Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Abdelwahed R, Tretiakova M. Acquired cystic disease associated. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumormalignantacquiredcysticRCC.html. Accessed January 6th, 2025.
Definition / general
- Renal cell carcinoma (RCC) arising exclusively in patients with acquired cystic disease (ACD)
- Characterized by microcystic sieve-like, papillary and solid architecture, eosinophilic and clear cells and abundant calcium oxalate crystals (Am J Surg Pathol 2006;30:141)
Essential features
- Most common RCC in patients with ACD (Eur Urol 2016;70:93)
- Abundant intratumoral oxalate crystals
- Heterogenous morphology with mixed sieve-like, solid, microcystic, papillary architecture and eosinophilic to clear cells
Terminology
- Acquired cystic disease associated renal cell carcinoma (ACD-RCC)
ICD coding
- ICD-O: 8316/3 - acquired cystic disease associated renal cell carcinoma
- ICD-11: 2C90.0 & XH0RU3 - renal cell carcinoma of kidney, except renal pelvis & acquired cystic disease associated renal cell carcinoma
Epidemiology
- ACD typically occurs after dialysis for end stage renal disease (ESRD)
- Incidence of ACD progressively increases with duration of dialysis: from 10 - 20% after 3 years to > 90% after 10 years of hemodialysis or peritoneal dialysis
- Overall incidence of ACD-RCC is 3 - 7% in end stage kidney, which is 100 times greater than in the general population (Kidney Int 2002;61:2201)
- ACD-RCC is the most common RCC subtype in both ACD (40%) and ESRD (30%)
- Other tumors that occur in end stage kidneys include clear cell papillary renal cell tumors and clear cell, papillary and chromophobe RCCs
Sites
- Kidney
Pathophysiology
- Causes of increased tumorigenesis in end stage kidney and ACD are multifactorial, including
- Depressed humoral and cellular immunity in renal failure
- Increased production of reactive oxygen species and impaired antioxidant defense (Virchows Arch 2013;463:553)
- Use of immunosuppressive medications
- Oxalate crystals induced tubular proliferative activity (Arch Pathol Lab Med 2017;141:600)
Etiology
- See Pathophysiology
Clinical features
