Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Velagapudi RK, Paueksakon P. Light chain cast nephropathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneylightchaincastnephropathy.html. Accessed December 25th, 2024.
Definition / general
- Generically included under plasma cell dyscrasias or dysproteinemias affecting the kidney
- Myeloma defining event that results from precipitation of monoclonal light chains in distal, nephron forming casts
- May coexist with other manifestations of the monoclonal light chains, such as amyloidosis, light chain proximal tubulopathy or light chain deposition disease
Essential features
- Pathognomic appearance of casts with angulated and fractured appearance, associated with syncytial giant cell reaction and chronic interstitial nephritis (Am J Kidney Dis 2016;67:e17)
- Clonal staining of casts by immunofluorescence or immunohistochemistry for either kappa or lambda
Terminology
- Also called myeloma cast nephropathy, myeloma kidney or Bence Jones cast nephropathy
ICD coding
Epidemiology
- ~90% of patients with light chain cast nephropathy have overt myeloma
- Age: median age of 66 years
- Gender: M:F = 3:2
Sites
- Kidney, tubulointerstitial disease
Pathophysiology
- Mechanism by which urinary light chains (Bence Jones proteins) lead to kidney failure is incompletely understood
- It can be because of direct toxicity of the light chains or secondary to obstruction (J Clin Med 2021;10:3871)
- When light chains excessed the threshold of reabsorption in the proximal tubules, they are delivered to the distal tubules and collecting ducts
- Here they form casts as a result of coaggregation of light chains and Tamm-Horsfall proteins (uromodulin) produced by the thick ascending limb of the loop of Henle
