Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Dasgupta AD, Nadasdy T. Fibrillary glomerulonephritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneyfibrillarygn.html. Accessed March 31st, 2025.
Definition / general
- Glomerular disease caused by the deposition of randomly oriented, nonperiodic noncongophilic fibrils with a mean diameter of 20 nm
Essential features
- Rare form of glomerulonephritis characterized by organized, nonbranching fibrils in random orientation with a diameter of 15 - 25 nm and without a hollow core
- Most deposits are positive for IgG, C3 and kappa and lambda light chains and are negative for Congo red
- DNAJB9 heat shock protein comprises a major component of the fibrils and IHC for DNAJB9 is sensitive and specific for fibrillary glomerulonephritis
- Treatment options are limited, prognosis is poor and transplant recurrence is frequent
- Most patients present with a variable degree of proteinuria
Terminology
- Fibrillary glomerulopathy
ICD coding
- ICD-10: N03.8 - chronic nephritic syndrome with specified morphological changes
Epidemiology
- Middle aged to older adults, most studies show a mean age close to 55 years (range of 20 - 80 years)
- Slight female predominance (M:F = 1.0:1.3 - 1.8)
- Most frequently seen in White patients (up to 87%)
- Can be seen in association with malignancy (more frequently solid organ neoplasms, up to 23% of patients), hepatitis C virus infection (up to 23%) and autoimmune diseases (13 - 30%) (Am J Nephrol 2017;45:248)
Sites
- Kidneys
