Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagnosis | Laboratory | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Electron microscopy description | Electron microscopy images | Genetics | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Akilesh S. COVID-19 associated kidney injury. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneynontumorCOVIDinjury.html. Accessed March 31st, 2025.
Definition / general
- Acute kidney injury, nephrotic range proteinuria and acute thrombotic microangiopathy (TMA) that can be seen during or following COVID-19 disease
- Kidney disease may occur even with mild COVID-19 symptoms in susceptible individuals
- Kidney allograft recipients may experience rejection episodes
Essential features
- Autopsy based studies often have patients who died with COVID-19, while biopsy based studies often include patients with primary presentation of kidney dysfunction, often with only mild COVID-19 symptoms
- Acute tubular injury / acute tubular necrosis is the most common finding in autopsy and biopsy based studies
- In biopsy based studies, collapsing glomerulopathy is seen almost exclusively in Black patients with high risk APOL1 genotypes
- Acute endothelial cell injury / acute thrombotic microangiopathy can also be seen in 15% of patients
- Chronic tubulointerstitial injury, even with microcystic tubular atrophy (which may be driven by COVID-19 or pre-existing in the patient), is variable
Terminology
- Sometimes called COVID-19 associated nephropathy (COVAN) when collapsing glomerulopathy is present
ICD coding
Epidemiology
- Causative agent is the novel coronavirus, SARS-CoV-2
- In autopsy series, 70% are men, mean age of 73 years; 59% have hypertension and 33% have diabetes (Curr Opin Nephrol Hypertens 2021;30:324)
- Almost all cases of collapsing glomerulopathy have been detected in Black patients; of those tested, virtually all have high risk APOL1 genotypes
Sites
- Kidney injury is likely an indirect effect of pulmonary failure (severe COVID-19) or cytokine mediated injury (mild COVID-19); direct infection of the kidney does not seem to be a common mechanism of injury
Pathophysiology
