Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Positive stains | Electron microscopy description | Electron microscopy images | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Albadri ST. Tubulointerstitial nephritis-general. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytubulointerstitialnephritis.html. Accessed December 24th, 2024.
Definition / general
- Acute interstitial inflammation is commonly associated with involvement of the tubules due to a variety of causes
Essential features
- Acute inflammation involving tubulointerstitial compartments
- Might be associated with acute tubular injury or tubulointerstitial scarring
- Common etiologies include drug, autoimmune, infection, hereditary and idiopathic
Terminology
- Acute interstitial nephritis (AIN)
ICD coding
- ICD-10:
- N10 - acute pyelonephritis
- N11 - chronic tubulointerstitial nephritis
- N12 - tubulointerstitial nephritis, not specified as acute or chronic
- N13 - obstructive and reflux uropathy
- N14 - drug and heavy metal induced tubulointerstitial and tubular conditions
- N15 - other renal tubulointerstitial diseases
- N16 - renal tubulointerstitial disorders in diseases classified elsewhere
Epidemiology
- Incidence: ~15 - 27% of renal biopsies for acute kidney failure (Am J Kidney Dis 2000;35:433)
Sites
- Kidney, interstitium and tubules
Pathophysiology
- High exposure to nephrotoxic drugs
- Injury of the tubulointerstitial compartment due to decreased blood supply and increase in metabolic demand
- Escalating the inflammatory processes by production and activation of cytokines, tissue necrosis factor (TNF) alpha
- Type IV hypersensitivity reactions in drug induced tubulointerstitial nephritis (Adv Chronic Kidney Dis 2017;24:107)
Etiology
- Drugs (J Nephrol 2016;29:611, Am J Kidney Dis 1998;31:108):
- Accounts for about 60 - 70% of all tubulointerstitial nephritis
- Allergic (nonsteroidal anti-inflammatory [NSAIDs], antibiotics, proton pump inhibitors [PPI])
- Toxic (lithium)
- Autoimmune:
- Primary (antibrush border antibody [ABBA])
