Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Genetics | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Soares MF. IgA nephropathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneyiga.html. Accessed April 2nd, 2025.
Definition / general
- Immunoglobulin A (IgA) nephropathy: dominant or codominant mesangial IgA deposits in the absence of systemic diseases
- Variable light microscopic and clinical features
Essential features
- Most common primary glomerulonephritis worldwide
- Macro / microscopic hematuria with or without proteinuria
- 80% renal survival in 10 years; 25 - 50% progression to end stage renal disease over 20 years; 30% recurrence in transplants
- Etiology: abnormally glycosylated IgA1
- Dominant or codominant IgA deposits in mesangium; variable light microscopic features; electron microscopy most often with mesangial electron dense deposits
- Histopathological grading: Oxford classification - mesangial hypercellularity (M), endocapillary hypercellularity (E), segmental glomerulosclerosis (S), tubular atrophy / interstitial fibrosis (T) and crescents (C) are independent prognostic factors
Terminology
- Immunoglobulin A nephropathy
- Berger disease
ICD coding
- ICD-10: N02.8 - Recurrent and persistent hematuria with morphologic changes
- SNOMED CT: 68779003 - Primary immunoglobulin A nephropathy
- SNOMED II: D67300 - Mesangial IgA / IgG disease
- SNOMED II is no longer supported but is still in use in some histopathology databases (SNOMED International 2019: A Brief History of SNOMED Code Systems [Accessed 17 April 2020])
Epidemiology
- Most common primary glomerulonephritis worldwide (UptoDate: Clinical Presentation and Diagnosis of IgA Nephropathy [Accessed 6 April 2020])
- More common in Southern Europe, Asia and Native Americans; less common in individuals of African lineage
- First to seventh decade of life; peak 20 - 30 years