- In severe COVID-19, pulmonary failure and circulating cytokines are thought to injure the kidney (autopsy studies)
- In mild COVID-19, the immune response to viral infection in the lungs / upper airways is thought to injure glomerular podocytes via interferon mediated increase in expression of high risk APOL1 proteins → collapsing glomerulopathy (biopsy studies)
- Indirect cytokine mediated effects are also thought to be responsible for acute tubular injury and acute endothelial injury, though mechanisms have not been completely elucidated (Curr Opin Nephrol Hypertens 2021;30:324)
Etiology
- Direct or recent infection with SARS-CoV-2
Diagnosis
- Urinalysis, blood metabolic panel (BMP), 24 hour urine protein quantification, serum albumin quantification
Laboratory
- Elevated serum creatinine, blood urea nitrogen (acute kidney injury)
- Decreased serum albumin, increased proteinuria (collapsing glomerulopathy)
- Decreased hemoglobin, lowered platelets, increased lactate dehydrogenase (LDH), decreased haptoglobin (thrombotic microangiopathy)
- Reference: Am J Kidney Dis 2021;77:82
Case reports
- 29 year old man, kidney transplant patient, who developed collapsing glomerulopathy in the allograft in the setting of COVID-19 (Am J Kidney Dis 2020;76:590)
- 49 year old woman, kidney transplant patient, who developed minimal change disease during COVID-19 disease (Transplant Proc 2020;52:2693)
- 54 year old man, kidney transplant patient, with chronic active antibody mediated rejection following COVID-19 disease (Transplant Proc 2021;53:1202)
- 69 year old woman with COVID-19 who developed thrombotic microangiopathy (Kidney Int 2020;98:509)
- Early 70s man who died of COVID-19 pneumonia and was treated with hydroxychloroquine (Ultrastruct Pathol 2020;44:519)
Treatment
- If kidney injury is severe, kidney replacement therapy (dialysis) may be required, either on a short term or permanent basis
Microscopic (histologic) description
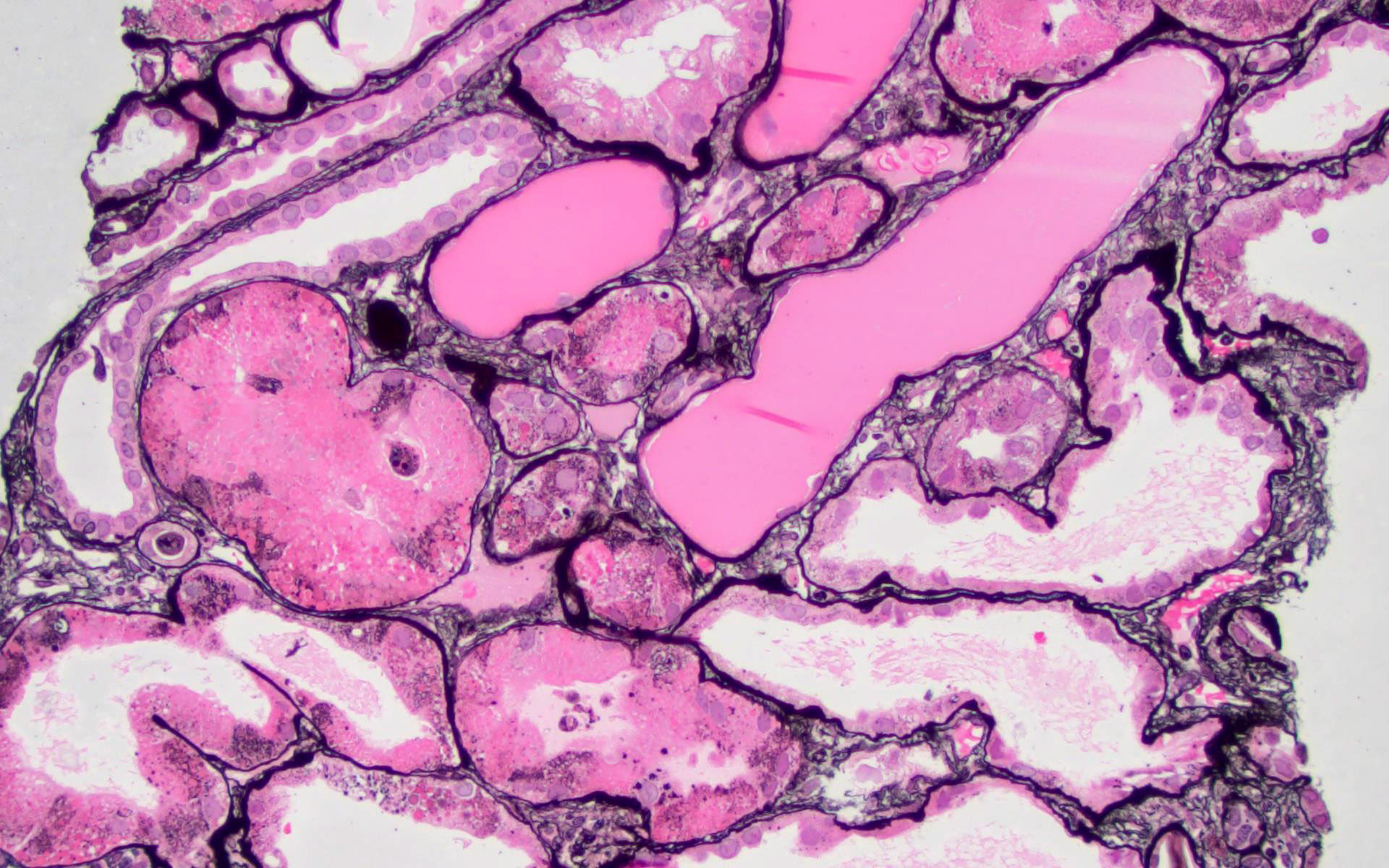
- Acute tubular injury: tubular epithelial cell attenuation / simplification, shedding of epithelial cells, tubular apoptosis, regenerative mitosis, occasionally frank necrosis; some tubules may have eosinophilic cast material and atrophic appearing epithelium (microcystic tubular atrophy)
