Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Andeen NK, Tretiakova M. FH deficient. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumorHLRCC.html. Accessed December 3rd, 2024.
Definition / general
- Hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome associated renal cancer may be papillary, solid and infiltrative
- It has characteristic inclusion-like nucleoli with perinucleolar clearing
- Due to germline fumarate hydratase (FH) mutations
- Other common clinical manifestation is nonrenal leiomyomatosis
Essential features
- Oncogenesis driven by metabolic derangements due to defective fumarate hydratase enzyme
- High grade, papillary, solid or infiltrative with prominent CMV inclusion-like nucleoli with perinucleolar clearing (may be only focal)
- Immunohistochemically shows overexpression of modified cysteine (2SC) and loss of fumarate hydratase
- May be confirmed by germline fumarate hydratase mutation
Terminology
- HLRCC syndrome has germline mutations of fumarate hydratase gene, conferring an increased risk of uterine and cutaneous leiomyomata as well as renal cancer
- The associated renal cell carcinoma is termed HLRCC associated renal cancer
- Also called FH deficient
Epidemiology
- Rare
- HLRCC syndrome has been reported in more than 300 families worldwide (GeneReviews 2006;2015:NBK1252)
Sites
- Kidney
- Leiomyomas in uterus and skin in HLRCC syndrome
Pathophysiology
- Mutations in the Fumarate Hydratase (FH) gene lead to a defective FH enzyme in the citric acid cycle, causing metabolic derangement, "pseudohypoxic" upregulation of hypoxia inducible factor 1 alpha (HIF1a) and nonenzymatic modification of cysteine residues in multiple proteins (succination), altering their function and ultimately driving oncogenesis (Am J Surg Pathol 2014;38:567, Oncogene 2014;33:2547)
Diagrams / tables
