Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Anderson D, Tretiakova M. Primary thyroid-like follicular. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumormalignantprimarythyroidlike.html. Accessed April 2nd, 2025.
Definition / general
- Rare kidney tumor that morphologically mimics well differentiated thyroid follicular neoplasms
- Considered an emerging / provisional entity (Am J Surg Pathol 2018;42:1585, Transl Androl Urol 2021;10:1506, Mod Pathol 2021;34:1167)
Essential features
- Extremely uncommon (~40 cases reported)
- Resembles well differentiated thyroid follicular neoplasms
- Encapsulated mass with thyroid-like follicles (macro and microfollicles) containing inspissated, eosinophilic colloid-like material
- Negative for TTF1 and thyroglobulin
- Most have low malignant potential
Terminology
- Thyroid-like follicular renal cell carcinoma
ICD coding
- ICD-10: C64.9 - malignant neoplasm of unspecified kidney, except renal pelvis
Epidemiology
- Predominance in women (2:1)
- Age range between 10 - 83 years, with mean age of 41 - 44.5 years (Am J Surg Pathol 2009;33:393, Pathology 2018;50:24, Mod Pathol 2021;34:1921)
- Median age: 35 years (Transl Androl Urol 2021;10:1506)
- ~10% of patients had concurrent or historical hematopoietic neoplasia (Pathology 2018;50:24)
Sites
- Renal cortex
Clinical features
- Asymptomatic and found incidentally in most but may be symptomatic (hematuria, flank pain, abdominal pain) in up to 33% of patients (Pathology 2018;50:24)
Diagnosis
- Diagnosis is made primarily on H&E (see Essential features and Microscopic description)
- Essentially a diagnosis of exclusion; adequate sampling should be applied and immunohistochemistry could be considered, if clinically indicated, to exclude morphologic mimics (see Differential diagnosis)
Radiology description
- Typically solid, low attenuation mass without measurable postcontrast enhancement, metastatic disease or renal involvement
- May contain calcifications and possible necrosis
- Corresponding lack of thyroid mass suggestive of primary thyroid-like follicular renal cell carcinoma over metastatic thyroid carcinoma
- References: Case Rep Pathol 2013;2013:687427, Mol Clin Oncol 2016;4:143, Medicine (Baltimore) 2016;95:e3314
Radiology images
Prognostic factors
- Majority appear to have low malignant potential (Am J Surg Pathol 2009;33:393)