- Rare cases of splenic and pulmonary involvement have been reported (Ultrastruct Pathol 2008;32:113, N Engl J Med 1992;326:36)
Pathophysiology
- In fibrillary glomerulonephritis (FGN), there is an abnormal deposition of haphazardly arranged fibrils with a diameter between 15 and 25 nm in most cases (Kidney Int Rep 2019;4:917)
- These fibrils are composed of DNAJB9 (a heat shock protein that is a chaperone in the endoplasmic reticulum), IgG (mainly IgG1 and IgG4) and components of the classical complement pathway
- Exact pathophysiology of fibrillary glomerulonephritis is not yet completely understood but studies indicate that DNAJB9 may act as an autoantigen that elicits an autoimmune response with abnormal deposition of DNAJB9, IgG and complement components within the kidney
Etiology
- Etiology is poorly understood
- DNAJB9 may act as an autoantigen that elicits an abnormal autoimmune response with DNAJB9, IgG and complement components abnormally deposited within the kidney in a fibrillary structure (Kidney Int Rep 2019;4:917)
Clinical features
- Most patients present with a variable degree of proteinuria, which is commonly within the nephrotic range; the disease is usually insidious and the diagnosis is frequently made when patients are already in an advanced stage with chronic renal failure (Clin J Am Soc Nephrol 2019;14:1741)
- Can be seen in association with malignancy (more frequently solid organ neoplasms, up to 23% of patients), hepatitis C virus infection (up to 23%) and autoimmune diseases (13 - 30%)
Diagnosis