- These casts lead to kidney injury and obstruction by incompletely understood mechanisms
Etiology
- Plasma cell dyscrasia leading to overproduction of mutated monoclonal light chains
- Precipitating factors include dehydration, hypercalcemia, use of nephrotoxic drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs), contrast media or infections (Int J Nephrol Renovasc Dis 2022;15:173)
Clinical features
- Patients present with acute kidney function deterioration / injury or frank kidney failure or nephrotic range proteinuria
- Most common cause of acute kidney injury (AKI) in patients with myeloma
- It is seen in approximately half of patients with multiple myeloma who have renal disease (Int J Nephrol Renovasc Dis 2022;15:173)
- On the other hand, ~90% of patients with light chain cast nephropathy have overt myeloma (Colvin: Diagnostic Pathology - Kidney Diseases, 4th Edition, 2023)
- It can also be seen in patients with monoclonal protein, who do not meet hematologic criteria for multiple myeloma
Diagnosis
- Patients frequently have proteinuria that is predominantly composed of light chains (Bence Jones proteins) and can be nephrotic range
- Routine urinalysis using a dipstick fails to pick up monoclonal protein as it detects albuminuria rather than light chains
Laboratory
- May show a monoclonal protein on serum and urine protein electrophoresis
- Increased serum or urine free light chains (Clin J Am Soc Nephrol 2016;11:2273)
Prognostic factors
- Renal function improves in ~50% associated with reduction of free light chains
- 5 year survival rate 20 - 25%