- M:F = 2:1 in Europe / U.S. and 1:1 in Asia
Sites
- Renal cortex
Pathophysiology
- Increased serum levels of poorly galactosylated IgA1 (galactose deficient IgA1; GD-IgA1)
- Overproduction of GD-IgA1 in response to immune challenges in mucosal sites (upper respiratory and GI tract infections)
- GD-IgA1 binds to CD71 on mesangial cells; it also triggers autoimmune response with autoantibody production against GD-IgA1 GalNAc epitopes (Colvin: Diagnostic Pathology - Kidney Diseases, 3rd Edition, 2019)
- Disease progression (Colvin: Diagnostic Pathology - Kidney Diseases, 3rd Edition, 2019):
- Mesangial cell proliferation
- IgA / anti-IgA complex deposition in mesangium
- Cytokine release by mesangial cells leading to podocyte injury
- 25 - 50% of patients will progress to renal failure at 20 years; recurs in 20 - 60% of allografts (average 30%)
Etiology
- Heightened IgA response to mucosal antigens
- Secretion of poorly galactosylated IgA1
- Autoantibodies to poorly galactosylated IgA1
Clinical features
- 40 - 50%: at least one episode of visible hematuria associated to upper respiratory tract infection (synpharyngitic hematuria) (UptoDate: Clinical Presentation and Diagnosis of IgA Nephropathy [Accessed 6 April 2020])
- 30 - 50%: microscopic hematuria
- < 10%: nephrotic syndrome or rapidly progressive glomerulonephritis
- Rare: acute kidney injury (due to either rapidly progressive glomerulonephritis or red cell cast nephropathy)
- Secondary IgA nephropathy: associated with chronic liver disease, celiac disease and HIV
Diagnosis
- Renal biopsy with immunofluorescence / immunohistochemistry is the cornerstone of the diagnosis (UptoDate: Clinical Presentation and Diagnosis of IgA Nephropathy [Accessed 6 April 2020])
Laboratory
- Serum polymeric IgA1: elevated in 30 - 50% of cases (UptoDate: Clinical Presentation and Diagnosis of IgA Nephropathy [Accessed 6 April 2020])