- Secondary to systemic diseases (Sjögren syndrome, IgG4 related disease, tubulointerstitial nephritis with uveitis) or immune upregulation (check point inhibitor therapy)
- Infection:
- Primary kidney (pyelonephritis, BK polyomavirus tubulointerstitial nephritis)
- Secondary to infection associated glomerulonephritis
- Hereditary / toxic / metabolic:
- Autosomal dominant interstitial kidney disease (Semin Nephrol 2010;30:366)
- Idiopathic: 8%
Clinical features
- Acute or subacute renal failure
- Subnephrotic range proteinuria
- Sometimes microscopic hematuria
- Drug induced tubulointerstitial nephritis: fever, skin rash, arthralgia and eosinophilia (Pediatr Clin North Am 2019;66:111)
Diagnosis
- Clinical history of newly exposure to new drug (allergic etiology) or presence / absence of systemic disease
- Physical examination; skin rashes (morbilliform, maculopapular, erythroderma and epidermal necrolysis) (Nat Rev Nephrol 2010;6:461)
- Bilateral normal to increased size of the kidney and diffusely increased cortical hyperechogenicity by renal ultrasound (Nat Rev Nephrol 2010;6:461)
Laboratory
- Elevation of serum creatinine and blood urea (Clin J Am Soc Nephrol 2017;12:2046)
- Hyperkalemic
- Hyperchloremic metabolic acidosis
- Elevation of eosinophils level (nonspecific)
- Elevation the level of serum erythrocyte sedimentation rate (ESR) or C reactive proteins
- Positive proteinuria in dipstick test and microscopic or macroscopic hematuria
Prognostic factors
- Good prognosis for drug induced tubulointerstitial nephritis (Nat Rev Nephrol 2010;6:461)
- Poor prognosis for granulomatous tubulointerstitial nephritis (Clin Kidney J 2015;8:516)
Case reports
- 14 year old girl with one sided uveitis and renal involvement (J Med Case Rep 2021;15:443)
- 28 year old man with a history of ulcerative colitis and sacroiliitis with progressive kidney dysfunction (Intern Med 2019;58:79)
- 59 year old man with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and acute kidney injury (AKI) (Clin Kidney J 2021;14:2151)
- 70 year old man with renal dysfunction, a medical history of bile duct stenosis, an inflammatory pancreatic mass and elevation of serum creatinine and IgG4 (Ren Fail 2019;41:657)
