Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Cheng L, Tretiakova M. Glomus tumor. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumorglomus.html. Accessed April 1st, 2025.
Definition / general
- Very rare pericytic (perivascular) tumor in kidney, with ~30 cases reported in English literature (Case Rep Pathol 2017;2017:7423642, Hum Pathol 2017;64:106)
Essential features
- Variable proportion of glomus cells, blood vessels and smooth muscle cells
- Glomus cells are uniform, round to ovoid, with abundant cytoplasm, distinctive cell borders and centrically located nuclei
- Glomus cells forming nests or trabeculae and surrounding dilated thin walled vessels
Terminology
- Subtypes include solid glomus tumor, glomangioma (glomuvenous malformation) and glomangiomyoma
- Other related names: glomangiomatosis, symplastic glomus tumor, glomus tumor of uncertain malignant potential and malignant glomus tumor (glomangiosarcoma)
ICD coding
- ICD-O
- ICD-10: D30.00 - benign neoplasm of unspecified kidney
- ICD-11
- 2F35 & XH47J2 - benign neoplasm of urinary organs & glomus tumor, NOS
- 2C9Y & XH21E6 - other specified malignant neoplasms of urinary tract & glomus tumor, malignant
Epidemiology
- M:F = 1.1:1 to 2:1 (its subungual counterpart shows M:F = 1:3) (Case Rep Pathol 2017;2017:7423642, Hum Pathol 2017;64:106)