- Renal biopsy with the characteristic light microscopic, immunofluorescence, immunohistochemical and ultrastructural findings is currently the only means of definitive diagnosis (Kidney Int Rep 2019;4:917)
Laboratory
- Patients usually present with proteinuria (Am J Kidney Dis 2013;62:679, Am J Kidney Dis 2015;66:e27)
- Proteinuria seen in most patients (mean urine protein is between 4.1 and 7.3 g/d)
- Full nephrotic syndrome (nephrotic range proteinuria, low serum albumin, edema) is seen in 25 - 69% of patients
- Microscopic hematuria is seen in 25 - 95% of patients
- Decreased renal function is seen in ~67% of patients (mean serum creatinine between 2.1 and 3.7 mg/dL)
- Acute decline in renal function can be seen in patients whose fibrillary glomerulopathy is associated with crescent formation
- Patients usually (> 90%) have normal serum complement levels
- Monoclonal serum or urine protein is rarely present
- Majority of which are thought to be a coincidental finding due to the age of the patient population and frequent lack of concordance with the staining seen in the glomeruli
- Monoclonal fibrillary glomerulonephritis is rare (3 - 11% of cases) and the monoclonality of the deposits must match what is seen in the serum or urine (see Immunofluorescence description for additional information)
- References: Kidney Int 2003;63:1450, Clin J Am Soc Nephrol 2011;6:775
Prognostic factors
- Overall prognosis is poor, with 33 - 50% of patients advancing to end stage renal disease (ESRD) within 4 years of diagnosis (Kidney Int 2019;96:581)
- Poor prognostic factors include advanced age, elevated serum creatinine levels and extent of glomerulosclerosis, tubular atrophy and interstitial fibrosis
