Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Negative stains | Electron microscopy description | Genetics | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Bashir A, Memon AH. Malignant hypertension and accelerated nephrosclerosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneymalignanthyper.html. Accessed April 3rd, 2025.
Definition / general
- Also called hypertensive emergency, malignant nephrosclerosis
- Severe vascular damage caused by malignant hypertension, characterized by fibrinoid necrosis and thrombosis in renal arterioles and glomeruli
Essential features
- Malignant (accelerated) hypertension is a medical emergency and is characterized by extremely high blood pressure (≥ 180/120 mmHg)
- Men are affected more commonly than women
- ~50% of cases have a history of arterionephrosclerosis
- Histological features include mucoid widening with red cell fragments in subacute stage, fibrinoid necrosis of arterioles in acute stage and onion skin thickening of arteriolar walls in chronic stage
- Malignant hypertension has a 2 year survival rate of 20% if left untreated (J Hypertens 2023;41:453)
Terminology
- Accelerated nephrosclerosis
- Malignant nephrosclerosis
- Malignant / accelerated hypertension
- Malignant hypertensive nephropathy
ICD coding
- ICD-10
- I10.10 - malignant essential hypertension without mention of hypertensive urgency
- I10.11 - malignant essential hypertension with mention of hypertensive urgency
- I12.9 - hypertensive chronic kidney disease with stage 1 through 4 chronic kidney disease or unspecified chronic kidney disease
- I12.0 - hypertensive chronic kidney disease with stage 5 chronic kidney disease or end stage renal disease