- Age range: 17 - 81
Sites
- Renal primary is very rare
- Most common extrarenal sites are subungual areas
Pathophysiology
- Uncertain in kidney given the absence of glomus bodies in visceral organs
- In soft tissue counterpart, it resembles the perivascular modified smooth muscle cells of the normal glomus body
Etiology
- Not clear in renal location
- Sporadic glomus tumor in soft tissue may harbor NOTCH gene rearrangement, BRAF or KRAS mutations (Genes Chromosomes Cancer 2013;52:1075, Am J Dermatopathol 2012;34:533)
- Familial glomus tumor in soft tissue may have glomulin (GLMN) mutations, uniparental disomy of chromosome 1p or NF1 biallelic inactivation (Am J Hum Genet 2002;70:866, Am J Hum Genet 2013;92:188, Cancer Res 2009;69:7393)
Clinical features
- Asymptomatic or nonspecific symptoms, such as vague abdominal pain, flank pain and microscopic hematuria (Case Rep Pathol 2017;2017:7423642)
Diagnosis
- Imaging study of renal mass and histological examination
Radiology description
- Ultrasound: isoechoic mass (Int J Urol 2010;17:187)
- Computed tomography (CT): well defined heterogeneous enhancing lesion (Case Rep Pathol 2017;2017:7423642)