Treatment
- Eliminate the causative agents (drugs / toxins)
- Treat associated systemic disorders
- Corticosteroid therapy
- In steroid resistant cases and steroid contraindicated cases, mycophenolate mofetil could be considered (Adv Chronic Kidney Dis 2017;24:94)
- Azathioprine could be used in cases associated with systemic inflammatory and autoimmune diseases, such as Sjögren syndrome
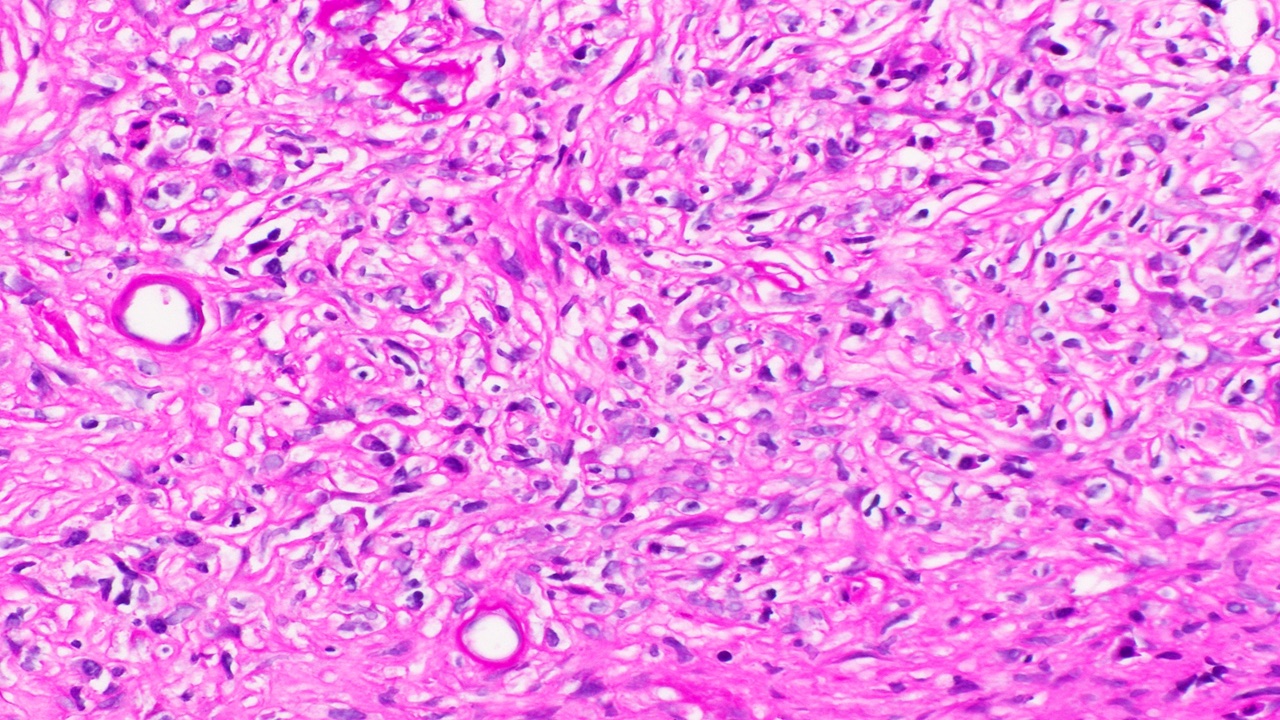
Microscopic (histologic) description
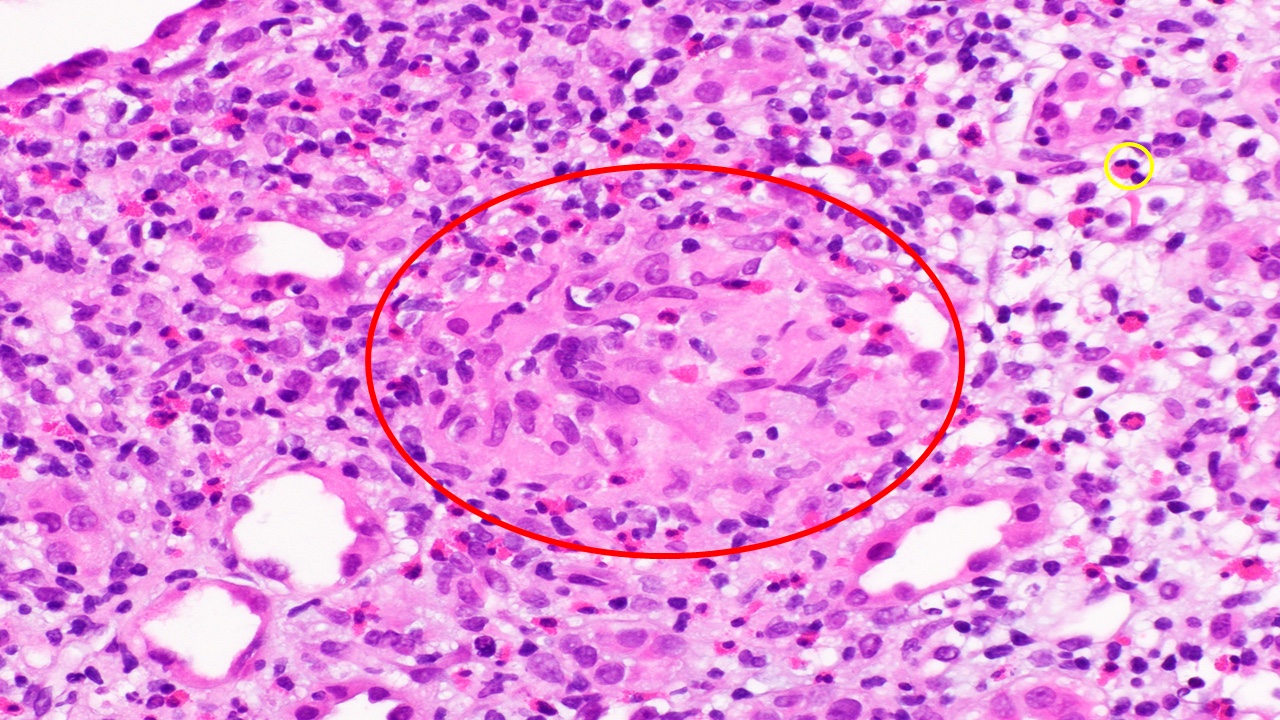
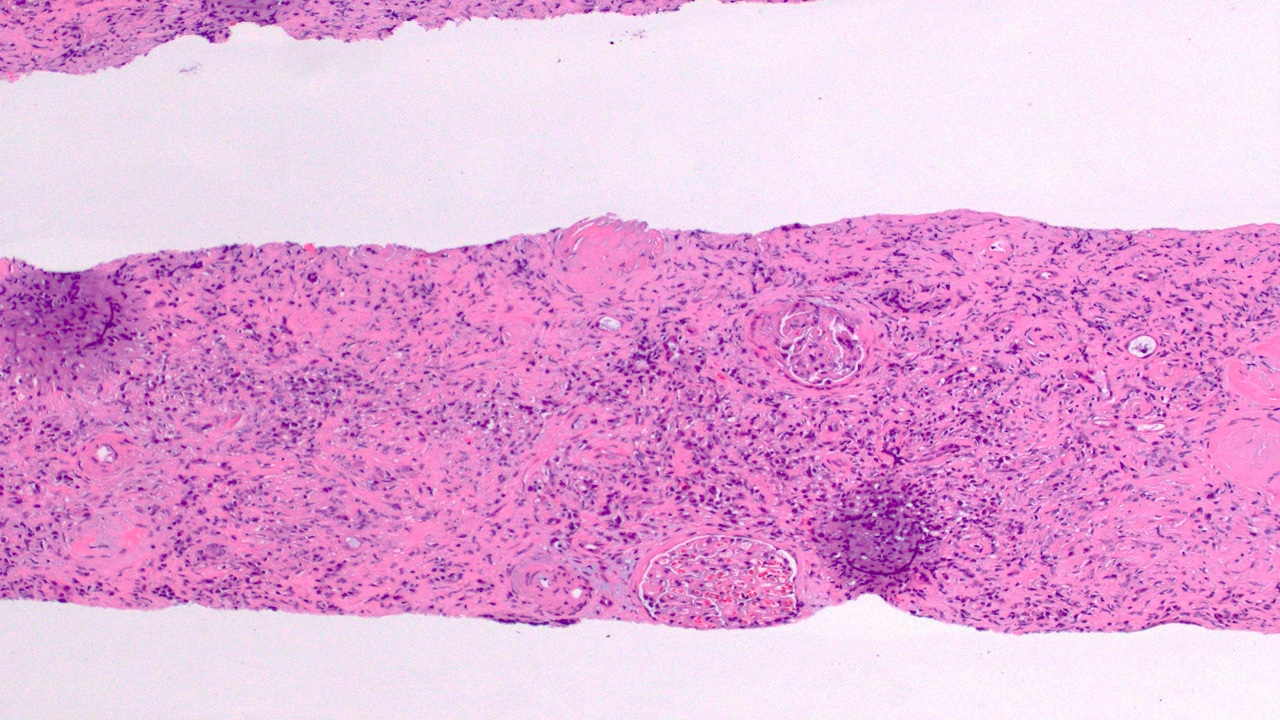
- Interstitial inflammatory cell infiltrate composed of lymphocytes, macrophages, plasma cells and eosinophils (in different proportion) (Adv Chronic Kidney Dis 2017;24:72, Pediatr Clin North Am 2019;66:111, Clin Rheumatol 2018;37:257)
- Predominance of eosinophils suggests allergic etiology (nonspecific)
- Predominance of plasma cells suggest autoimmune etiology (nonspecific)
- Granulomatous inflammatory interstitial nephritis (Indian J Nephrol 2020;30:26):