- Urine dip: hematuria with or without proteinuria
Prognostic factors
- Oxford classification MEST-C scores: mesangial hypercellularity (M), endocapillary hypercellularity (E), segmental glomerulosclerosis (S), tubular atrophy / interstitial fibrosis (T) and crescents (C) are independent prognostic factors (Curr Opin Nephrol Hypertens 2017;26:165):
- MEST-C scores and eGFR can predict outcome as accurately as 2 year follow up eGFR and proteinuria (JAMA Intern Med 2019;179:942)
- Limitations: original cohort excluded patients with proteinuria < 0.5 g/day, those with eGFR < 30 ml/min and follow up < 1 year; angiotensin blockade and immunosuppressive regimens were uncontrolled, resulting in treatment bias to outcome data
- Online risk calculator (Calculate by QxMD: International IgAN Prediction Tool [Accessed 6 April 2020])
- In patients with proteinuria < 0.5 g/24 h: M1 and E1 predict proteinuria > 1 g/24 h over 5 year follow up; M1 independently predicts rapid loss of renal function
- E1: independently predicts rapid loss of renal function in patients not treated with steroids (J Nephrol 2016;29:367, Kidney Int 2017;91:235)
- S1 with podocyte hypertrophy and tip lesions (S1p): associated to higher proteinuria/24 h and worse renal survival in patients not treated with steroids (Kidney Int 2017;91:235)
- Endocapillary hypercellularity, crescents and necrosis seem to be responsive to immunosuppression (J Nephrol 2015;28:441)
- Extent of interstitial fibrosis / tubular atrophy: reflects chronic damage; associated with long term outcome
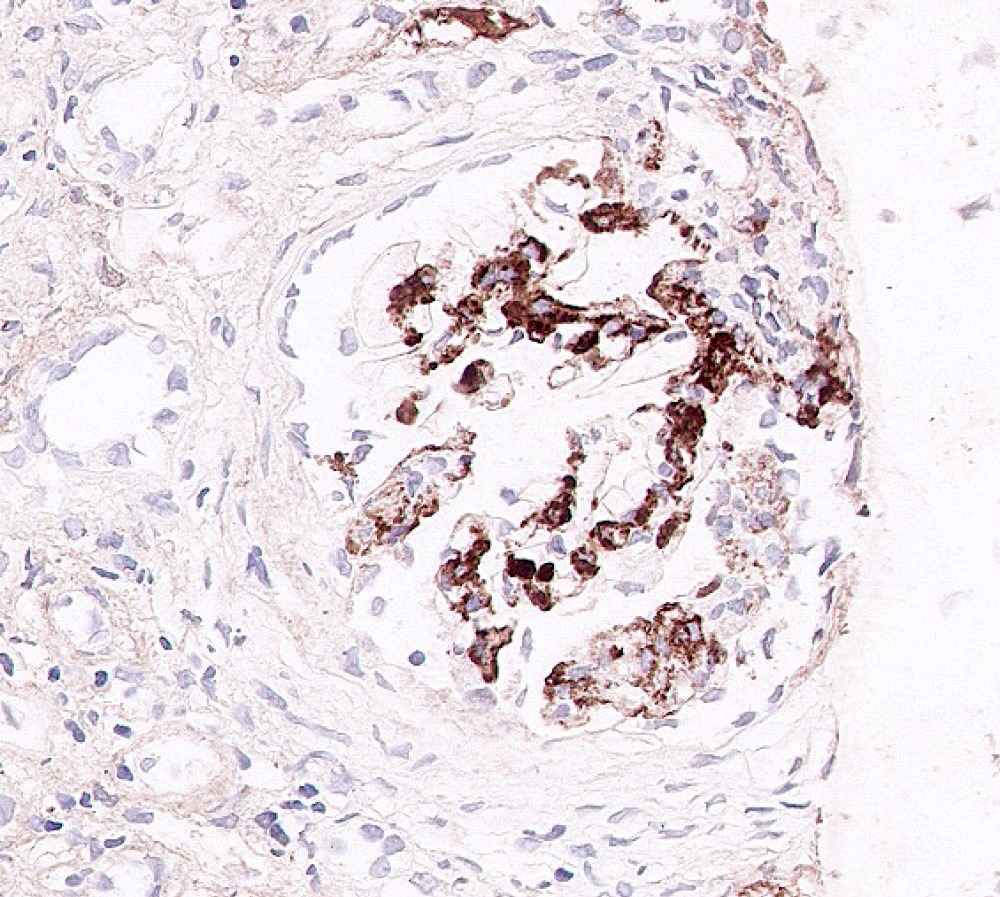
- Immunohistochemistry:
- Evidence of lectin pathway activation (deposition of mannose binding lectin, L ficolin, MASP1/3 and C4d): seen in 25 - 30% of cases and is associated with more severe histologic damage and proteinuria (Kidney Int Rep 2017;3:426)
- Mesangial C4d: predicts worse long term renal outcome (J Nephrol 2016;29:1)