Clinical features
- HLRCC associated renal cancer occurs in 1/3 with HLRCC germline mutation
- Mean age of presentation with renal cancer: 36 years (Am J Surg Pathol 2014;38:627)
- Leiomyomas of skin and uterus are the most common features (seen in 85%), usually develop in the 3rd decade
- Uterine leiomyomas are often numerous and large, 50% of women have hysterectomy before age 30 (18 - 52 years)
Diagnosis
- Description of clinical and genetic diagnostic criteria for HLRCC syndrome (GeneReviews 2006;NBK1252:)
Prognostic factors
- HLRCC has a poor prognosis, with early and widespread metastases, even with small tumors
Case reports
- Decreased fumarate hydratase activity and identification of FH mutation in circulating lymphocytes in 2 young patients with fibroids (J Obstet Gynaecol Res 2013;39:410)
- Development of cutaneous leiomyomas and diagnosis of HLRCC syndrome in pregnancy (J Cutan Med Surg 2016;20:334)
- 59 year old woman with widespread metastases (Am J Surg Pathol 2014;38:567)
- 64 year old man and his 39 year old son without cutaneous leiomyomata (BMC Res Notes 2014;7:203)
Gross description
- Solitary, unilateral
- Solid or cystic, 2.5 - 12 cm
Microscopic (histologic) description
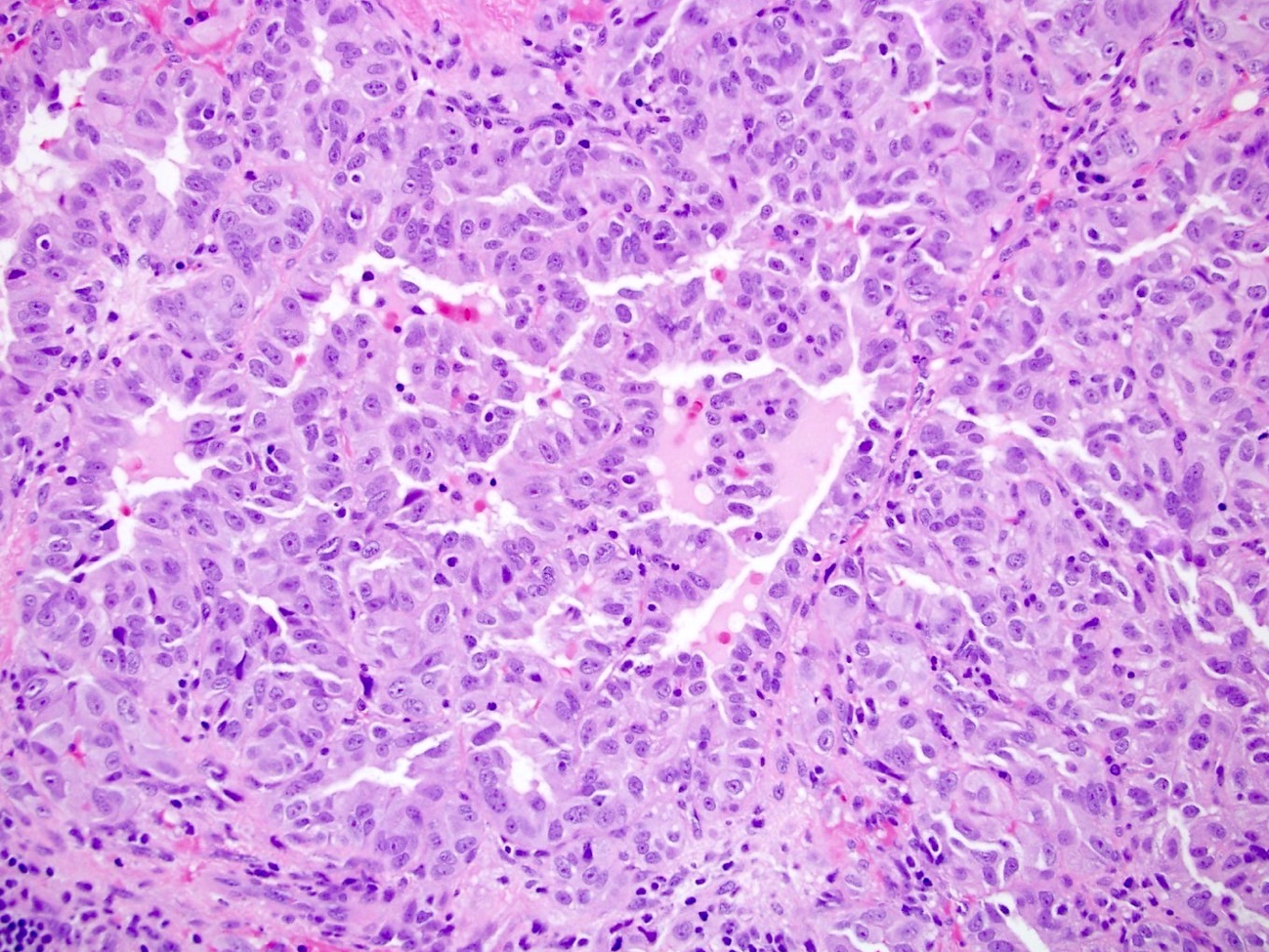
- High grade with various patterns: papillary, tubular, solid, cribriform, cystic, collecting duct carcinoma-like, sarcomatoid (Am J Surg Pathol 2014;38:627)
- Prominent eosinophilic CMV-like nucleoli with perinucleolar halo (may be only focal)
- May have hyalinized and edematous fibrovascular cores with micropapillary fronds but no foamy histiocytes (Am J Surg Pathol 2014;38:627)
Microscopic (histologic) images
Contributed by Debra Zynger, M.D., Nicole K. Andeen, M.D. and Maria Tretiakova, M.D., Ph.D.
Images hosted on other servers:
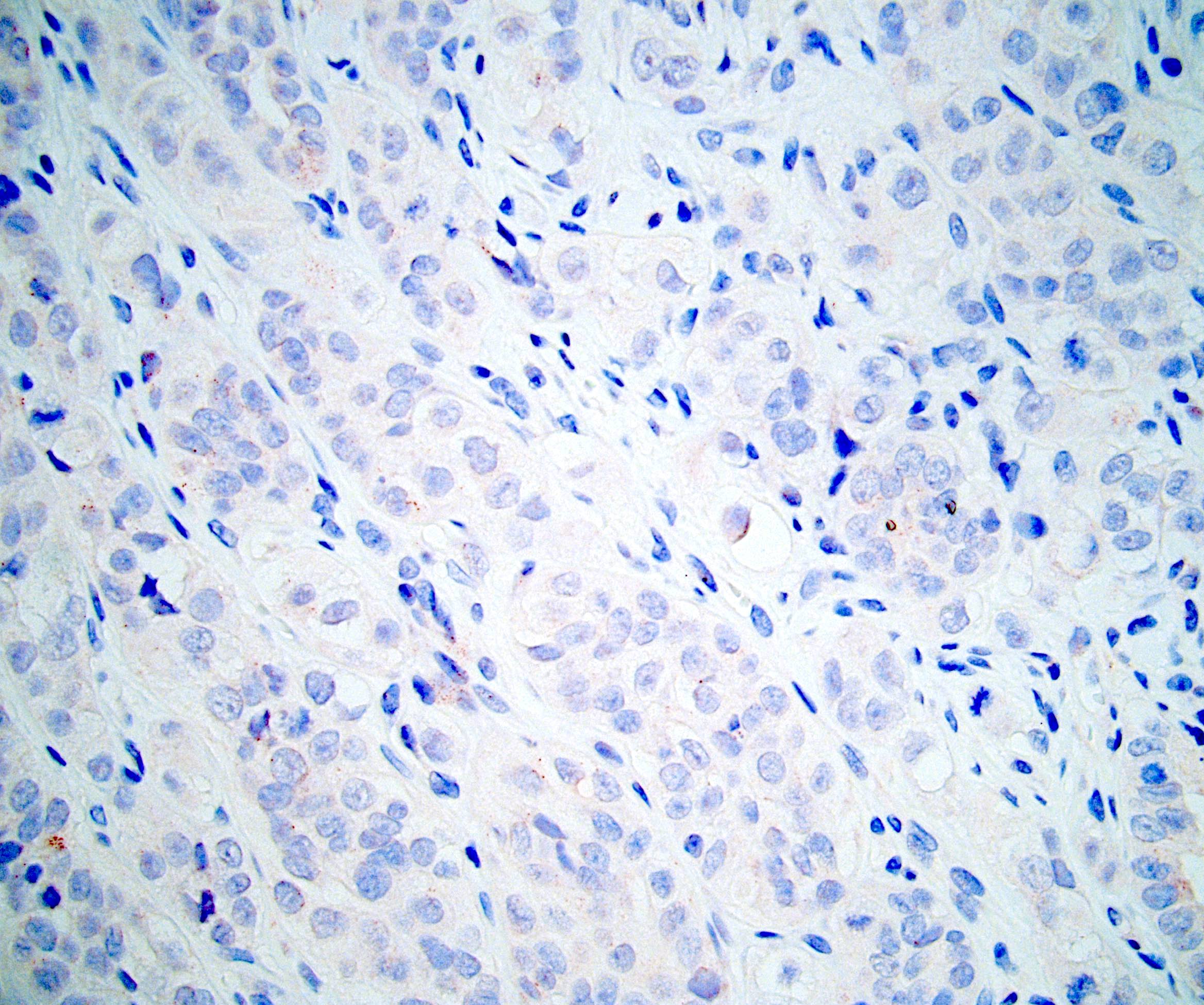
Positive stains