- Magnetic resonance imaging (MRI): well circumscribed lobulated mass, isointense to muscle on T1, inhomogeneous high signal on T2 (Open Access Maced J Med Sci 2019;7:4082)
- Positron emission tomography (PET): unevenly increased FDG uptake (Am J Med Sci 2017;353:310)
Radiology images
Prognostic factors
- Majority of cases in kidney are benign (Case Rep Pathol 2017;2017:7423642)
- Rare cases are reported as glomus tumor of uncertain malignant potential or histologically malignant (Hum Pathol 2010;41:145, Clin Genitourin Cancer 2017;15:e151)
- Only 1 histologically malignant case showed bone metastasis (Hum Pathol 2011;42:1200)
Case reports
- 31 year old woman with recurrent kidney glomus tumor, 33 year old woman with glomus tumor invading into the renal capsule and 55 year old man with renal glomangiomyoma (Clin Genitourin Cancer 2017 Sep 7 [Epub ahead of print])
- 38 year old woman with glomus tumors involving multiple organs, including bilateral kidneys (Open Access Maced J Med Sci 2019;7:4082)
- 57 year old man with left kidney mass (Case Rep Pathol 2017;2017:7423642)
- 58 year old man with 3 cm right kidney mass (Int J Surg Case Rep 2020;66:178)
- 67 year old man with right kidney mass (Cureus 2021;13:e19479)
- 69 year old woman with right kidney lesion (Urol Case Rep 2024;55:102774)
Treatment