- End stage kidney disease has major impact on survival: median survival with renal recovery is 43 months and is around 8 months without renal recovery (Blood 2020;135:1833)
Case reports
- 57 year old man with new onset acute kidney injury, anemia and new diagnosis of multiple myeloma (Case Rep Hematol 2022;2022:7531142)
- 57 and 72 year old men with multiple myeloma and acute kidney injury (BMC Nephrol 2021;22:42)
- 64 year old man with diastolic heart failure and chronic kidney disease of unknown etiology (J Community Hosp Intern Med Perspect 2019;9:319)
- 65 year old woman with generalized weakness and low back ache (Indian J Nephrol 2019;29:204)
- 73 year old man with 2 week history of oliguria (Korean J Intern Med 2021;36:1025)
Treatment
- Reduction of circulating light chains by targeting plasma cell dyscrasia
- Plasmapheresis to decrease the concentration of circulating light chains
- Supportive care with hydration and reduction of hypercalcemia
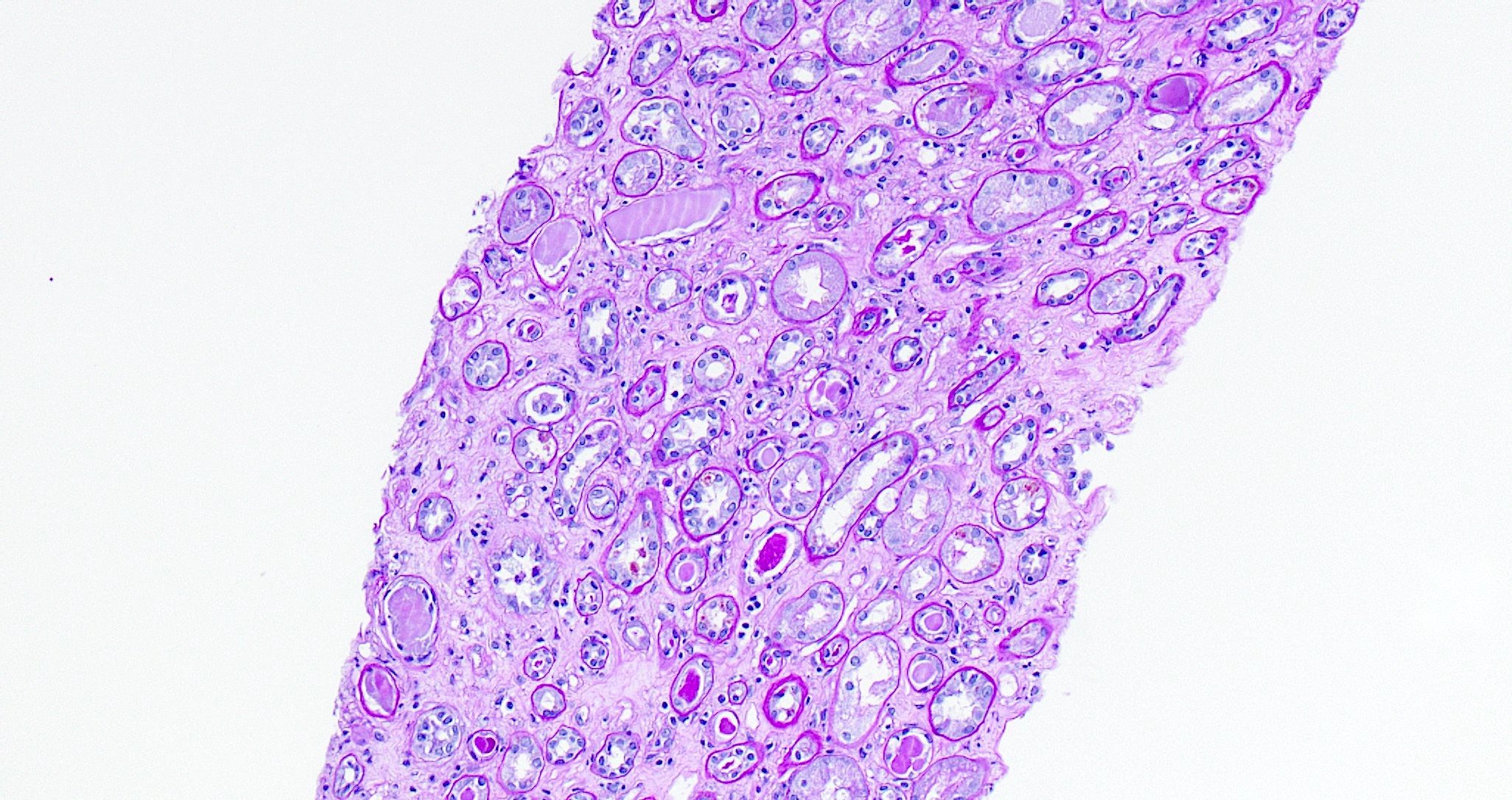
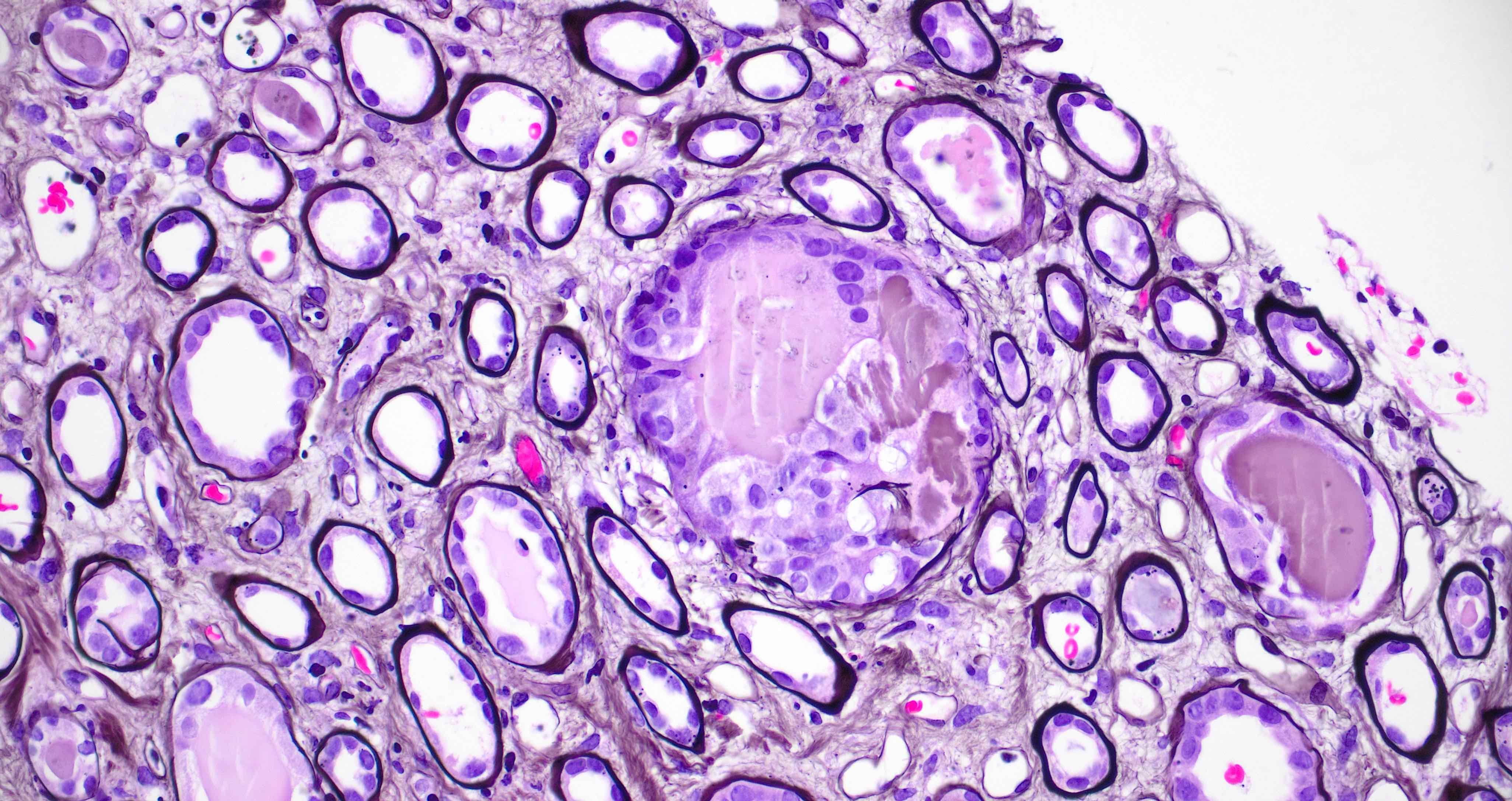
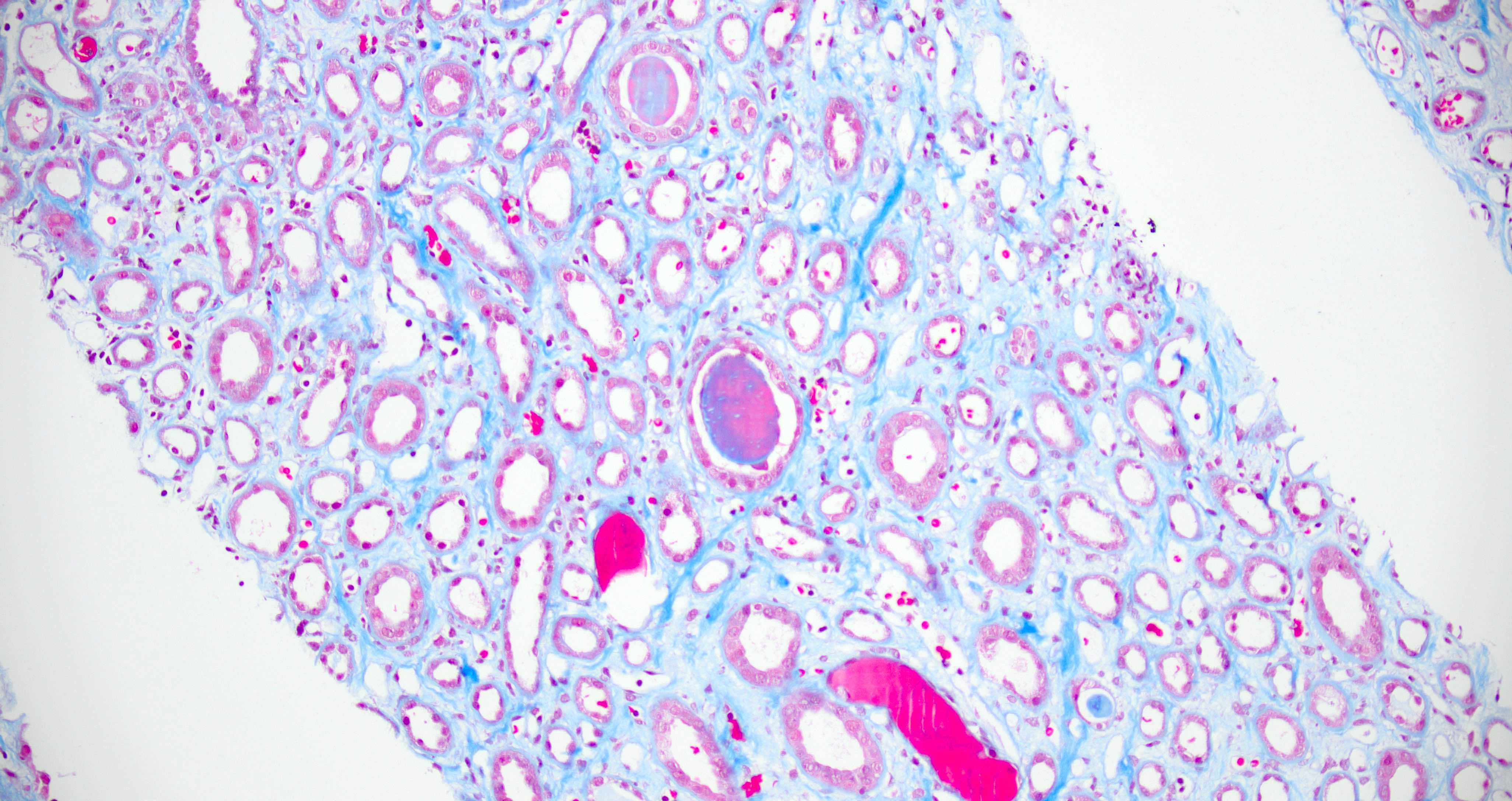
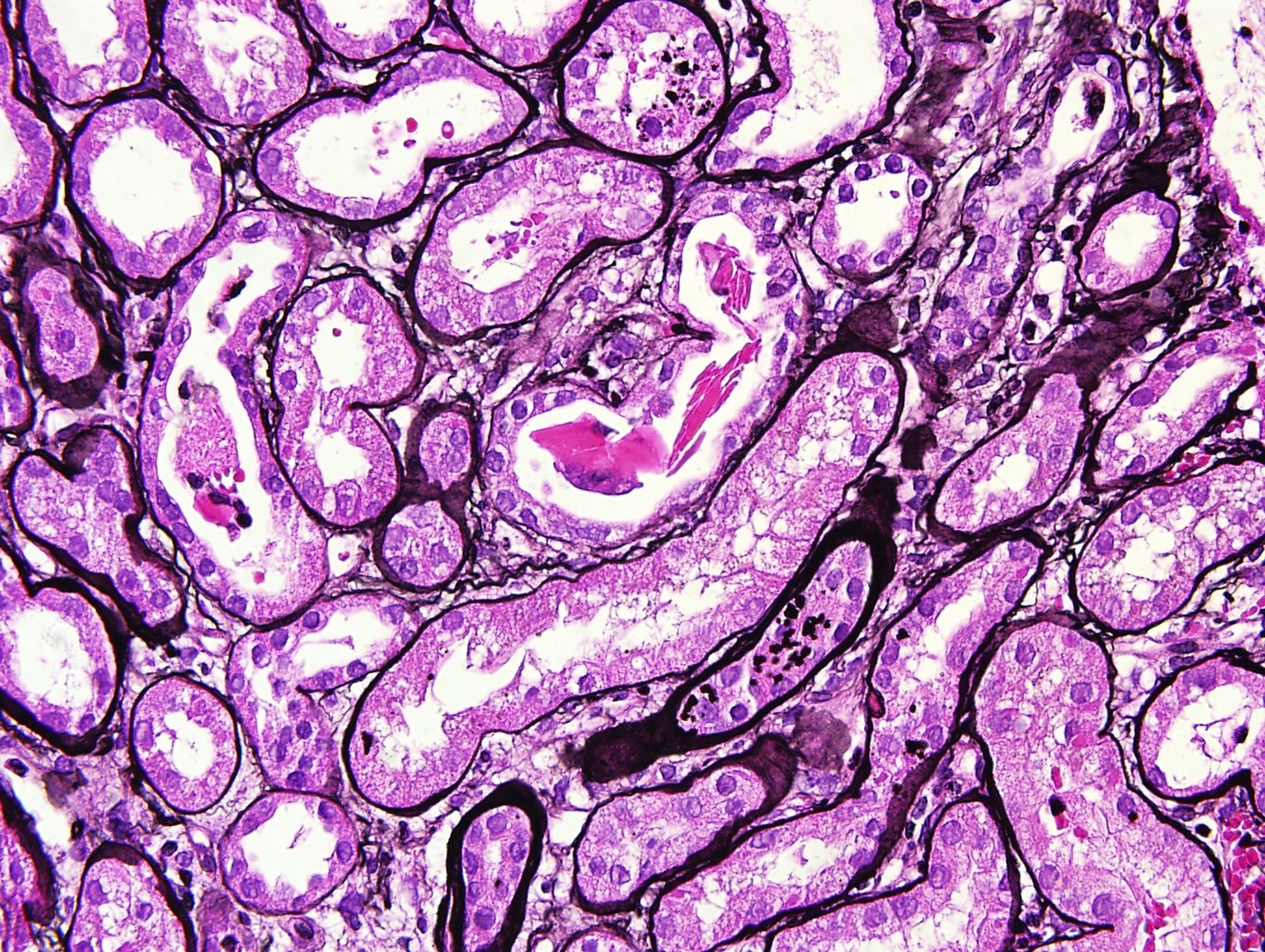
Microscopic (histologic) description
- Glomeruli
- Nonspecific changes that can be related to preexisting conditions or other monoclonal protein related findings
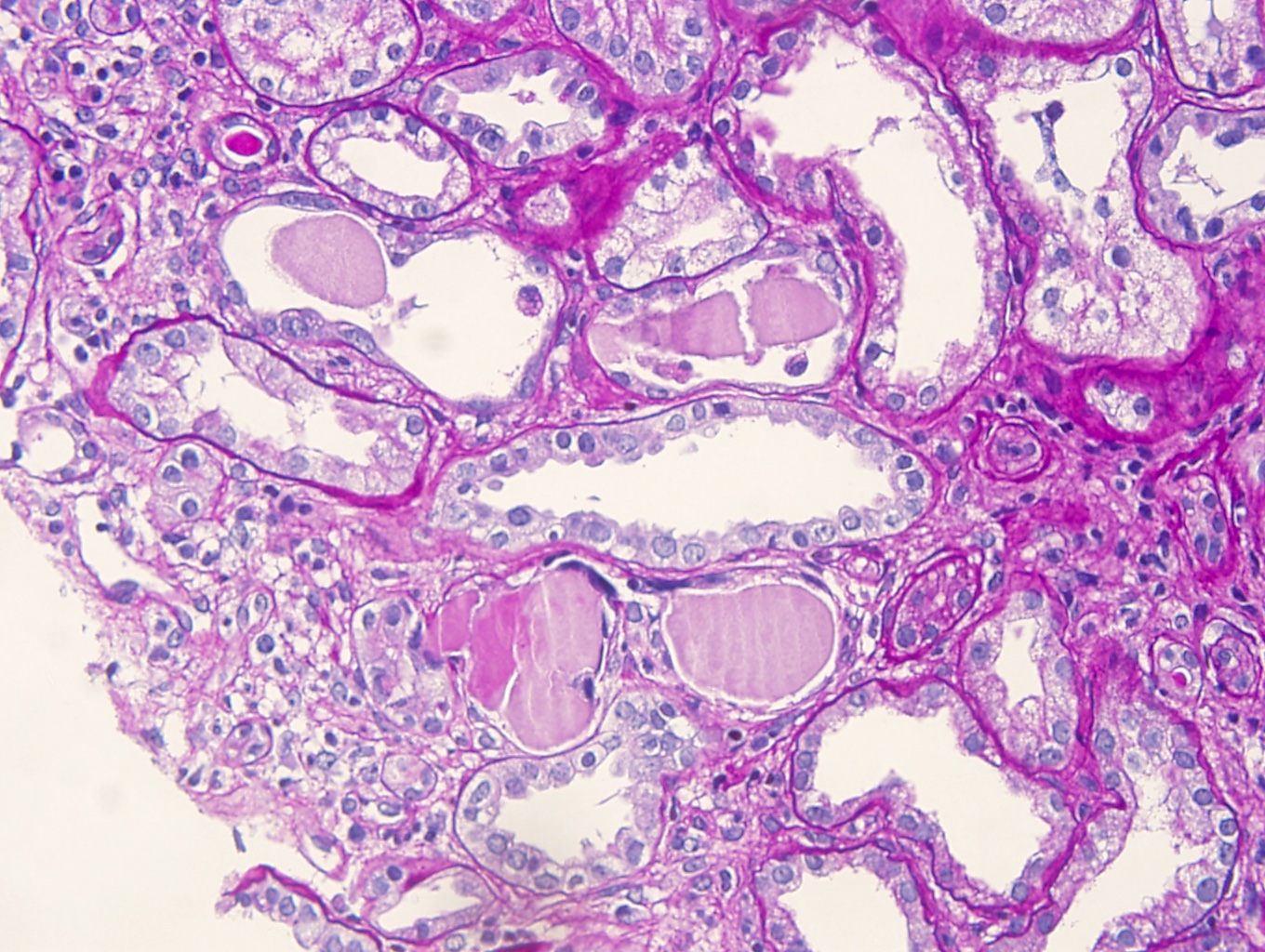
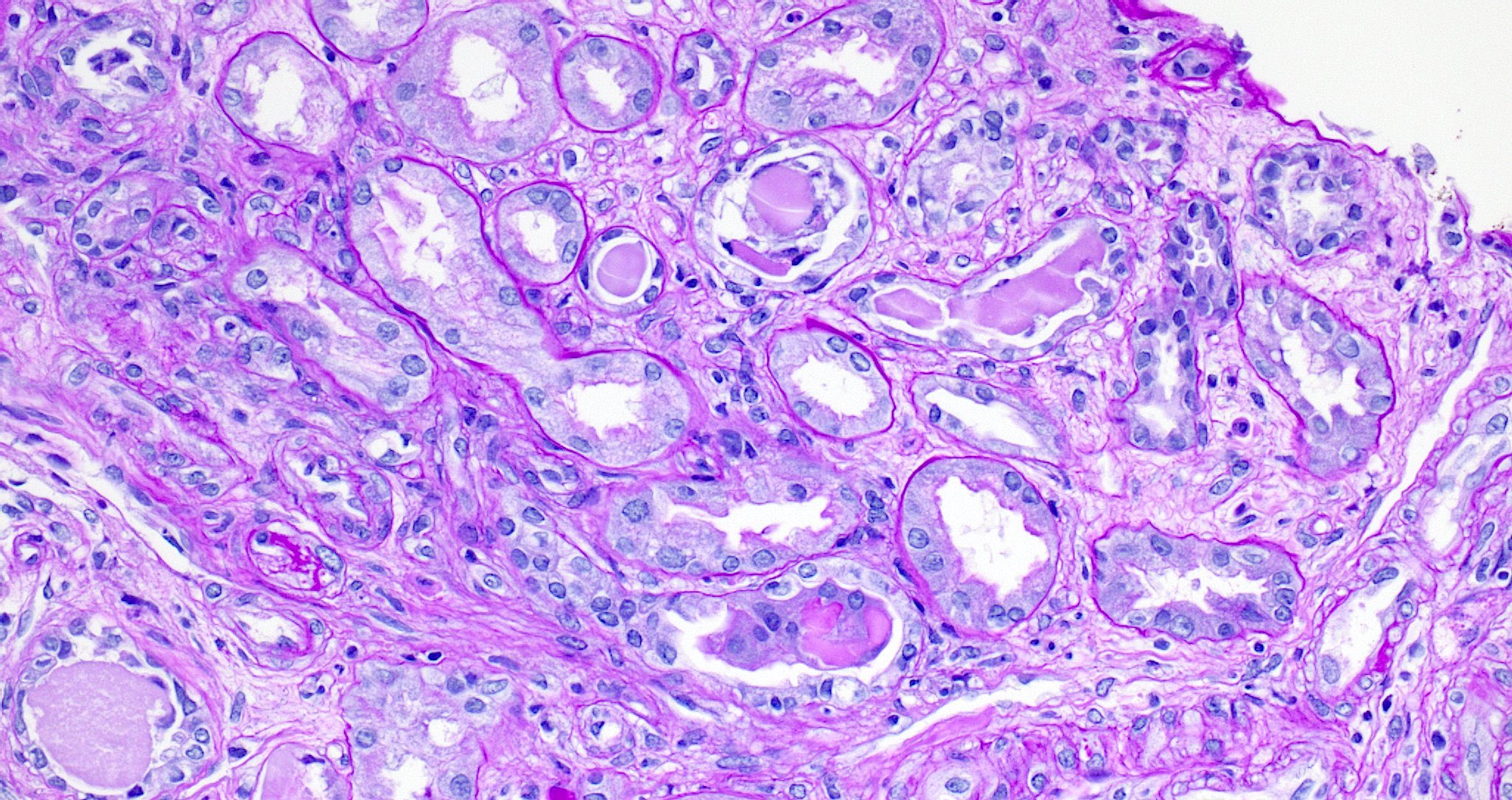
- Tubules
- Distal convoluted tubules and collecting ducts show presence of casts
- Casts show a characteristic appearance with irregular, angulated and geometric shapes and fracture planes and sometimes with a peculiar jigsaw puzzle type of arrangement
- Occasionally, they have lamellated appearance or crystalline appearance