- PAX8, vimentin, GLUT1, p53, S100A1, SDHB, INI1 (Am J Surg Pathol 2018;42:279, Histopathology 2018;72:588)
- 2-succino-cysteine / 2SC overexpression (nuclear and cytoplasmic staining), which is more sensitive and specific for FH gene mutation than loss of FH by IHC (Am J Surg Pathol 2016;40:982, Am J Surg Pathol 2015;39:1529)
Negative stains
Molecular / cytogenetics description
- Fumarate Hydratase (FH) gene is located on 1q42-43, and consists of 10 exons
- Autosomal dominant inheritance
- In HLRCC, oxidative phosphorylation is impaired, and cells undergo a metabolic shift to aerobic glycolysis (Clin Cancer Res 2013;19:3345)
- Without fumarate hydratase activity, fumarate increases and acts as an oncometabolite
- Fumarate impairs the function of hypoxia inducible factor prolyl hydroxylase, resulting in increased levels of HIF1alpha (WHO 2016)
Differential diagnosis
- Overall, careful examination for characteristic nucleolar features, cytoplasmic and nuclear reactivity for S (2 succino) cysteine (2SC) and loss of fumarate hydratase expression appear to be most useful in the differential diagnosis
- Papillary type 2 RCC: unlike HLRCC, often expresses AMACR, may express CK7 (20%)
- 22% show cytoplasmic reactivity for 2SC, but nuclear staining is less likely to be diffuse compared with HLRCC (Am J Surg Pathol 2014;38:627)
- FH deficient RCC
- Remarkably similar to HLRCC clinically
- Morphologically and immunophenotypically similar, but harbor somatic and not germline mutations (Am J Surg Pathol 2016;40:865)
- Clear cell RCC: has membranous CAIX staining and no 2SC reactivity, unlike HLRCC
- Collecting duct carcinoma: CD10 and 2SC negative
- Microphthalmia transcription factor (MiT) family translocation associated RCC: TFE3 positive, 2SC negative
- Unclassified RCC: 2SC negative (Am J Surg Pathol 2014;38:627)
Additional references