- Surgical resection
Gross description
- Well circumscribed and often encapsulated, brownish or white-tan solid mass
- Usually cut surface is homogenous and may show cystic, hemorrhagic or myxoid areas (Arch Pathol Lab Med 2005;129:1172)
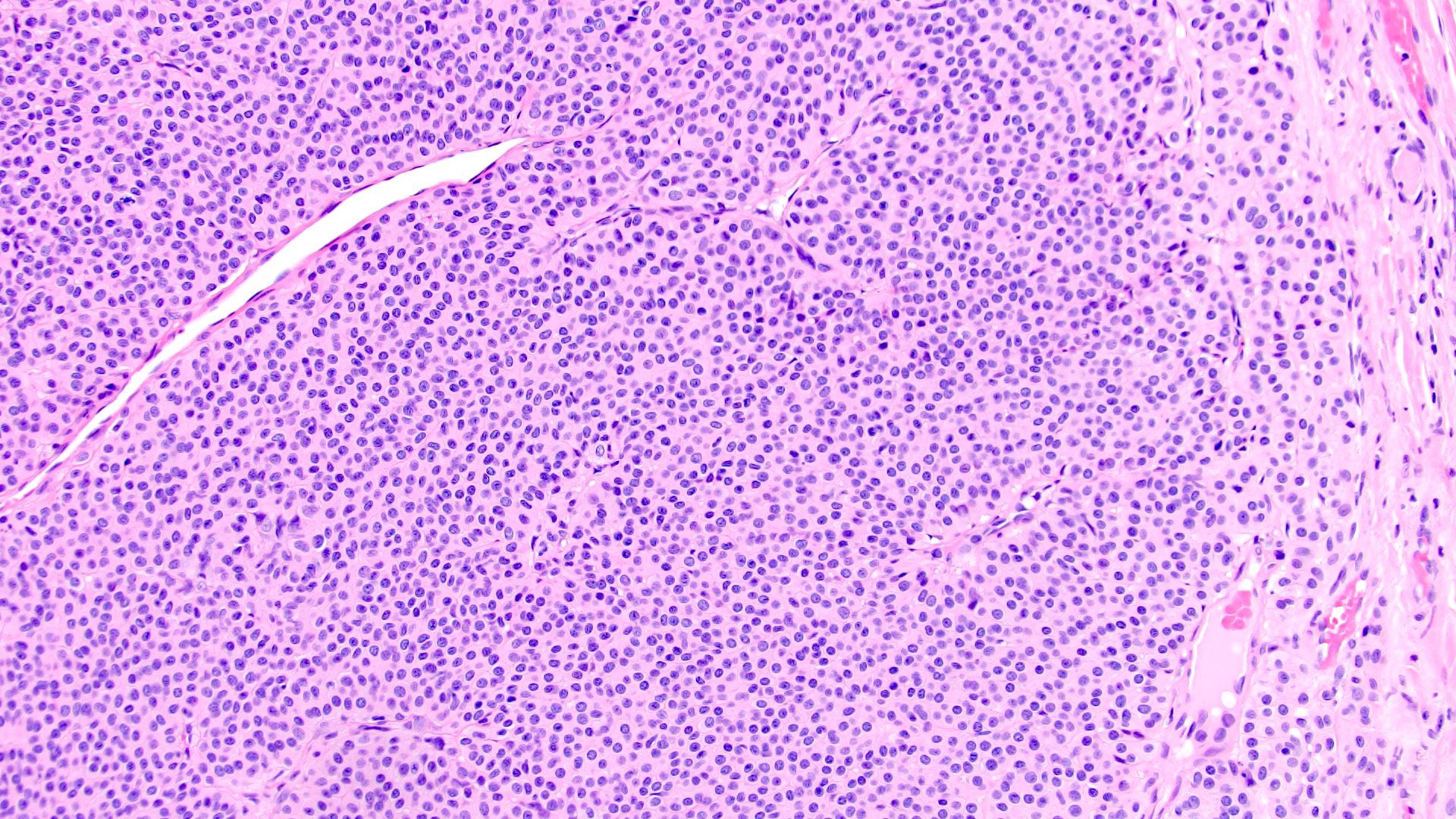
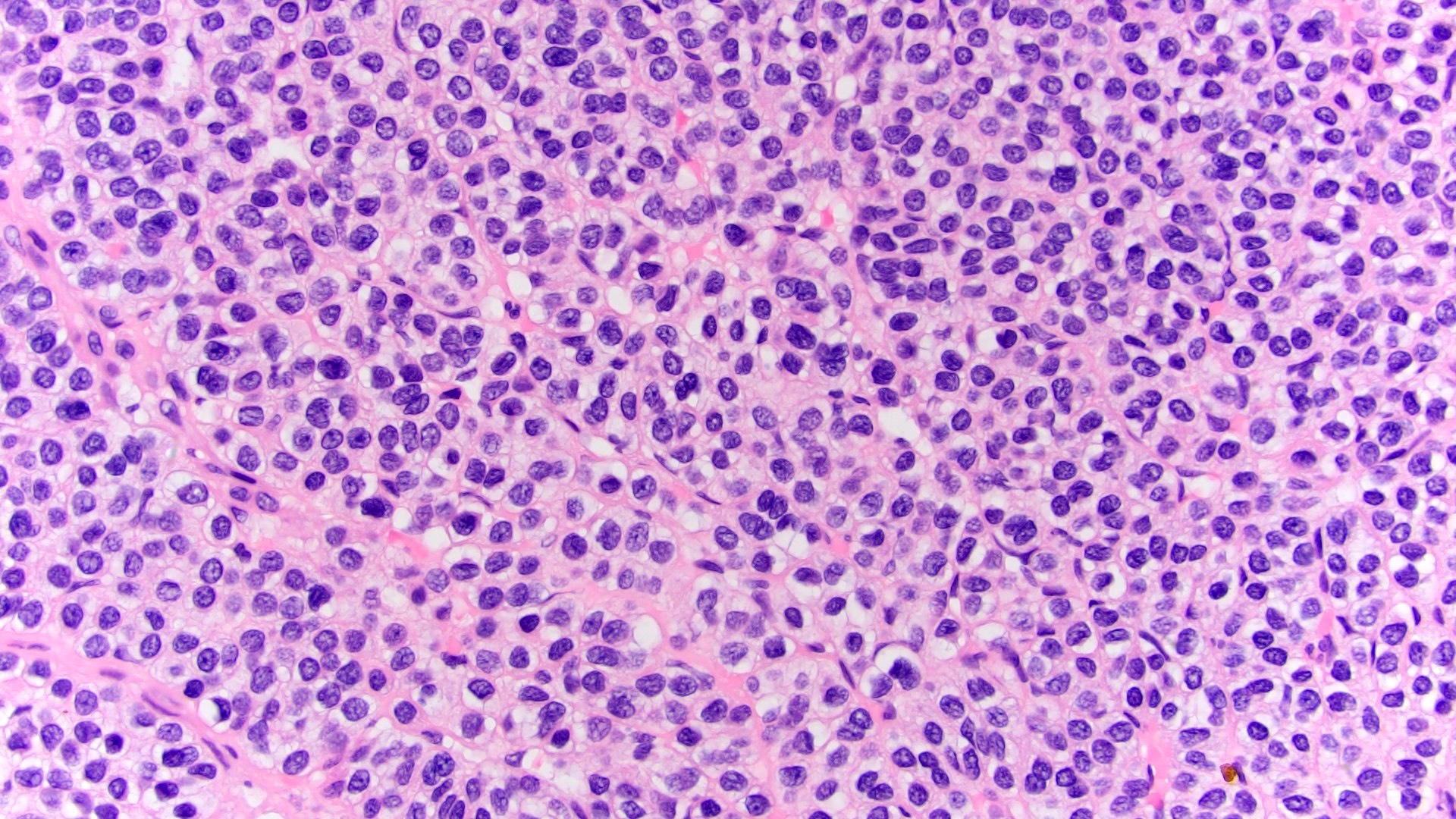
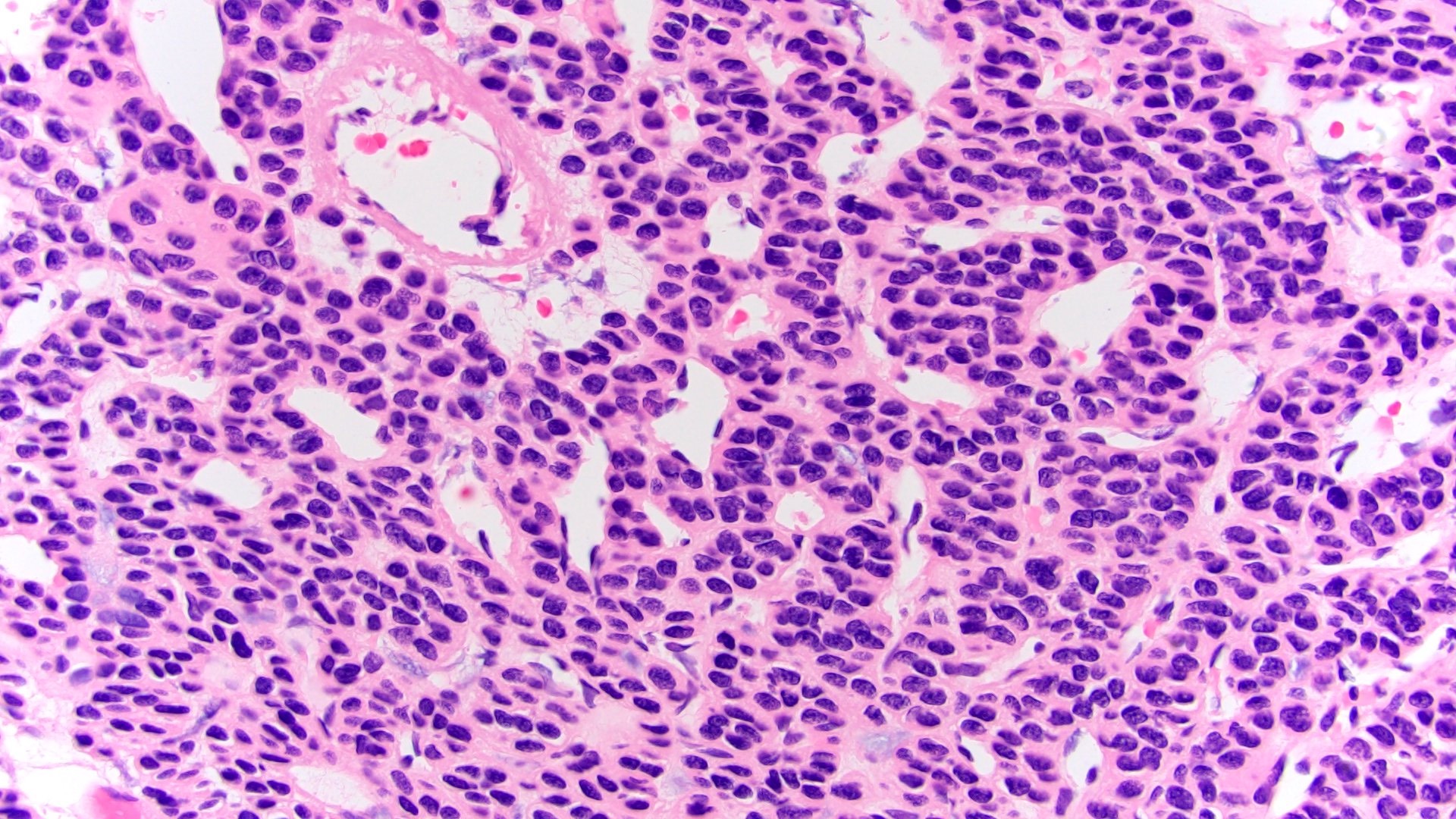
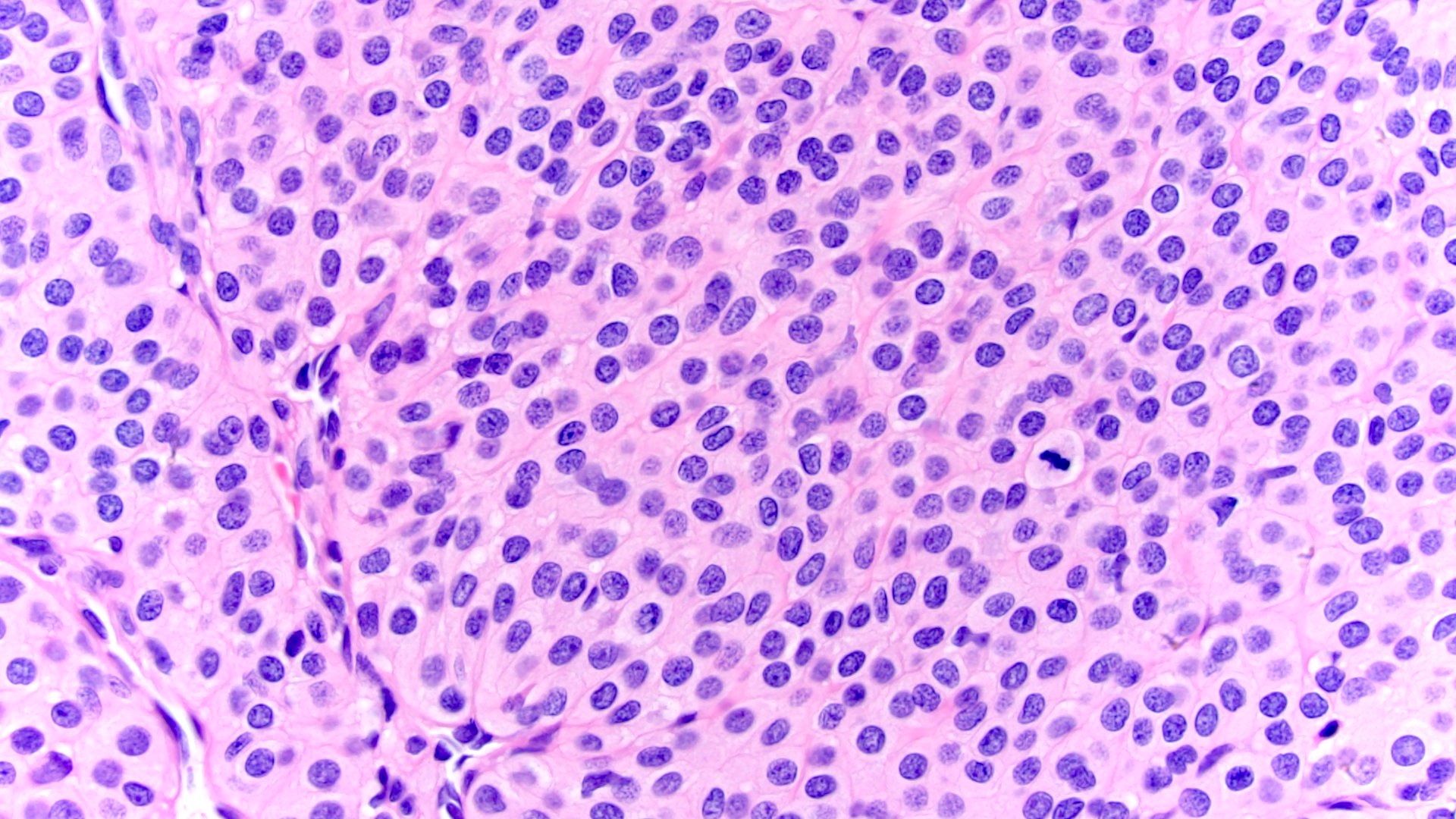
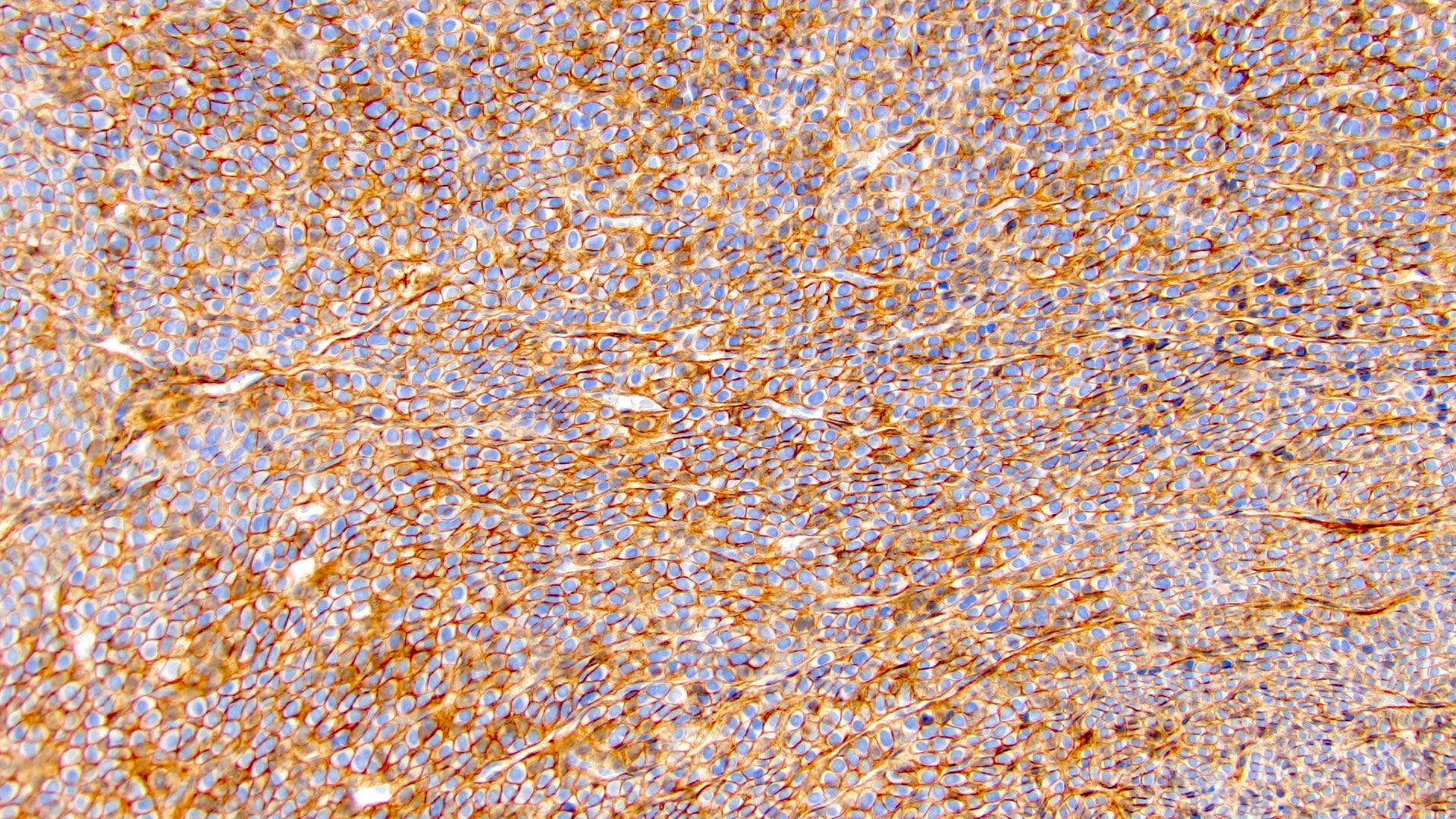
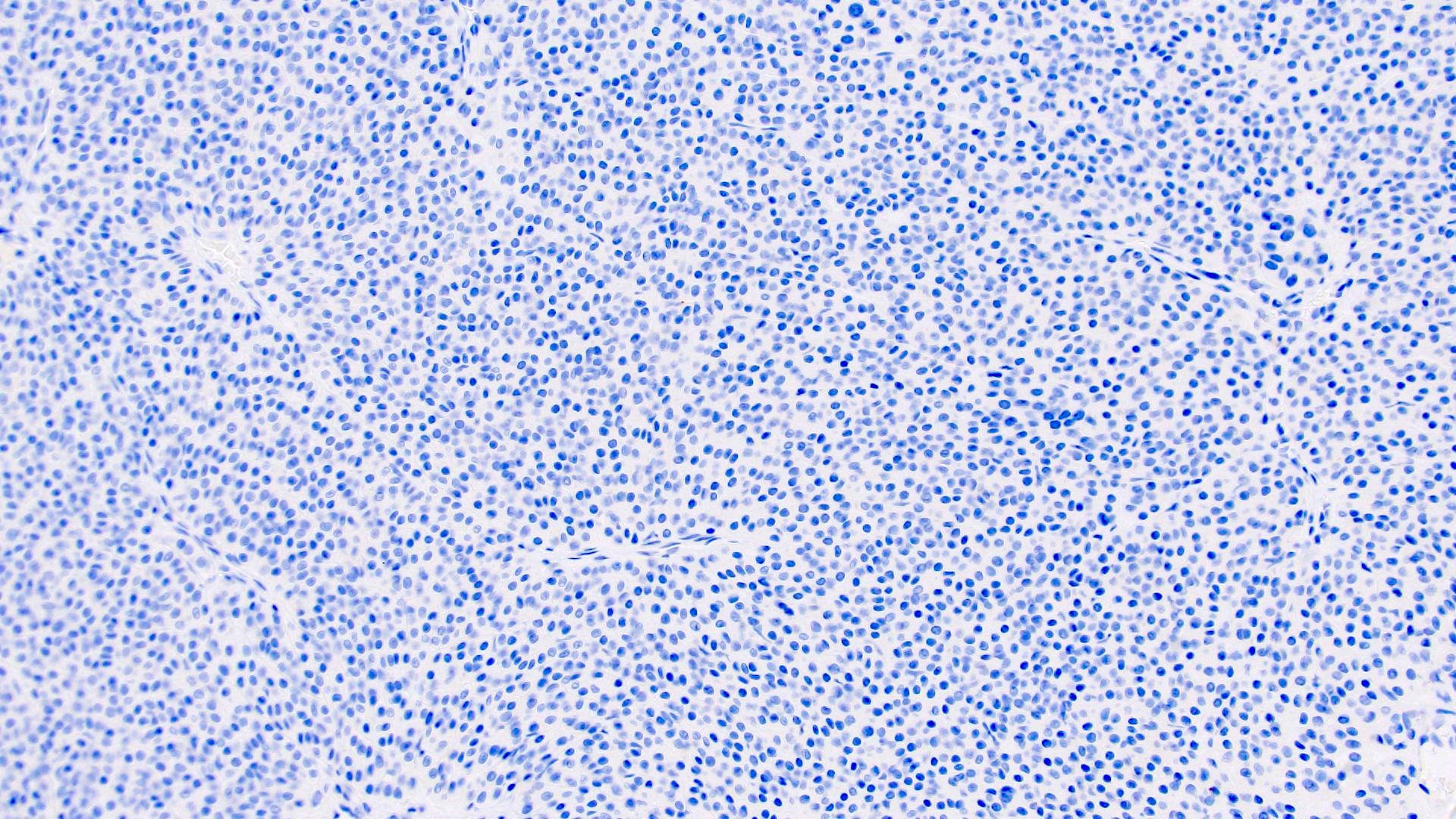
Microscopic (histologic) description
- Contains 3 components: glomus cells, blood vessels and smooth muscle cells
- Glomus cells: small and uniform, round to oval shaped, with distinctive cell borders, centrally located punched out nuclei, light eosinophilic or amphophilic cytoplasm (Hum Pathol 2017;64:106)
- Blood vessels: usually thin walled, capillary sized, dilated or branching
- Smooth muscle cells: elongated, mature looking (Arch Pathol Lab Med 2005;129:1172)
- Subtyping depends on the proportion of the 3 components
- Solid glomus tumor
- Glomus cells predominant
- Cuffs of uniform glomus cells forming nests or trabeculae and surrounding thin walled vessels
- Glomangioma
- Vessels predominant
- Cavernous hemangioma-like vasculature surrounded by small clusters or rare layers of glomus cells