- Black patients with concomitant hepatitis C virus infection and fibrillary glomerulonephritis have an exceptionally poor renal prognosis (Am J Nephrol 2017;45:248)
- Patients with ESRD due to fibrillary glomerulonephritis show no difference in mortality compared to those with ESRD from other causes (Am J Nephrol 2015;42:177)
Case reports
- 63 year old man with hypertension, edema, proteinuria, monoclonal gammopathy of undetermined significance (MGUS) and fibrillary glomerulonephritis (Cureus 2023;15:e47862)
- 63 year old man with cirrhosis secondary to hepatitis C virus, multiple myeloma and fibrillary glomerulonephritis (Cureus 2022;14:e28250)
- 66 year old woman with vulvar squamous cell carcinoma and fibrillary glomerulonephritis (Cureus 2023;15:e35068)
Treatment
- Unfortunately, no therapies have been shown to clearly improve outcomes in patients with fibrillary glomerulonephritis
- Some studies indicate that almost 50% of patients with fibrillary glomerulonephritis will progress to ESRD within 5 years of diagnosis (Clin J Am Soc Nephrol 2011;6:775)
- Fibrillary glomerulonephritis can recur in the renal allograft, with recurrence rates of up to 50% reported
- Recurrence usually occurs after several years with one study reporting a median time to recurrence of 10 years (Am J Kidney Dis 2020;76:500)
- References: Am J Kidney Dis 2015;66:e27, Kidney Int Rep 2020;6:239
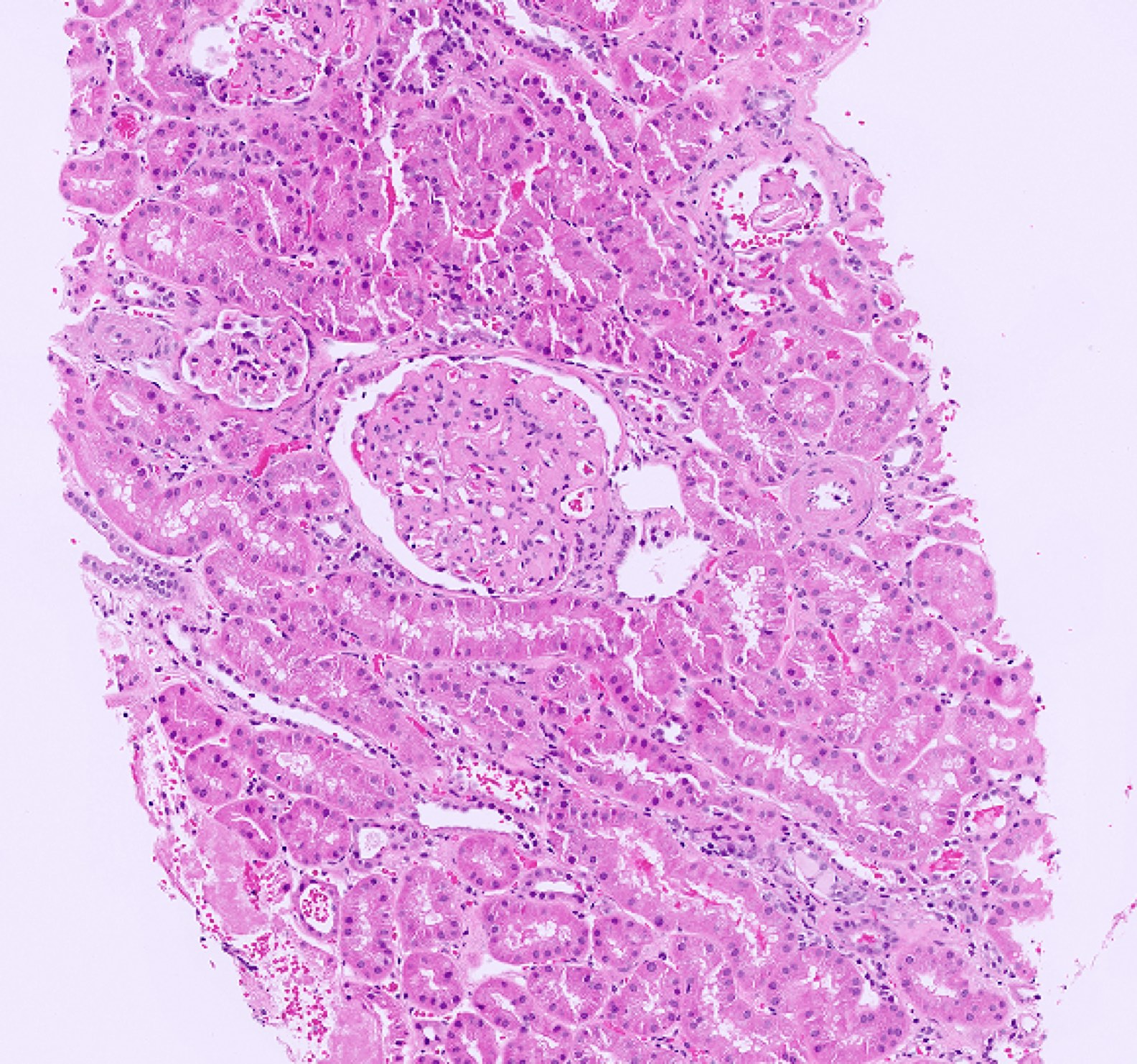
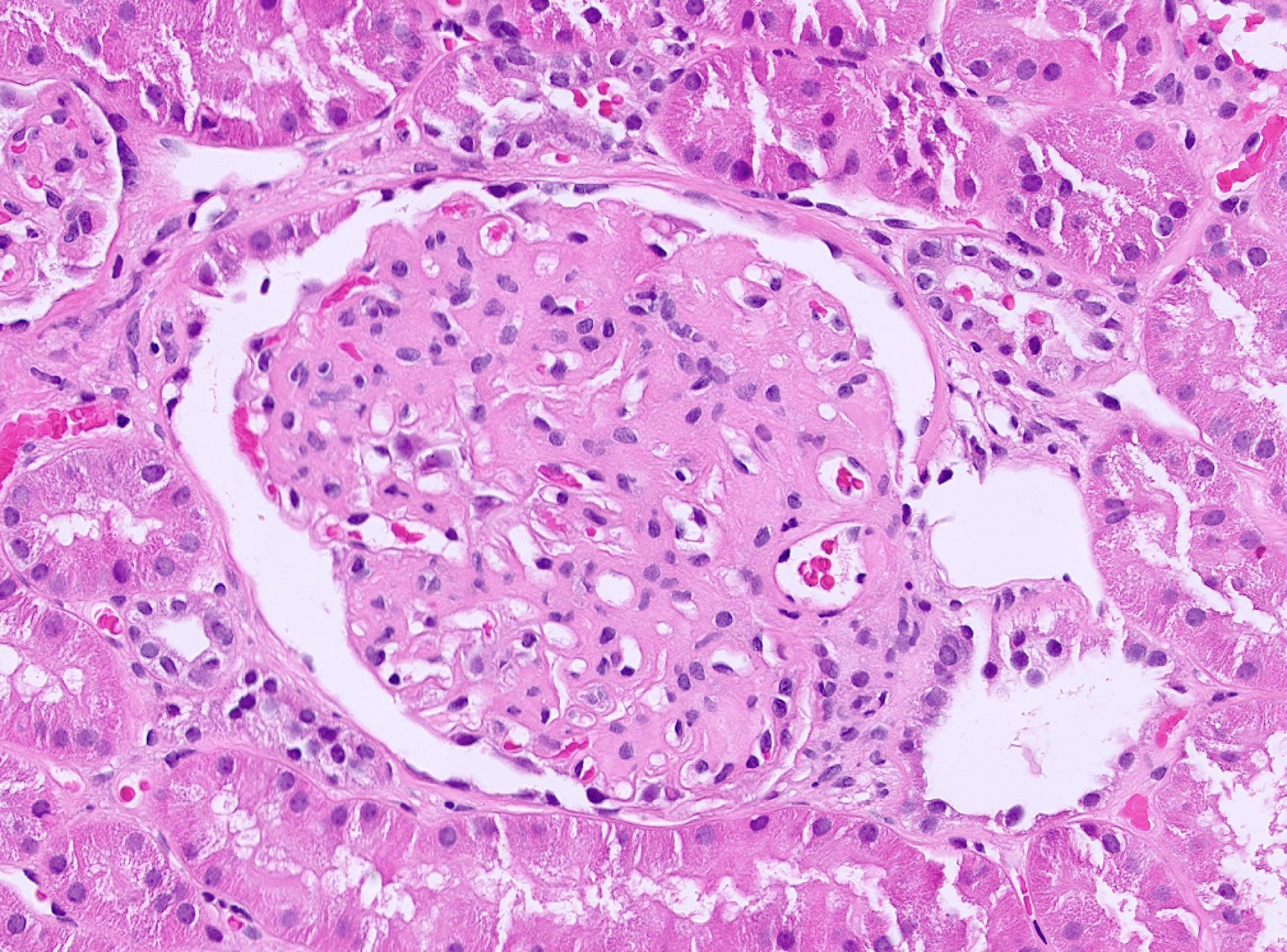
Microscopic (histologic) description