Epidemiology
- Average age of diagnosis is 40 years
- Men are affected more commonly than women
- More common in people of African decent (Kidney Int Rep 2016;1:10, Nephrol Dial Transplant 2023;38:1848)
- ~50% of cases have a history of arterionephrosclerosis
- More common in patients with adrenal gland disorders (e.g., pheochromocytoma)
- Pre-existing kidney disease is a significant risk factor
Sites
- Renal arterioles and small arteries
- Glomeruli
- Tubulointerestitium
Pathophysiology
- High blood pressure causes shear stress, leading to cellular hyperplasia, thickening and narrowing of arterioles
- Endothelial injury triggers inflammation and fibrinoid necrosis (Nephrol Dial Transplant 2015;30:1833)
- Loss of elastic fibers weakens vessel walls, making them prone to rupture
- Arterioles spasm, forcing blood through damaged areas, causing further injury
- Microhemorrhages appear as red blotches on the kidney surface
- Reduced blood flow results in ischemia (oxygen deprivation) and edema (swelling)
- Damaged vessels are prone to forming microthrombi, further impairing circulation
- Persistent hypertension leads to acute kidney injury, quickly progressing to kidney failure if untreated (Hypertens Res 2024;47:3383)
- Abnormalities in the renin angiotensin system have been postulated to play a role (J Hum Hypertens 2014;28:74)
- Hypertension associated thrombotic microangiopathy (TMA) is a diagnosis of exclusion, requiring complement studies and ADAMTS13 testing to rule out atypical hemolytic uremic syndrome (aHUS) / thrombotic thrombocytopenic purpura (TTP) (Kidney Int 2017;91:1420)