- Glomangiomyoma
- Vessels and smooth muscle cells predominate
- Shows gradual transition from glomus cells to smooth muscle cells (Arch Pathol Lab Med 2005;129:1172)
- Solid glomus tumor
- Histological predictors of aggressive behavior (histologically malignant): atypical mitotic figures, moderate to high nuclear atypia, ≥ 5 mitotic figures/50 high power fields (Am J Surg Pathol 2001;25:1)
- Glomus tumor with uncertain malignant potential: does not meet above criteria for histologically malignant but has at least 1 atypical feature other than nuclear pleomorphism, > 2 cm in size and deep location
Microscopic (histologic) images
Positive stains
- Smooth muscle actin (SMA), muscle specific actin (MSA), h-caldesmon, calponin, CD57, vimentin (Int J Surg Pathol 2011;19:393)
- Collagen type IV: pericellular distribution
- CD34: 50% of cases (Hum Pathol 2017;64:106)
- S100: positive in stroma in soft tissue counterpart (J Bone Joint Surg Am 2013;95:725)
Negative stains
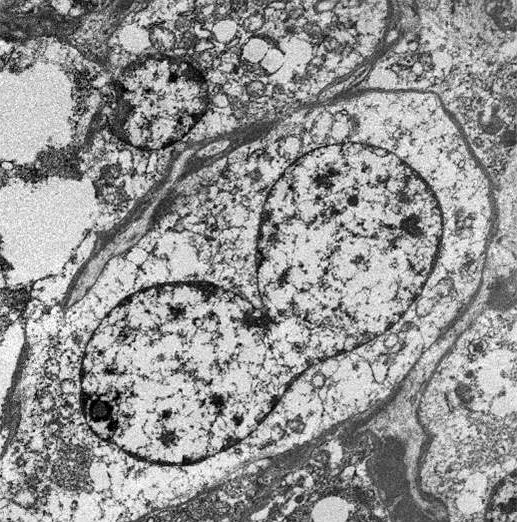
Electron microscopy description
- Cells show dense basal lamina and no intracellular mucin, neurosecretory, glycogen or renin granules (Int J Surg Pathol 2011;19:393)
