Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Electron microscopy description | Electron microscopy images | Genetics | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Larqué AB. Minimal change glomerulopathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneyminchange.html. Accessed April 1st, 2025.
Definition / general
- Idiopathic glomerular disease that causes nephrotic syndrome
- Little or no light or immunofluorescent microscopic abnormalities
- Diffuse podocyte foot process effacement on electron microscopy (BMC Nephrol 2018;19:207)
Essential features
- Renal glomeruli appear normal by light and immunofluorescence microscopy
- Extensive effacement of podocyte foot processes by electron microscopy (hallmark)
- Highly selective proteinuria, mainly albuminuria
- Responds well to treatment with corticosteroids (90 - 95%)
Terminology
- Also called minimal change disease, idiopathic nephrotic syndrome, nil disease, lipoid nephrosis and foot process disease
ICD coding
Epidemiology
- Most common type of nephrotic syndrome in children: 70 - 90%; in adults: 11 - 16%
- Peak incidence in children: 2 - 3 years; in adults: 80 - 91 years
- In children, M:F = 2:1; in adults, M = F
- More common in white than in black and Asian patients (Clin J Am Soc Nephrol 2007;2:445)
Sites
- Glomerular disease
Pathophysiology
- Extensive foot process effacement appears to be due to epithelial injury with loss of glomerular anionic charge (Kidney Int 1984;25:696)
- Abnormal T cell and B cell function and immune dysregulation (Pediatr Nephrol 2018;33:573, Clin J Am Soc Nephrol 2016;11:710)
- Unknown circulating factor that triggers podocyte dysfunction has been postulated (Pediatr Nephrol 2018;33:1101)
- Nephrin autoantibodies have been discovered in a subset of adults and children with minimal change disease; this aligns with published animal studies and provides further support for an autoimmune etiology (J Am Soc Nephrol 2022;33:238)