Etiology
- MYH9 / APOL1 gene associated with high risk (Presse Med 2012;41:116)
- Renin secreting neoplasms (CEN Case Rep 2023;12:116)
- Hypertension associated TMA (Kidney Int 2017;91:1420)
Clinical features
- Associated with persistent elevated blood pressure and ischemic organ damage
- Severe headache, nausea, vomiting, chest pain, visual disturbances, transient cortical blindness, seizures and congestive heart failure
- Severe retinopathy with hemorrhages, exudates and papilledema
- May have proteinuria, even nephrotic range, oliguria with progressive renal insufficiency and renal failure (J Am Coll Cardiol 2024;83:1688)
Diagnosis
- Diagnosis is usually made by clinical presentation of extremely high blood pressure (≥ 180/120 mmHg) along with deranged renal function tests
- Renal biopsy is the gold standard for characteristic vascular and glomerular changes
Laboratory
- Raised serum creatinine levels at presentation
- Azotemia
- Proteinuria
- Hematuria with red cell casts
- Reference: CEN Case Rep 2023;12:116
Radiology description
- Renal ultrasound shows reduced size of kidneys in chronic cases
- Renal cortical thinning with increased parenchymal echogenicity, which reflects sclerosis and fibrosis (Niger J Clin Pract 2018;21:578)
- Simple renal cysts and renal artery stenosis are common findings in hypertension (J Family Med Prim Care 2020;9:2411)
Prognostic factors
- Depends on early diagnosis, duration and severity of hypertension (Expert Opin Pharmacother 2010;11:2675)
- Also depends on underlying conditions (diabetes, connective tissue disorder, chronic kidney disease)