- Aggressive cases have been described with ~10% metastases and 13% of cases invading perinephric tissues (Hum Pathol 2011;42:146, Medicine (Baltimore) 2016;95:e3314, Pathology 2018;50:24)
- Rare cases have reported spread to lymph nodes and distant metastasis, including to skull, meninges and lung but all patients survived after surgical resection (Transl Androl Urol 2021;10:1506, Pathology 2018;50:24)
Case reports
- 10 year old girl with thyroid-like follicular renal cell carcinoma (Int Braz J Urol 2019;45:834)
- 32 year old woman with immunohistochemical and genetic analysis (Am J Surg Pathol 2006;30:411)
- 34 year old woman with metastasis to lungs and retroperitoneal lymph nodes (Hum Pathol 2011;42:146)
- 47 year old man with bilateral renal tumors of different subtypes, including thyroid-like follicular of the right kidney (Front Oncol 2021;11:659706)
- 48 year old woman with primitive small round / spindle cell sarcomatoid differentiation and metastatic disease (Int J Surg Pathol 2019;27:678)
- 68 year old woman with skull and meningeal metastasis (Medicine (Baltimore) 2016;95:e3314)
Treatment
- Partial or radical nephrectomy
Gross description
- Solitary mass, 1 - 16.5 cm (mean 4.7 cm) (Mod Pathol 2021;34:1167)
- Well circumscribed with solid to cystic cut surface; may show areas of hemorrhage and necrosis but not typical (Mod Pathol 2021;34:1921, Pathology 2018;50:24)
- Tan to brown in color; some tumors have been described as yellow or gray (Pathology 2018;50:24)
Gross images
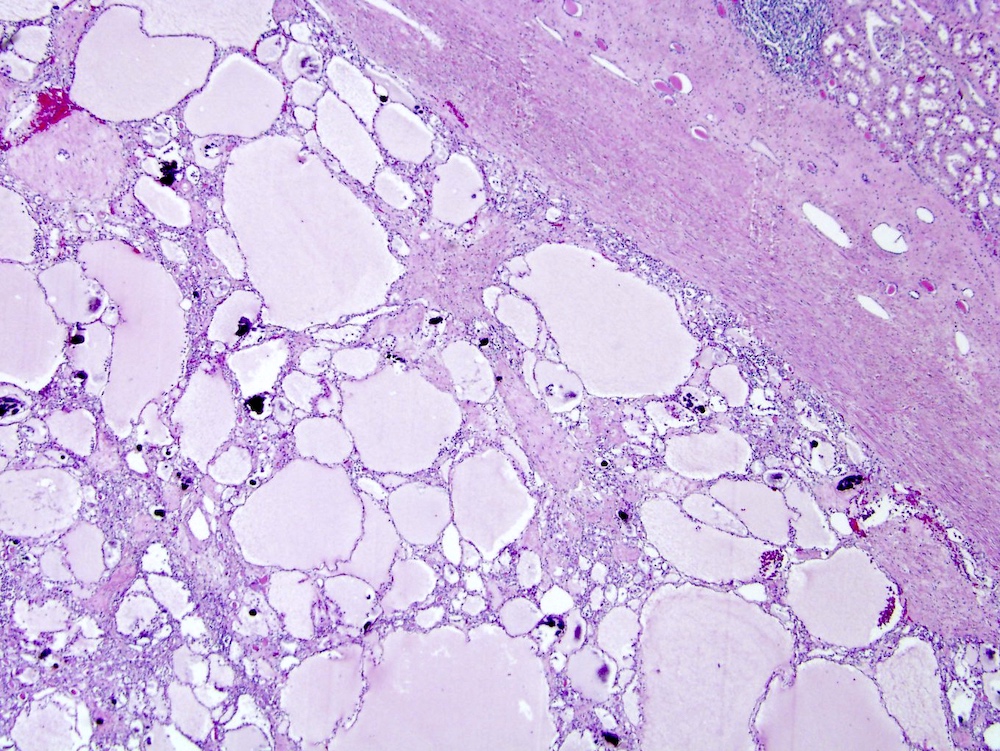
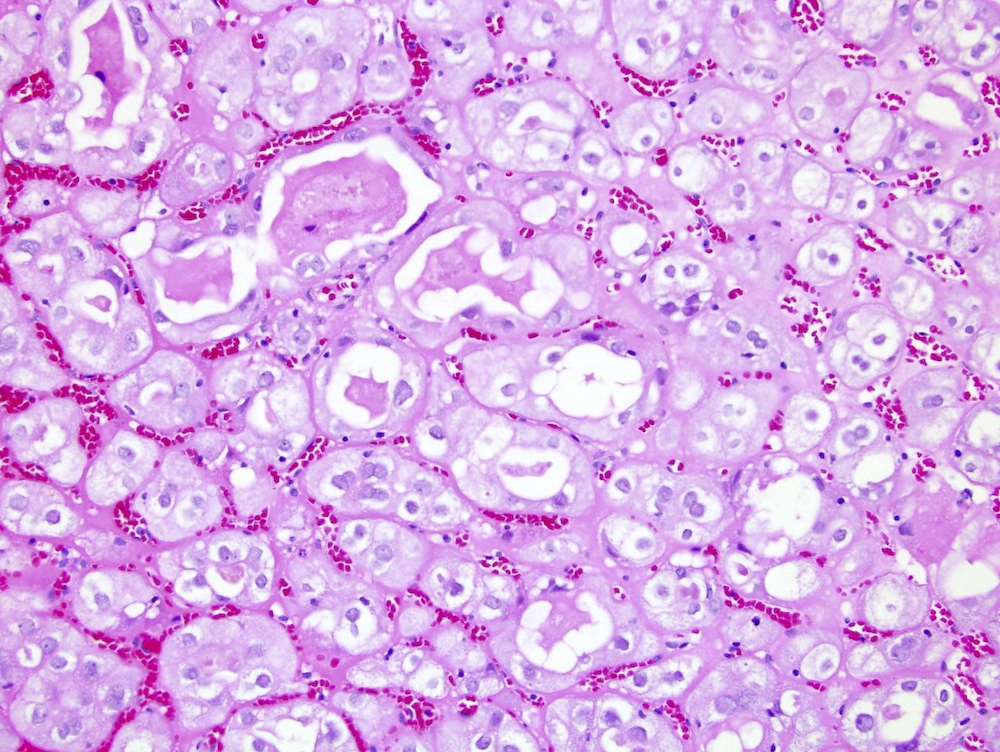
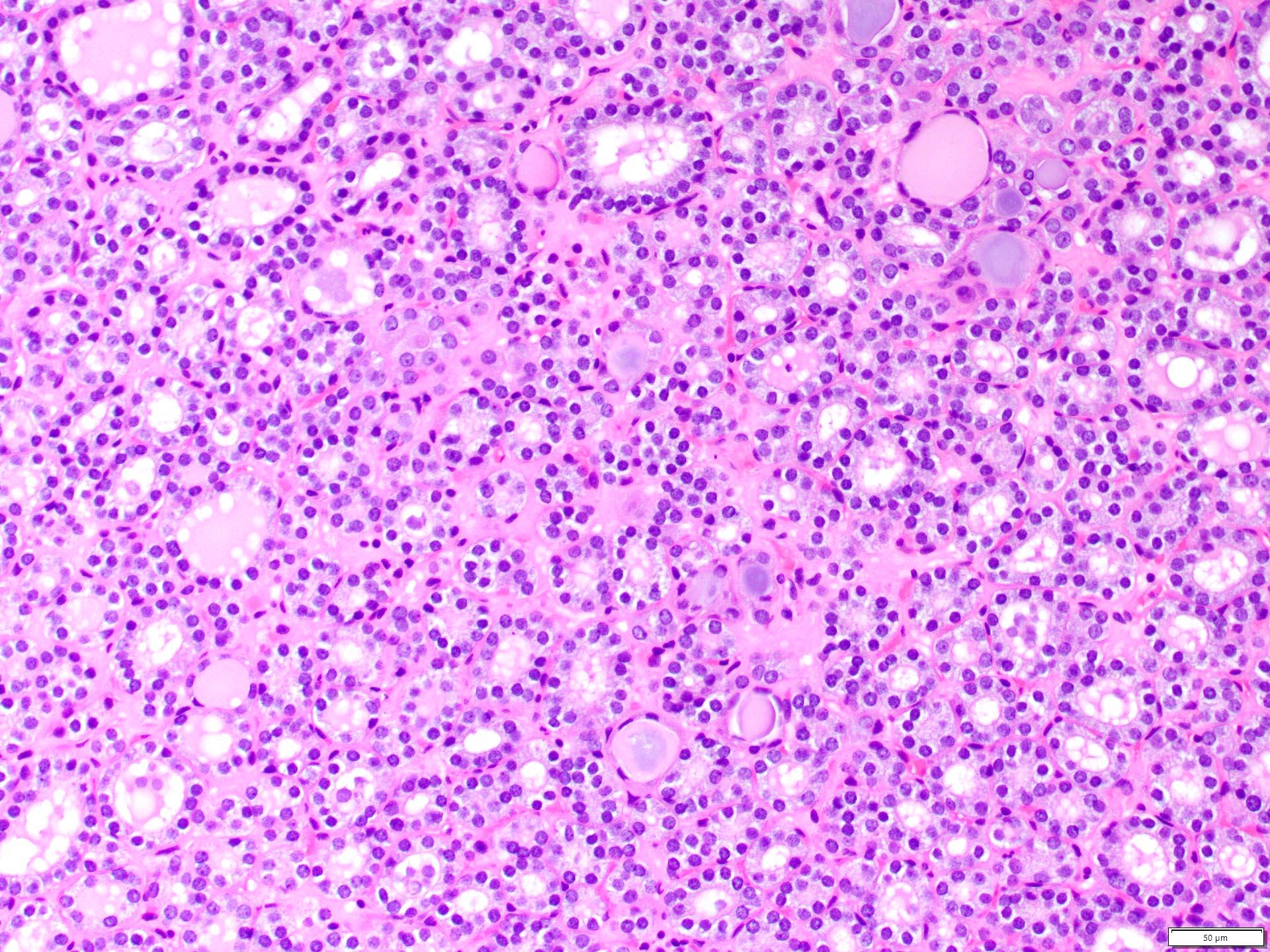
Microscopic (histologic) description
- Follicular-like architecture with variably sized follicles, with micro and macrofollicles, containing inspissated, eosinophilic colloid-like material
- Follicles are lined by a single layer of cuboidal or low columnar epithelium with moderate amphophilic to eosinophilic cytoplasm, round nuclei, mostly inconspicuous to occasionally prominent nucleoli
- Majority of tumors show pure follicular architecture, with some variations including branching, resulting in focal papillary-like pattern (Mod Pathol 2021;34:1167)
- Papillary areas appear to be broken interfollicular septa rather than true papillae (Pathology 2018;50:24)
- May be cystically dilated (Diagn Pathol 2014;9:186)
- May have focal tightly packed follicles without secretions, imparting a somewhat solid appearance
- Few cases demonstrate nuclear grooves or ground glass nuclear appearance (Pathology 2018;50:24)