- Minimal change disease, diffuse mesangial hypercellularity and focal segmental glomerulosclerosis may be a continuum of the same disease (Kidney Int 2004;65:1690)
Etiology
- Usually idiopathic, especially in children (Clin J Am Soc Nephrol 2017;12:332)
- Secondary forms due to virus, drugs, allergic reactions, immunologic diseases and neoplasia at all ages (BMC Nephrol 2018;19:162, Intern Med 2014;53:1131, Case Rep Nephrol 2015;2015:987212, J Surg Oncol 2010;102:704)
- Rarely familial (gene mutations: NPHS2, dysferlin) (Semin Nephrol 2003;23:141)
Clinical features
- Nephrotic syndrome
- Proteinuria selective for albumin, causing hypoalbuminemia leading to severe edema
- Lipiduria, hypercholesterolemia but usually no hypertension, no hematuria and no azotemia
- Microhematuria (10 - 30%)
- Can present as acute renal insufficiency in adults (Clin J Am Soc Nephrol 2017;12:332)
- Can present with IgA nephropathy (Clin J Am Soc Nephrol 2014;9:1033)
Diagnosis
- Nephrotic syndrome with little or no light or immunofluorescent microscopic abnormalities
- Diffuse foot process effacement on electron microscopy
Laboratory
- CD80 in urine may be a marker (Pediatr Nephrol 2015;30:309)
Prognostic factors
- Rarely, if ever, leads to end stage renal disease without development of focal segmental glomerulosclerosis
- Adults with minimal change disease and acute renal failure also usually fully recover (Medicine (Baltimore) 2014;93:e300)
- Relapses common and often lead to steroid dependence
Case reports
- 2 and 15 year old boys with steroid responsive nephrotic syndrome complicated by cerebral venous sinus thrombosis (Nefrologia 2015;35:497)
- 29 year old woman with type I neurofibromatosis and complete remission after neurofibroma resection (Korean J Intern Med 2017;32:186)