- Glomerular deposition of complement factor H related protein 5 (CFHR5): associated to disease progression (Kidney Int Rep 2017;3:426)
- Clinical predictors (UptoDate: Treatment and Prognosis of IgA Nephropathy [Accessed 6 April 2020]):
- High serum creatinine / reduced eGFR
- Hypertension (> 140/90 mmHg)
- Proteinuria > 1 g/24 h for over 6 months
Case reports
- 24 year old man with atypical celiac disease presenting with nephrotic syndrome (Cent Eur J Immunol 2019;44:106)
- 36 year old man with recurrent crescentic disease in renal allograft (Clin Case Rep 2019;7:1773)
- 50 year old woman with concomitant primary membranous glomerulonephritis (Saudi J Kidney Dis Transpl 2019;30:531)
- 74 year old woman with systemic lupus erythematosus and acute kidney injury due to crescentic disease (Case Rep Nephrol 2019;2019:8354823)
- 81 year old man with differential diagnosis of IgA dominant infection associated glomerulonephritis (Am J Case Rep 2019;20:508)
Treatment
- Aims at slowing progression of renal damage (nonimmunosuppresive measures: control of blood pressure and proteinuria) and dampening inflammatory activity (immunosuppression: steroids) (UptoDate: Treatment and Prognosis of IgA Nephropathy [Accessed 6 April 2020])
- If hematuria, normal eGFR with or without proteinuria < 0.5 g/day: watchful monitoring at 6 to 12 month intervals
- If proteinuria > 500 mg/day over 6 months and or mildly reduced eGFR and mild to moderate histologic findings on renal biopsy: nonimmunosuppressive therapies (ACE-I / ARB)
- If rising creatinine, active lesions on renal biopsy (E1, C1/2) or nephrotic range proteinuria or proteinuria after 3 - 6 months of nonimmunosuppressive: consider association of immunosuppressive therapy in addition
- There is some evidence that patients with E1, podocytopathic S1 lesions and C1 and C2 have a markedly lower rate of decline in eGFR when immunosuppressed (J Am Soc Nephrol 2017;28:691)