- ACD-RCC has overall indolent clinical behavior, likely because of early detection with periodic imaging of ESRD patients (Eur Urol 2016;70:93)
- 10 - 15% of tumors present with recurrence and metastases, commonly associated with sarcomatoid and rhabdoid phenotypes (Am J Surg Pathol 2006;30:141)
Diagnosis
- Majority are asymptomatic tumors detected incidentally on routine imaging (Eur Urol 2011;60:e35)
- A minority of patients present with microscopic hematuria or flank pain
Radiology description
- On computed tomography (CT) scan: well defined lesions of variable size, rounded and often exophytic
- Often isodense on nonenhanced exam; can be solid, cystic or mixed in attenuation on enhanced exam (Front Oncol 2023;13:1187495)
- May have numerous calcifications
Case reports
- 41 year old man and 46 year old woman with clear cell and papillary RCCs with abundant calcium oxalate crystals arising in acquired cystic disease of the kidney (Arch Pathol Lab Med 2003;127:E89)
- 56 year old man with sarcomatoid and rhabdoid change (Ann Diagn Pathol 2011;15:462)
- 58 year old man with PTCH1 mutation (Front Oncol 2024;14:1349610)
- 78 year old woman with sarcomatoid change (Histol Histopathol 2008;23:1327)
Treatment
- Standard treatment for ACD-RCC is nephrectomy, either partial or total
- Chemotherapeutic agents have not been evaluated specifically for ACD-RCC
- Imaging for masses or large cysts is recommended for patients with ESRD and frequent screening is recommended, especially after ≥ 10 years on dialysis (Nephrol Dial Transplant 2011;26:1677)
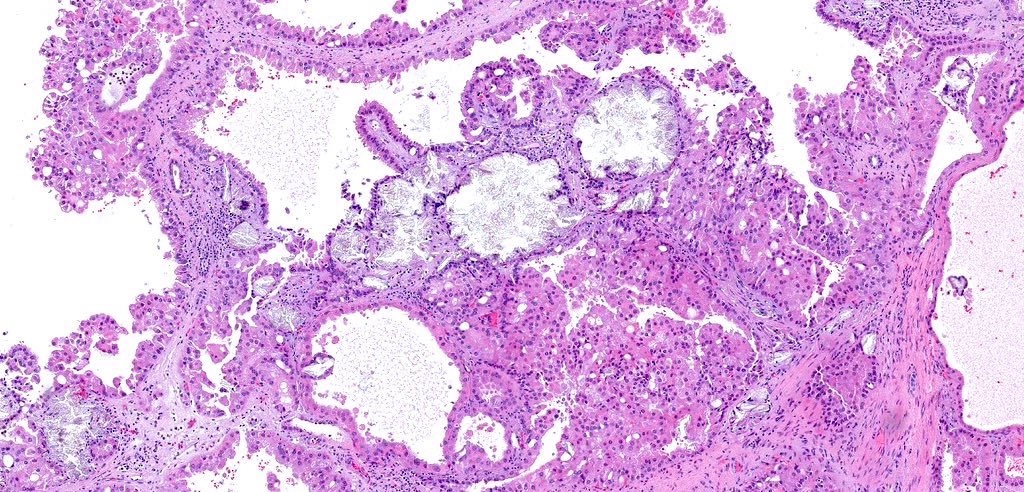
Gross description
- Mass lesion: usually ≤ 3 cm or less in ACD background of atrophic kidney with corticomedullary junctions obscured by diffuse, small cortical cysts
- Multifocal (~50%) and bilateral (~25%)
- May be found in association with atypical cysts, adenomas or additional neoplasms
- Generally circumscribed and often arises in a cyst; larger tumors with thick, fibrous capsules
- Brown to yellow cut surface with focal hemorrhage and necrosis (Eur Urol 2016;70:93)
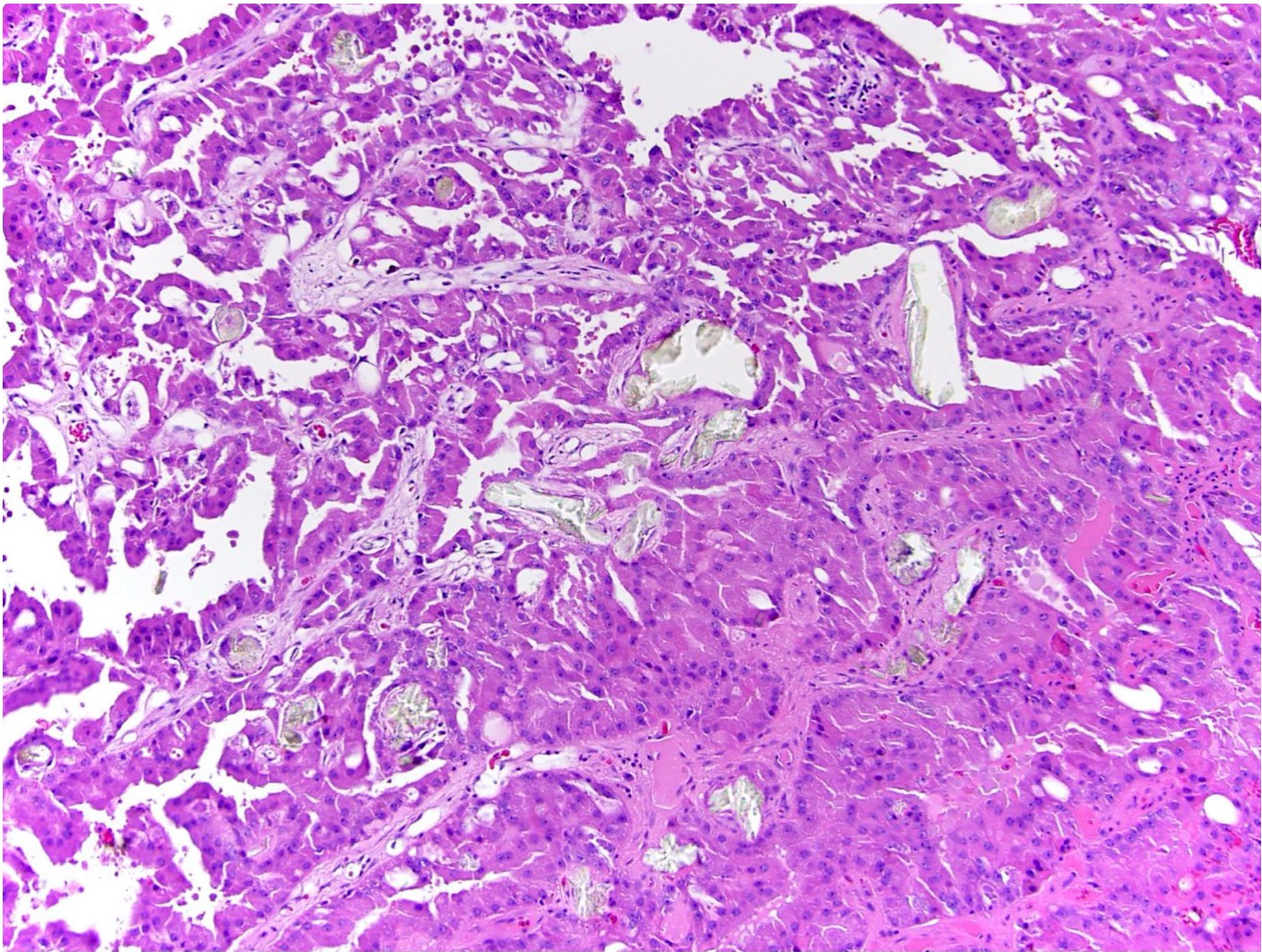
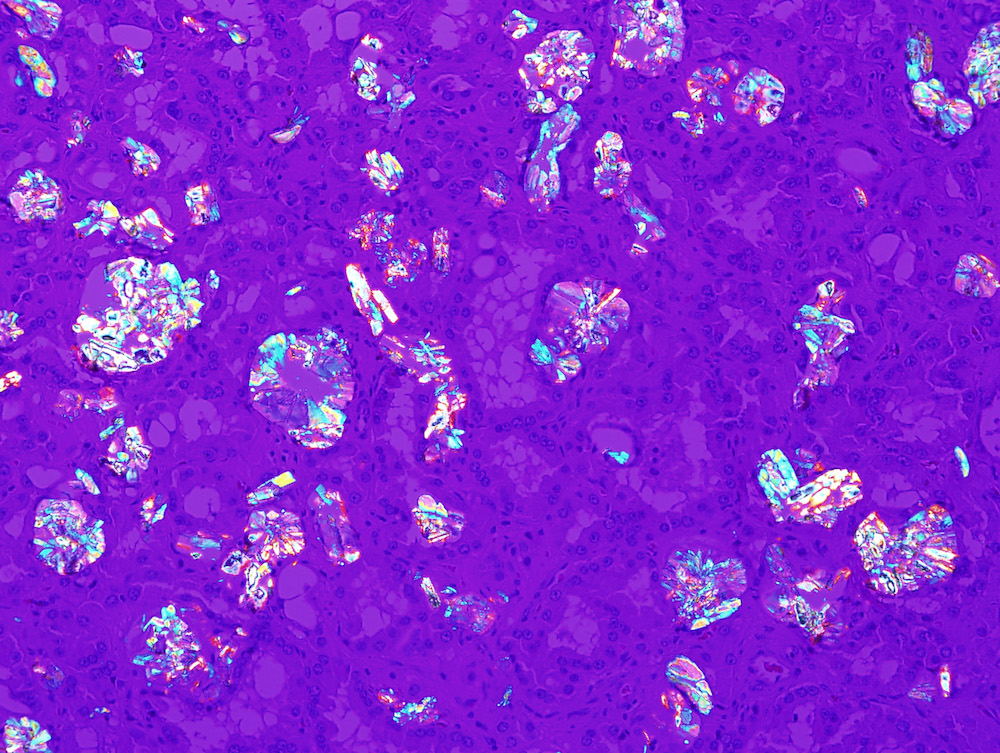
Microscopic (histologic) description