- Lymphocytic infiltrate may be present intratumorally or around periphery and macrophages may be present in background (Diagn Pathol 2013;8:108)
- Calcifications may be seen (Pathology 2018;50:24)
- Necrosis and lymphovascular invasion are absent in most tumors
- Sarcomatoid differentiation has been reported (Int J Surg Pathol 2019;27:678, Int J Surg Pathol 2021;29:327, Histopathology 2022;80:745)
Microscopic (histologic) images
Cytology description
- May be hypercellular and arranged in sheets (Diagn Cytopathol 2014;42:273)
- Presence of acellular eosinophilic material is associated with the neoplastic epithelial cells in the background of the smear
- Individual tumor cells may be oval, round and plasmacytoid with mild nuclear pleomorphism, finely stippled nuclear chromatin and inconspicuous nucleoli with a moderate amount of eosinophilic cytoplasm and rare nuclear grooves (Diagn Cytopathol 2014;42:273, Diagn Pathol 2013;8:108)
Positive stains
Negative stains
- Thyroglobulin, TTF1
- May be negative but focal to variable reactivity has been reported for RCC (14%), AMACR (17%), CD10 (23%), CK20 (40%) (Mod Pathol 2021;34:1167)
- Typically negative for CD56, WT1 (Zhou: Uropathology - A Volume in the High Yield Pathology Series, 1st Edition, 2012, Mod Pathol 2021;34:1921)
- Other reports claim carcinoembryonic antigen, CK7, CD15, CK19, CK 34 beta E12 and epithelial membrane antigen are typically negative (Am J Surg Pathol 2006;30:411)
Molecular / cytogenetics description
- In 3 of 3 tumors tested in one study, an in frame fusion of exon 8 of EWSR1 and intraexonic of PATZ1, both on chromosome 22, were detected by RNA sequencing and confirmed with reverse transcription PCR; per authors, other approaches instead of FISH may be preferable to detect the EWSR1::PATZ1 fusion (Mod Pathol 2021;34:1921, Histopathology 2022;80:745)
- Gene expression profile is distinct from clear cell and chromophobe renal cell carcinoma
- Amin et al. reported overexpression in cell cycle regulatory genes and mixed lineage leukemia (MLL) / trithorax homolog in 3 tumors; however, comparative genetic hybridization failed to reveal cytogenetic alterations in one study (Am J Surg Pathol 2009;33:393)
- Another study showed chromosomal gains of 7q36, 8q24, 12, 16, 17p11-q11, 17q24, 19q, 20q13, 21q22.3 and Xp and losses of 1p36, 3 and 9q21-33 detected by comparative genomic hybridization (Am J Surg Pathol 2006;30:411)