- 33 year old man with severe chronic sinusitis (Intern Med 2015;54:2373)
- 43 year old man with nephrotic syndrome following the COVID-19 vaccine (BMC Nephrol 2021;22:376)
- 50 year old woman with minimal change disease after a type B influenza infection (BMC Nephrol 2018;19:162)
- 63 year old man with nephrotic syndrome (JNMA J Nepal Med Assoc 2022;60:399)
- 68 year old man with marginal zone MALT lymphoma manifesting as nephrotic range proteinuria (Clin Nephrol 2016;85:184)
Treatment
- Corticosteroids
- Immunosuppressive agents in steroid resistant cases (cyclophosphamide, rituximab, abatacept) (Kidney Int 2013;83:511, Pediatr Nephrol 2015;30:469)
Gross description
- Enlarged, waxy, yellow cortex due to lipid accumulation in proximal tubules
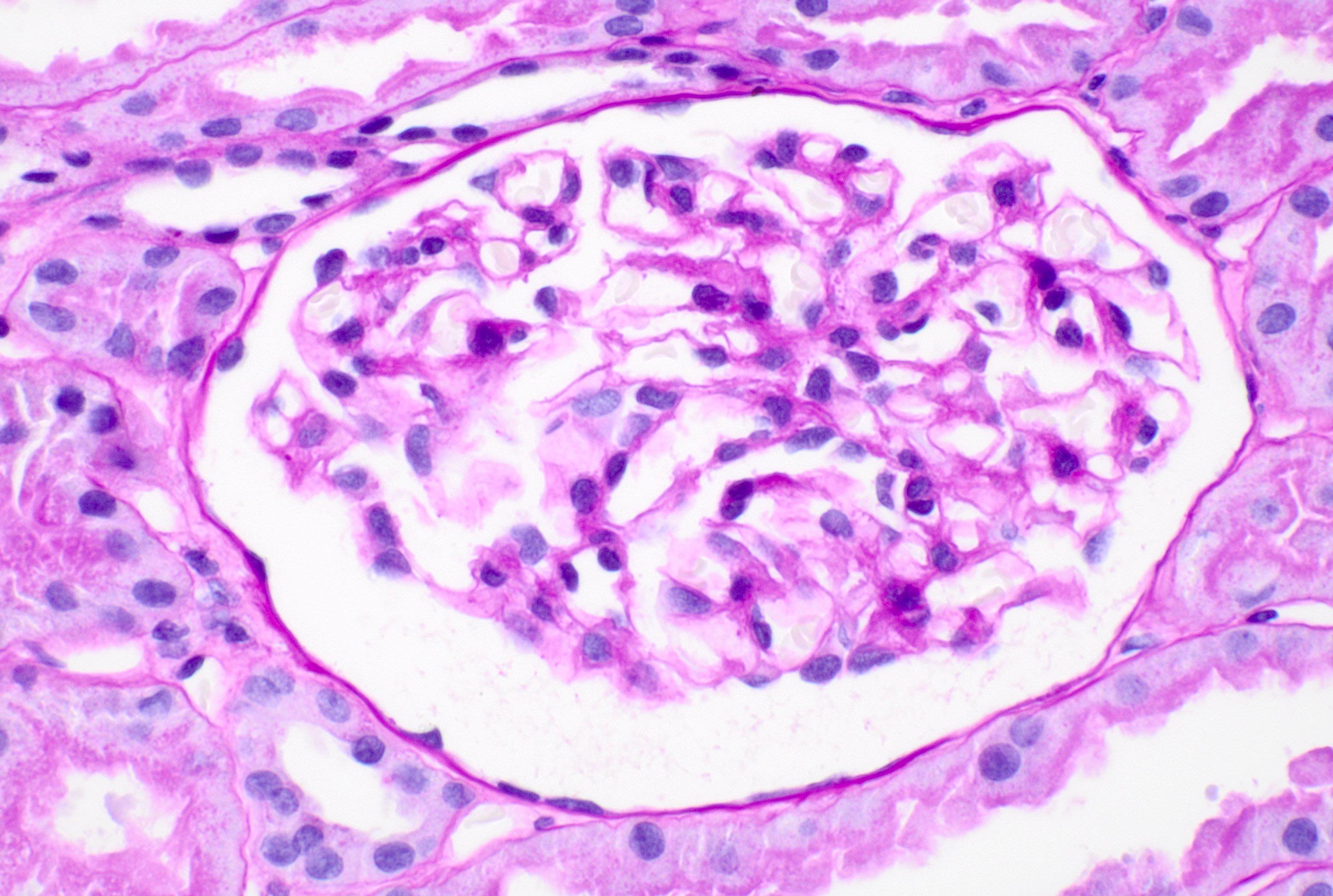
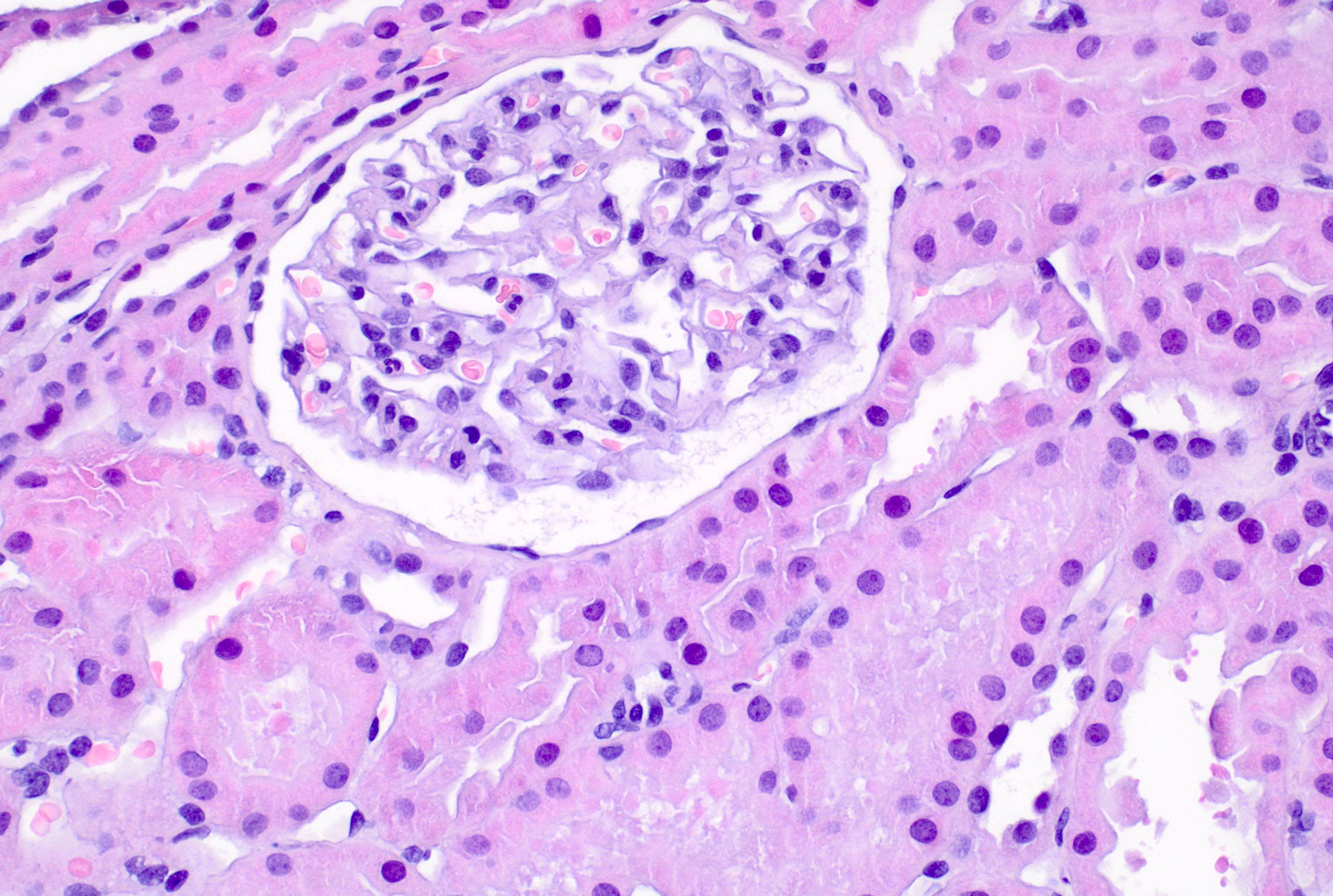
Microscopic (histologic) description
- Glomerulus normal by light microscopy except for variable podocyte hypertrophy