- Highly variable architecture: cribriform, microcystic, sieve-like, tubulopapillary and solid patterns
- Cells with large nuclei, prominent nucleoli and abundant granular eosinophilic cytoplasm with intracytoplasmic holes and intercytoplasmic lumina due to crystal depositions
- Intratumoral calcium oxalate crystals are very common but not necessary for diagnosis (Am J Surg Pathol 2005;29:443)
- May be nodules arising from cyst walls or solid masses separate from cysts (Am J Surg Pathol 2013;37:1469)
- Sometimes prominent clear cell cytology
Microscopic (histologic) images
Contributed by Nicole Andeen, M.D., Maria Tretiakova, M.D., Ph.D., Gregory T. MacLennan, M.D. and @katcollmd on Twitter
Cytology description
- Moderately cellular, papillary clusters of polygonal to columnar cells with abundant eosinophilic granular cytoplasm, round and central nuclei, finely granular chromatin, prominent central grade 3 nucleoli (Diagn Cytopathol 2008;36:344)
Positive stains
- PAX8, CD10, AE1 / AE3, RCC, AMACR (Mod Pathol 2006;19:780, Eur Urol 2016;70:93)
- Specific immunohistochemical profile is not required for diagnosis (Am J Surg Pathol 2013;37:1469)
Negative stains
Molecular / cytogenetics description
- Comparative genomic microarray and FISH studies reveal gains and losses of multiple chromosomes (Am J Surg Pathol 2013;37:1469)
- Gains of sex chromosomes and gains of 3, 7, 16, 17 (Eur Urol 2016;70:93)
- High prevalence of gains of Y, 3 and 16 distinguishes from papillary RCC, which also has gains in chromosomes 7 and 17 (Eur Urol 2016;70:93)
- Recurrent KMT2C or TSC2 gene mutations (Am J Surg Pathol 2020;44:1479)
Sample pathology report
- Right kidney, radical nephrectomy:
- Acquired cystic disease associated renal cell carcinoma with the following features (see cancer summary report and comment)
- Size: 2.5 cm in greatest dimension
- Tumor stage: organ confined (pT1a)
- Margins: all surgical margins are negative for carcinoma
- Background end stage kidney with acquired cystic disease
- Comment: Intramural oxalate crystals and background of cystic end stage kidney are characteristic of this diagnosis. Immunohistochemical stains are positive for CD10, AMACR and AE1 / AE3 and negative for CK7, supportive of this diagnosis.