Sample pathology report
- Right kidney, partial nephrectomy:
- Thyroid-like follicular renal cell carcinoma (2.2 cm) (see synoptic report and comment)
- Comment: The tumor cells are positive for PAX8, CK7 and are negative for TTF1, thyroglobulin and WT1.
Differential diagnosis
- Follicular architecture is not unique to thyroid-like follicular renal cell carcinoma (RCC) and may be seen in other RCC subtypes, such as papillary RCC, clear cell RCC, FH deficient RCC, tubulocystic RCC, SDHB deficient RCC, microcystic chromophobe RCC, atrophic kidney-like tumor / lesion (provisional entity) and mixed epithelial and stromal tumor (Mod Pathol 2021;34:1167, Am J Surg Pathol 2018;42:1585)
- Papillary RCC:
- Will demonstrate ordinary papillary renal cell carcinoma areas
- Atrophic kidney-like tumor / lesion (provisional entity):
- Atrophic / flattened epithelium with occasional hobnailing within follicles, more pronounced microcalcifications, entrapped benign atrophic renal tubular structures and morphologic similarity to glomerulocystic change
- Will demonstrate WT1 positive / PAX8 negative / CK7 negative IHC profile (Mod Pathol 2021;34:1921, Am J Surg Pathol 2018;42:1585)
- Metastatic thyroid carcinoma (Case Rep Pathol 2015;2015:701413, Mol Clin Oncol 2021;15:268):
- Very rare to have metastatic disease to kidney; usually obvious thyroid primary with widely disseminated metastases
- Thyroglobulin+ or TTF1+
- Most follicular and follicular variant of papillary thyroid carcinomas have RAS or BRAF mutations, respectively (Mod Pathol 2021;34:1921)
- Thyroid carcinomas can have a Hürthle (oncocytic) phenotype, which could be a potential pitfall for eosinophilic / oncocytic renal neoplasms; these more commonly metastasis to the lung and bone (Thyroid 2010;20:429, Nucl Med Mol Imaging 2017;51:256)
- Metastatic follicular carcinoma arising in struma ovarii in women:
- If this metastasizes, usually goes to bone (Pathologica 2020;112:224, Int J Gynecol Pathol 2009;28:405, J Clin Neurosci 2010;17:269)
- Chronic pyelonephritis and end stage kidney disease:
- May be considered due to presence of colloid-like hyaline casts in atrophic, microcytic tubules resembling thyroid (thyroidization)
- Differentiated by clinical history, lack of mass formation and histologic differences (inflammation, demonstration of normal constituents, such as glomeruli and tubules, with chronic injury pattern resulting in fibrosis, atrophy, etc.)