- Protein reabsorption droplets in tubules (Zhou: Silva's Diagnostic Renal Pathology, 2nd Edition, 2017)
Microscopic (histologic) images
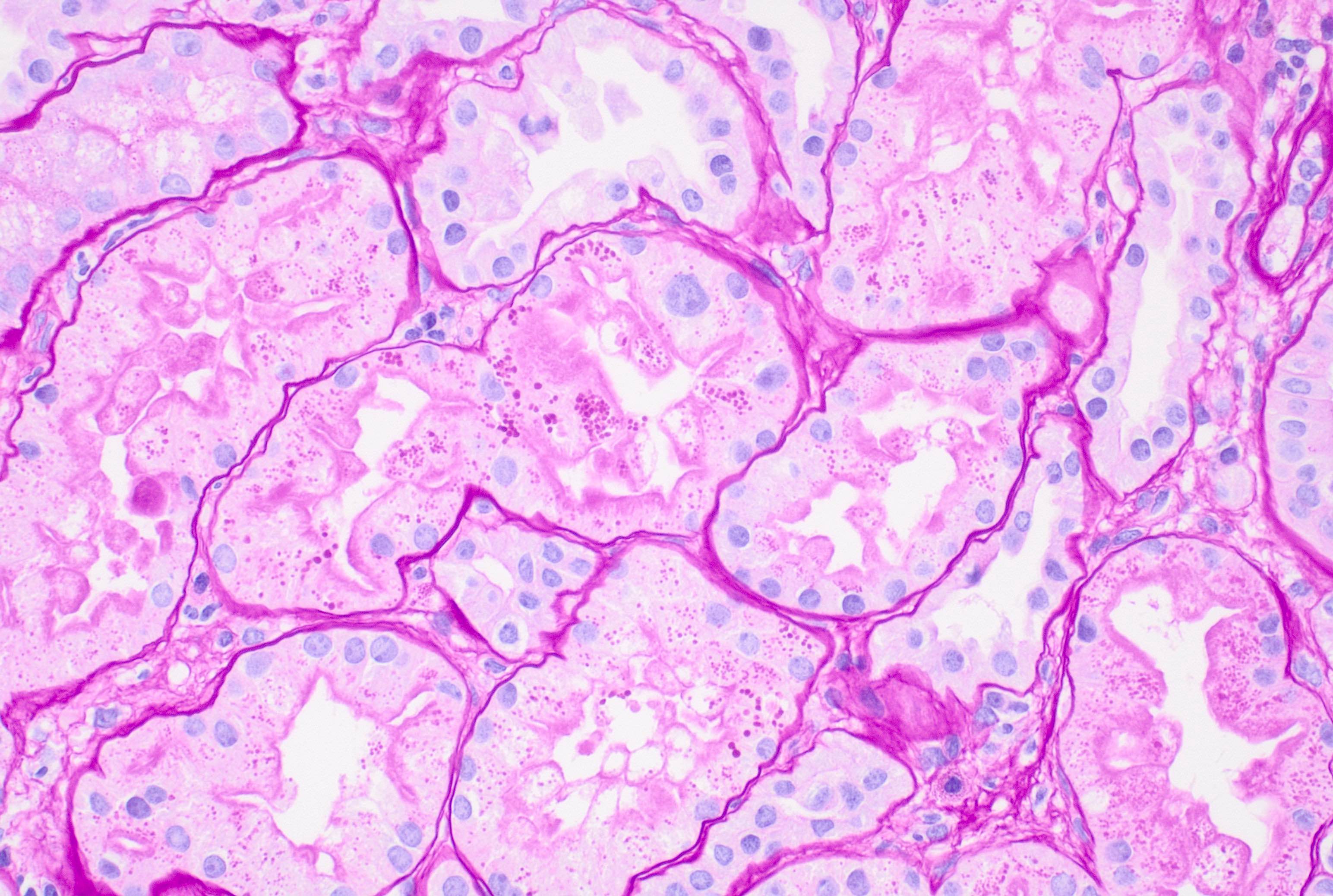
Immunofluorescence description
- Negative except for variable focal IgM with or without C3
- Punctate IgG podocyte staining in a subset of cases associated with antinephrin antibodies (J Am Soc Nephrol 2022;33:238)
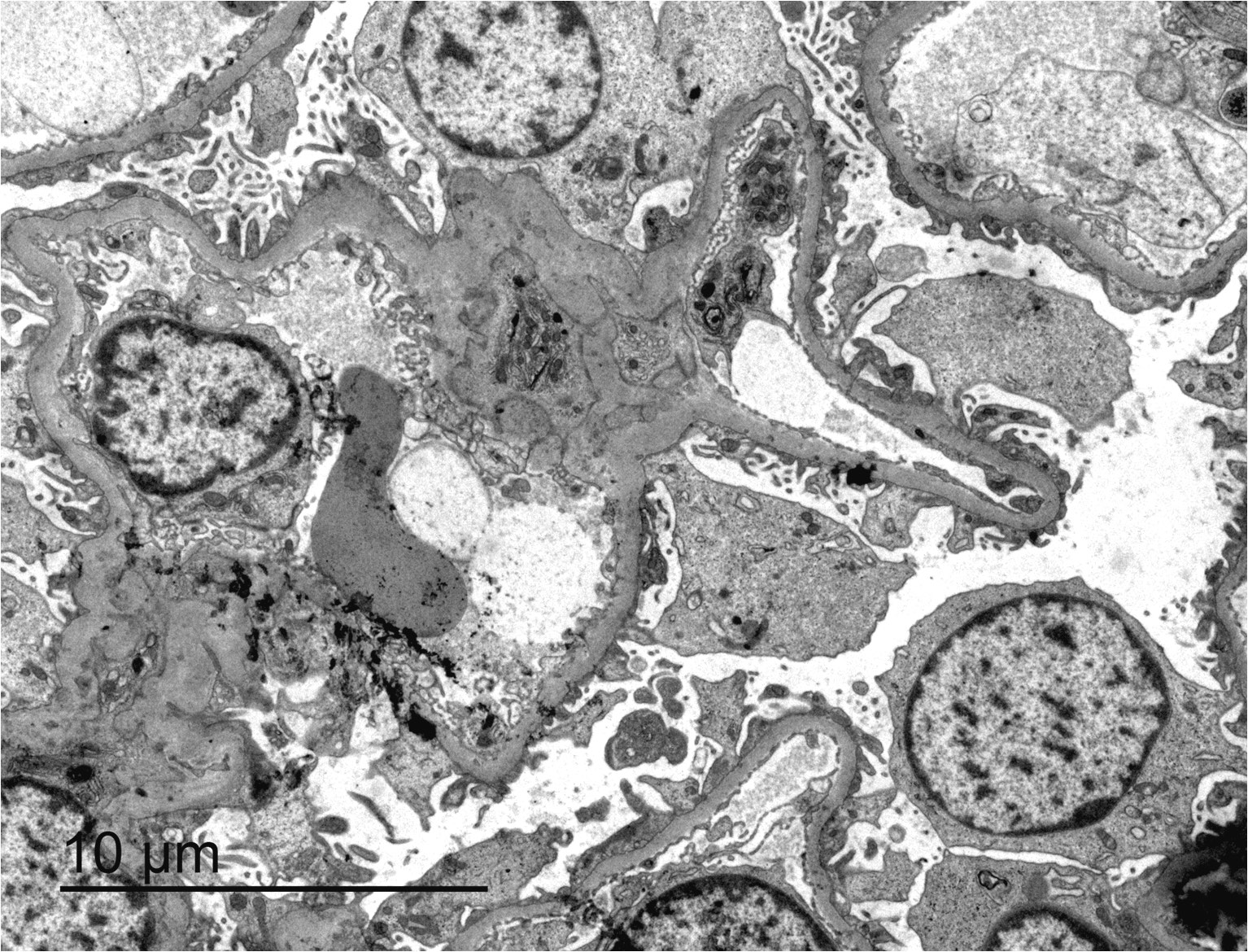
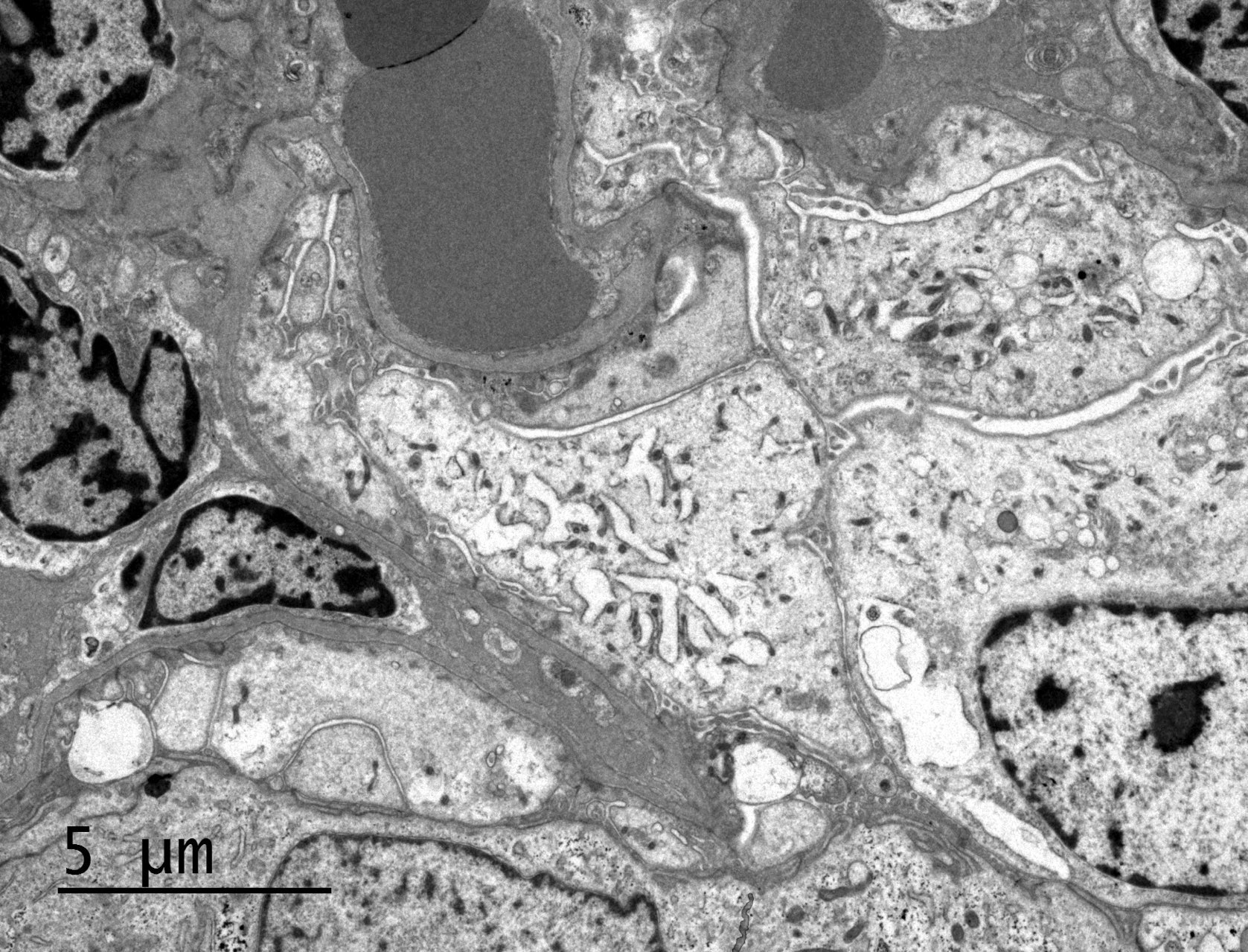
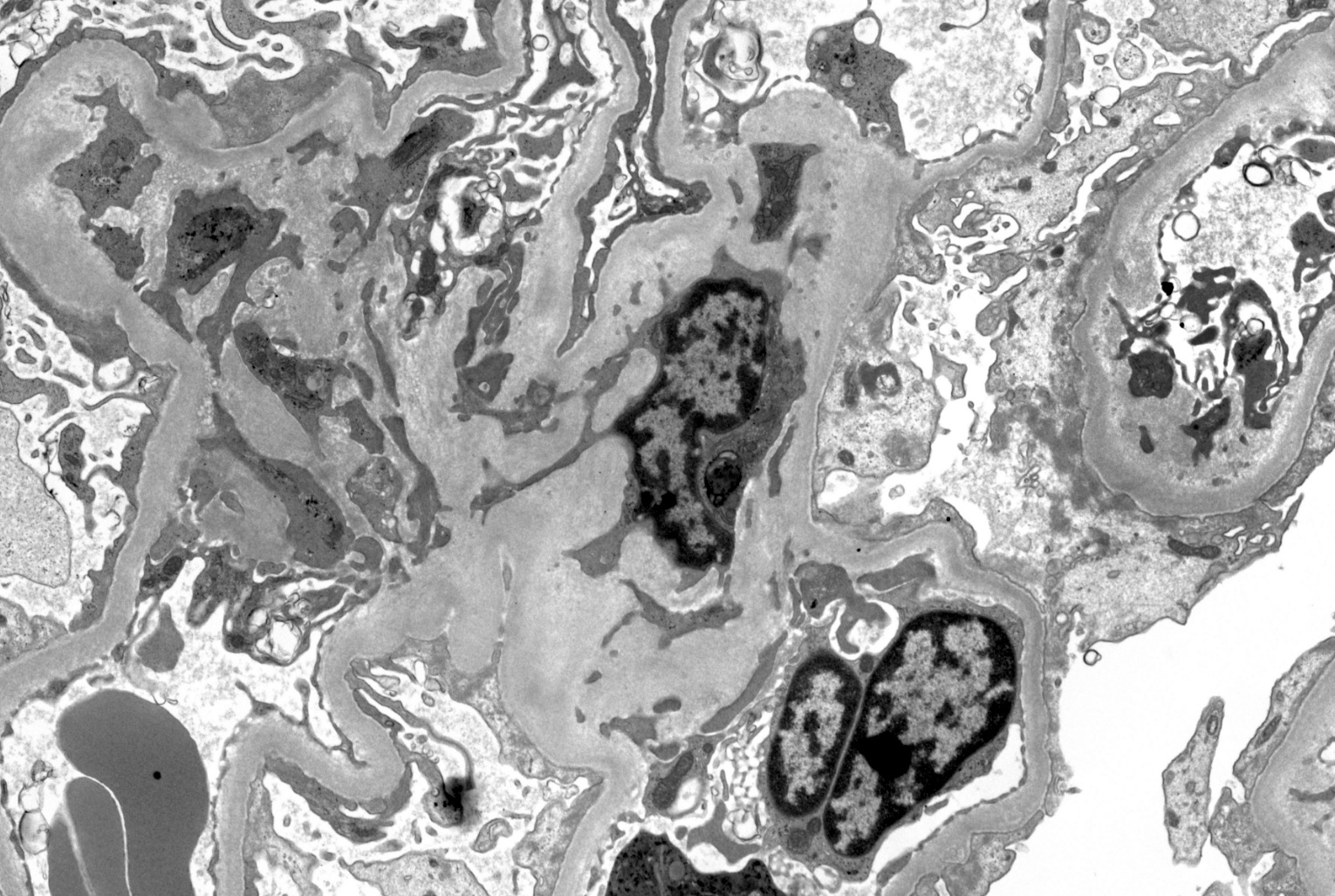
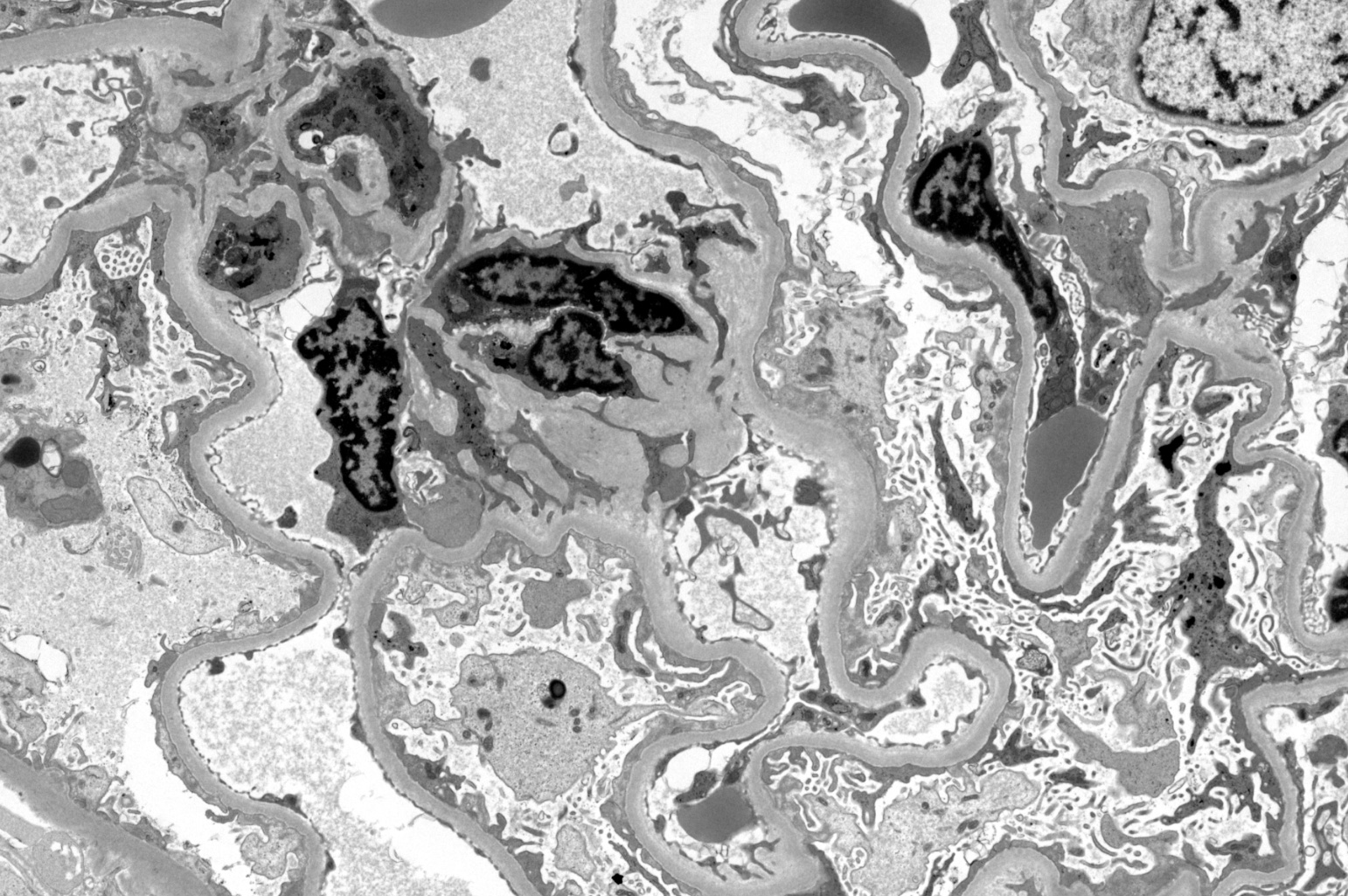
Electron microscopy description
- Extensive foot process effacement (foot processes retract into cell bodies, not actually fusion) (Nephrology (Carlton) 2014;19:392)
- Microvillous transformation of epithelial cells, cyst formation
Electron microscopy images
Genetics
- Rarely familial (Semin Nephrol 2003;23:141, Hum Mol Genet 1995;4:2155, J Am Soc Nephrol 2002;13:388)
- Histologic findings of focal segmental glomerulosclerosis or more rarely minimal change glomerulopathy are a part of the autosomal recessive steroid resistant nephrotic syndrome
- Mutations in NPHS2 have been detected in both familial and sporadic steroid resistant nephrotic syndrome
- NPHS2 gene, formerly SRN1, encodes podocin, a protein that is almost exclusively expressed in glomerular podocytes
- More than 24 genes are currently known to be pathogenic in steroid resistant nephrotic syndrome (Clin J Am Soc Nephrol 2013;8:637)
Sample pathology report
- Left kidney, biopsy:
- Minimal change glomerulopathy
- Adequacy: adequate (cortex 85%, medulla 15%)
- Microscopic description: 19 glomeruli showed normal size and cellularity. There is no interstitial inflammation and no significant interstitial fibrosis or tubular atrophy. Tubules are preserved, without significant evidence of injury. Small arteries and arterioles show minimal interstitial fibrosis. There is no vasculitis.