- Acquired cystic disease associated renal cell carcinoma with the following features (see cancer summary report and comment)
Differential diagnosis
- Clear cell renal cell carcinoma:
- Both entities may have clear cells and nested architecture
- ACD-RCC has predominantly eosinophilic cells, variable cribriform, solid and papillary architecture, oxalate crystals and background cystic renal parenchyma
- CAIX is negative in ACD-RCC but positive in clear cell RCC
- Papillary renal cell carcinoma:
- Both entities may have papillary architecture and eosinophilic cells
- ACD-RCC has characteristic sieve-like architecture, oxalate crystals and background cystic renal parenchyma
- CK7 is usually negative in ACD-RCC but positive in papillary RCC
- Chromophobe cell renal cell carcinoma and oncocytoma:
- These tumors characterized by granular eosinophilic cells and solid architecture also observed in ACD-RCC but
ACD-RCC has characteristic sieve-like architecture, oxalate crystals and background cystic renal parenchyma
- CKIT is negative in ACD-RCC but positive in chromophobe RCC and oncocytoma
- These tumors characterized by granular eosinophilic cells and solid architecture also observed in ACD-RCC but
ACD-RCC has characteristic sieve-like architecture, oxalate crystals and background cystic renal parenchyma
Board review style question #1
What is the most helpful feature to distinguish the tumor captured on this image from other RCCs?
- Intratumoral oxalate crystals and background of end stage renal disease (ESRD) with cysts
- Presence of papillary architecture and eosinophilic cells
- Specific recurrent cytogenetic abnormality
- Unique immunohistochemical profile
Board review style answer #1
A. Intratumoral oxalate crystals and background of end stage renal disease (ESRD) with cysts are hallmark features of ACD-RCC. When present, these allow definitive diagnosis. Answer B is incorrect because papillary architecture and eosinophilic cells could be seen in multiple RCC subtypes. Answers C and D are incorrect because ACD-RCCs do not have specific immunoprofile and their molecular abnormalities overlap with other RCC entities.
Comment Here
Reference: Acquired cystic disease associated renal cell carcinoma
Comment Here
Reference: Acquired cystic disease associated renal cell carcinoma
Board review style question #2
Which of the following is true about acquired cystic disease associated renal cell carcinoma (ACD-RCC)?
- Aggressive tumors usually diagnosed at advanced stage
- CAIX can be used to differentiate it from clear cell RCC
- Intratumoral oxalate crystals are required to make the diagnosis
- The only tumor that arises in end stage kidney
Board review style answer #2
B. CAIX can be used to differentiate it from clear cell RCC. CAIX is positive in clear cell RCC but negative in acquired cystic disease associated RCC. Answer C is incorrect because acquired cystic disease associated RCC is commonly associated with intratumoral oxalate crystals but it is not required to make the diagnosis. Answer A is incorrect because these tumors are indolent and usually diagnosed early due to routine screening of patients with end stage kidney. Answer D is incorrect because other tumors can arise in end stage kidney and include clear cell papillary renal cell tumors, clear cell, papillary and chromophobe RCCs.
Comment Here
Reference: Acquired cystic disease associated renal cell carcinoma
Comment Here
Reference: Acquired cystic disease associated renal cell carcinoma