- Fibrillary glomerulonephritis can cause several histologic patterns (Clin J Am Soc Nephrol 2011;6:775)
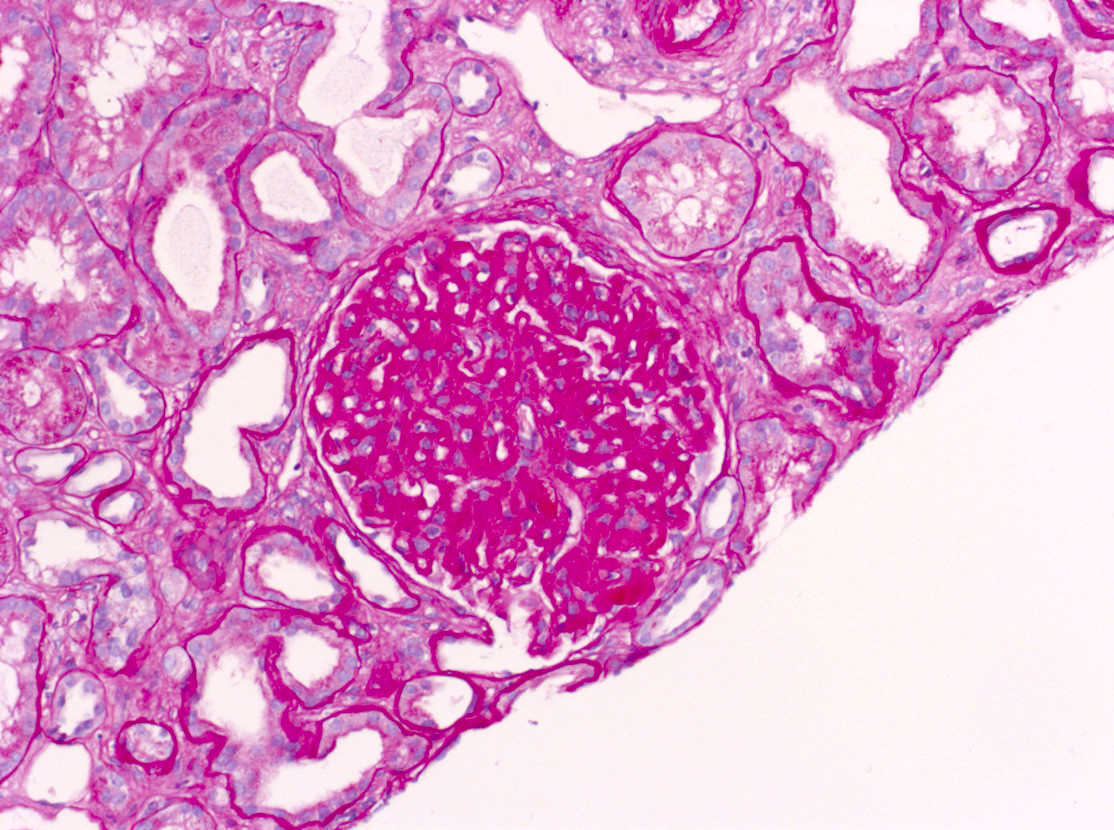
- Most common glomerular finding is mesangial expansion by eosinophilic material that is PAS positive, silver negative or weak and Congo red negative; this characteristic finding gives a moth eaten appearance similar to that described in amyloidosis (Case Rep Med 2013;2013:935172)
- In more advanced cases, there is glomerular capillary wall thickening owing to fibrillary deposits in the glomerular basement membrane (GBM)
- Glomerular hypercellularity is usually mild
- Occasionally, the fibrils can be seen in the tubular basement membranes and vessel walls, although usually only appreciated on immunohistochemistry or immunofluorescence staining
- Other glomerular patterns include
- Membranoproliferative pattern with focal glomerular basement membrane duplication (Cureus 2023;15:e47862)
- Crescentic glomerulonephritis
- May occur in up to 25% of cases
- Usually a focal process but has rarely been reported as diffuse (over 50% glomerular involvement by crescents)
- Crescentic disease portends a worse prognosis (Am J Kidney Dis 2023;81:368)
- Secondary segmental sclerosis can be seen
- Tubular atrophy and interstitial fibrosis are common findings but the extent can vary depending on the severity and chronicity of the disease
- Congo red staining is negative
- Rare Congo red positive cases have been reported but these may represent concomitant amyloid deposition