- Fish oil: low quality evidence; tonsillectomy: evidence from randomized controlled trials missing
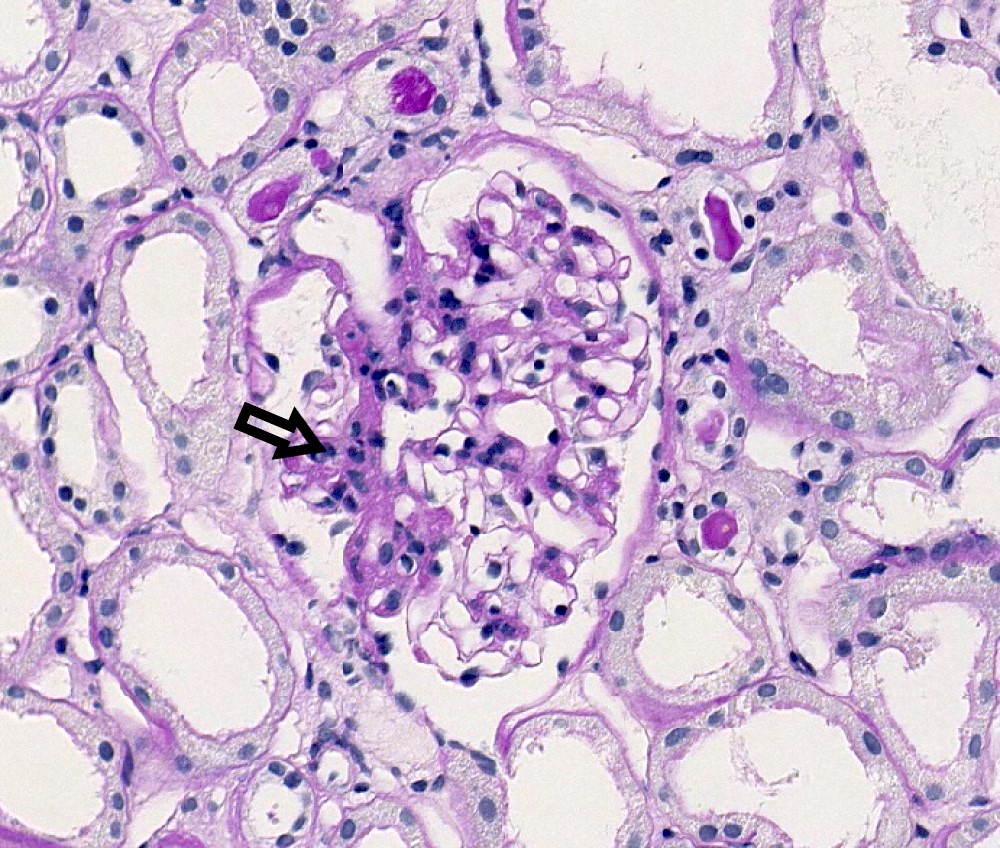
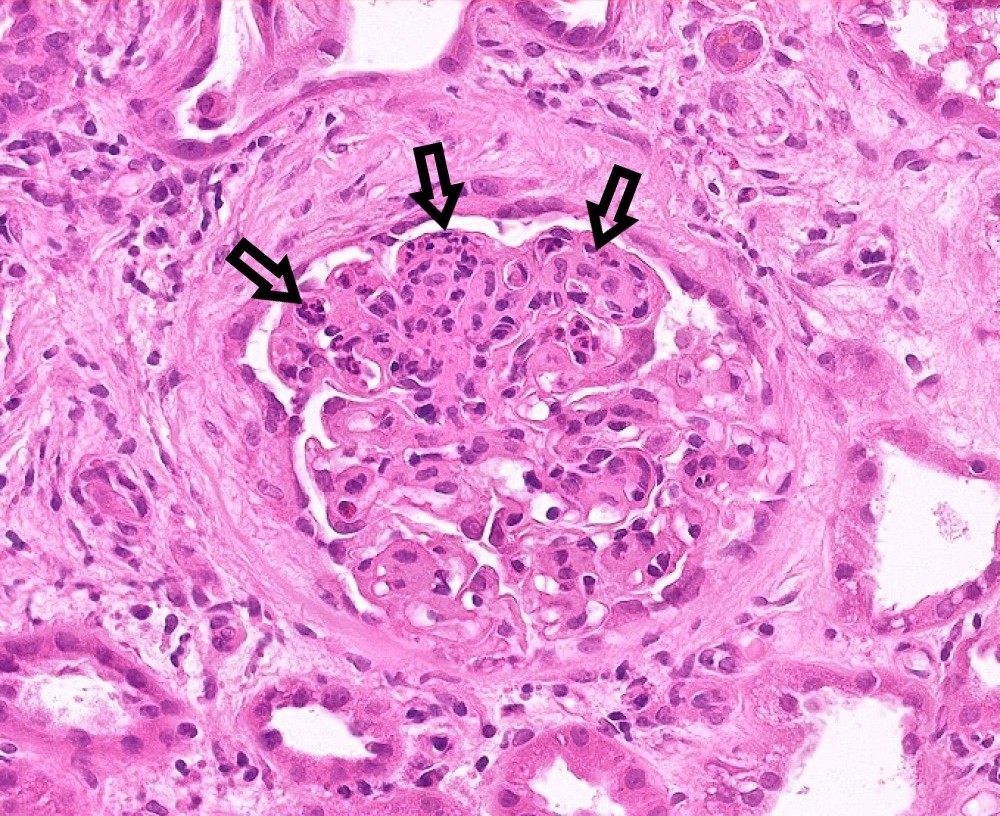
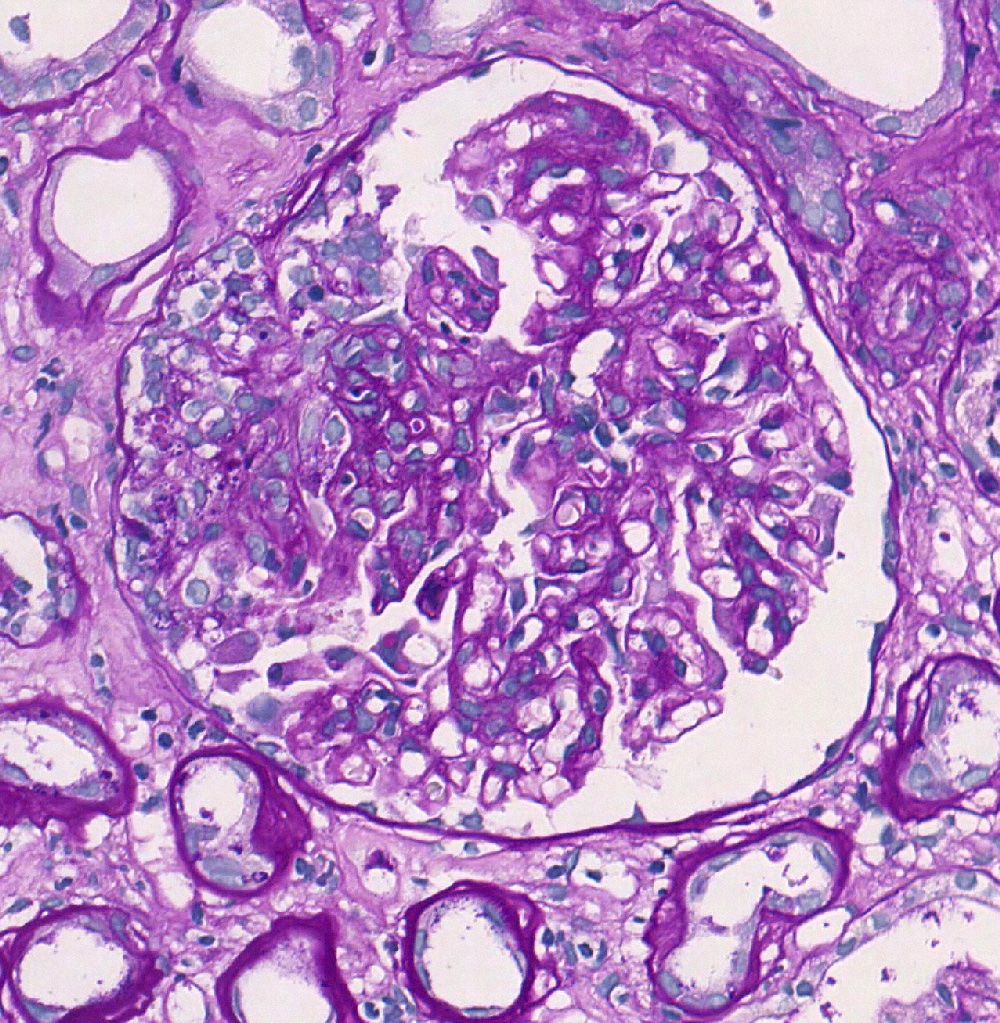
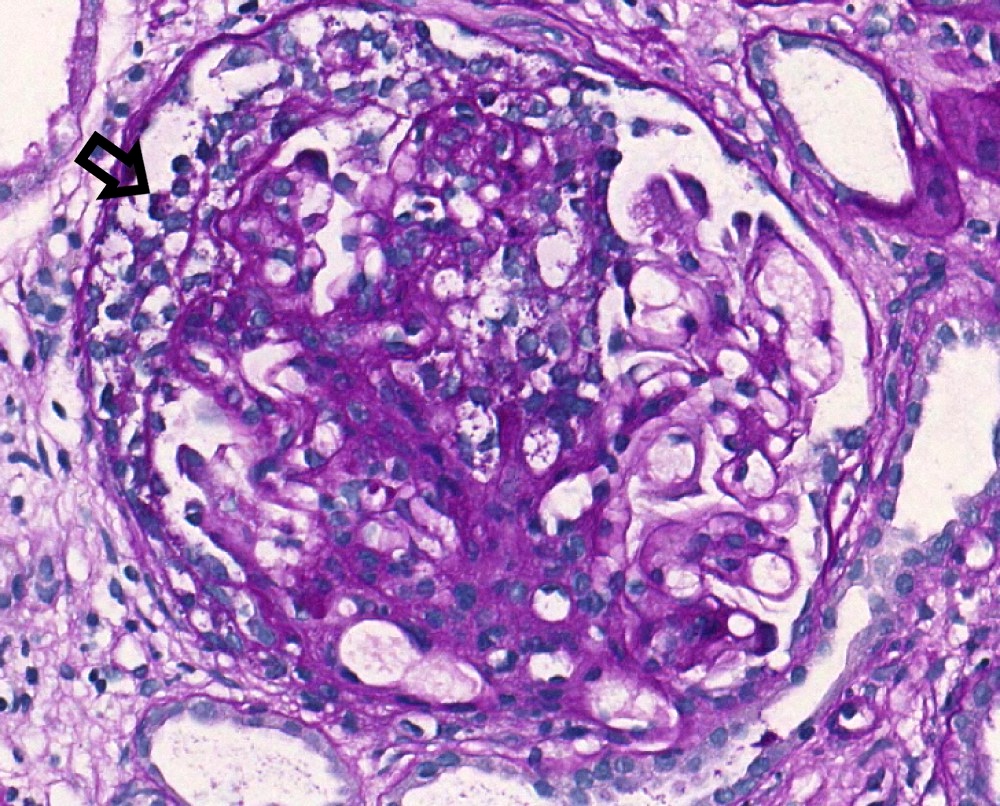
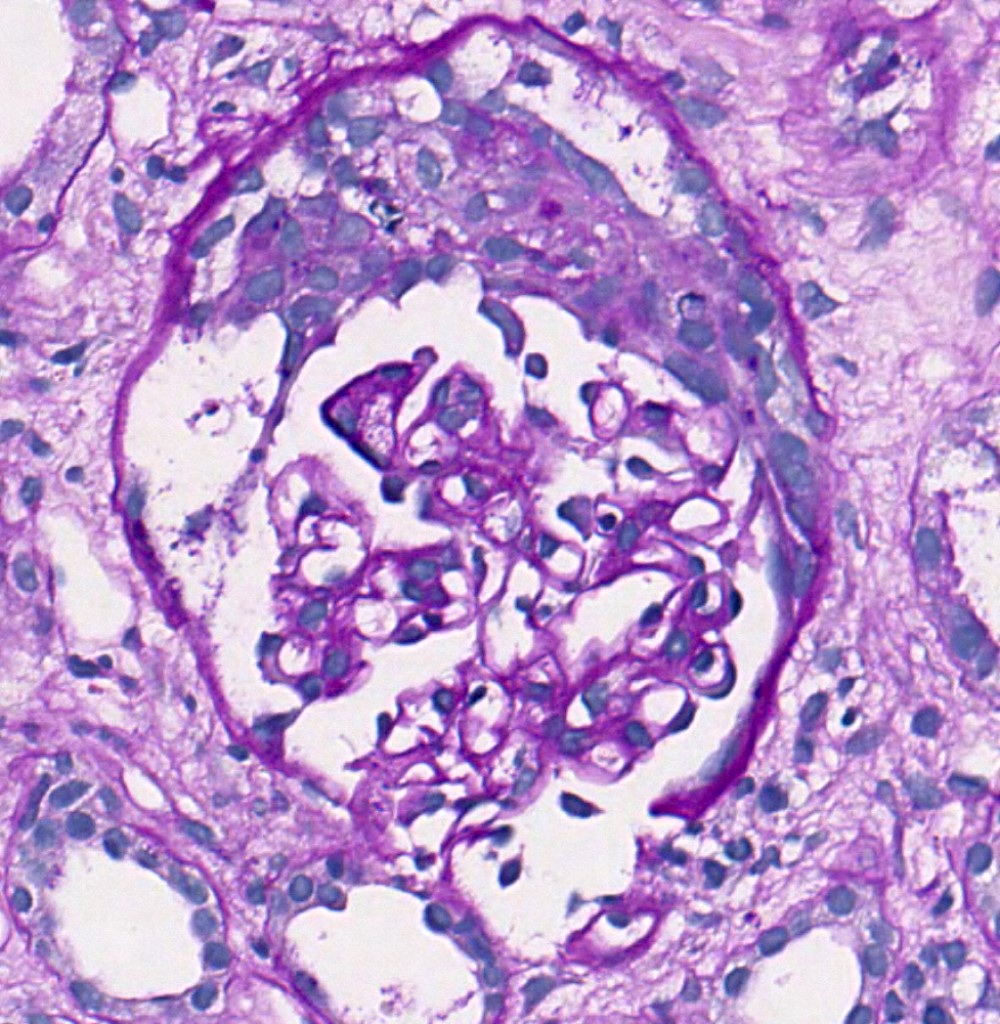
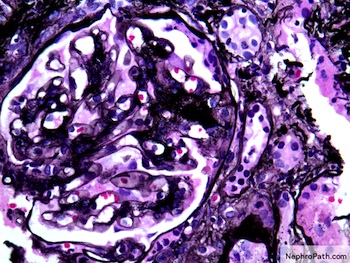
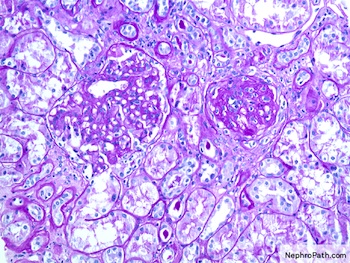
Microscopic (histologic) description
- Oxford classification: first evidence based glomerular disease classification (Semin Nephrol 2018;38:477)
- Variable light microscopic patterns; in the original classification 4 lesions were reproducible and predictive of outcome (Kidney Int 2017;91:1014):
- Mesangial hypercellularity (M0 ≤ 50% of glomeruli; M1 > 50% of glomeruli): > 3 mesangial cell nuclei / peripheral mesangial area, not adjacent to vascular pole, in 2 - 3 μm thick PAS stained section
- Endocapillary hypercellularity (E0 absent; E1 present): CD68 count > 6 in most affected glomerulus of the sample is associated with E1
- Segmental glomerulosclerosis / adhesions / synechiae (S0 absent; S1 present): due to hyperfiltration, healed necrotizing lesions or podocytopathy
- Tubular atrophy / interstitial fibrosis (T0 absent to involving ≤ 25% of the cortex; T1 26 - 50% of the cortex; T2 > 50% of the cortex)
- Crescents: added to the classification in 2016 (C0 absent; C1 1 - 24% of glomeruli with cellular / fibrocellular crescents; C2 ≥ 25% of glomeruli with cellular / fibrocellular crescents)
- Other lesions: fibrinoid necrosis (10% of biopsies), glomerular basement membrane duplication (< 10% of biopsies), thrombotic microangiopathy changes (5 - 50% of biopsies; usually associated with malignant hypertension) (Colvin: Diagnostic Pathology - Kidney Diseases, 3rd Edition, 2019)
Microscopic (histologic) images
Contributed by Maria Fernanda Soares, M.D., Ph.D.