- Well differentiated neuroendocrine tumor (carcinoid):
- Rare
- Patterns are insular, cords, nests or ribbons but not follicular
- Neuroendocrine histology
- Positive for neuroendocrine markers synaptophysin and chromogranin
- Urothelial carcinoma with cystitis cystica pattern:
- Arises from the renal pelvis
- GATA3 positivity (Mod Pathol 2021;34:1921)
- Oncocytoma:
- Areas of classical oncocytoma with nests of oncocytic cells embedded in loose myxoid stroma
Additional references
Board review style question #1
A 42 year old woman undergoes a left radical nephrectomy for a 4 cm renal mass. Which of the following is most consistent with a diagnosis of thyroid-like follicular renal cell carcinoma?
- Grossly well circumscribed renal tumor with microscopic follicular growth and inspissated colloid-like material
- Immunohistochemistry demonstrates tumor cells to be negative for PAX8 and CK7 and positive for WT1
- Poor clinical prognosis after diagnosis with high mortality rate
- Will demonstrate NRAS and HRAS or BRAF mutations by sequencing
Board review style answer #1
A. Grossly well circumscribed renal tumor with microscopic follicular growth and inspissated colloid-like material. Thyroid-like follicular renal cell carcinoma usually presents asymptomatically over a wide age range with female predominance. On gross, the tumor is well circumscribed tan to brown, solid to cystic mass. Microscopically, it demonstrates follicular-like architecture with micro and macrofollicles, filled with inspissated colloid-like material. The follicles are lined by cuboidal cells with moderate amount of amphophilic to eosinophilic cytoplasm, oval nuclei with uniform chromatin and inconspicuous nucleoli. This entity typically has an indolent clinical behavior. Immunohistochemical profile is typically PAX8+ / CK7+ / WT1- / TTF1- / thyroglobulin-, in contrast to atrophic kidney-like tumor / lesion and metastatic thyroid carcinoma, the 2 closest morphologic mimics. The tumor will be negative for NRAS, HRAS and BRAF mutations, in contrast to metastatic thyroid carcinoma.
Comment Here
Reference: Primary thyroid-like follicular carcinoma
Comment Here
Reference: Primary thyroid-like follicular carcinoma
Board review style question #2
A 65 year old woman undergoes a right radical nephrectomy for a 3 cm renal mass. The tumor displays follicular architecture with inspissated colloid-like material without papillary-like nuclear features or papillary growth. By immunohistochemistry, the tumor cells are positive for TTF1 and thyroglobulin. This patient will likely have which of the following?
- An intact thyroid with no nodules
- No evidence of other metastatic foci on PET / CT
- PAX8 IHC negativity
- RAS mutation
Board review style answer #2
D. RAS mutation. The question describes a metastatic follicular carcinoma of the thyroid. These patients will typically have evidence of prior thyroid surgery or an obvious thyroid primary with widely metastatic disease. The most common somatic mutations to occur in follicular thyroid carcinoma are RAS point mutations (most often codon 61 of NRAS and codon 61 of HRAS) followed by PPARG gene fusions (e.g., PAX8::PPARG). RAS mutations are found in almost half of conventional follicular carcinomas. They stabilize the protein in its active guanosine triphosphate (GTP) bound form, leading to constant stimulation of the downstream signaling pathways, particularly MAPK and PI3K / AKT cascades. Both metastatic thyroid-like follicular renal cell carcinoma and metastatic follicular carcinoma of the thyroid will demonstrate PAX8 positivity and therefore this stain should not be used to distinguish between these entities.
Comment Here
Reference: Primary thyroid-like follicular carcinoma
Comment Here
Reference: Primary thyroid-like follicular carcinoma