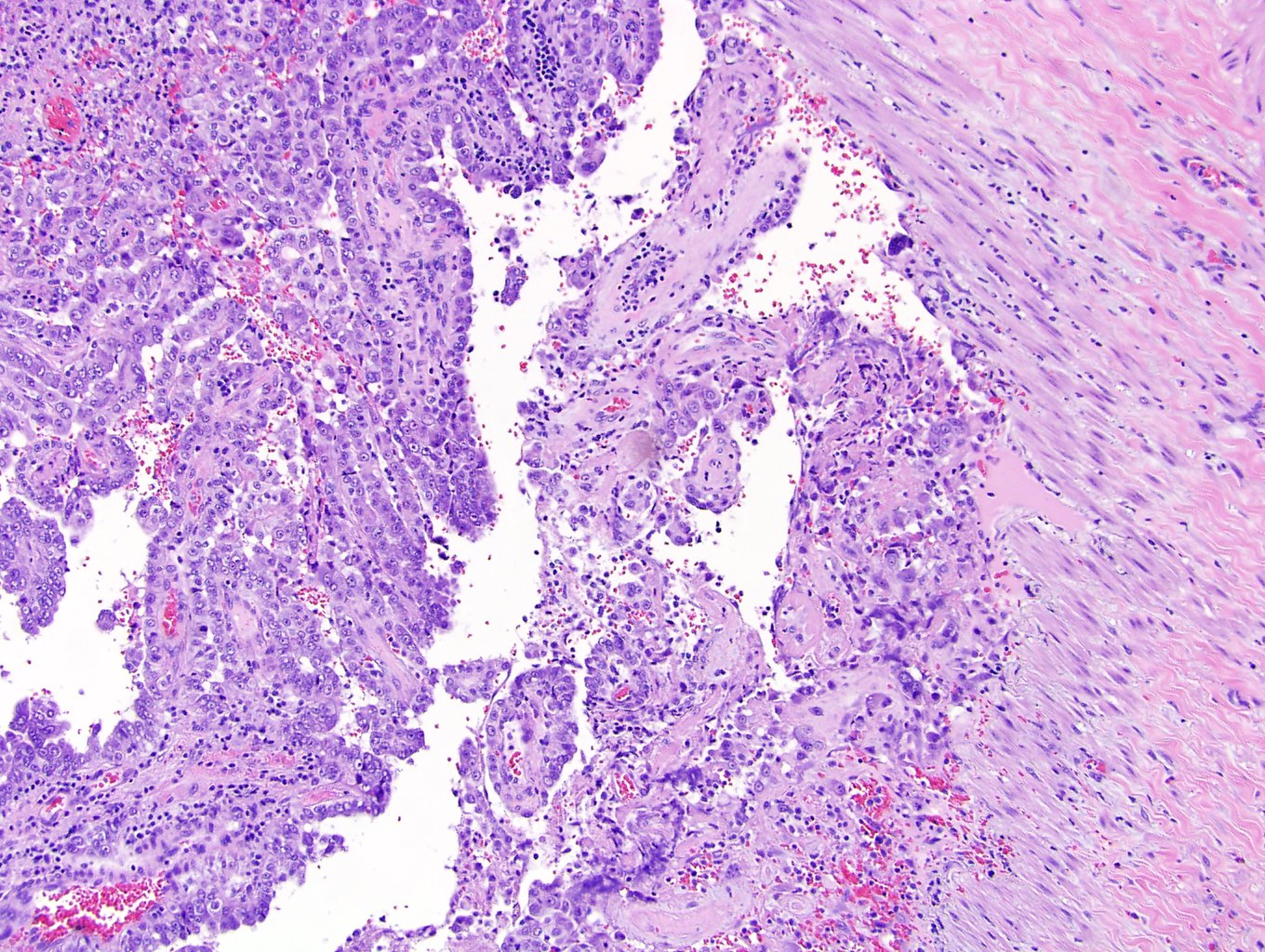
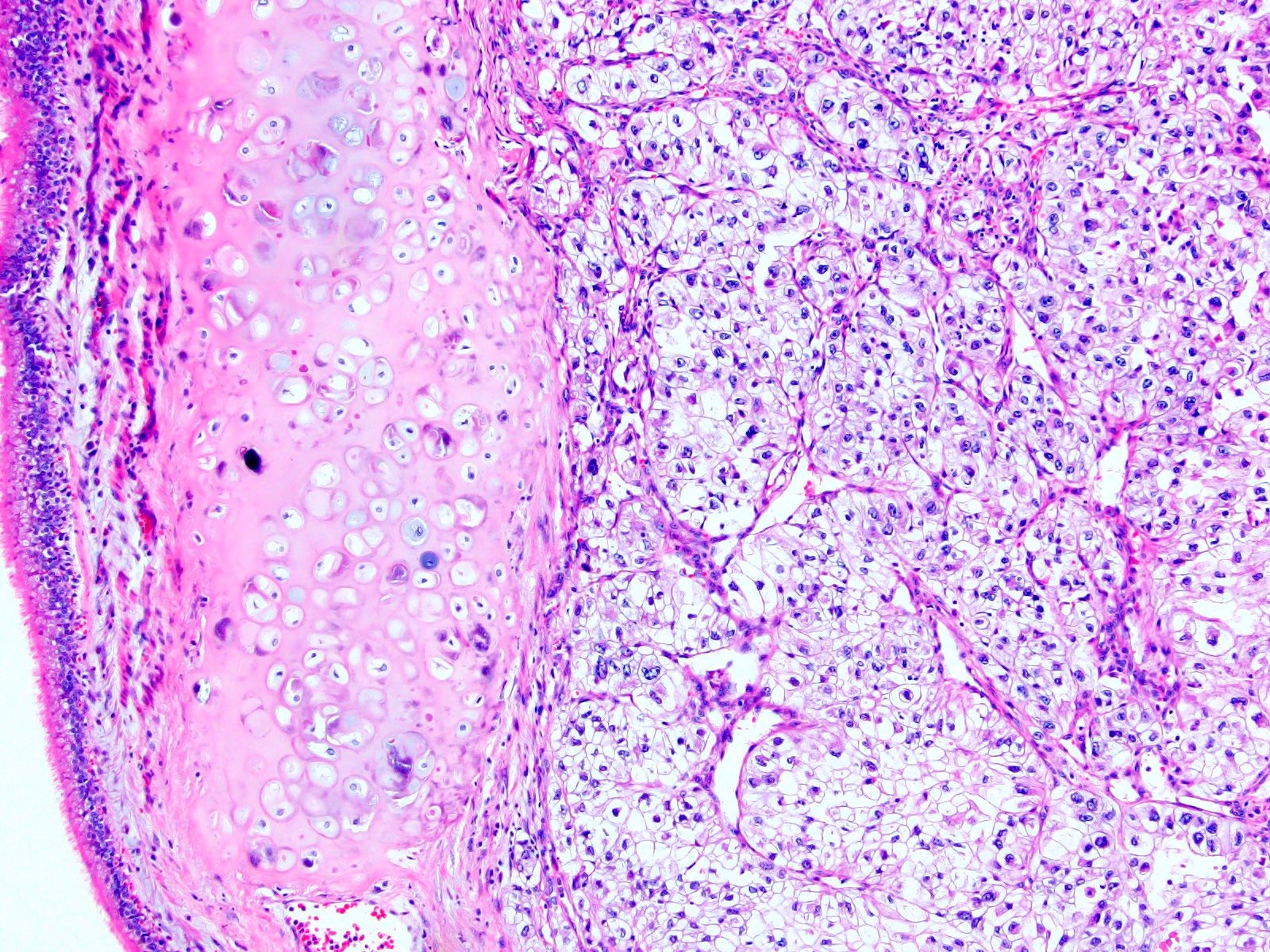
A. Either pM1 or pT4. This photomicrograph depicts clear cell renal cell carcinoma with residual adrenal cortex (bottom periphery). The determination of whether to classify the tumor as pT4 versus pM1 is based on the gross findings, which are not able to be discerned based on this picture. Answer C is incorrect because tumor extending from the superior pole of the kidney, through the perinephric fat and into the adrenal is consistent with pT4, not pM1. Answer D is incorrect because absence of tumor extending from the superior pole of the kidney, through the perinephric fat and into the adrenal is consistent with pM1, not pT4.