- Necrotizing granulomatous inflammation in infection etiology, such as tuberculosis and fungal infection
- Nonnecrotizing granulomatous inflammation in drug induced tubulointerstitial nephritis and sarcoidosis
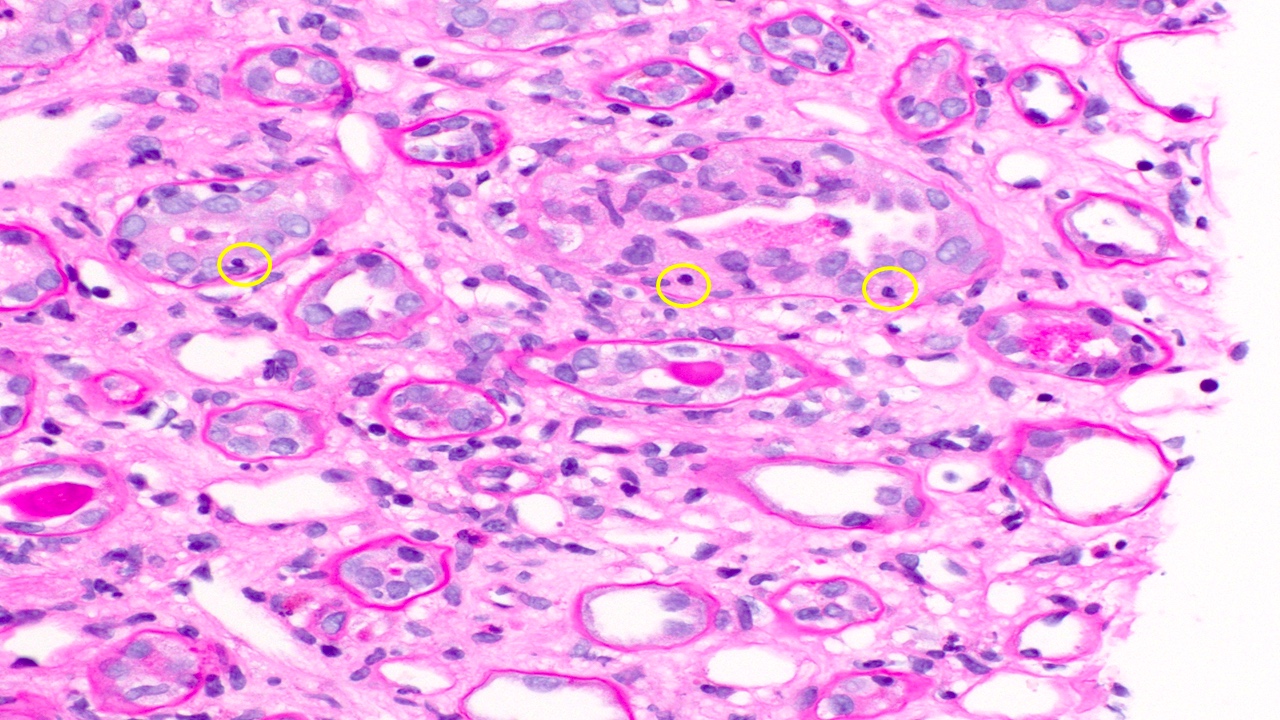
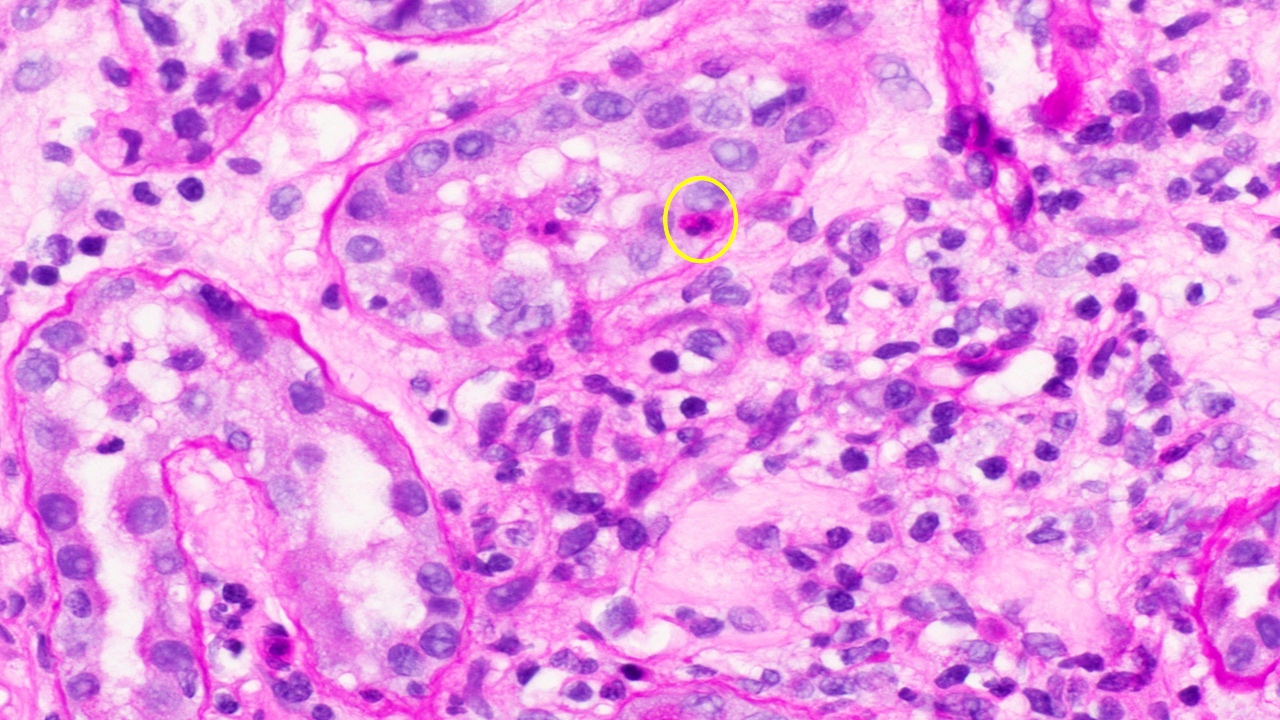
- Tubulitis (mild, moderate and severe) (Adv Chronic Kidney Dis 2017;24:72, Pediatr Clin North Am 2019;66:111)
- Acute tubular injury (luminal ectasia, simplification of the epithelium, loss of brush border or intraluminal necrosis) (Adv Chronic Kidney Dis 2017;24:72, Pediatr Clin North Am 2019;66:111)
- In chronic cases, tubular atrophy and interstitial fibrosis with evidence of active tubulitis in nonseverely atrophic tubules (Pediatr Nephrol 2017;32:577)
Microscopic (histologic) images
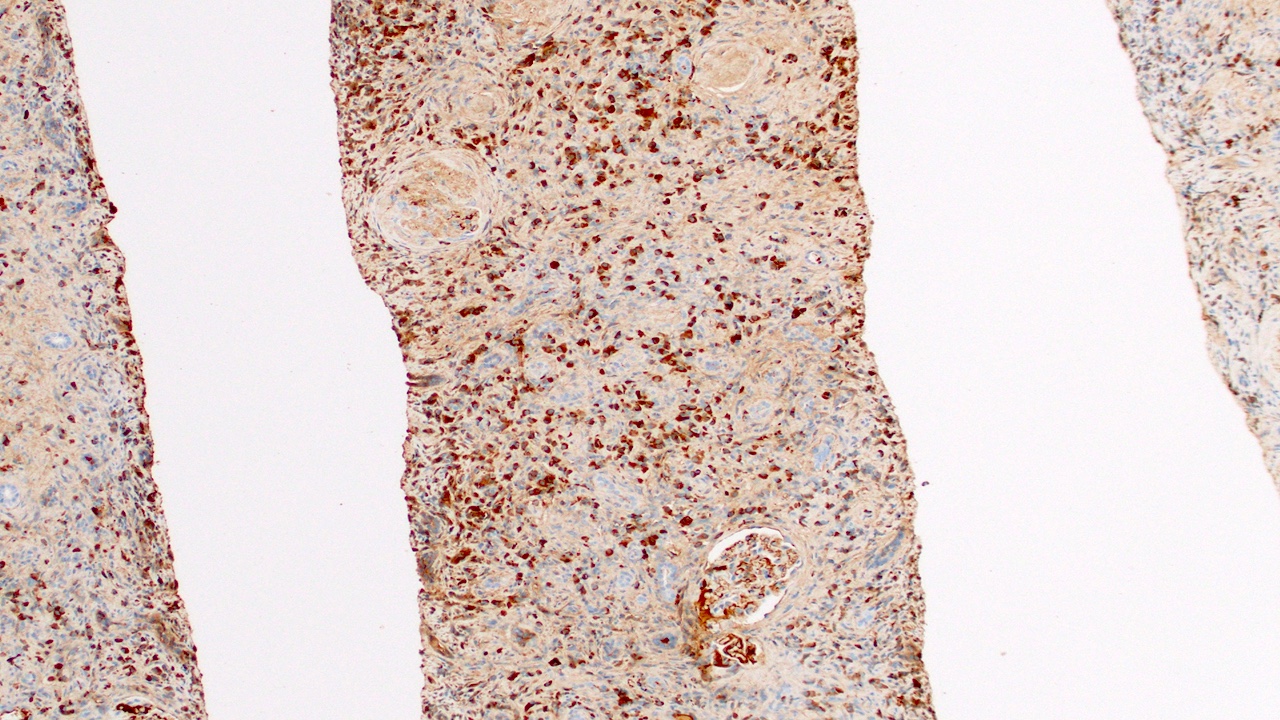
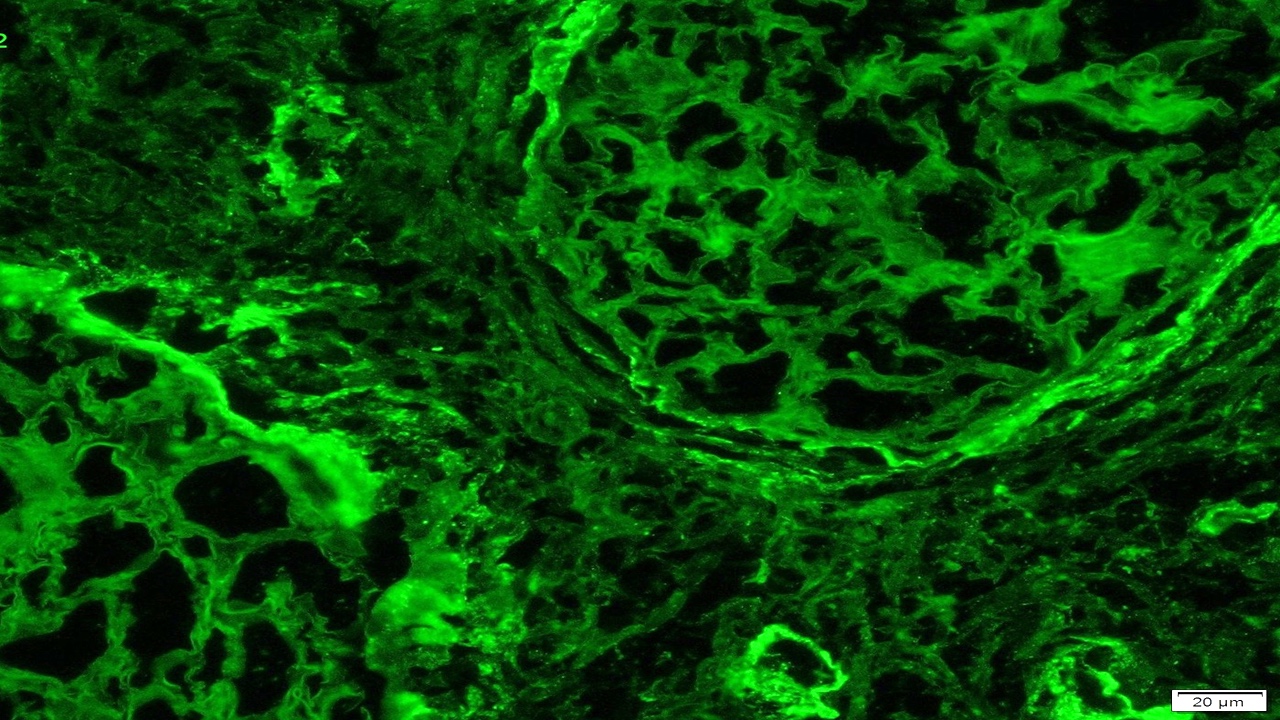
Immunofluorescence description
- Granular tubular basement membranes deposits with IgG (IgG4 related tubulointerstitial nephritis)