Contributed by Arkana
Virtual slides
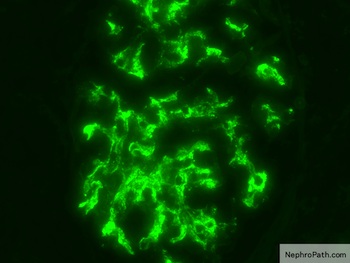
Immunofluorescence description
- Dominant IgA mesangial deposits (100%) - only defining and consistent feature of the disease
- Predominance of J chain containing IgA1 and lambda light chains
- Other mesangial deposits: C3 (90%), IgG (20 - 30%), IgM (50%), C1q (< 10% - almost always absent, indicating lack of activation of classical pathway) (Colvin: Diagnostic Pathology - Kidney Diseases, 3rd Edition, 2019)
- Occasional capillary loop subendothelial deposits
Immunofluorescence images
Positive stains
- CD68: maximum count of glomerular CD68 positive shows relationship with E score (Histopathology 2019;74:629)
- C4d and mannan binding lectin (MBL): mesangial staining associated with worse prognosis (J Nephrol 2016;29:1)
Negative stains
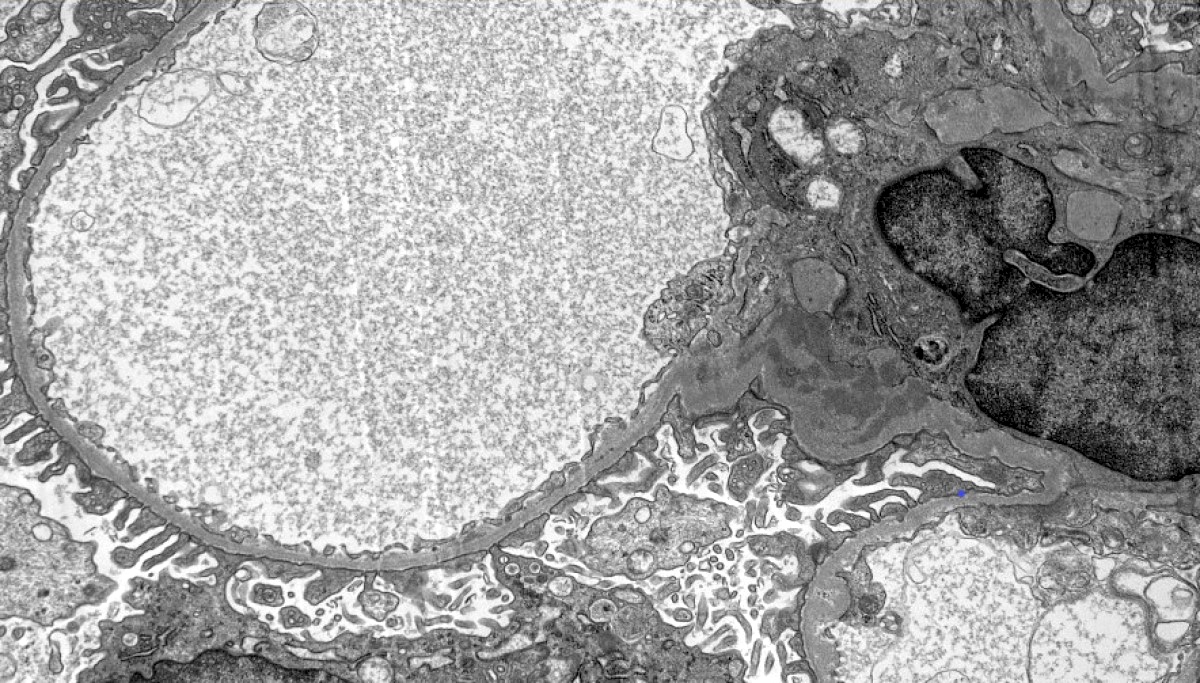
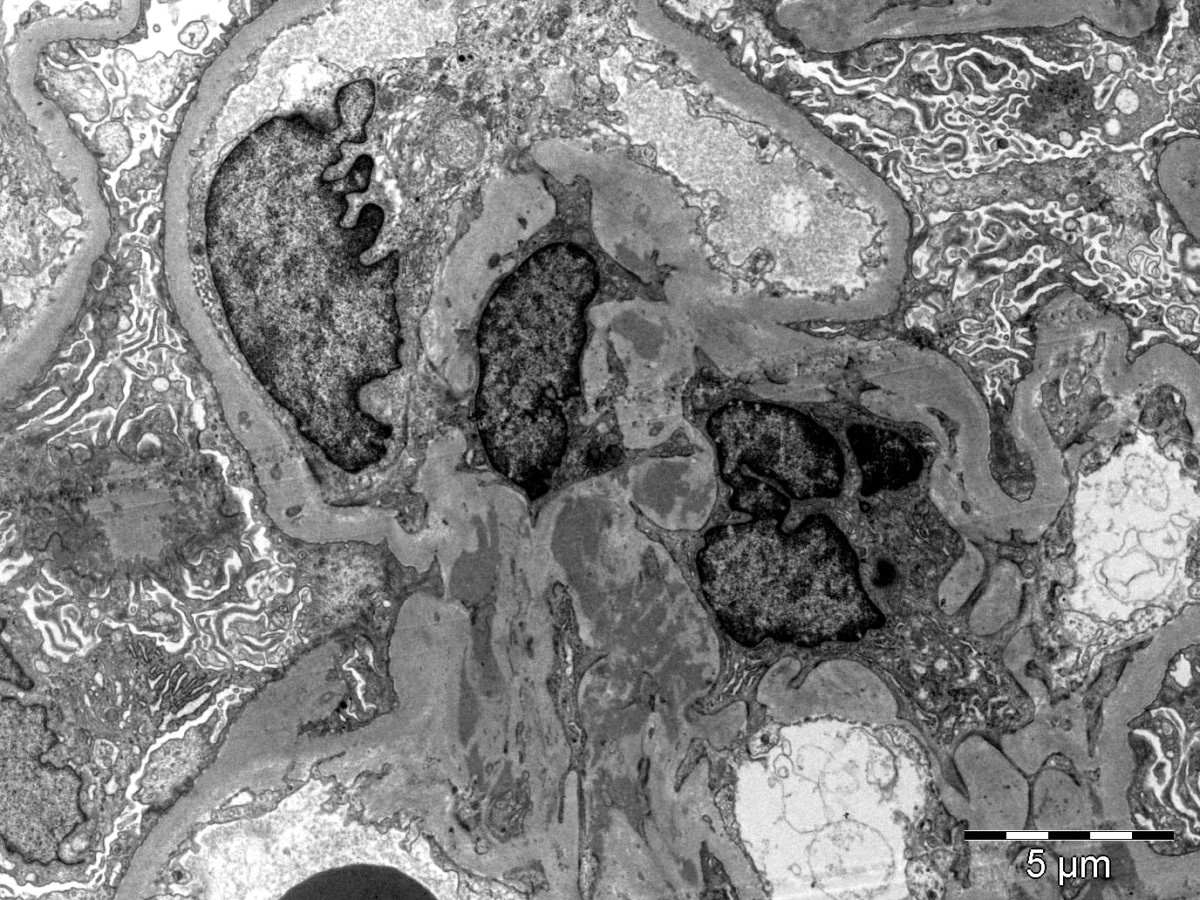
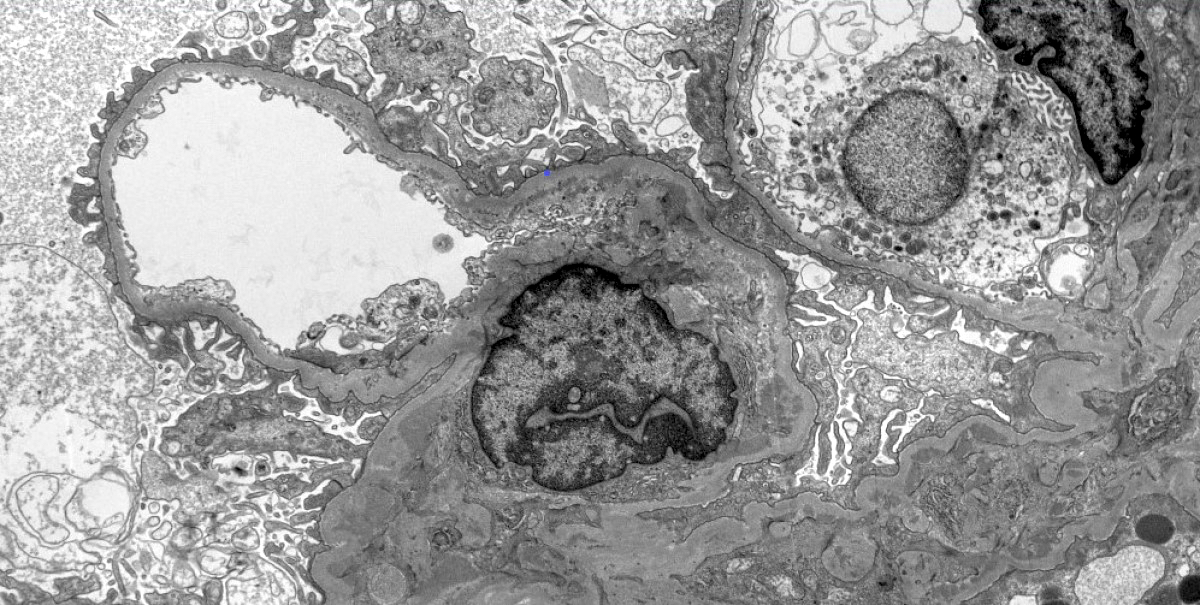
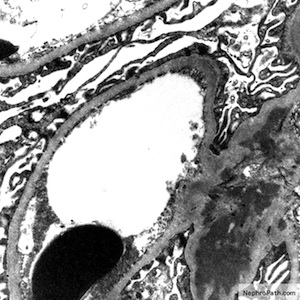
Electron microscopy description
- Electron dense deposits without substructure (Colvin: Diagnostic Pathology - Kidney Diseases, 3rd Edition, 2019)
- Most commonly mesangial
- Subendothelial deposits associated to more active lesions on light microscopy
- Subepithelial deposits exceedingly rare
Electron microscopy images
Genetics
- Family history in 10 - 15% of cases (Colvin: Diagnostic Pathology - Kidney Diseases, 3rd Edition, 2019)
- Autosomal dominant IgA nephropathy identified in a Sicilian family with SPRY2 mutation that causes inhibition of inhibition of MAPK / ERK1/2
- Genome wide association study studies: susceptibility loci at 1q32 (CFH and CFHR1-5 genes), 16p11 (ITGAM / ITGAX), 17p13 (α defensin gene cluster), 8q23 (TNFSF13), 1p13 (VAV3) and 9q34 (CARD9)
Sample pathology report
- Left kidney, core biopsy:
- IgA nephropathy (see comment)
- Comment: There is an IgA nephropathy with diffuse mesangial hypercellularity and focal segmental glomerulosclerosis with podocytopathic features. There is severe chronic tubulointerstitial damage. Oxford classification: M1 E0 S1p T2 C0.