- If the Congo red stain is positive, mass spectrometry testing is recommended to exclude renal amyloidosis
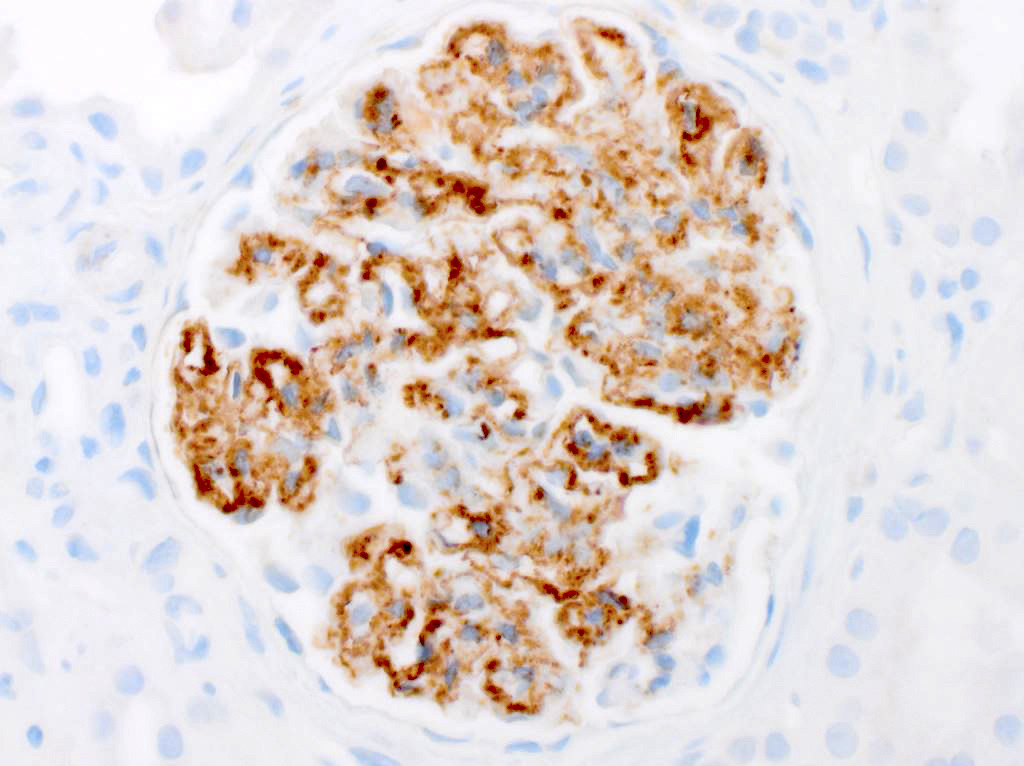
- DNAJB9 immunohistochemical stain is very sensitive and specific (up to 99% reported for both) (Kidney Int Rep 2017;3:56)
- References: Cureus 2022;14:e26001, Am J Kidney Dis 2015;66:e27
Microscopic (histologic) images
Immunofluorescence description
- Bright mesangial and glomerular capillary wall staining for IgG
- Staining can appear smudgy to granular
- Most cases are IgG4 dominant (90%) with colocalization of IgG1 (80%)
- Rare cases are positive for IgG1 only (10%)
- Most cases show equal kappa and lambda light chain staining (85%)
- Rare cases appear monotypic, usually kappa light chain
- Staining for C3 (92%), C1q (60%), IgM (47%) or IgA (28%) can also co-occur; however, staining for these antigens is usually less intense than that seen with IgG
- Staining within the arteries or tubular basement membranes can also occur
- References: Kidney Int Rep 2019;4:917, Kidney Int 2019;96:581, Kidney Int Rep 2022;8:202
Immunofluorescence images
Positive stains
- DNAJB9
- Immunohistochemical stain for DNAJB9, a member of the heat shock protein family
- Positive staining within the mesangium and capillary walls (Biomedicines 2022;10:2102)
- Has a sensitivity of 88 - 98% and specificity of > 99%
- Reference: Kidney Int Rep 2017;3:56
Negative stains
- Congo red
- Should be negative but congophilic fibrillary glomerulonephritis has been reported (Am J Kidney Dis 2018;72:325)
- If it is positive, consider a diagnosis of renal amyloidosis