- Extent of kidney damage is a risk predictor for long term morbidity in malignant hypertension (Indian J Nephrol 2021;31:467)
- Malignant hypertension has a 2 year survival rate of 20% if left untreated (J Hypertens 2023;41:453)
Case reports
- 28 year old man presented with dyspnea and hypertension (Medicine (Baltimore) 2022;101:e30416)
- 37 year old Japanese man with severe hypertension and proteinuria (CEN Case Rep 2023;12:116)
- 38 year old African American man with thrombotic microangiopathy (BMJ Case Rep 2017;2017:bcr2017220457)
- 41 year old man with diffuse alveolar hemorrhage (Clin Nephrol Case Stud 2020;8:53)
Treatment
- Immediate blood pressure reduction by intravenous / oral antihypertensive medication (Cardiol Rev 2010;18:102)
- Hemodialysis
- Kidney transplant
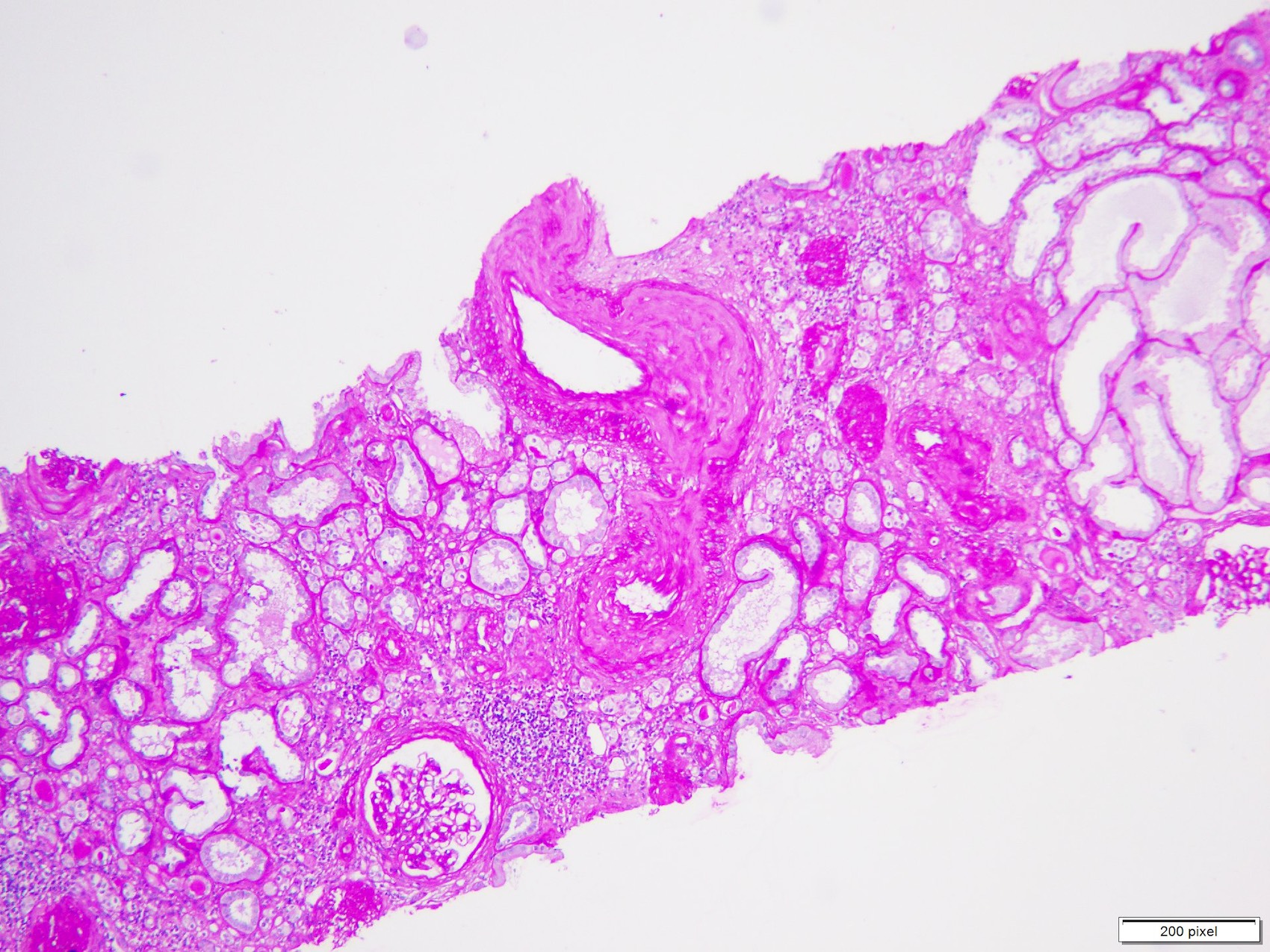
Gross description
- Petechial hemorrhages on the cortical surface of the kidney secondary to arteriolar necrosis, giving rise to a flea bitten appearance
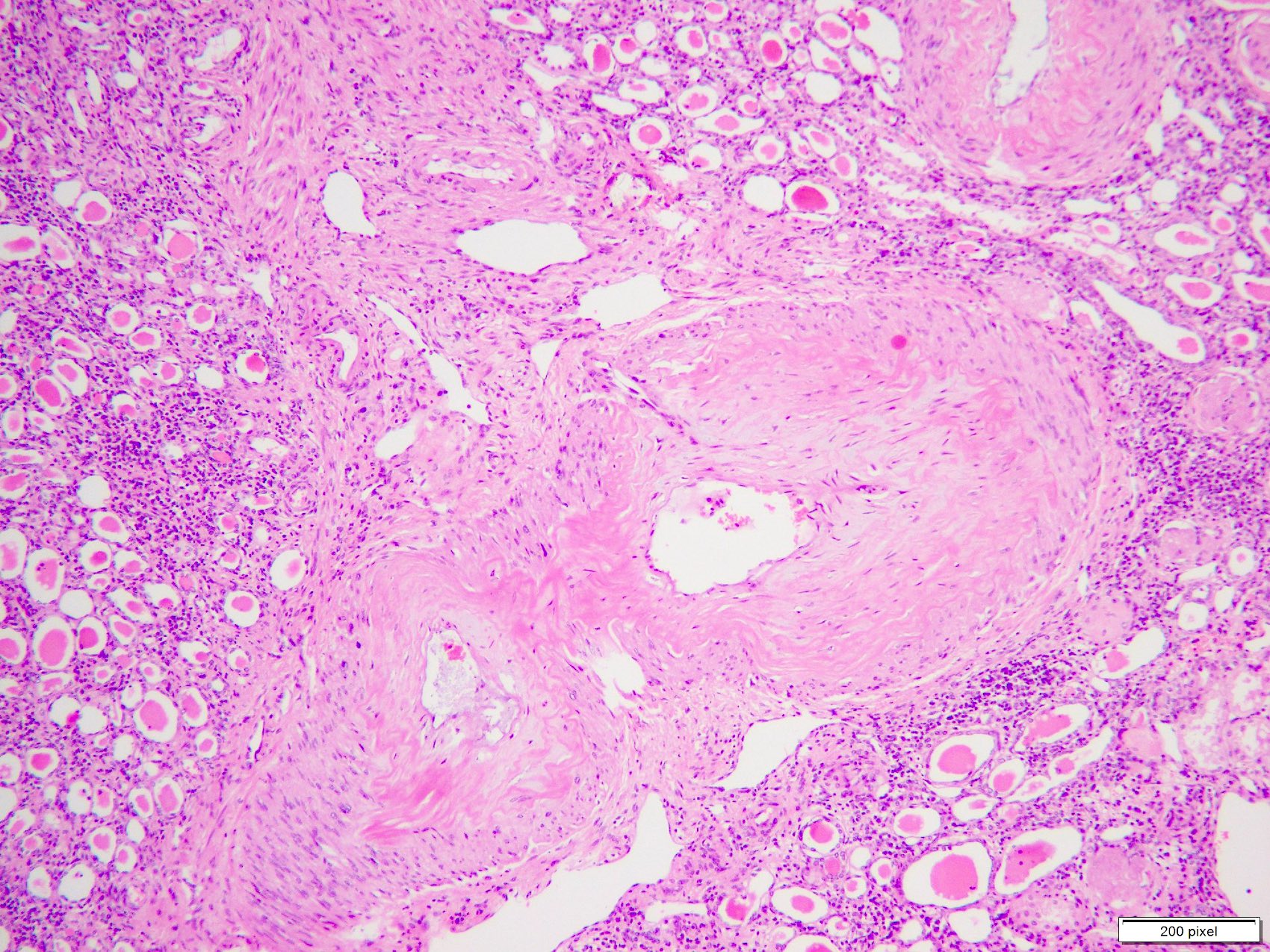
Microscopic (histologic) description
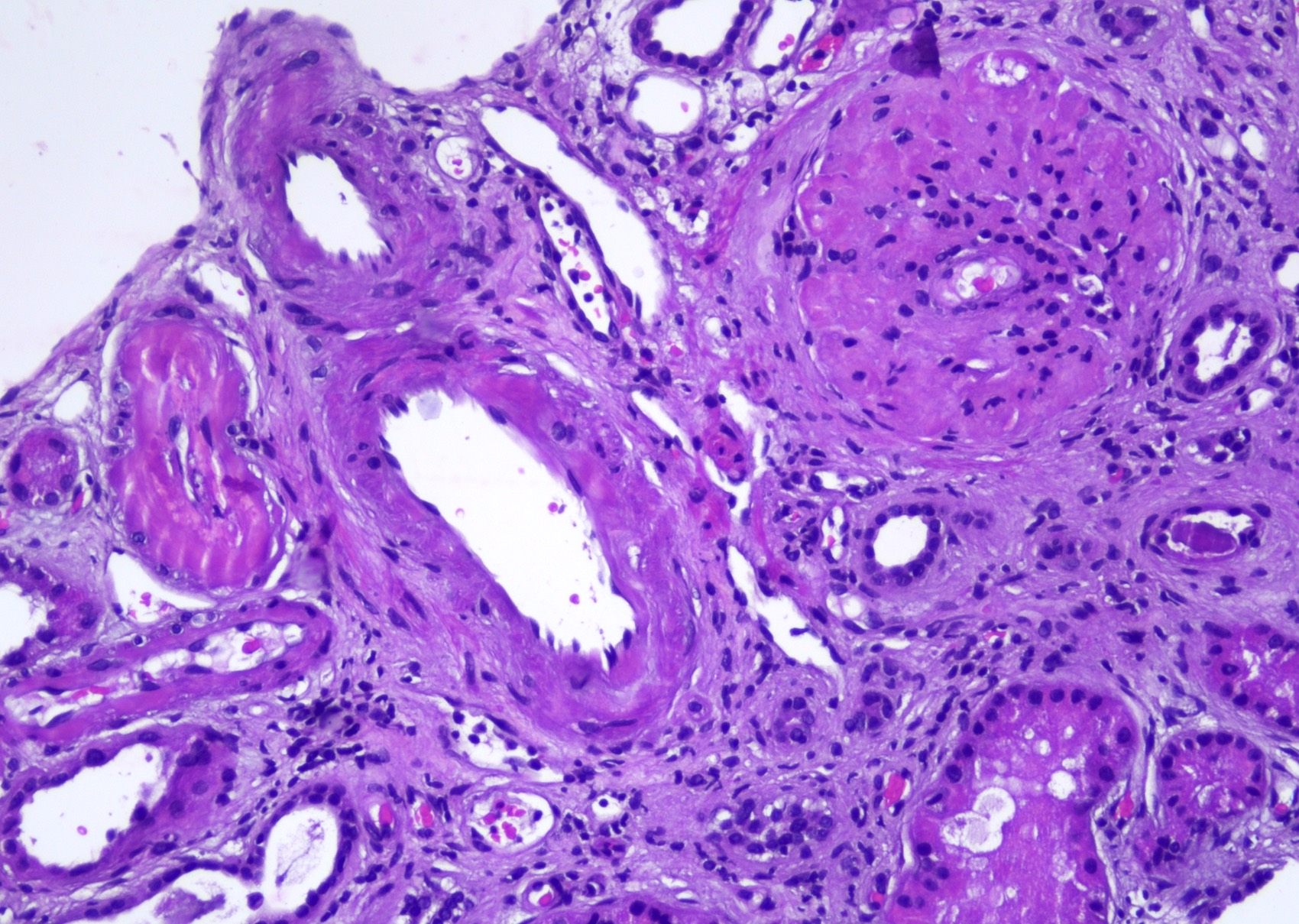
- Edematous or mucoid intimal thickening
- Prominent intimal edema, more frequent in interlobular and arcuate arteries, with narrowing of the lumen
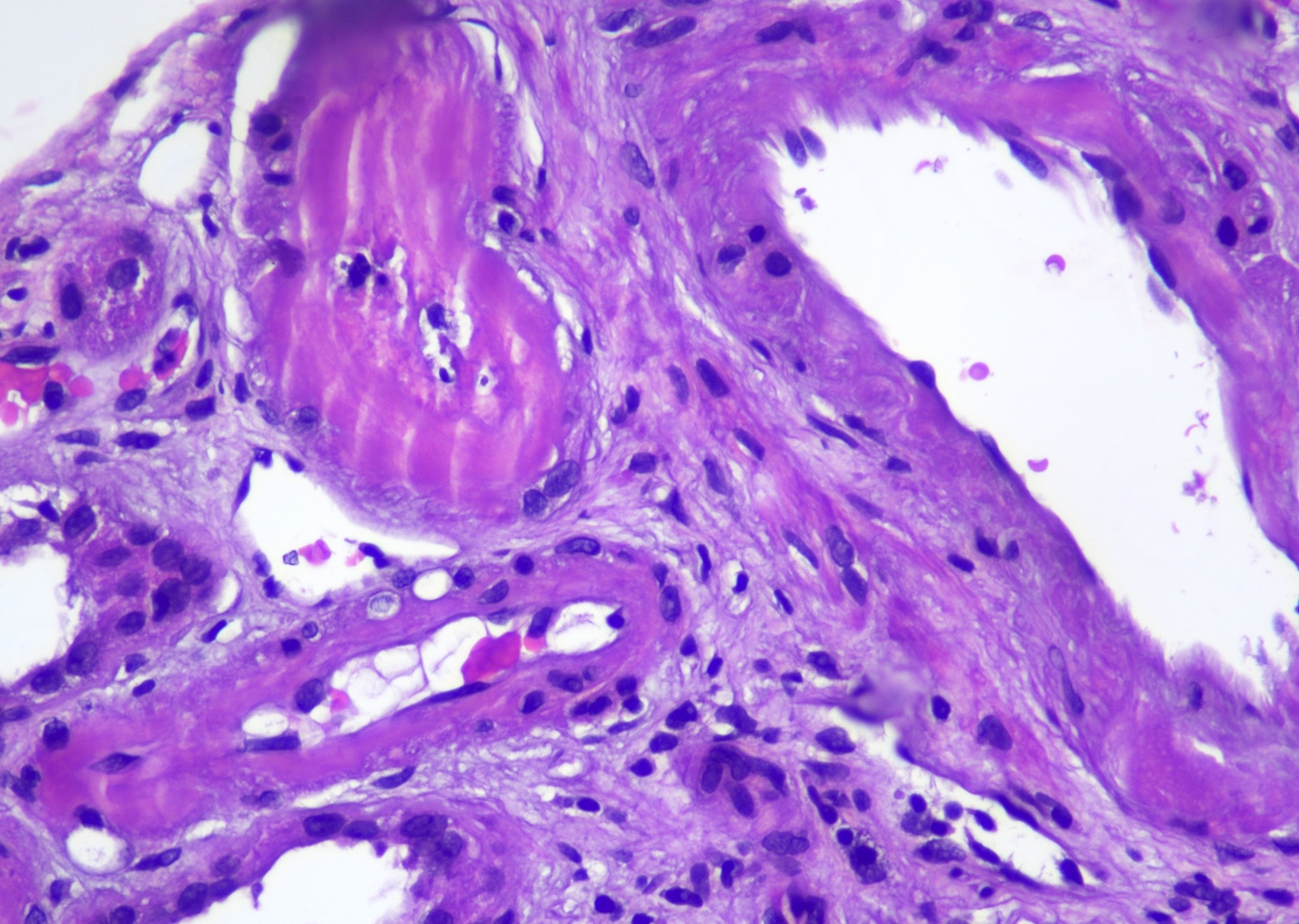
- Fibrinoid necrosis (variable)
- Fibrinoid necrosis of arterioles and small arteries may be present, characterized by eosinophilic fibrin deposition within vessel walls, although not always observed
- This affects afferent rather than efferent arterioles (Nephrol Dial Transplant 2023;38:1848)
- It may extend contiguously into the hilar regions of glomeruli