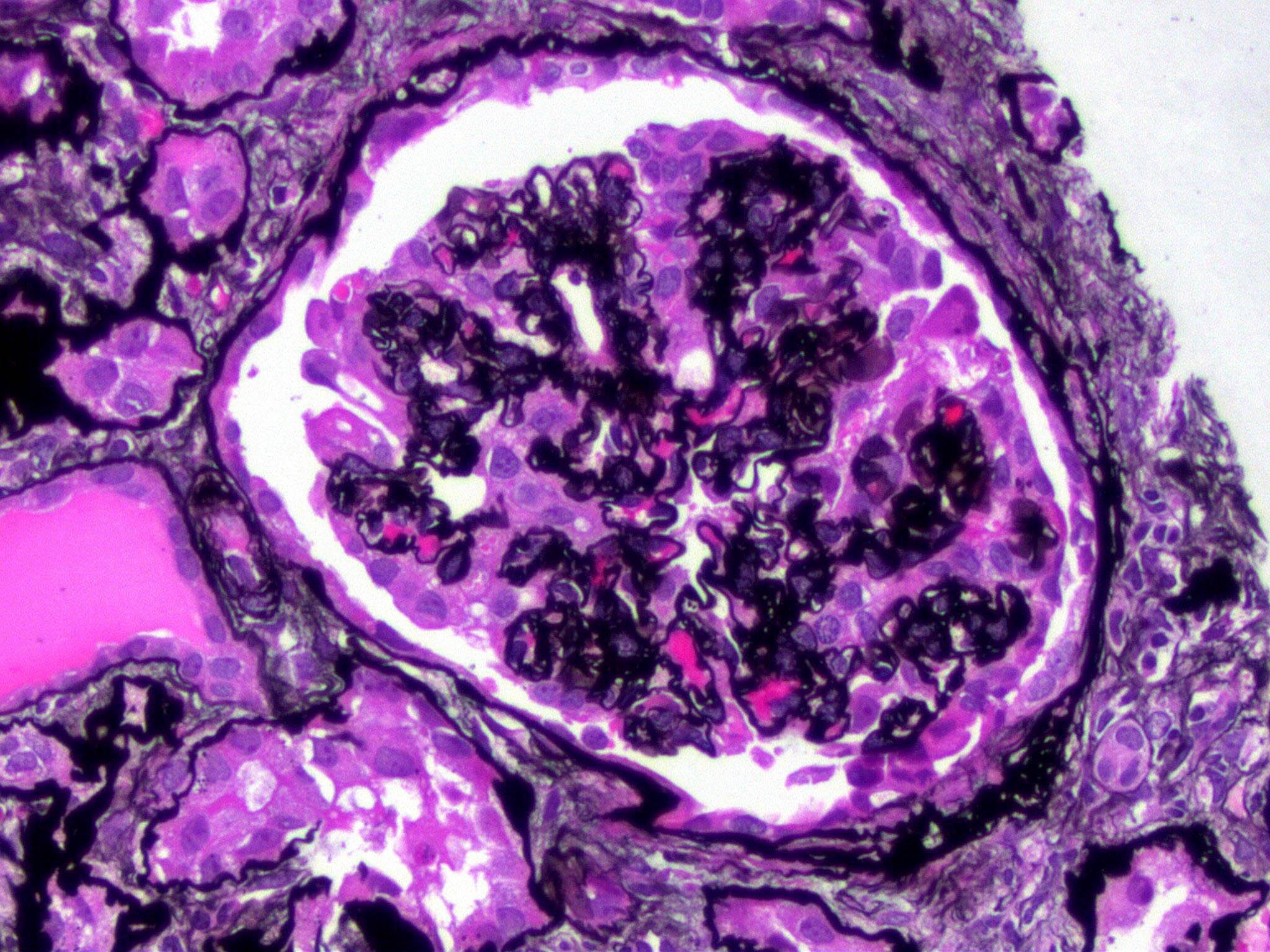
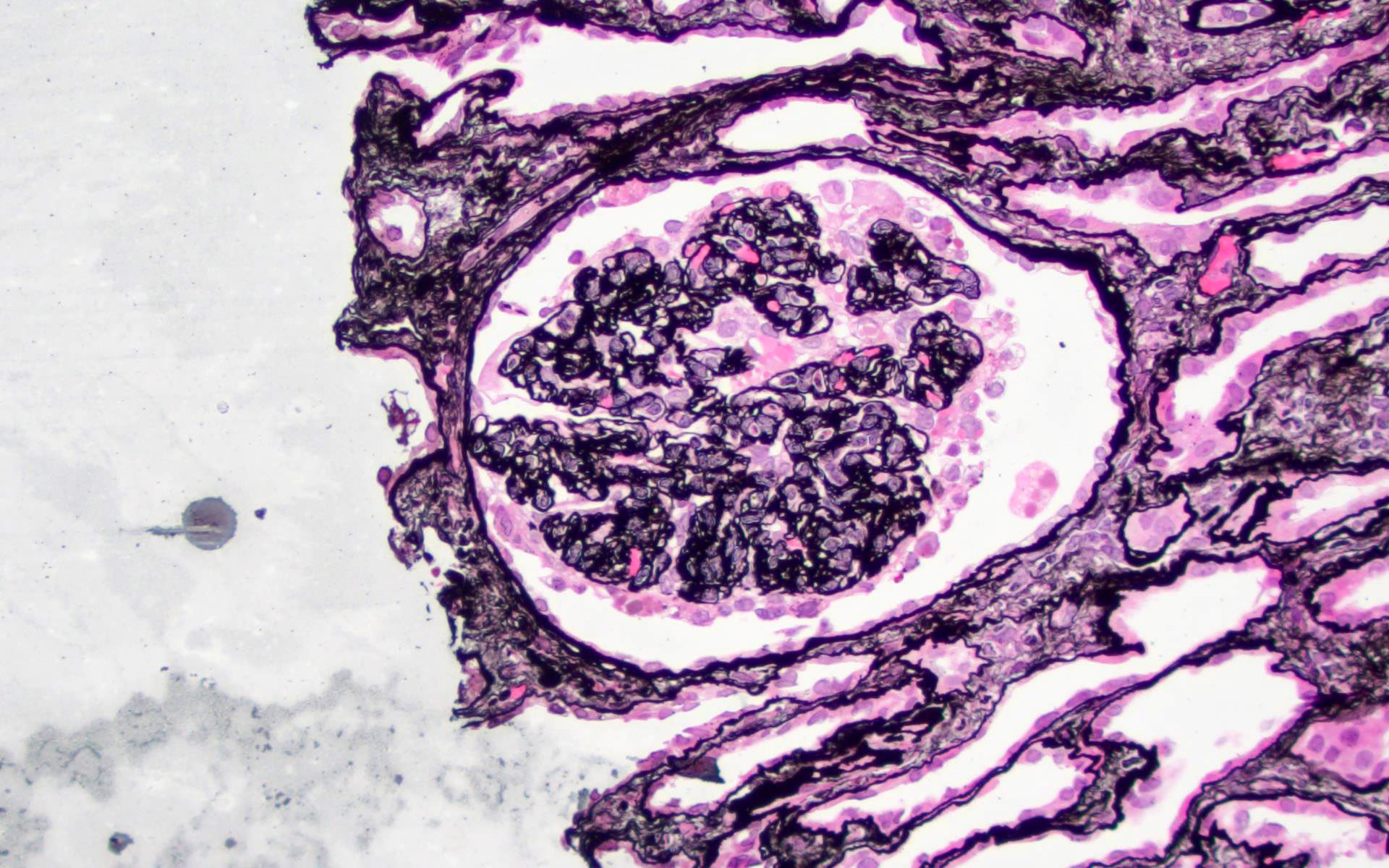
- Collapsing glomerulopathy: collapse of capillary loops, prominence of overlying epithelial cells, some of which may have eosinophilic cytoplasmic droplets
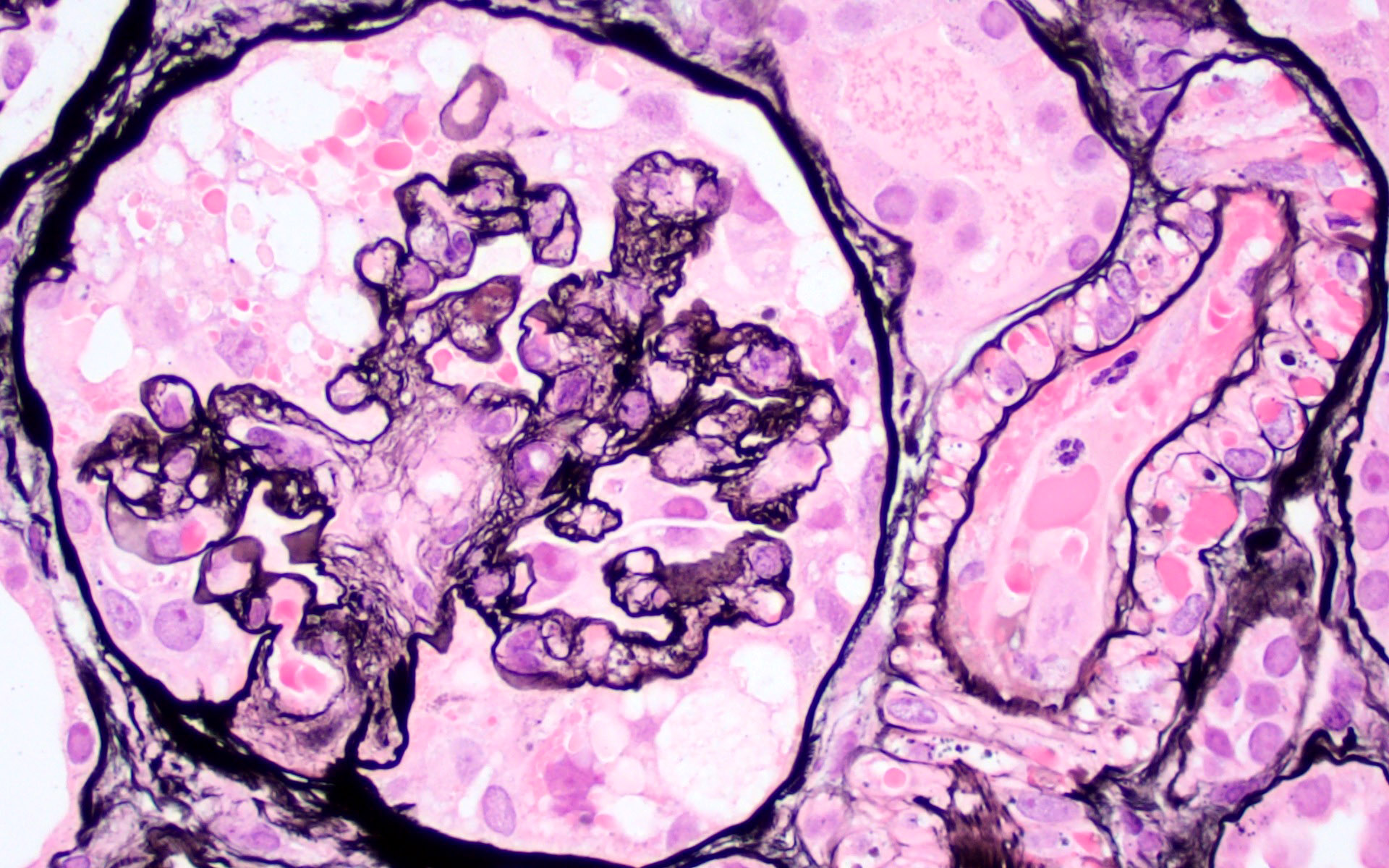
- Thrombotic microangiopathy (TMA): intimal edema or onion skinned appearance of blood vessels, presence of thrombi and sheared red blood cell fragments in blood vessel lumens or trapped in expanded intima; glomeruli may appear shrunken and bloodless
- May occur together with collapsing glomerulopathy
- Myoglobin cast nephropathy and proliferative glomerulonephritis with monoclonal IgG deposits are enriched in this patient population (Kidney Int 2021 Aug 2 [Epub ahead of print])
Microscopic (histologic) images
Immunofluorescence description
- No specific immunofluorescence findings
- May incidentally detect concurrent renal injury processes with immune complexes (e.g. membranous nephropathy, IgA nephropathy, etc.)