- Staining for DNAJB9 and mass spectrometry testing should be considered to differentiate between fibrillary glomerulonephritis and renal amyloidosis (Kidney Int Rep 2017;3:56)
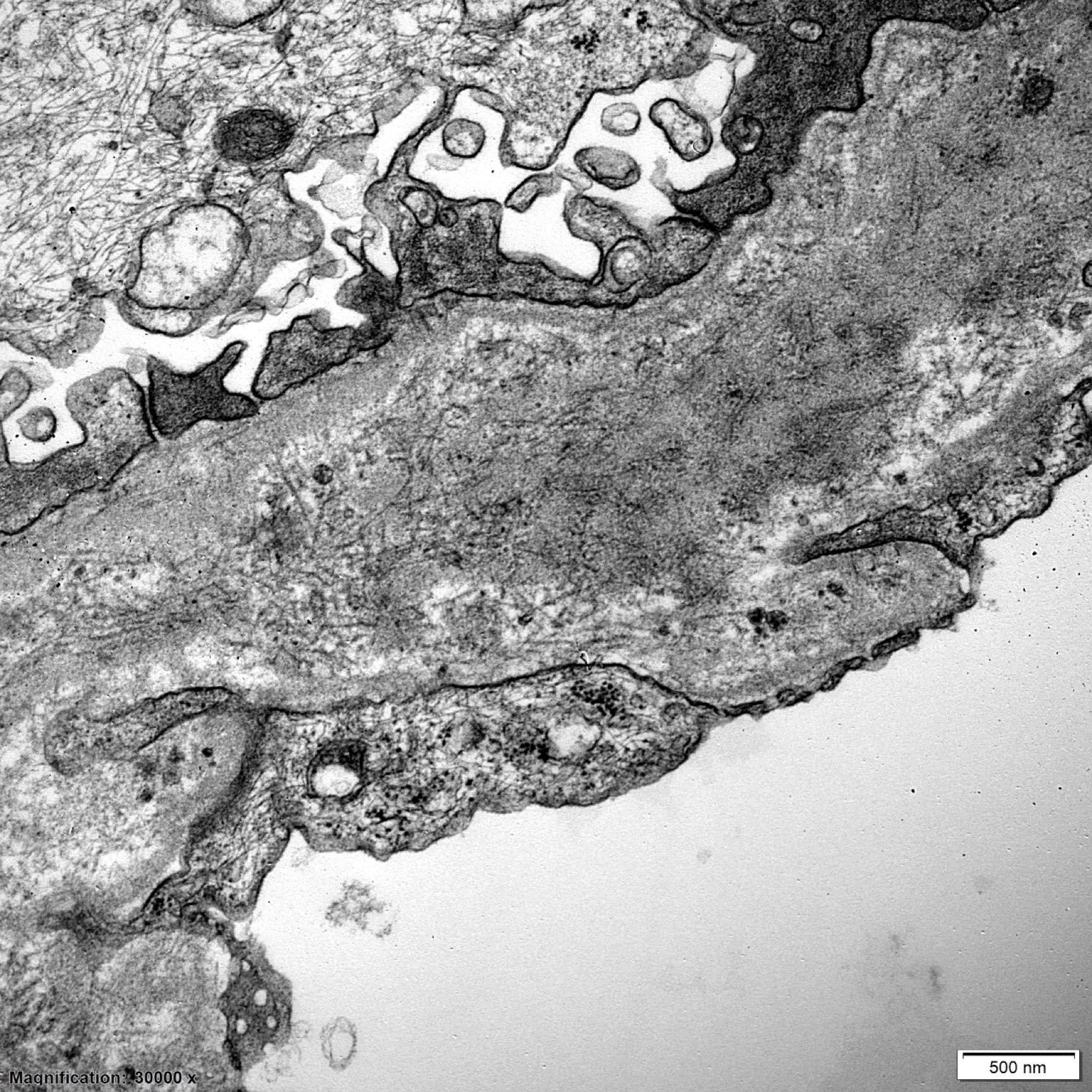
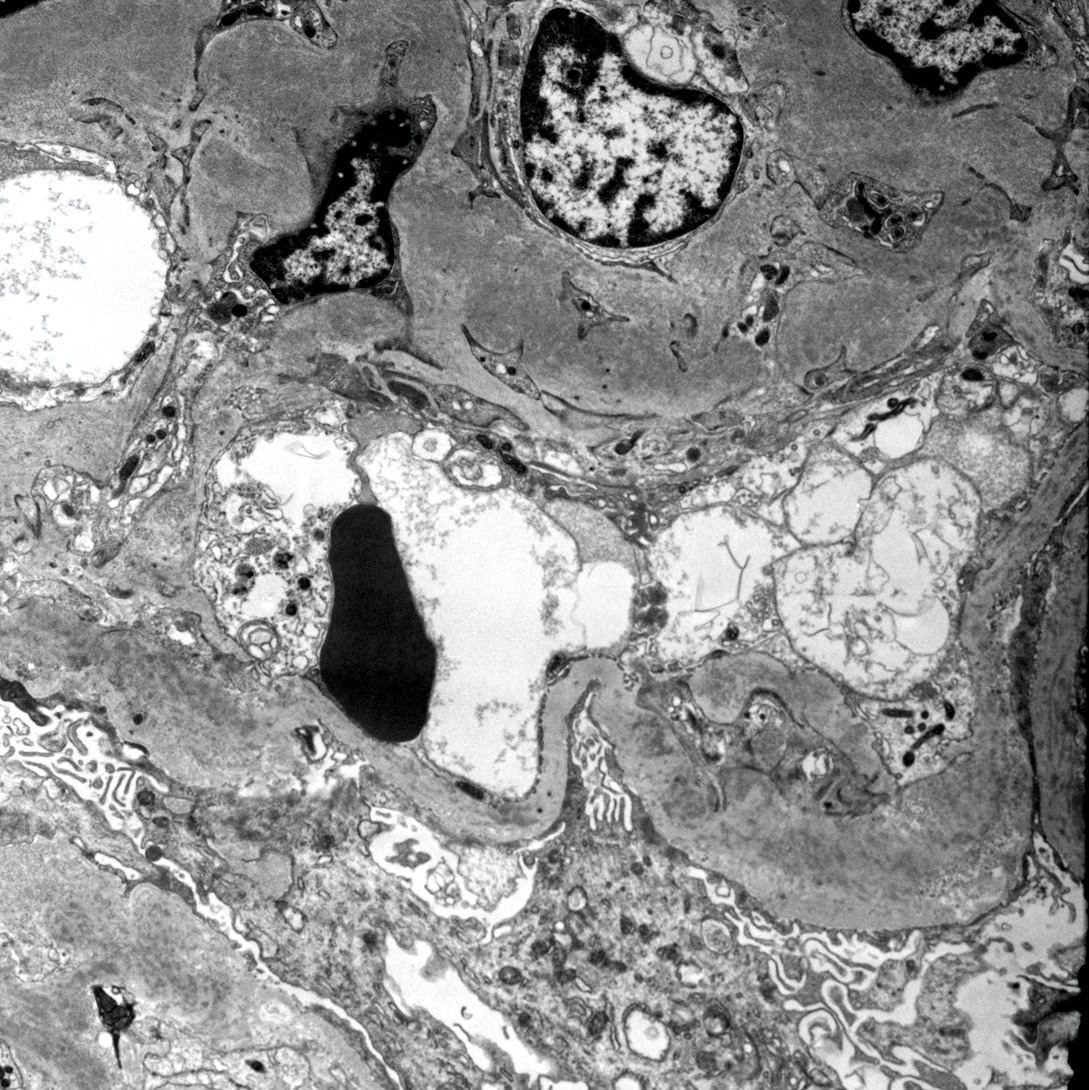
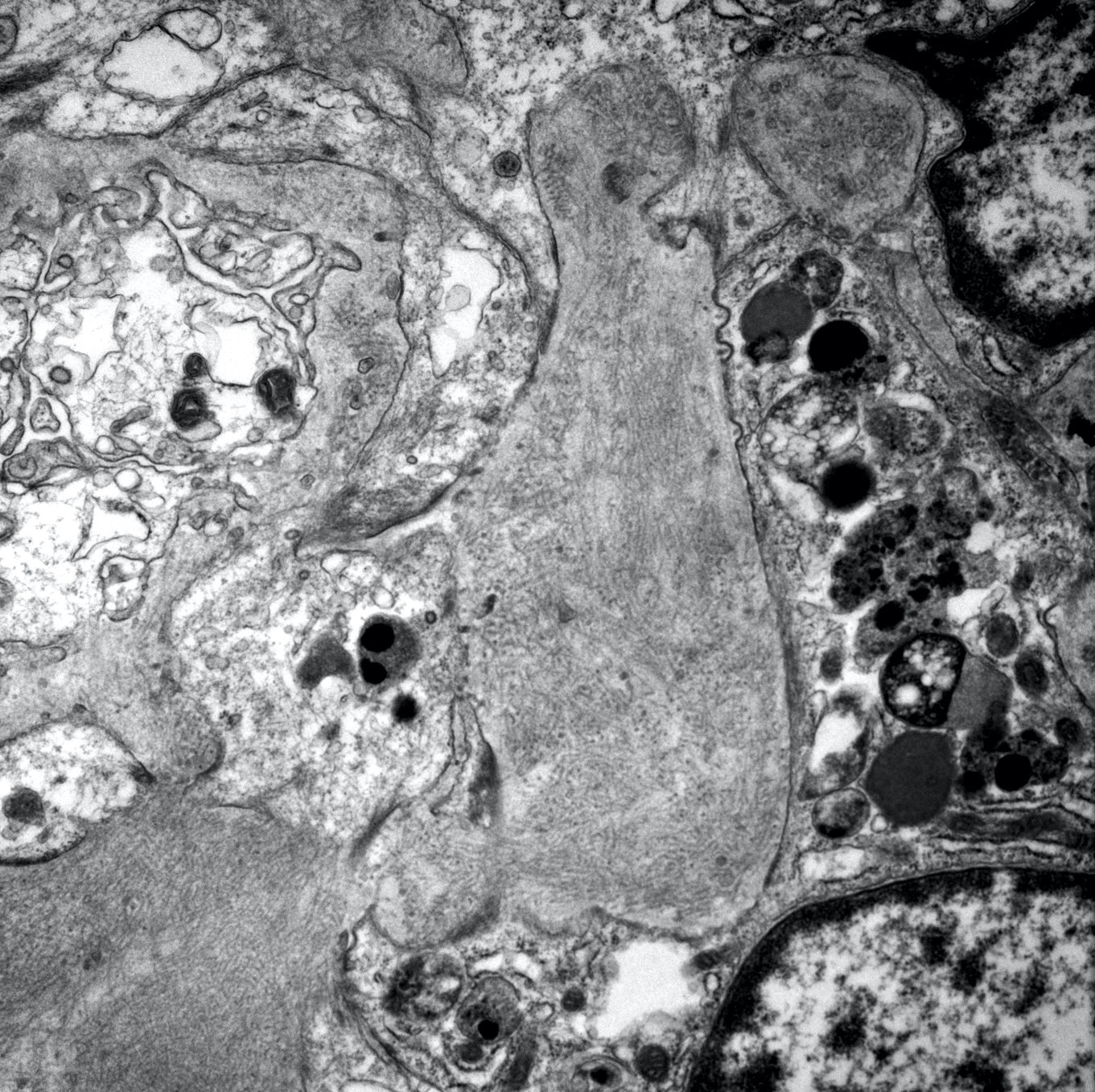
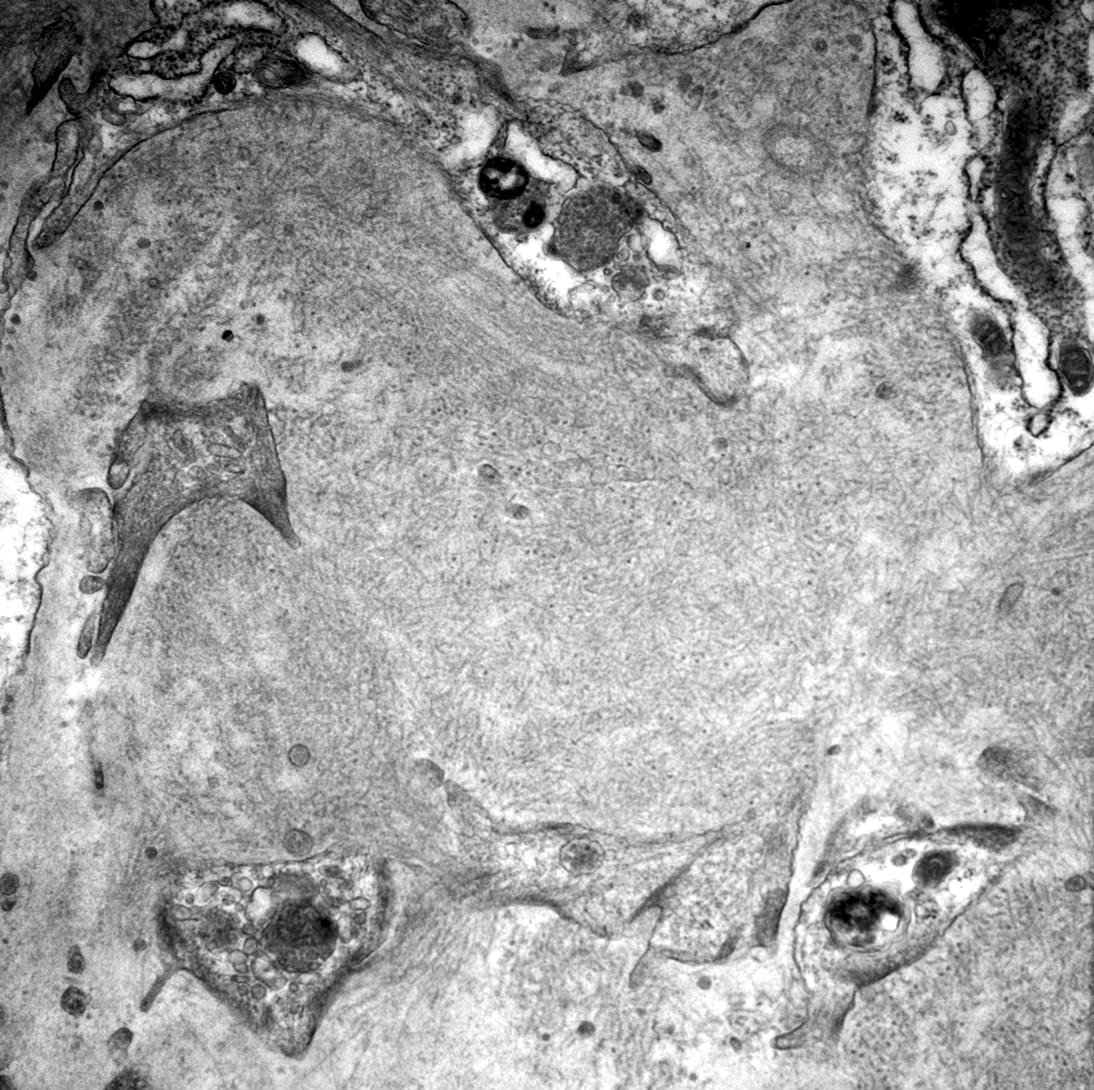
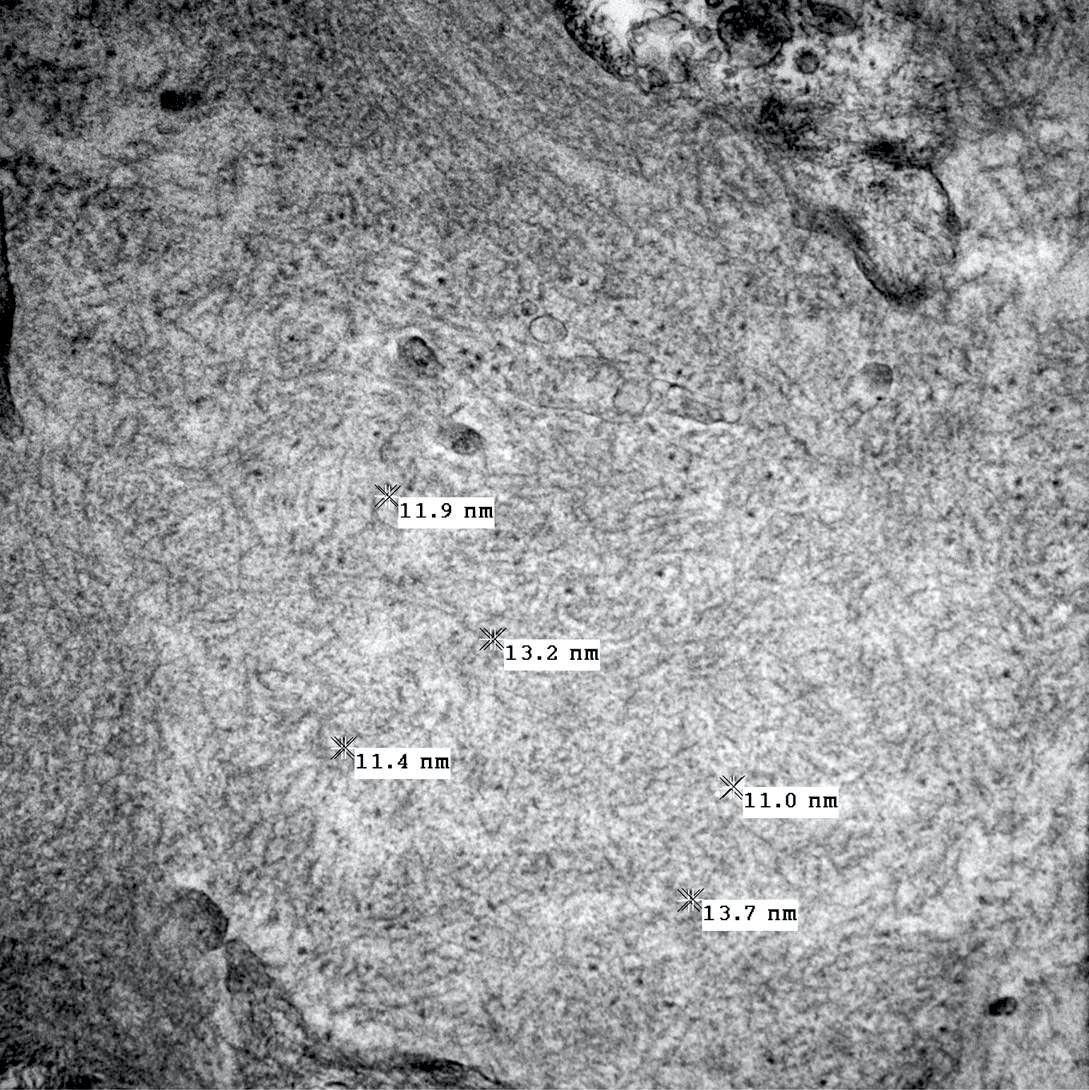
Electron microscopy description
- Nonbranching, haphazardly arranged fibrils with an average diameter between 15 and 25 nm are found within the mesangium and glomerular basement membranes (GBM) (Kidney Int Rep 2019;4:917, Kidney Int Rep 2020;6:239)
- These fibrils should lack a hollow core (they are not microtubules)
- Fibrillary deposits can occasionally be seen within the tubular basement membranes
Electron microscopy images
Sample pathology report
- Kidney, native, biopsy:
- Fibrillary glomerulonephritis (see comment)
- Comment: The biopsy shows enlarged glomeruli with mesangial expansion by material that is silver and Congo red negative. Immunofluorescence shows polyclonal IgG (IgG1 and IgG4) and C3 staining within the mesangium and capillary walls. Electron microscopy confirms the presence of haphazardly arranged fibrils with a mean diameter of 15 nm within the mesangium and glomerular basement membrane. An immunohistochemical stain for DNAJB9 is positive in these areas as well. Overall, these findings are consistent with a diagnosis of fibrillary glomerulonephritis. The background cortex shows focal global glomerulosclerosis (20%) and mild tubular atrophy and interstitial fibrosis.