Comment Here
Reference: Kidney tumor - Features to report
Comment Here
Reference: Kidney tumor - Features to report
Board review style question #2
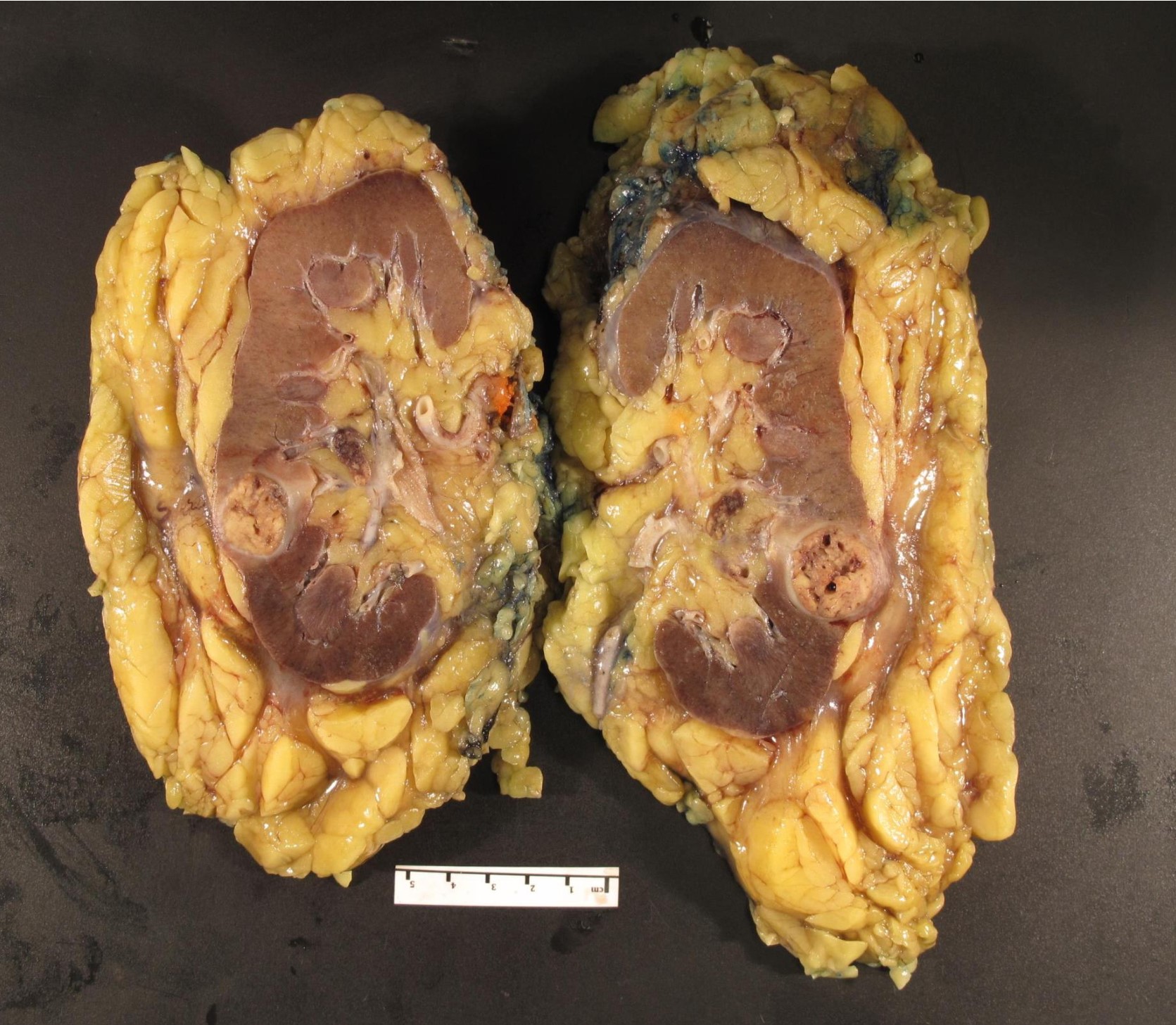
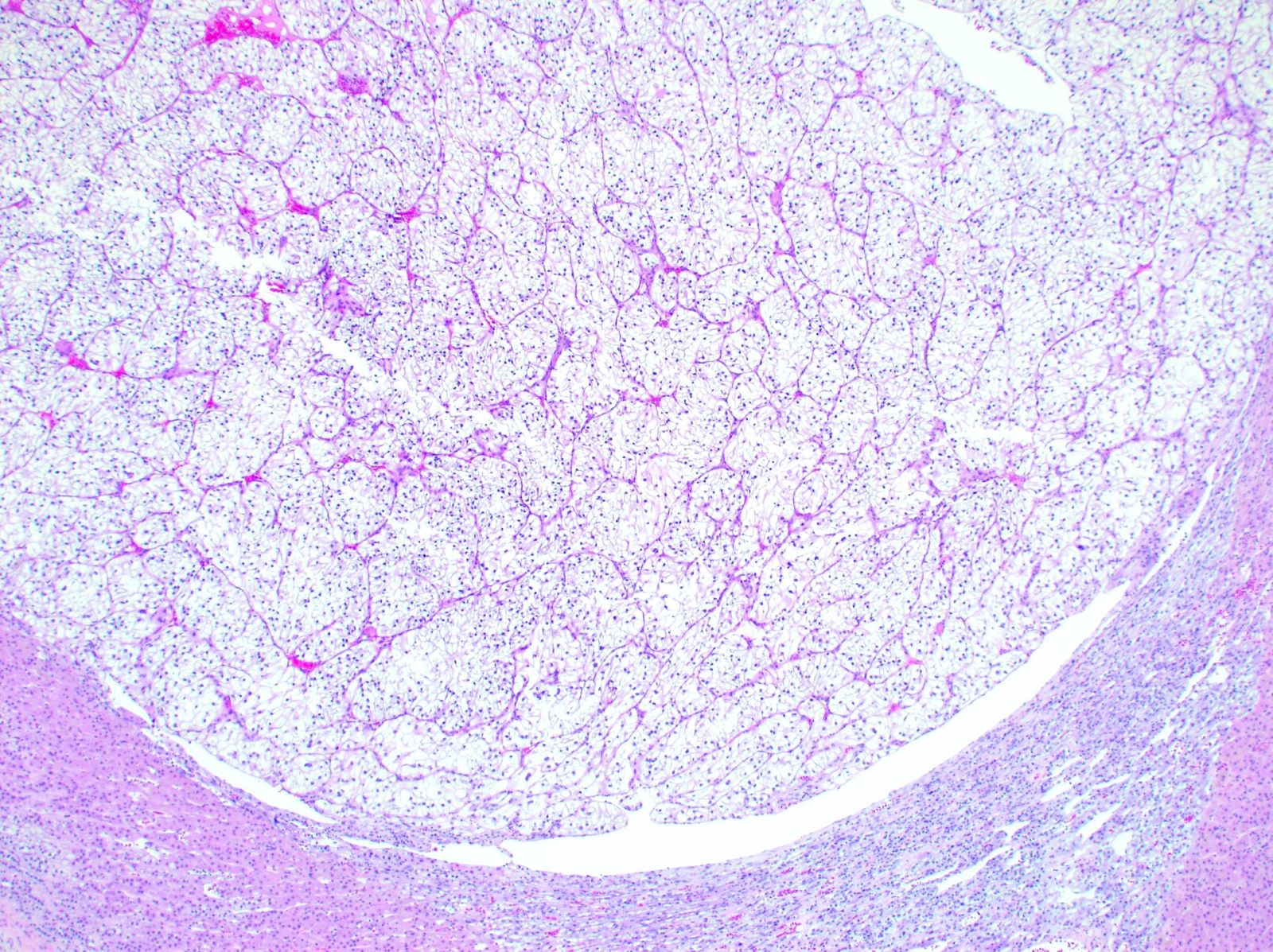
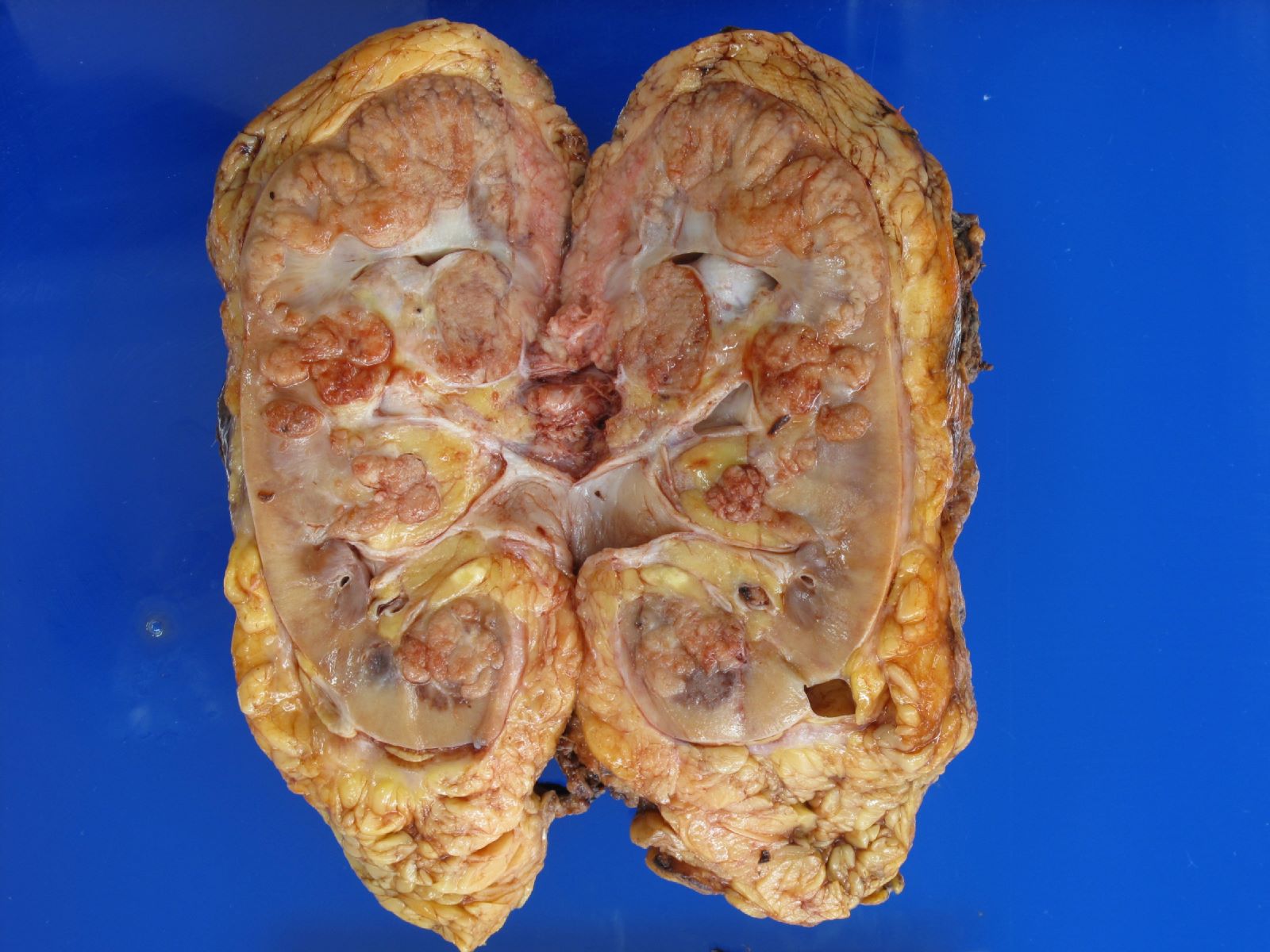
Which one of the following options is most likely to be true for the image of a nephrectomy specimen containing renal cell carcinoma shown above?