- Glomangiomyoma cells show dense basal lamina and numerous cytoplasmic thin microfilaments with dense bodies (Arch Pathol Lab Med 2005;129:1172)
Electron microscopy images
Sample pathology report
- Right kidney, partial nephrectomy:
- Benign glomus tumor, 1.5 cm; margins of resection free of involvement (see comment)
- Comment: Clinically, this patient presented with flank pain and microhematuria. CT showed a heterogenous enhancing right renal mass. No other lesions or history of any malignancies are identified. The histological examination shows nests of small uniform tumor cells surrounding dilated capillary sized, thin walled vessels. The tumor cells are round to ovoid, with distinctive cell borders, amphophilic cytoplasm and centrally located nuclei. No mitosis is seen. Immunohistochemistry studies show that the tumor cells are positive for SMA and negative for pancytokeratin, synaptophysin and chromogranin. Collagen IV immunostain shows pericellular positivity. The overall findings are consistent with a benign glomus tumor, likely renal primary.
Differential diagnosis
- Myopericytoma:
- Also belongs to pericytic / perivascular tumors
- Bland, myoid appearing spindle cells showing concentric perivascular growth
- May have PDGFRB mutations
- Juxtaglomerular cell tumor:
- Young patients with severe hypertension, hypokalemia and elevated plasma renin
- Overlapped features with glomus tumor by light microscopy
- Expresses KIT in ~50% of cases, unlike glomus tumor (Hum Pathol 2013;44:47)
- Rhomboid shaped renin crystals on electron microscopy
- Paraganglioma:
- Zellballen / organoid growth pattern
- Sustentacular cells are positive for S100 and chief cells are positive for neuroendocrine markers
- Negative for cytokeratin, SMA and collagen IV
- Misnomers (such as glomus jugulare, glomus tympanicum, etc.) are paragangliomas
- Well differentiated neuroendocrine tumor:
- Nests or organoid architecture, plasmacytoid cells with stippled chromatin
- Positive for cytokeratin and neuroendocrine markers
- Negative for SMA and collagen IV
- Solitary fibrous tumor:
- Fibroblastic spindle cell tumor with patternless pattern and staghorn vasculature
- Positive for STAT6 immunostain
- Angiomyolipoma:
Additional references
Board review style question #1
Which of the following describes the histological features of a glomus tumor?
- Fibroblastic tumor with patternless pattern and staghorn vasculature
- Myoid appearing spindle cells showing concentric perivascular growth
- Nests of uniform round cells with distinctive cell borders and centrically located nuclei surrounding the dilated thin walled vessels
- Sustentacular cells and chief cells forming zellballen pattern
- Triphasic tumor with mature adipose tissue, smooth muscle and thick walled vessels
Board review style answer #1
C. Glomus tumor can show nests of uniform round cells with distinctive cell borders and centrically located nuclei surrounding the dilated thin walled vessels.
Answer A is incorrect because it describes the histological features of a solitary fibrous tumor.
Answer B is incorrect because it describes the histological features of myopericytoma.
Answer D is incorrect because it describes the histological features of paraganglioma.
Answer E is incorrect because it describes the histological features of angiomyolipoma.
Comment Here
Reference: Glomus tumor
Comment Here
Reference: Glomus tumor
Board review style question #2
Board review style answer #2
A. Collagen IV. Glomus tumors are usually positive for collagen IV with pericellular staining pattern.
Answers B, C, D and E are incorrect because these markers are usually negative in glomus tumors but positive in angiomyolipomas (HMB45), solitary fibrous tumors (STAT6) and neuroendocrine tumors (pancytokeratin and synaptophysin).
Comment Here
Reference: Glomus tumor
Comment Here
Reference: Glomus tumor