- Casts appear strongly eosinophilic on H&E, pale or weak positive on PAS and red-violet (metachromatic) on trichrome stained sections
- Casts can appear metachromatic because of the varying composition of light chains (pale on PAS stain) and Tamm-Horsfall proteins (eosinophilic on PAS stain)
- Casts may be lined with flattened to reactive tubular epithelium
- Casts can be associated with polymorphonuclear cell or syncytial giant cell or granulomatous reaction
- Some of the casts are congophilic and elicit apple green birefringence on Congo red stain (amyloidogenic activity)
- This finding may be a risk factor for systemic amyloidosis (Mod Pathol 2018;31:452)
- Some casts contain crystals
- Proximal convoluted tubules may show acute tubular injury
- Interstitium
- Varying degrees of inflammation with mononuclear cells, plasma cells, polymorphonuclear cells and occasional eosinophils that is sometimes similar to chronic interstitial nephritis often can be seen
- When casts break through tubular basement membranes, multinucleated giant cell reaction or peritubular granulomas are seen
- Rarely neoplastic plasma cells may infiltrate kidney
- Varying degree of interstitial fibrosis and tubular atrophy can be seen
- Vasculature
- Nonspecific changes that can be related to preexisting conditions or other monoclonal protein related findings
Microscopic (histologic) images
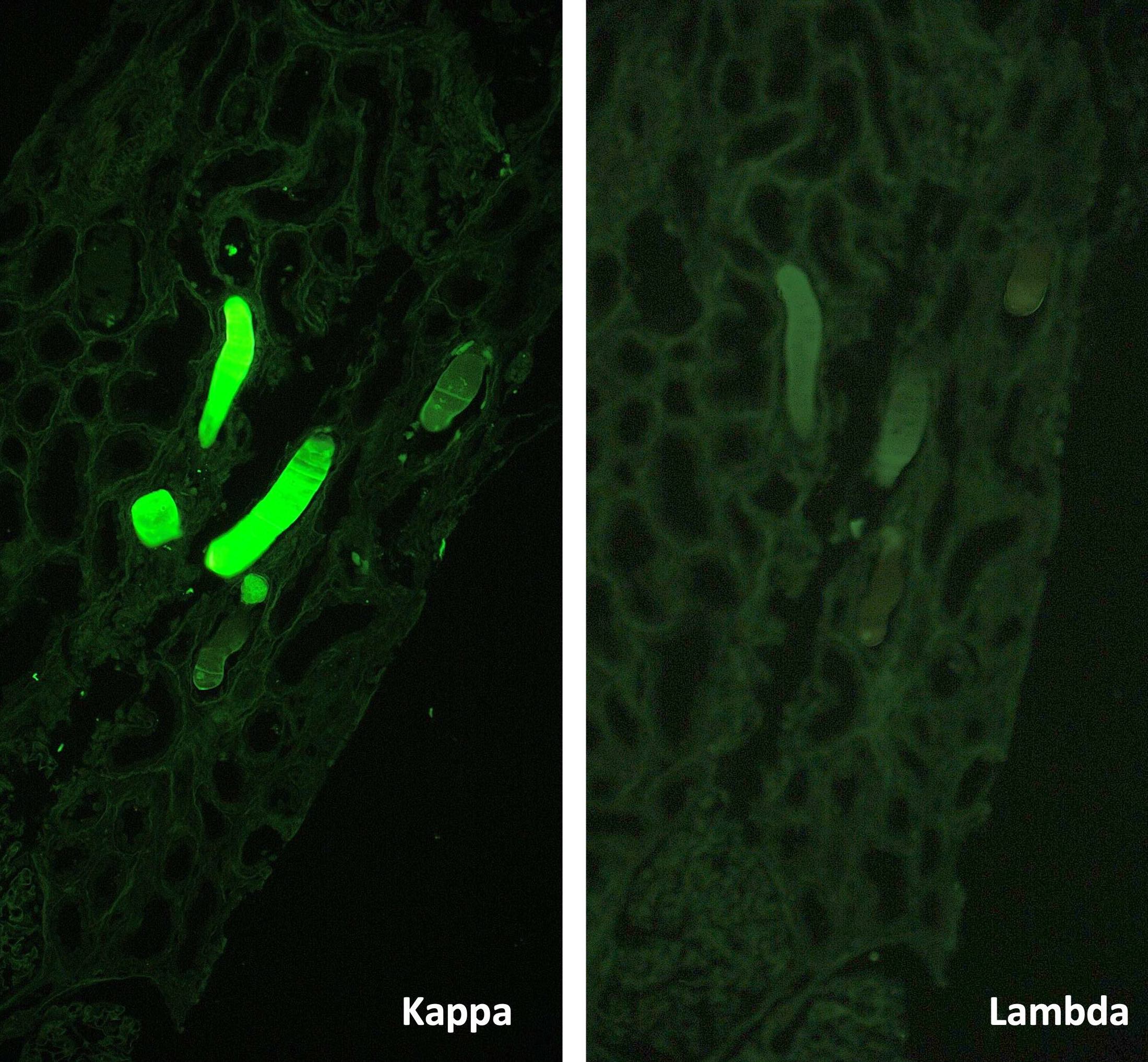
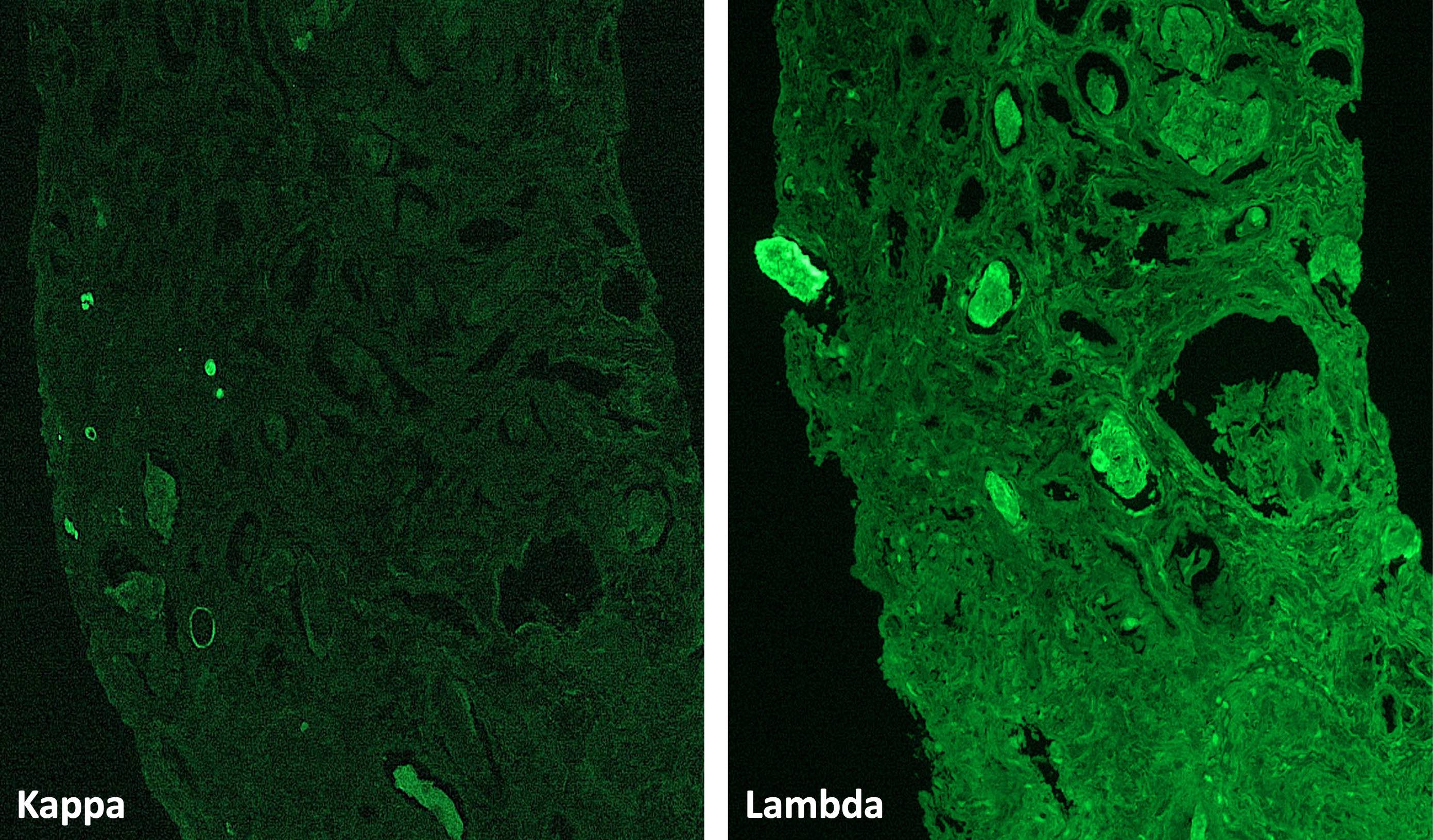
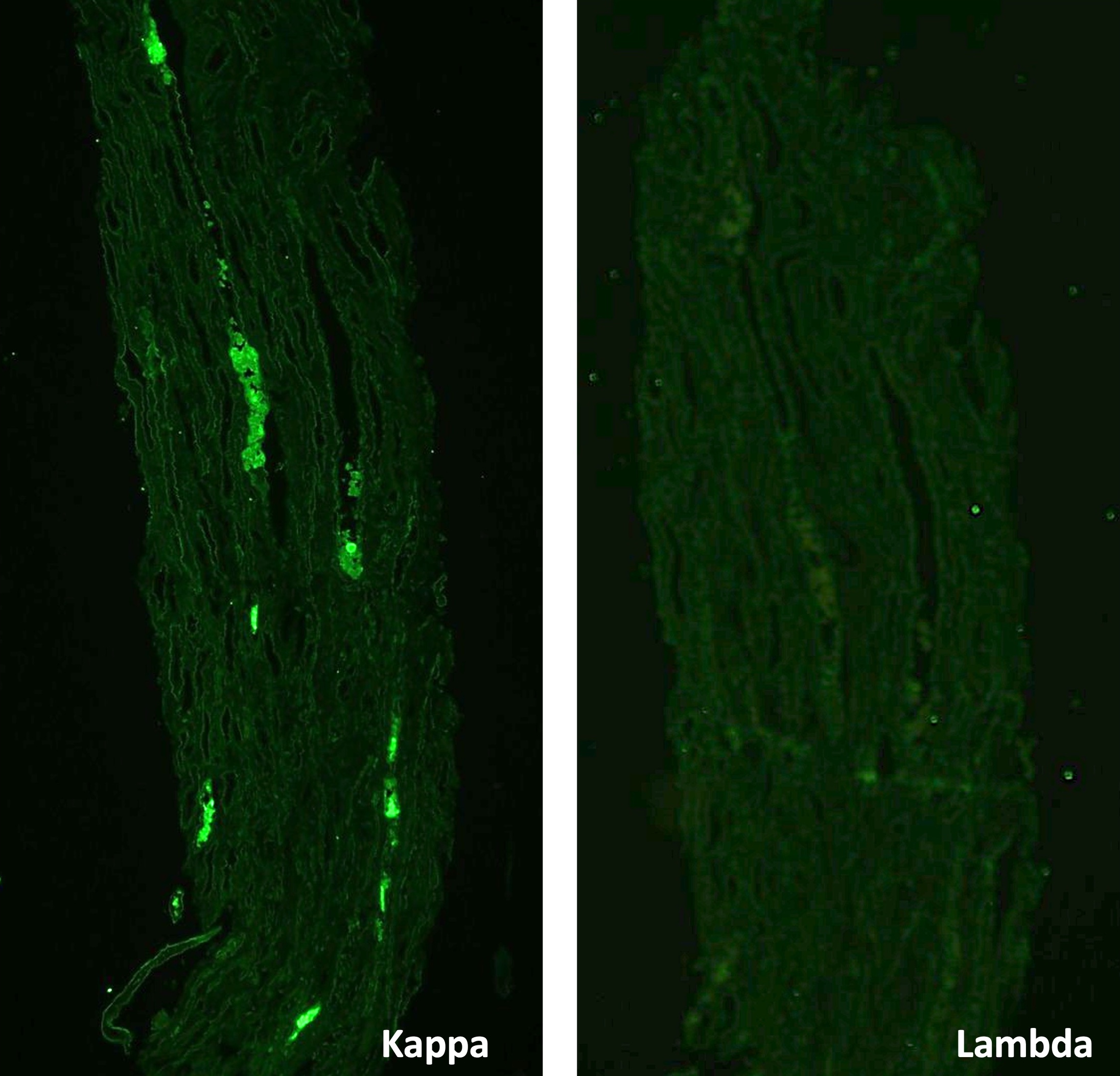
Immunofluorescence description
- Light chain restricted staining of the casts for either kappa or lambda helps to confirm the diagnosis
- Only seen when casts are acutely formed but not when they are present for a prolonged period