- Immunofluorescence microscopy:
- Number of glomeruli: 4
- There were no deposits of IgA, IgM, IgG, C3, C1q or fibrin
- Electron microscopy: Extensive effacement of the foot processes covering over 80% of the glomerular capillary surface. The glomerular basement membrane showed normal thickness and a generally smooth contour. No electron dense deposits were noted on the glomerular capillary basement membranes or mesangial areas. The mesangial area contained normal amounts of matrix and cells.
Differential diagnosis
- Focal segmental glomerulosclerosis:
- Segmental hyalinosis or synechiae to Bowman capsule, interstitial fibrosis or tubular atrophy
- Cases with unsampled glomerulosclerosis may be misdiagnosed as minimal change disease
- Secondary causes of minimal change disease (Nephrol Dial Transplant 2003;18:vi52):
- Secondary to drugs, especially nonsteroidal anti-inflammatory drugs
- Features of acute interstitial nephritis support the diagnosis
- May precede or occur simultaneously with the diagnosis of Hodgkin disease or other diseases (hematologic malignancies, thymoma, food allergies, infectious, etc.)
- Genetic disease (Front Med (Lausanne) 2021;8:761600):
- Should be considered in patients with family history of nephrotic syndrome, disease onset within the first 6 months of life or steroid resistant nephrotic syndrome
- Mesangial glomerulonephritis:
- Early mesangial glomerulonephritis can be indistinguishable on light microscopy
- Positive immunofluorescence and electron dense subepithelial deposits on electron microscopy
- Chyluria:
- Normal podocytes with heavy proteinuria
- IgA nephropathy:
- Minimal change disease could be superimposed on IgA nephropathy
- IgM nephropathy:
- Possibly a variant of minimal change disease / focal segmental glomerulosclerosis
- Diffuse, global mesangial staining for IgM (≥ 2+) in cases that otherwise resemble minimal change disease; codeposits of C3 in 30+%
- C1q nephropathy:
- Dominant or codominant mesangial staining for C1q (≥ 2+) by immunofluorescence; other deposits are C3, IgG and IgM
- Light microscopic findings range from normal appearing glomeruli to mesangial proliferation to focal or diffuse endocapillary proliferation and frequently reveal focal segmental glomerulosclerosis
Additional references
Board review style question #1
Which of the following is true about minimal change glomerulopathy?
- Interstitial inflammation and fibrosis are usually absent
- It is the most common type of nephrotic syndrome in adults
- Monoclonal antibody therapy should be the first line therapy
- Pretreatment biopsy is always done
Board review style answer #1
A. Interstitial inflammation and fibrosis are usually absent. Answer B is incorrect because membranous nephropathy is the most frequent cause of nephrotic syndrome in adults. Answer C is incorrect because corticosteroids are the first line therapy. Answer D is incorrect because in the pediatric setting, a renal biopsy is usually not performed if presentation is typical and the patient responds to therapy with oral prednisone at conventional doses.
Comment Here
Reference: Minimal change glomerulopathy
Comment Here
Reference: Minimal change glomerulopathy
Board review style question #2
Which of the following signs and symptoms is common in minimal change disease?
- Azotemia
- Hypertension
- Macrohematuria
- Selective proteinuria
Board review style answer #2
D. Selective proteinuria. Minimal change disease usually presents with proteinuria selective for albumin, causing hypoalbuminemia leading to severe edema. Answers A - C are incorrect because minimal change disease is associated with lipiduria and hypercholesterolemia but usually no hypertension, no hematuria and no azotemia.
Comment Here
Reference: Minimal change glomerulopathy
Comment Here
Reference: Minimal change glomerulopathy
Board review style question #3
Board review style answer #3
D. Podocyte foot process effacement. Minimal change disease is an idiopathic glomerular disease that causes nephrotic syndrome with little or no immunofluorescent microscopic abnormalities. The pathologic hallmark of disease is absence of visible alterations by light microscopy and effacement of foot processes by electron microscopy.
Comment Here
Reference: Minimal change glomerulopathy
Comment Here
Reference: Minimal change glomerulopathy