- Fibrinoid material may contain erythrocyte fragments and nuclear debris
- Fibrin thrombi may be seen in the lumen of affected vessels
- Hyperplastic arteriolitis
- Concentric, onion skin thickening of arteriolar walls due to subendothelial edema and smooth muscle cell proliferation
- Luminal narrowing or complete obstruction
- Glomerular changes
- Glomeruli may be normal or may show focal and segmental necrosis and congestion
- With chronic ischemic injury, there is corrugation of the glomerular basement membrane with occasional segmental duplication
- Global or less frequently segmental glomerular sclerosis and ischemic collapse of glomeruli secondary to arteriolar obstruction (Indian J Nephrol 2021;31:467)
- Enlarged and hypertrophic glomeruli in areas where blood flow remains intact
- Tubulointerstitial damage
- Extensive tubulointerstitial fibrosis and tubular atrophy, often involving a significant portion of the renal cortex
- Histological features reflect severe vascular injury and downstream ischemic damage caused by the elevated pressures characteristic of malignant hypertension (J Am Heart Assoc 2022;11:e023397)
- Histological changes are usually superimposed on lesions of benign arterionephrosclerosis, which include arterial medial hypertrophy, subintimal fibrosis, afferent arteriolar hyalinosis and global glomerulosclerosis with proportional tubulointerstitial fibrosis
Microscopic (histologic) images
Immunofluorescence description
- No immunoglobulin deposition is seen; occasionally there is mild nonspecific trapping of immunoglobulins like IgM and complement factors like C3 in glomeruli and arterioles (Exp Ther Med 2013;6:1243)