- Only about half of the casts in proven light chain cast nephropathy stain in a monoclonal pattern; therefore, absence of monoclonal staining cannot be taken as definitive evidence to rule out light chain cast nephropathy (Fogo: Diagnostic Renal Pathology, 4th Edition, 2022)
- Clonal staining may be absent when casts are present in few numbers focally only or secondary to mutated light chains not recognized by commercial antibodies
- Kappa and lambda staining on paraffin embedded sections after pronase digestion may help
- Glomeruli and vasculature reveal no specific findings
Immunofluorescence images
Positive stains
- Kappa or lambda IHC stains can be done to demonstrate monoclonal staining in biopsies without any casts in the tissue submitted for immunofluorescence studies
- Casts can be Congo red positive (amyloidogenic activity) in 28% of cases
Negative stains
- Monoclonal staining of the casts can be absent when casts are few and focal and when the mutated proteins are not recognized by commercially available antibodies
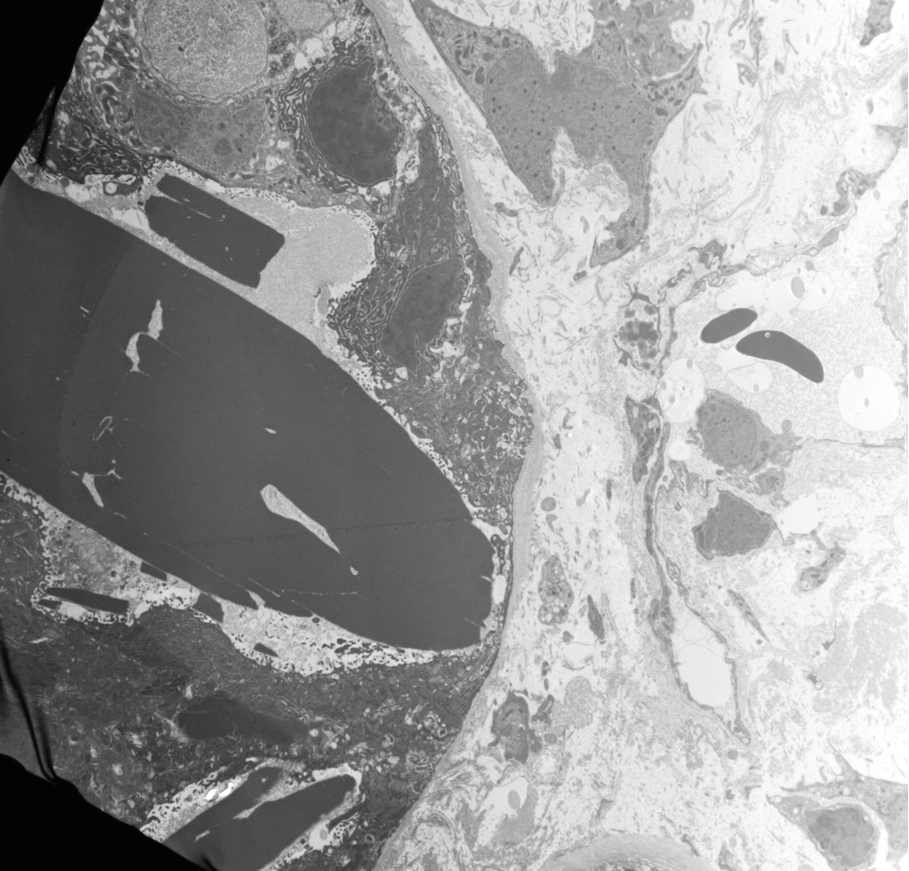
Electron microscopy description
- Glomeruli and vasculature show no specific findings
- Tubular casts composed of finely granular material of moderate electron density are seen
- Spectrum of appearances including fibrillar, microvesicular or crystalline substructure can be seen
- Ultrastructural immunogold labeling to demonstrate monoclonality can be performed in cases where immunofluorescence is not diagnostic
Electron microscopy images
Videos
Washington University in St. Louis: renal pathology teaching series
Sample pathology report
- Kidney, percutaneous needle biopsy:
- Light chain cast nephropathy (see comment)
- Comment: There are scattered granular to globular PAS pale and metachromatic casts with fractured appearance with rare syncytial giant cell reaction and associated acute tubular injury. These casts demonstrate monoclonal lambda staining by immunofluorescence without corresponding staining for kappa. In this patient with a history of lambda light chain myeloma, these findings are diagnostic of light chain cast nephropathy.
Differential diagnosis
- Myoglobin cast nephropathy:
- Pigmented globular casts that stain positive for myoglobin
- Absence of light chain restriction by immunofluorescence (IF)
- Vancomycin cast nephropathy:
- Casts stain for vancomycin
- Absence of light chain restriction by IF
- Electron microscopy shows vancomycin nanospheres entangled with uromodulin
- Monoclonal immunoglobulin deposition disease:
- Deposition of monoclonal light or heavy chains along glomerular basement membrane (GBM) and tubular basement membranes (TBM)
- Monoclonal linear / ribbon staining along GBMs and TBMs by IF
- Electron microscopy shows powdery deposits along GBMs and TBMs
- Can occur concurrently with light chain cast nephropathy in 10% of cases
- Light chain proximal tubulopathy:
- Intracytoplasmic crystalline or noncrystalline deposits that are PAS and trichrome positive within proximal tubular epithelial cells
- Granular cytoplasmic positivity for either kappa or lambda on IF
- Electron microscopy shows intracytoplasmic electron dense crystals with sharp edges
- Other drug related cast nephropathies:
- Chemotherapy drugs such as ripamycin, etc.
- End stage kidney with hyaline casts:
- PAS positive casts by light microscopy