- Specimen: A core of renal cortex containing up to 28 glomeruli in the planes of section.
- Glomeruli: 15/28 are globally sclerosed. 6 show segmental sclerosis, 4 of which with podocytopathic features. There is diffuse mesangial hypercellularity but no endocapillary or extracapillary hypercellularity. Basement membranes appear normal on silver stain. Congo red stain is negative for amyloid.
- Tubules and interstitium: There is severe chronic damage with 60% of the cortex showing interstitial fibrosis and tubular atrophy. There is a mild mononuclear infiltrate, which is confined to the areas of fibrosis. There are uromodulin casts but no red cell casts.
- Vessels: Arteries show moderate fibroelastosis. There is focal arteriolar hyalinosis.
- Immunofluorescence microscopy: There is diffuse mesangial and focal capillary wall positivity for IgA (3+), C3 (1+), kappa (2+) and lambda (3+). IgG, IgM and C1q are negative.
Differential diagnosis
- Henoch-Schönlein purpura nephritis:
- Morphologically indistinguishable
- Clinical information is important for differential diagnosis (e.g. history of purpuric rash, abdominal pain, arthritis)
- IgA dominant infection associated glomerulonephritis (in general, Staphylococcus associated):
- Electron microscopy contains hump shaped deposits
- Mesangial IgA deposits in chronic liver disease:
- Present in 60% of autopsies of cirrhotic patients
- Rarely associated with active glomerular disease (UptoDate: Clinical Presentation and Diagnosis of IgA Nephropathy [Accessed 6 April 2020])
Additional references
Board review style question #1
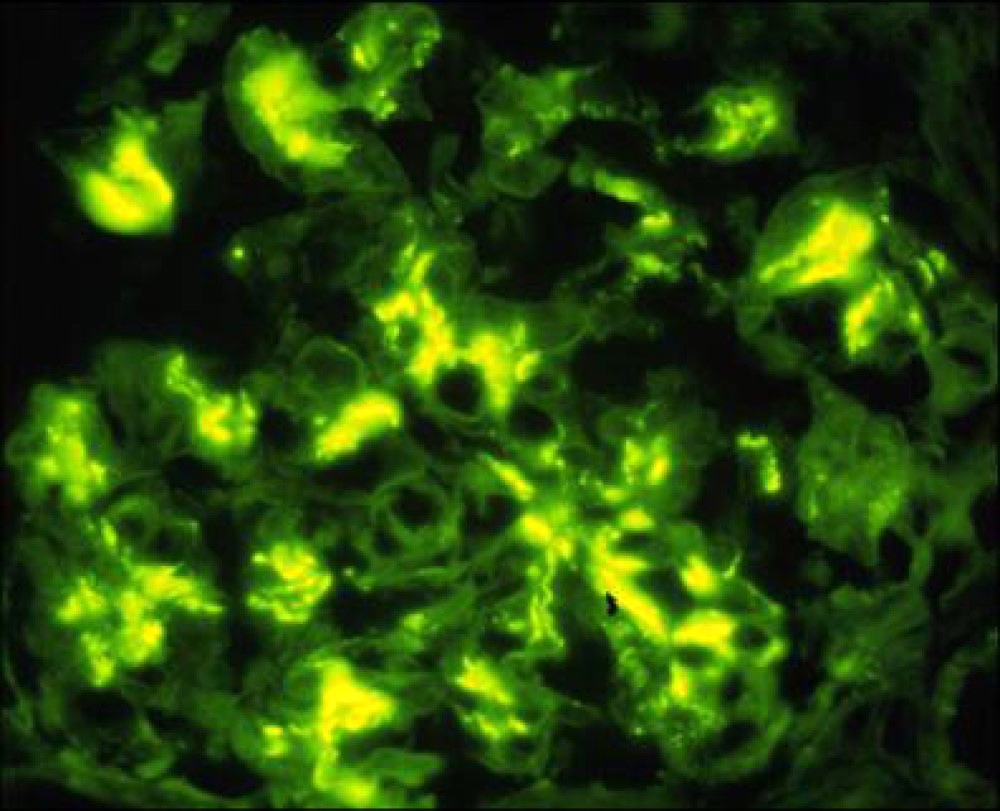
A 32 year old man presents with mild reduction in eGFR, proteinuria and microscopic hematuria. Urine protein / creatinine ratio in nephrotic range. Immunofluorescence microscopy of a renal biopsy core showed mesangial deposition of IgA (strong - see image), C3, kappa and lambda (moderate) and IgG (weak and focal). IgM and C1q were negative. Based on these findings, what is the best diagnosis?
- Accurate diagnosis of a renal biopsy cannot be assigned on the basis of the immunofluorescence findings only
- Alport syndrome
- Immunoglobulin A nephropathy
- Lupus nephritis
- Membranous glomerulonephritis
Board review style answer #1
Board review style question #2
Indicate the correct association in the Oxford classification of IgA nephropathy
- Absence of necrosis / karyorrhexis - NO
- Crescents in 10% of glomeruli - C2
- Interstitial fibrosis / tubular atrophy in 25 - 50% of the cortex - T2
- Presence of endocapillary hypercellularity - E1
- Presence of segmental sclerosis in > 50% of glomeruli - S2
Board review style answer #2