- Areas of arteriolar or glomerular fibrinoid necrosis and thrombosis may demonstrate positivity for fibrinogen
Positive stains
- PAS, Masson trichrome and Jones silver stains highlight concentric subendothelial thickening of arterioles
- Jones silver stain highlights glomerular ischemic changes and fibrinoid necrosis
- Fibrinoid necrosis is fuchsinophilic with red-pink staining on Masson trichrome stain
- Masson trichrome is also used to assess interstitial fibrosis
Negative stains
- Congo red stain
Electron microscopy description
- Thickening and corrugation of glomerular basement membrane and subendothelial edema with lucent expansion of subendothelial zone
- Segmental cellular interposition related to chronic endothelial injury
- Foot processes may show effacement in areas of secondary segmental sclerosis
- Fibrin tactoids may be visualized
- No electron dense deposits are seen (Medicine (Baltimore) 2022;101:e30416)
Genetics
- Risk variants G1 and G2 of apolipoprotein L1 (APOL1) (Clin J Am Soc Nephrol 2021;16:294)
- MYH9 gene polymorphisms (Nefrologia 2010;30:687)
Sample pathology report
- Right kidney, ultrasound guided trucut biopsy:
- Malignant nephrosclerosis (see comment)
- Comment: The findings are consistent with malignant nephrosclerosis secondary to severe, uncontrolled hypertension. The vascular changes indicate severe endothelial injury and downstream ischemic damage. The extent of tubulointerstitial fibrosis suggests chronicity, while fibrinoid necrosis indicates ongoing vascular insult. Clinical correlation with blood pressure history and laboratory data, including renal function tests, is recommended.