- Absence of syncytial giant cell reaction
- No monoclonal staining by IF
Additional references
Board review style question #1
A 65 year old man with history of chronic kidney disease now presents with oliguria, fatigue and nausea for the past 2 weeks. Laboratory studies show anemia with a hemoglobin of 8.6 g/dL, serum creatinine of 5.2 mg/dL compared to 1.7 mg/dL a few months ago. Urine studies show 2+ proteinuria without hematuria. Spot urine protein creatinine ratio is 4.8. Serum and urine free light chains show elevated lambda levels. Renal biopsy was performed and is shown in the images above. A Congo red stain is negative. Electron microscopy does not show any fibrillar deposits, no powdery deposits along tubular basement membranes and glomerular basement membranes and no crystals within the tubules. What is the diagnosis?
- AL amyloidosis
- Light chain cast nephropathy
- Light chain deposition disease
- Light chain proximal tubulopathy
Board review style answer #1
B. Light chain cast nephropathy. Monoclonal staining of casts by immunofluorescence that show fractured appearance and syncytial giant cell reaction on light microscopy, metachromatic appearance on trichrome staining are diagnostic of light chain cast nephropathy.
Answer A is incorrect because a Congo red stain is negative and there are no fibrillar type deposits by electron microscopy. Answer C is incorrect because there is no monoclonal tubular basement membrane staining by immunofluorescence and electron microscopy does not show powdery deposits. Answer D is incorrect because there is no monoclonal droplet staining within the tubules by immunofluorescence and no intratubular crystals by electron microscopy.