- Clinical history: The patient is a 65 year old man who presents with a history of proteinuria and decreased renal function. Medical history includes diabetes, hypertension and obesity. Serum creatinine has gradually increased from 1.0 mg/dL to 1.5 mg/dL over the past 2 years. Urinalysis shows proteinuria (3.7 g/24 h) without hematuria. Autoimmune, infectious and monoclonal testing are negative.
- Light microscopy: Sections stained with H&E, PAS, Jones and trichrome contain 3 cores of the renal cortex (60%) and medulla (40%). Up to 15 glomeruli are present per section, 3 of which are globally sclerosed. The patent glomeruli are slightly enlarged but normocellular. There is mesangial expansion by eosinophilic material that is PAS positive but appears negative on silver and Congo red stains. A DNAJB9 immunohistochemical stain is positive within the mesangium and segmentally along glomerular capillary loops. No crescents, necrosis or thrombi are identified. There is mild tubular atrophy and interstitial fibrosis, estimated to involve 20% of the cortical sample. The preserved proximal tubules are unremarkable. There is focal mononuclear interstitial inflammation primarily in areas of atrophy. Up to interlobular size arteries are sampled and show moderate fibrointimal thickening. The arterioles show mild hyaline deposition.
- Immunofluorescence microscopy: 4 glomeruli are available for evaluation by immunofluorescence microscopy. Granular staining is seen within the mesangium and segmental glomerular capillary walls for IgG (3+), IgG1 (1+), IgG4 (3+), C3 (2+) and kappa (3+) and lambda (3+) light chains.
- Electron microscopy: Semithin sections contain renal cortex with 2 glomeruli, both of which are examined under the electron microscope. Ultrastructurally, there are innumerable haphazardly arranged fibrils within the mesangium and glomerular basement membranes. These fibrils have a mean diameter of 15.2 nm (+/- 1.2 nm). Podocyte foot process effacement is mild and segmental. No tubuloreticular inclusions are seen. Tubular basement membranes are unremarkable.
Differential diagnosis
- Immunotactoid glomerulopathy:
- Material deposited in the glomeruli is also silver and Congo red negative
- Ultrastructurally, in most cases the immuntactoid organized substructure is localized to otherwise electron dense discrete deposits (the substructure may not be evidence on low magnification under the electron microscope)
- Usually monoclonal staining is seen on immunofluorescence (mostly IgG1 kappa) (Kidney Int 2003;63:1450)
- Substructure consists of hollow tubules arranged in parallel arrays with a larger diameter (usually 20 - 90 nm)
- Renal amyloidosis:
- Diabetic nephropathy:
- Diffuse linear accentuation of the GBM and tubular basement membrane (TBM) with IgG, kappa and lambda light chains and albumin
- Expanded mesangium positive for PAS, silver and trichrome
- Glomerular fibrillary deposits are noncongophilic and DNAJB9 negative (Lab Invest 2024;104:100322)
- Membranous glomerulopathy:
- Fibrillary GN may resemble membranous glomerulopathy immunofluorescent staining
Additional references
Board review style question #1
A 65 year old woman presents to her nephrologist with decreased renal function, proteinuria and hematuria. She undergoes a renal biopsy which shows mesangial expansion by silver and Congo red negative material within the glomeruli. Immunofluorescence reveals dominant polyclonal staining for IgG within the mesangium and glomerular capillary walls. Electron microscopy shows haphazardly arranged fibrils with a mean diameter of 18 nm within the mesangium and glomerular basement membrane. What is the diagnosis?
- Fibrillary glomerulonephritis
- Immunotactoid glomerulopathy
- Proliferative glomerulonephritis with monoclonal IgG deposits
- Renal amyloidosis
Board review style answer #1
A. Fibrillary glomerulonephritis. Fibrillary glomerulonephritis frequently presents with proteinuria, hematuria and decreased renal function. It causes mesangial expansion by eosinophilic material that is Congo red negative with polyclonal IgG staining on immunofluorescence. The presence of haphazardly arranged fibrils with a mean diameter of 15 nm is diagnostic.
Answer D is incorrect because for renal amyloidosis, the material expanding the mesangium would be Congo red positive. The fibrils should have a smaller mean diameter (8 - 12 nm).
Answer C is incorrect because the immunofluorescence pattern is not monoclonal and there are organized (fibrillary) deposits.
Answer B is incorrect because for immunotactoid glomerulopathy, the material expanding the mesangium would likely be monoclonal and the deposits would consist of microtubules with a hollow core and larger mean diameter (14 - 90 nm).
Comment Here
Reference: Fibrillary glomerulonephritis
Comment Here
Reference: Fibrillary glomerulonephritis
Board review style question #2
A renal biopsy from an elderly woman shows mesangial expansion by eosinophilic material that is silver and Congo red negative. Immunofluorescence shows polyclonal IgG deposition within the mesangium and glomerular basement membranes. The image above is seen on electron microscopy. Fibril diameter ranges from 15 to 25 nm. What is the best diagnosis?
- Fibrillary glomerulonephritis
- Immunotactoid glomerulopathy
- Lupus nephritis
- Renal amyloidosis
Board review style answer #2
A. Fibrillary glomerulonephritis. Fibrillary glomerulonephritis frequently presents with proteinuria, hematuria and decreased renal function. It causes mesangial expansion by eosinophilic material that is Congo red negative with polyclonal IgG staining on immunofluorescence. The presence of haphazardly arranged fibrils with a diameter of 15 - 25 nm is diagnostic.
Answer D is incorrect because, for renal amyloidosis, the material expanding the mesangium would be Congo red positive. The fibrils should have a smaller diameter (8 - 12 nm).
Answer C is incorrect because lupus nephritis would have full house immunofluorescence staining and would not show fibrillary deposits on electron microscopy.
Answer B is incorrect because for immunotactoid glomerulopathy, the material expanding the mesangium would likely be monoclonal and the deposits would consist of microtubules with a hollow core and larger diameter (14 - 90 nm).
Comment Here
Reference: Fibrillary glomerulonephritis
Comment Here
Reference: Fibrillary glomerulonephritis