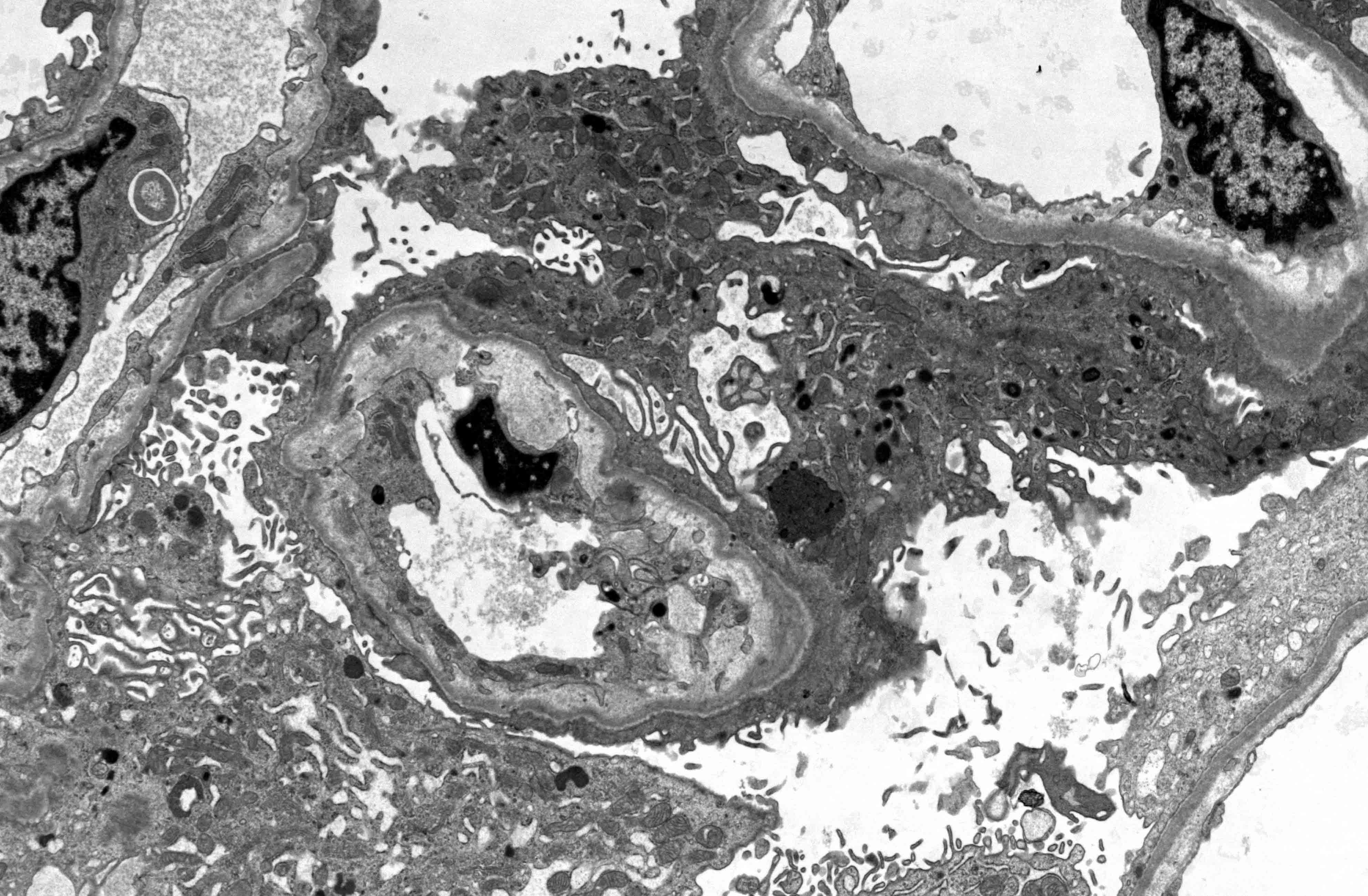
Electron microscopy description
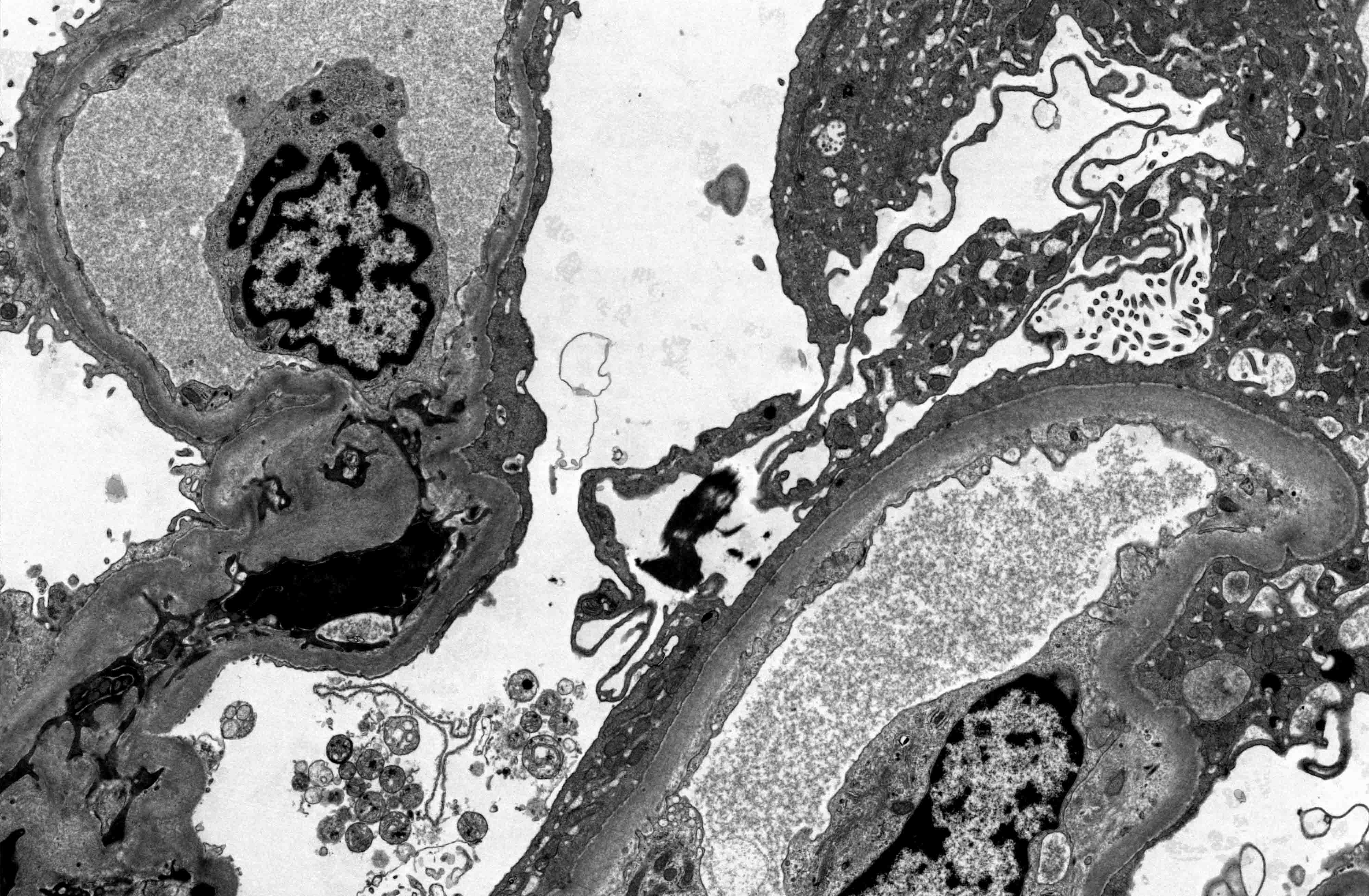
- Collapsing glomerulopathy typically exhibits diffuse effacement of podocyte foot processes
- Thrombotic microangiopathy (TMA) shows expansion of the subendothelial space with electron lucent material and swelling of glomerular endothelial cells, which may lose their fenestrae
- Viral particles have not been conclusively detected in kidney biopsy / autopsy tissue; studies purporting to detect viral particles in the kidney have misidentified normal structures as viral particles (J Pathol 2020;252:346, Histopathology 2021;78:358, J Am Soc Nephrol 2020;31:2223)
- Fabry disease-like myelin figures / zebra bodies were seen in some patients treated with hydroxychloroquine before the drug was no longer recommended for treating COVID-19 (Ultrastruct Pathol 2020;44:519)
- Tubuloreticular inclusions may be seen in some cases (Kidney Int 2020;98:241)
Electron microscopy images
Genetics
- Individuals with high risk APOL1 genotypes (homozygous G1, homozygous G2 or G1 / G2) are most at risk for collapsing glomerulopathy, even with only mild COVID-19 symptoms (Am J Kidney Dis 2021;77:82)
Sample pathology report
- Kidney, biopsy:
- COVID-19 associated nephropathy (COVAN) with features of collapsing glomerulopathy, acute tubular injury and acute endothelial cell injury (see comment)
- Comment: The finding of collapsing glomerulopathy in patients with ongoing or recent COVID-19 infection is highly associated with high risk APOL1 genotypes. Acute tubular injury is a common but nonspecific finding in patients with COVID-19 disease. Acute endothelial cell injury can also be seen with COVID-19, though the mechanisms driving this injury process are unclear.