Differential diagnosis
- Arterionephrosclerosis:
- Mucoid intimal change, red blood cell fragmentation, fibrinoid necrosis in acute phase and onion skinning of arterioles in the chronic phase are characteristically seen in malignant hypertension and absent in benign arterionephrosclerosis
- Systemic sclerosis:
- Similar biopsy findings as malignant hypertension; requires clinical history to distinguish between etiologies
- Necrotizing vasculitis (such as polyarteritis nodosa and microscopic polyangiitis):
- Both show fibrinoid necrosis of the vessel wall
- Systemic vasculitis is usually accompanied by substantial leukocyte infiltration
- Thrombotic microangiopathy:
- Malignant hypertension can also show fibrin thrombi similar to other causes of thrombotic microangiopathy, including hemolytic uremic syndrome, thrombotic thrombocytopenic purpura, systemic sclerosis crisis, antiphospholipid antibody syndrome and acute postpartum renal failure
- Vascular changes are prominent in patients with malignant hypertension especially mucoid intimal change and hyperplasia of arterial vessel walls
- Correlation with history and laboratory investigations is mandatory for reaching an accurate diagnosis
Board review style question #1
A 60 year man with known hypertension for 20 years presented to the nephrology clinic with uncontrolled blood pressure, proteinuria and increased creatinine level. Renal biopsy was performed that showed changes consistent with malignant nephrosclerosis, as shown in the image above. What is the most characteristic histological feature of this entity?
- Fibrinoid necrosis of arterioles
- Global glomerulosclerosis
- Hyalinosis of arterioles
- Medial hypertrophy
- Subintimal fibrosis
Board review style answer #1
A. Fibrinoid necrosis of arterioles. Hypertensive associated kidney disease can show all hyalinosis of arterioles, medial thickening, subintimal fibrosis and global sclerosis; however, the most characteristic histological feature associated with malignant hypertension is fibrinoid necrosis of the vessel wall.
Answer D is incorrect because medial hypertrophy can be present in benign arterionephrosclerosis.
Answer C is incorrect because hyalinosis of arterioles can be seen in both benign arterionephrosclerosis and diabetic nephropathy.
Answer E is incorrect because subintimal fibrosis can be seen with benign arteriolonephrosclerosis.
Answer B is incorrect because global glomerulosclerosis is a nonspecific diagnosis and can be seen in a variety of chronic kidney diseases.
Comment Here
Reference: Malignant hypertension and accelerated nephrosclerosis
Comment Here
Reference: Malignant hypertension and accelerated nephrosclerosis
Board review style question #2
A 50 year old woman with a long history of hypertension presented with mild hematuria and moderate proteinuria. A renal biopsy was performed, which showed thickened vessels with hyalinosis and mucoid change, patchy glomerulosclerosis and moderate tubulointerstitial scarring. What are the expected immunofluorescence findings in this patient?
- C1q deposits in mesangium
- Granular C3 deposits in mesangium
- IgG granular deposits along the capillary loop
- Mesangial IgA positivity
- Trapping of IgM and C3 in sclerotic segments
Board review style answer #2
E. Trapping of IgM and C3 in sclerotic segments. Malignant nephrosclerosis can show nonspecific trapping for IgM and C3 in sclerotic segments. Necrotic vessels and glomeruli may stain for fibrinogen.
Answer D is incorrect because mesangial IgA positivity is seen in cases of IgA nephropathy.
Answer B is incorrect because granular C3 deposits in mesangium are seen with C3 glomerulopathies and postinfectious glomerulonephritis.
Answer C is incorrect because IgG granular deposits along the capillary loop are seen in membranous glomerulopathy.
Answer A is incorrect because C1q deposits in mesangium are seen in cases of C1q nephropathy.
Comment Here
Reference: Malignant hypertension and accelerated nephrosclerosis
Comment Here
Reference: Malignant hypertension and accelerated nephrosclerosis