- Linear tubular basement membranes deposits (antitubular basement membrane disease) (Curr Opin Nephrol Hypertens 2012;21:279)
Immunofluorescence images
Positive stains
- AFB: positive in acid fast bacilli infection
- GMS highlights fungal elements
- IgG and IgG4 positive plasma cells (increased IgG4/IgG ratio) in IgG4 related disease (Am J Kidney Dis 2017;69:e19)
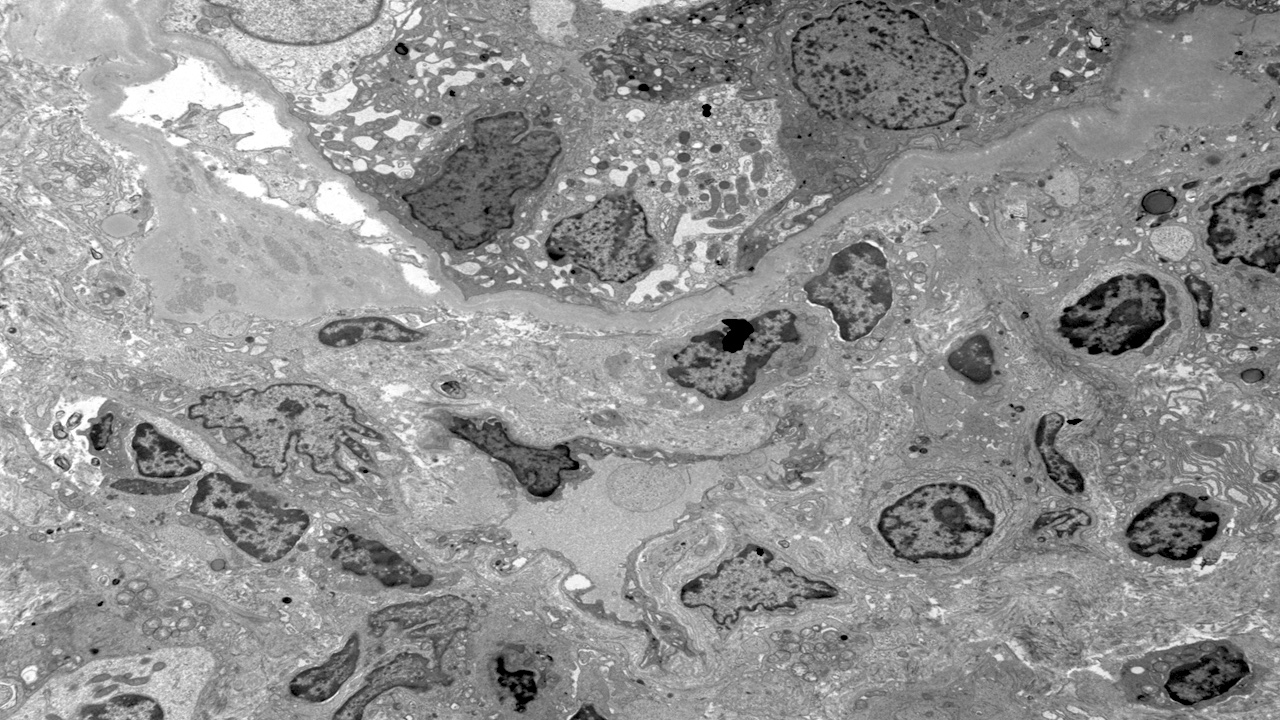
Electron microscopy description
- Nonspecific; evidence of inflammatory cells in the interstitium and tubules
Electron microscopy images
Videos
Histopathology kidney - interstitial nephritis
Sample pathology report
- Kidney, core needle biopsy:
- Acute and chronic interstitial nephritis, moderate (see comment)
- Comment: There is no evidence of a glomerular disease of the immune complex type seen on immunofluorescence. Light microscopy exhibits mild acute and chronic interstitial nephritis. Given the positive ANA and SSA and the plasma cell rich infiltrate, this could be due to autoimmune disease, such as Sjögren syndrome. Other possibilities include tubulointerstitial nephritis and uveitis (TINU) syndrome and drug allergies. Clinical correlation is recommended.
Differential diagnosis
- Interstitial inflammation secondary to glomerulonephritis:
- Neoplastic processes:
- Infiltrating lymphoid neoplasm or cast nephropathy
- Acute cellular rejection in renal transplant
- Medullary capillaritis:
- IgA vasculitis, pauci-immune necrotizing and crescentic glomerulonephritis
- Urinary tract infection:
- White blood cell casts
- Leukocytosis
- Positive dipstick test for leukocyte esterase
Board review style question #1
Board review style answer #1
Board review style question #2
What is the most important histopathologic finding in acute tubulointerstitial nephritis?
- Crescentic lesions
- Glomerulitis
- Inflammation of the interstitium with active tubulitis
- Segmental sclerosis of the glomeruli
Board review style answer #2
C. Inflammation of the interstitium with active tubulitis
Comment Here
Reference: Tubulointerstitial nephritis
Comment Here
Reference: Tubulointerstitial nephritis