Comment Here
Reference: Light chain cast nephropathy
Comment Here
Reference: Light chain cast nephropathy
Board review style question #2
A 77 year old woman with new diagnosis of multiple myeloma presents with anuria and acute kidney injury. Laboratory studies show serum creatinine of 3.9 mg/dL compared to 1.3 mg/dL a few months ago. Renal biopsy was performed and shows intratubular casts with fractured appearance and associated giant cell reaction and metachromatic appearance on trichrome staining. Immunofluorescence staining shows monoclonal staining of casts for kappa only without staining for lambda. A Congo red stain is negative and electron microscopy is noncontributory. What is the diagnosis?
- AL amyloidosis
- Light chain cast nephropathy
- Light chain deposition disease
- Light chain proximal tubulopathy
Board review style answer #2
B. Light chain cast nephropathy. Monoclonal staining of casts for kappa by immunofluorescence that show fractured appearance and syncytial giant cell reaction on light microscopy and metachromatic appearance on trichrome staining are diagnostic of light chain cast nephropathy.
Answer A is incorrect because a Congo red stain is negative and there are no fibrillar type deposits by electron microscopy. Answer D is incorrect because there is no monoclonal droplet staining within the tubules by immunofluorescence and no intratubular crystals by electron microscopy. Answer C is incorrect because there is no monoclonal tubular basement membrane staining by immunofluorescence and electron microscopy does not show powdery deposits.
Comment Here
Reference: Light chain cast nephropathy
Comment Here
Reference: Light chain cast nephropathy