Differential diagnosis
- Collapsing glomerulopathy (unrelated to COVID-19):
- Associated with other viral infections (HIV, parvovirus B19), medications (bisphosphonates), drugs (heroin)
- Collapse of capillary loops with hypertrophy of overlying epithelial cells / podocytes
- No specific immunofluorescence findings
- Electron microscopy usually shows diffuse effacement of podocyte foot processes, no immune deposits
- Strongly associated with high risk APOL1 genotypes
- Focal and segmental glomerulosclerosis:
- Segmental occlusion of capillary loops with matrix, hyaline or foam cells with attachment to Bowman capsule
- No specific immunofluorescence findings
- Electron microscopy usually shows diffuse effacement of podocyte foot processes, no immune deposits
- Membranous nephropathy:
- Immune complex mediated glomerulopathy presenting with nephrotic syndrome
- Light microscopy shows thickened capillary loops with epimembranous spikes, best seen on Jones methenamine silver stained sections
- Immunofluorescence microscopy shows granular glomerular capillary wall immune deposits staining for IgG, C3, kappa and lambda light chains
- Electron microscopy shows numerous subepithelial immune deposits and diffuse effacement of podocyte foot processes
- Primary / idiopathic membranous nephropathy is associated with circulating antibodies against PLA2R (~70% of cases); minor antigenic targets include THS7DA, NELL1 and others
- Mesangial, subendothelial and extraglomerular immune deposits suggest a secondary form of membranous nephropathy (e.g. lupus, malignancy, infection, drug induced)
- Diabetic nephropathy:
- Early stages show thickened basement membranes and mesangial matrix accumulation / hypercellularity
- Later stages show large Kimmelstiel-Wilson nodules, mesangiolysis and microaneurysm formation
- Severe arteriolar hyalinosis and arteriosclerosis are also common
- Tubular atrophy and interstitial fibrosis usually concomitant with chronic glomerular injury
- No specific immunofluorescence findings
- Electron microscopy shows thickening of glomerular and tubular basement membranes, mesangial matrix expansion, occasional fibrils in the mesangium (diabetic fibrillosis)
- Minimal change disease:
- Usually no changes in glomeruli by light microscopy; may have mild mesangial expansion
- No specific immunofluorescence findings
- Electron microscopy shows diffuse effacement of podocyte foot processes, no immune deposits
- Acute tubular injury:
- Proximal tubules are most commonly affected
- Characterized by loss of brush borders, epithelial attenuation, luminal ectasia, blebbing of epithelial cell cytoplasm, cytoplasmic vacuolization, widening of basolateral interdigitations
- Severe cases can display epithelial cell apoptosis / frank necrosis
- Tubular cells can also display regenerative mitoses and cellular atypia
- No specific immunofluorescence findings
- Acute interstitial nephritis:
- Inflammation and edema of the tubules and interstitium
- Increased numbers of eosinophils suggests an allergic / hypersensitivity etiology (e.g. drug induced)
- Lymphocyte rich acute interstitial nephritis can still have an allergic trigger
Additional references
Board review style question #1
Which of the following statements is true regarding kidney biopsies of patients presenting with COVID-19 associated kidney injury?
- Acute tubular injury is a rare histologic finding
- If present, collapsing glomerulopathy is associated with low risk APOL1 genotypes
- Immune complexes directed against SARS-CoV-2 are detected by immunofluorescence microscopy
- Viral particles are not routinely detected in tubular epithelial cells by electron microscopy
Board review style answer #1
D. Viral particles have not been conclusively detected in kidney biopsy / autopsy tissue. Studies purporting to detect viral particles in the kidney have misidentified normal structures as viral particles. Immune complexes directed against SARS-CoV-2 are not a feature of the disease process. Acute tubular injury is the most frequently found histologic pattern of injury in COVID-19 associated kidney injury. Collapsing glomerulopathy in COVID-19 patients is strongly linked to high risk APOL1 genotypes (J Pathol 2020;252:346, Histopathology 2021;78:358, J Am Soc Nephrol 2020;31:2223).
Comment Here
Reference: COVID-19 associated kidney injury
Comment Here
Reference: COVID-19 associated kidney injury
Board review style question #2
Board review style answer #2
A. APOL1. The image demonstrates a glomerulus with collapsing glomerulopathy, an aggressive form of focal and segmental glomerulosclerosis that can present clinically with nephrotic range proteinuria. COVID-19 patients with high risk APOL1 genotypes (homozygous G1, homozygous G2 or G1 / G2) are most at risk for developing collapsing glomerulopathy even with only mild COVID-19 symptoms (Am J Kidney Dis 2021;77:82).
Comment Here
Reference: COVID-19 associated kidney injury
Comment Here
Reference: COVID-19 associated kidney injury