- pT2a with size of dominant tumor nodule > 7 cm but ≤ 10 cm
- pT2b with aggregate tumor size > 10 cm
- pT3a multifocal tumor with likely retrograde spread via renal vein and its segmental branches
- pT4 tumor invading into Gerota fascia
Board review style answer #2
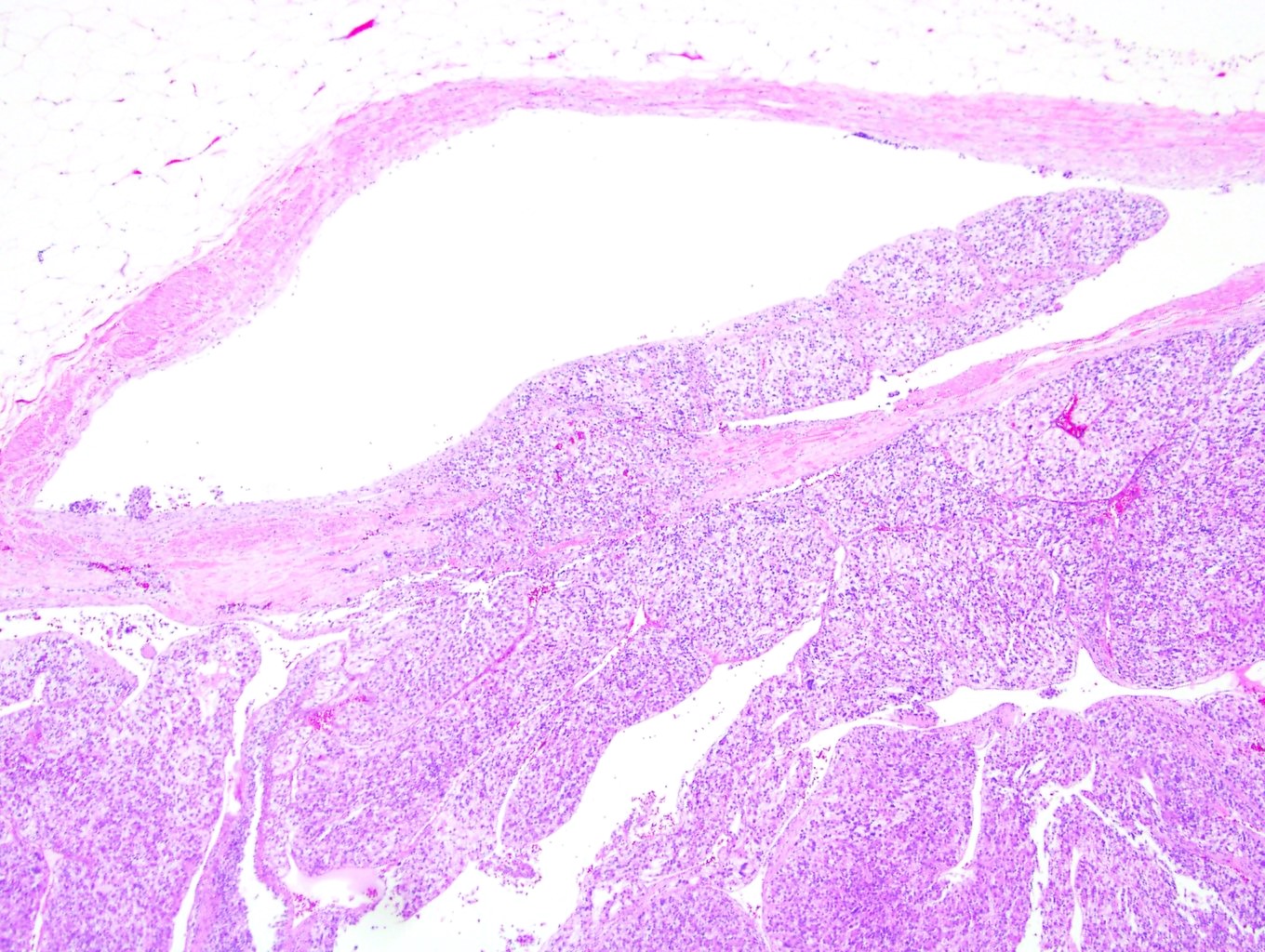
C. This is a pT3a multifocal tumor with likely retrograde spread via renal vein and its segmental branches. Multifocality and multinodularity are a frequent sign of intravenous renal cell carcinoma spread, with complete filling of the vascular lumina. As intravenous nodules enlarge, they can merge with the primary tumor, leading them to be falsely included in the measurement of the primary tumor size if the process of venous invasion is not recognized. Recognizing venous involvement is best assessed during gross examination when the kidney is bivalved. In a multifocal tumor, the gross examination should include assessing the size of each nodule separately (not aggregate size). Answers A and B for organ confined disease are incorrect because this tumor is locally invasive, extending to renal sinus and renal veins / branches. Answer D is incorrect because this tumor is surrounded by perinephric adipose tissue with intact Gerota fascia.
Comment Here
Reference: Kidney tumor - Features to report
Comment Here
Reference: Kidney tumor - Features to report